Abstract
The main objective was to find association between basal cortisol and neighborhood-level stress. Systematic searches, including electronic and hand searches, were conducted. The most recent date of the search was July 26, 2013. Primary observational studies included if they considered stress related outcomes in the neighborhood context. Using the EndNote X7 advanced search option; the authors examined the abstracts and titles of the 18,092 articles to exclude obviously irrelevant studies, gray literature, discussion papers, reviews and, studies with no complete data. Two authors independently extracted data from the original reports into pre-designed data extraction forms based on the Data Extraction Template of the Cochrane Consumer and Communication Review Group (CCCRG). Ten studies with a total of 2,134 participants were synthesized and analyzed. Two studies out of ten received expanded meta-analysis. The overall effect size (95% CI) for cortisol level for residents in neighborhoods with lower stress compared to inhabitants from higher was 0.12 (0.01, 0.23). This review is demonstrating a link between psychosocial or physical stress and cortisol obtained from saliva. However, living in high disorder neighborhoods results in higher level of cortisol. This represents a biological indicator of psychosocial/physical stress exposure (i.e., neighborhood disorder) that reflects variances in stress exposure levels.
Keywords: Urban stress, Community health, Environmental stress
Introduction
Investigations of health condition based on neighborhood boundaries date back nearly a century (1). However, later, the association between deteriorated regions and health, including behaviors and physical and mental health outcomes, were studied by Myerson (2). Today, a variety of theoretical and analytical models has identified the direct and indirect pathways between neighborhoods and health. These studies fall into three main domains, physical, psychosocial and biological, or involve a combination of the three. Whereas, there has been more emphasis on the physical and psychosocial aspects, this review emphasizes on biological factors. To be more precise, one of the most significant currently limitations are the lack of validated biomarkers to prove the underlying mechanisms through which neighborhood affect health.
Cortisol that is produced by stimulation of the hypothalamic-pituitary-adrenal (HPA) axis in response to stressors has been used as a biomarker in the study of neighborhoods in the last two decades (3–5). Nonetheless, in the study of environmental health, using cortisol as a biomarker could lead to the tracking of several health disparities, including cardiovascular disease, obesity and hypertension (6–8).
In past decades, different types of cortisol tests have been used to measure distinctive neighborhood stressors (9–11). Although there are number of stress biomarkers, cortisol is still the most commonly used for stress measurements due to the wide regulatory function it does in the nervous system, immune and metabolic system (12). It is one of the key molecules in exposure disease outcomes, which mediate the effect of stress.
On April 7, 2010, which has been nominated as Urban Health Day, the World Health Organization announced the essential contribution of urban planning as a first action for healthy behaviors and safety. This action significantly increases the chance of people to enjoy better urban living conditions. Likewise, understanding of the early roots of health disparities has been emphasized through other organizations such as the American Academy of Pediatrics. Health inequalities remain an important public health challenge, and early deaths have excessively been reported in disadvantaged neighborhoods (13). Despite this large body of literature identifying the significance of assessment, there is a lack of evidence from systematic or meta-analysis reviews regarding the biological risk factors in the neighborhood context. The main objective of this study is to assess cortisol as a stress biomarker in the neighborhood context in terms of lower-stress neighborhoods compared with higher-stress neighborhoods.
Methods
Data sources
Systematic searches were conducted for studies, which there were no publications status, no language or publication year limitations. July 26, 2013 was the last date of the searches.
Electronic searches
The following databases were searched as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0(14).
- Bibliographic databases
- Cochrane Central Register of Controlled Trials (CENTRAL),
- MEDLINE,
- EMBASE,
- General search engines; Google scholar, TRIP,
- Subject databases (Communi-tyWISE, Social Care Online, Social Services Abstracts, ASSIA, C2 SPECTR, PsycINFO, Social Policy and Practice, Sociological Abstracts),
- Citation indexes (Scopus, SciSearch, Web of knowledge, Social Sciences Citation Index),
- Dissertation and thesis (Index to Theses in Great Britain and Ireland, ProQuest Dissertation & Theses Database, DissOnline), and
- Gray literature (OpenSIGLE, HMIC, NTIS, PsycEXTRA)
- Journal and non-bibliographic-databases
- BioMed Central,
- PLoS,
- PMC,
- Free Medical Journals,
- HighWire Press, and
- Conference abstracts (Asco, Bio-sis, ISI Proceedings, RRM)
Unpublished and on-going studies.
Searching other resources
We supposed that searching other resources resulted in the risk of missing relevant studies were mitigated. The reference lists of recognized studies were examined for additional sources, and the authors were contacted when necessary. In addition, Google, PubMed and TRIP database were searched to retrieve existing literature reviews related to the study. Full electronic search strategies presented in databases search strategies.
Inclusion and exclusion criteria
Studies with observational design and a quantitative approach were selected for this review. Only primary research studies with primary or second ary data were considered. Primary data included face-to-face interviews, questionnaire, observation, census data and secondary data included national surveys, national programs including National Health and Examination Survey, Chicago Community Adult Health Study and Boston Metropolitan Immigrant Health and Legal Status Survey. Studies involving adults (18 years of age or older) who had not special disease included in the analysis. The main outcomes were detecting neighborhood stressors and developing cortisol as a neighborhood stress biomarker. Stress was the primary outcome and to be eligible for inclusion, a study should include at least one of the stress outcomes. However, secondary outcomes were depression, anxiety, cognitive ability, substance use, diet, drug, mortality, morbidity, cancers, and smoking, but only primary outcomes were counted in the meta-analysis. Pairs of authors examined the abstracts/titles and independently screened them for appropriateness, according to this criterion: studies with stress-related outcomes that were influenced by urban areas at the district or neighborhood-level. Using the Endnote X7 advanced search option; the authors considered the abstracts and titles of the remaining 353articles to remove clearly irrelevant reports that were: not stress related outcomes, not urban areas related investigations, gray literature such as meeting abstracts, reviews or meta-analyses, discussion papers or a guideline not a research paper and related to animals not human. A list of final exclusion for twenty studies and the reason for exclusion is included in the characteristics of excluded studies (7, 15–33).
Data extraction
Two authors extracted data from the original reports into pre-designed data extraction forms independently, based on the Cochrane Consumer and Communication Review Group (CCCRG) Data Extraction Template available on http://cccrg.cochrane.org/. The extracted data included the following (see characteristics of studies):
GENERAL: contact detail, author, title of paper and year of publication
PARTICIPANT: age, gender, ethnicity and sample size
CONTEXT: methods used and neighborhood characteristics assessed
OUTCOMES: names of stress outcomes, type of outcomes (primary or secondary), the tools used and results related to the stress.
The review authors evaluated the procedural quality of the studies included using a quality assessment checklist of the Cochrane Collaboration’s Risk code (14). Unclear bias judged when there is insufficient information, low and high risks coded as follows:
Selection bias (random allocation):
Low risk; random computer-selection or random numbers
High risk; name or data of birth
Detection bias (blinding): however, to these types of studies is incredibly difficult and in some cases impossible. Nonetheless, the outcome assessors could be blinded was coded as following:
Low risk; it is unlikely that blinding could be broken
High risk; no blinding or could had been broken
Attrition bias (Incomplete data)
Low risk; no missing data or attrition rate High risk; reasons for missing data not provided or inequity of numbers
Selective reporting
Low risk; primary and secondary outcome measures had been reported in a pre-defined method
High risk; not the study’s entire outcome measures had been reported or fail to include results from a key outcome that could be expected
Other sources of bias
Low risk; there were no other sources of bias
High risk; possible sources of bias associated to the specific study design
For each study effect size calculated from mean differences and standard deviation as bellow:
. To count the effectiveness of each study, subject to data availability, the mean differences with 95% confidence intervals (CIs) were reported (Table 1).
Table 1.
The effect size (95% CI) for the cortisol level for inhabitants in the lower stress neighborhoods compared with the higher stress neighborhoods
| Study | Neighborhood stressors | Low amount | High amount | SE* | ES** | 95% CI*** |
|---|---|---|---|---|---|---|
| Karb et al. | Perceives stress (wakeup) | 0.33 | 0.28 | 0.081633 | 0.27 | (0.11-0.43) |
| Do et al. | Violence (wakeup) | -14.50 | -14.25 | 0.030612 | 0.03 | (-0.03,0.09) |
| Do et al. | Disorder (wakeup) | -8.27 | -10.46 | 0.030612 | -0.02 | (-0.08,0.04) |
| Do et al. | Violence (30 min post-W) | 8.77 | 14.55 | 0.030612 | 0.01 | (-0.05,0.07) |
| Do et al. | Disorder (30 min post-W) | 3.88 | 14.29 | 0.030612 | 0.01 | (-0.05,0.07) |
| Karb et al. | Perceives stress (30 min post-W) | 0.40 | 0.32 | 0.086735 | 0.31 | (0.14-0.48) |
| Karb et al. | Perceives stress (evening) | 0.26 | 0.29 | 0.076531 | -0.11 | (-0.28-0.04) |
| Do et al. | Violence (>120 min post-W) | -0.08 | 0.79 | 0.030612 | 0.01 | (-0.05,0.07) |
| Do et al. | Disorder (>120 min post-W) | 0.02 | 0.71 | 0.030612 | 0.01 | (-0.05,0.07) |
| Do et al. | Violence (30-120 mm post-W) | 9.16 | 8.03 | 0.030612 | 0.01 | (-0.05,0.07) |
| Do et al. | Disorder (30-120 min post-W) | 5.62 | 3.99 | 0.030612 | 0.00 | (-0.06,0.06) |
| Do et al. | Social cohesion (wakeup) | -9.14 | -10.30 | 0.030612 | -0.02 | (-0.08,0.04) |
| Do et al. | Social cohesion (30 min post-W) | 7.21 | 2.76 | 0.030612 | 0.00 | (-0.06,0.06) |
| Karb et al. | Social support (morning) | 0.37 | 0.39 | 0.081633 | -0.07 | (-0.24, 0.09) |
| Do et al. | Social cohesion (>120 min post-W) | 0.98 | 0.59 | 0.030612 | 0.01 | (-0.05,0.07) |
| Karb et al. | Social support (evening) | 0.31 | 0.26 | 0.081633 | 0.20 | (0.03, 0.36) |
| Do et al. | Social cohesion (30-120 min post-W) | 3.59 | 5.22 | 0.030612 | 0.01 | (-0.05,0.07) |
| Karb et al. | Disadvantage (cortisol) | 0.34 | 0.29 | 0.081633 | 0.27 | (0.11-0.43) |
| Karb et al. | Disadvantage (morning) | 0.44 | 0.34 | 0.086735 | 0.39 | (0.22-0.56) |
| Karb et al. | Disadvantage (evening) | 0.26 | 0.30 | 0.081633 | -0.15 | (-0.31-0.01) |
| Do et al. | Poverty (wake up) | 8.65 | -3.04 | 0.030612 | 0.00 | (-0.06,0.06) |
| Do et al. | Poverty (30 min post-W) | -3.71 | 3.57 | 0.02551 | 0.00 | (-0.06,0.06) |
| Do et al. | Poverty (30-120 min post-W) | 2.41 | 7.44 | 0.030612 | 0.01 | (-0.05,0.07) |
| Do et al. | Poverty (>120 min post-W) | 0.03 | 0.49 | 0.030612 | 0.01 | (-0.05,0.07) |
*Standard Error/ ** Effect size = M2-M1/SD/ ***95% Confidence Interval = Effect Size ± (1.96 × Standard Error of the Effect Size)
When data were missing or a study’s bias were evident, attempts were made (where possible) to contact the original investigators for further information. If the data were still not available, the study was excluded.
Results
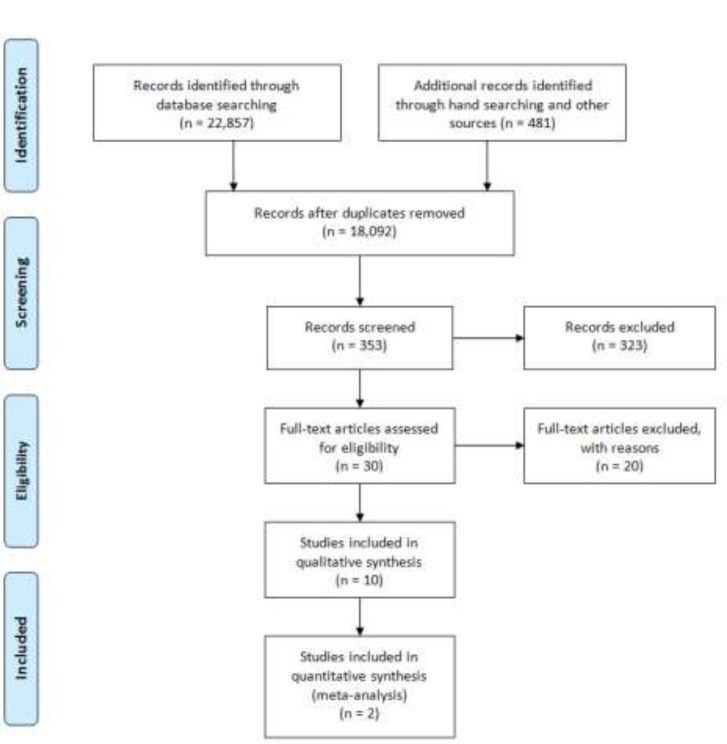
Figure 1 demonstrates the procedure of study selection for the review based on a PRISMA 2009 flow diagram that was lasted updated on July 26, 2013. The database searches yielded 22,706 records, as follows:
Fig. 1.
Study flow diagram
CENTRAL (261)
MEDLINE (5, 711)
EMBASE (3, 652)
PubMed (421)/Google scholar (751)
Trip (12)/ CommunityWISE (18)
Social Care Online (396)
Social Service Abstract (223)
Education Resources Information Center (ERIC) (997)
Journals@Ovid Full Text (1, 310)
APA PsycARTICLES (559)
Web of Science (3, 103)
Scopus (951)
ProQuest Dissertation & Theses Database (203)
Biomed central (266)
PMC (2, 178)
PLOS ONE (971)
High wire press (242)
Hand searching (481)
All citations along with their abstracts were exported to Endnote X7 software (library is available based on request). A two-member review team independently examined 10% of the 18,092 non-duplicate studies and came to agreement on almost all of the studies, and subsequently screened the remainder of the records. Thirty abstract/full-texts were considered as potentially relevant, and each of these articles was assessed separately for exclusion or inclusion by two authors. Differences were determined through discussion, and twenty papers were excluded because they: did not have a quantitative approach, did not consider cortisol as a primary or secondary outcome, and did not consider at least one neighborhood characteristics. Finally, ten studies met all requirements and were eligible to be included in the synthesis (4, 5, 10, 11, 17, 34-38).
Included studies
All ten included studies had observational designs, including six cross-sectional (4, 10, 17, 35, 36, 39) and four cohort studies (5, 34, 37, 38). The included studies recruited between 24 and 814participants. In total, 2,134 participants were recruited in the ten included studies. There were 983 (46.06%) male and 1,151 (53.94%) female samples with completed data. The maximum number of participants was 814 (41.4%) who were >25 years old.
A summary of each report would be found in the characteristics of included studies. In total, twelve neighborhood factors considered in all of studies including: neighborhood disorder (36, 40), neighborhood disadvantage (34), violence (17, 36), fear of violence (34), worry about getting hurt (5), participation (39), perceived stress (34, 36, 41), observed stress (6), social support (34, 39, 40, 42), social cohesion (17, 36), poverty (32, 36), noise (37, 43), substance use (34) and socio economic status (5, 16, 28).
Do et al (36) measured twelve items of neighborhood disorder, including six physical and six social disorder measurements, as adopted from a report (40). They also considered four items of violence based on a model introduced by Sampson (44) and using a four-point scale (1=often to 4=never). However, the authors mentioned census data from the year 2000 as the source of violence data. For fear of violence, 1 to 5 grade questions were used to identify residents afraid of violence in their neighborhood (34). Ina study (5) participants were asked if someone in their neighborhood would physically hurt them. This was also measured using a five-point scale, where higher values corresponded to greater levels of worry. Participation measured by four scales from civic activities, voting, resident organizational participation, and contact with community officials (39). For perceived stress factor, Brenner et al (34) used eleven items out of fourteen for past month measurements based on Cohen and colleagues’ Perceived Stress Scale (PSS)(41). The scale assesses the degree to which people believe their lives to be irregular, unmanageable, and overloading. Do et al. (36) implemented five items from survey, including perceived disorder, perceived violence, neighborhood safety, physical hazards, and the quality of neighborhood services. Observed stress included eight measures from the Social Systematic Observation, census, and uniform crime reports, physical disorder, vacant lots, vacant housing, and the circumstance of streets (6).
Furthermore, Brenner et al (34) used five items focused on emotional support that were adapted from perceived support scales of Procidano and Heller (40) to assess youth support from parents, peers, and other important relationships (42). In this regard, Karb and her colleagues (39) implemented four scales from neighborhood resident surveys measuring social support including social cohesion, social control, intergenerational closure, and reciprocal exchange. Social cohesion measured by Do et al. (36) with four items based on a model introduced by Sampson et al. (44) and a 5-pointLikertscale (1=strongly agreeto5=strongly disagree).
Considering Socioeconomic Stats, Kapuku et al. (5) used codes developed by the National Opinion Research Center. The education level corresponded approximately to an average vocational/training school education (using a scale from 1 = less than high school to 9 = graduate degree). The score was assigned based on twenty occupational classifications, ranging from private household work to professional. In addition, Keliewer (16) implemented eligibility criteria including families in the category of either a low-socioeconomic status neighborhood or a high-socioeconomic status neighborhood. Elliott (28) used 2000 US census data, at the family level, with the SES indicators being education (number of years of education), occupation using Hollings-head’s Four Factor Index of Social Status (42), income before taxes over the past year and family savings. In the other hand, the subjective perception of socioeconomic status was also considered using the MacArthur Scale of Subjective Social Status (45). In this study, adolescents were presented with an image of a ladder and questioned to place their family in comparison with others in society on the ladder, with higher rungs demonstrating higher status.
A well-established measure of family socioeconomic status, by the Hollingshead’s Four Factor Social Status Index, was also measured which is based on parental education and occupation levels (45). In between, socioeconomic status was the most common factor and was considered by nearly half of the studies. A wide variety of outcomes measurements were used in the ten studies, at different time points, and they also differ in the length of time. Nonetheless, some studies either included a cortisol measure (5, 6, 10, 34, 37), or blood pressure measure (17, 38). Cortisol measurements were the primary outcomes of four studies out of ten (6, 34, 36, 37). There were two locations for taking cortisol tests, including home and at the laboratory, with stressors such as video games or cold compressors.
Excluded studies
Twenty studies were formally excluded after two review authors assessed the full texts carefully. The reasons for which the studies excluded were as follows:
Cortisol was not the primary or secondary outcome.
Did not employ a validated measure related to this review.
Neighborhood characteristics were not accounted for as stressors.
They did not present completed data, and author contact is not successful.
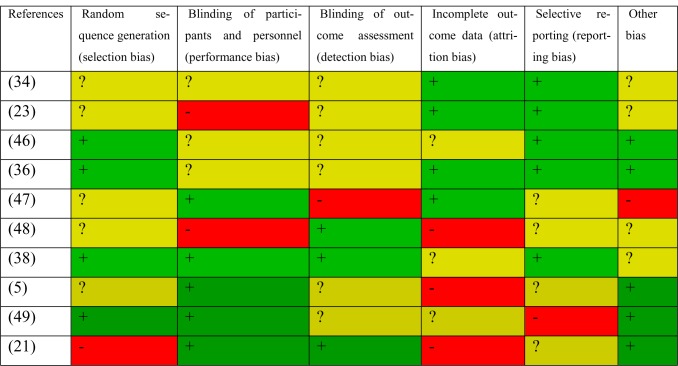
Gray literature was already excluded, even when the source met all criteria above, as they did not have sufficient information for synthesis. All included studies were considered for risk of bias based on the criteria in the Cochrane handbook section 8.5.d. The summary of judgments is shown in Fig.2.
Fig. 2.
Risk of bias in included studies
Effects of studies
The following part provides an explanation of the meta-analysis for the primary outcome of cortisol measurements. However, in the previous section a brief description of the studies that did not present sufficient data for meta-analyses was presented. Only two studies were eligible for the metaanalysis as they had comparable data (36, 39). Neighborhood stressors that were assessed in these two studies included 1) neighborhood perceived stress 2) neighborhood social support, and 3) neighborhood disadvantage. Data were collected from neighborhood resident surveys, systematic social observation, census data, uniform crime reports and structured face-to-face interviews.
Perceived stress included five scales: disorder, violence, safety, physical hazards and neighborhood services. In these studies, social support evaluated by four scales including reciprocal exchange, social control, social cohesion and inter-generational closure. Participation also included four scales including organizational participating, contact with community official, civic activities and voting. Socioeconomic disadvantage included income, education, employment and labor force. However, not all of these scales were considered by all studies, Karb et al. (39) reported on all scales and dimensions of neighborhood measurements. These studies were divided into five subgroups based on neighborhood stressors, but only three stressors were eligible for inclusion in the meta-analysis (perceived stress, social support and disadvantage). The effect size and 95% confidence interval and related forest plot for each group is shown in Table 2. Funnel plot of these effects and their standard error has been presented in Fig. 3 using QI Macros 2014. However, because of the limited number of studies interpretation of the publication bias would not be possible here. As seen in this Table, the overall effect size (95% CI) for the cortisol level for inhabitants in the lower stress neighborhoods compared with the inhabitants from higher stress neighborhoods was 0.12 (0.01, 0.23). This demonstrates that the neighborhood stress has a small effect on cortisol level inclusively. When analyzing the subgroups in the studies investigating neighborhood perceived stress, the effect on cortisol was 0.14 (0.03, 0.25), whereas the effect in studies analyzing social support and disadvantage was 0.10 (0.04, 0.21) and 0.20 (0.03, 0.25) respectively. It seems, among all these factors neighborhood poverty has a remarkable role to increase stress at neighborhood-level.
Table 2.
The effect Size (95% CI) and forest plot for the cortisol level for inhabitants in the lower stress neighborhoods compared with the higher stress neighborhoods
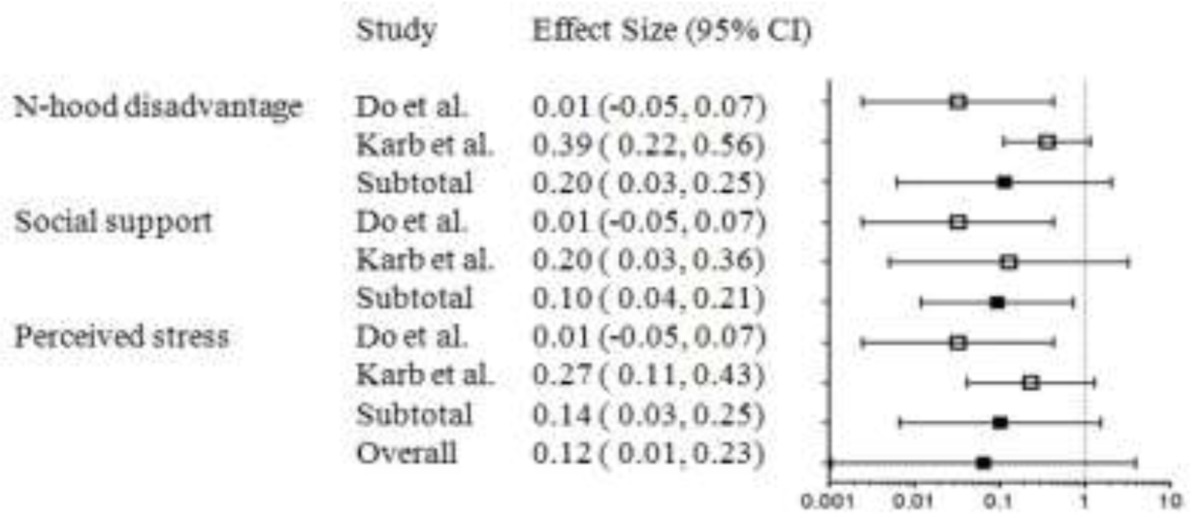
Fig. 3.
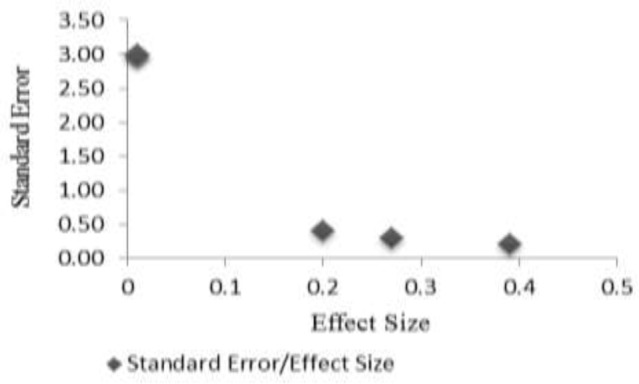
Funnel Plot of Studies
Discussion
This review included ten cross sectional and longitudinal studies, with a total of 2,134 participants. It examined research evaluating the consequences of three neighborhood stressors (perceived stress, social support and neighborhood disadvantage) on circadian cortisol over four different times of day. From these studies, there is no evidence that there is a strong association between neighborhood stress and alteration of cortisol level. However, the meta-analysis found evidence that people living in areas with high disadvantages have higher cortisol upon awakening than people living in lower-disadvantage areas. These findings generally extend the well-documented effect of neighborhood on stress outcomes and took an inclusive approach to the terms neighborhood stress and cortisol. Such an extensive approach may have introduced heterogeneity, but it also led to a large number of references being retrieved from the search, presenting the challenge of assessing and assimilating the evidence for relevant studies (n = 10). Because of the large number of references retrieved from the search for this patient population, gray literature was excluded, such as meeting abstracts. This action could have introduced a degree of publication bias. However, none of these studies had conducted subgroup analysis on cortisol level changes, or the data were not available after personal contact with the authors. This systematic review revealed that geographical areas affect individual stress after taking into account the relative level of disadvantage in the neighborhood. This effect might be a result of differing organizational policy as well as cultural differences existing across regions. However, every physiological interaction and response to different areas can be just as important factors as differences across each neighborhood.
A restriction of this study pertains to the number of searched databases and search terms used. In addition, a qualitative analysis is always subject to probable subjective interpretations, but by having two researchers independently code the individual studies, there was an attempt made to decrease this bias. This assessment of risk of bias indicated that the reviewed studies are of very high overall quality. One particular weakness is that studies in the meta-analysis used different neighborhood measures, which also might have contributed to the heterogeneity.
One of the other issues is that not every person in a given neighborhood will be affected by the same source of stress. Nonetheless, biological factors and genetic ability can be examined, but identifying people at more risk can be an important challenge. This review suggests that currently there is insufficient evidence to support the effect of neighborhood-level stress on circadian cortisol level. This review was also unable to provide any evidence to support any specific type of pathway in relation to neighborhood effects on stress. Samples should be screened to plan those at greatest risk of stress, as currently there is no evidence to suggest the need for worldwide involvement.
The neighborhood in which a person lives is not necessarily the area where he or she conducts most activities. Accordingly, when studying health and behavior in neighborhood, it is worth considering where actually the people spend their time. Another limitation is that census data do not have sufficient reliability for measurements of neighborhood disorder; however, a few studies used social systematic observation and police reports, as well. The unit of time can be a factor because the association between the time that a person spends in the area and amount of stress could have marked effects. In addition, presenting the results through maps results in increasing of compatibility and tracking of other possibilities through which neighborhoods affect stress level.
Conclusion
Additional investigations are encouraged because of the unclear results in these studies and the prevention linked to such factors and the effects of urban areas on health. People engage daily in different activities and contexts, all of which contribute to their health (e.g., a family, a small-scale neighborhood, a municipality, a region and a workplace). Finally, scientists are encouraged to include multiple area levels and present maps (visual presentation) in future investigations. The inclusion of these levels would provide more precise estimates of both individual effects and area-level effects on health.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgment
We would like to thank all team members who assisted in this study. Financial assistance for this study was provided by Fundamental Research Grant Scheme with grant number FP041-2013A from the University of Malaya, Kuala Lumpur. Special thanks to the management of University of Malaya for allowing us to conduct this study. The authors declare that there is no conflict of interests.
References
- Pfeiffer EH, Frankel LK, Dublin LI, Corwin HL (1917). A health census of Chelsea neighborhood: 14th to 42nd streets, 5th Avenue to the Hudson River. Community sickness survey/conducted by the Metropolitan Life Insurance Company and the Chelsea Neighborhood Association, New York City. [Google Scholar]
- Myerson A (1940). Mental Disorders in Urban Areas. An Ecological Study of Schhizophrenia and Other Psychoses. AM J Psychiat, 96(4): 995–997. [Google Scholar]
- Lupien SJ, King S, Meaney MJ, McEwen BS (2000). Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biol Psychiat, 48(10): 976–980. [DOI] [PubMed] [Google Scholar]
- Jacobs J (2010). The Death and Life of Great American Cities, West Sussex, UK: John Wiley & Sons, Ltd. [Google Scholar]
- Kapuku GK, Treiber FA, Davis HC (2002). Relationships among socioeconomic status, stress induced changes in cortisol, and blood pressure in African American males. Ann Behav Med, 24(4): 320–325. [DOI] [PubMed] [Google Scholar]
- Kumari M, Shipley M, Stafford M, Kivimaki M (2011). Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. J Clin Endocr Metab, 96(5): 1478–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogelzangs N, Beekman AT, Milaneschi Y et al. (2010). Urinary cortisol and six-year risk of all-cause and cardiovascular mortality. J Clin Endocr Metab, 95(11): 4959–4964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Steptoe A (2012). Cortisol responses to mental stress and incident hypertension in healthy men and women. J Clin Endocr Metab, 97(1): 29–34. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney M, McEwen B (2001). Can poverty get under your skin? Basal cortisol levels and cognitive function in children from low and high socioeconomic status. Dev Psychopathol, 13(3): 653–676. [DOI] [PubMed] [Google Scholar]
- Weiss L, Ompad D, Galea S, Vlahov D (2007). Defining Neighborhood Boundaries for Urban Health Research. Am J Prev Med, 32(6, Supplement): 154–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch D (2006). Neighborhood characteristics, housing and salivary cortisol secretion in low-income women. Annual Meeting. Retrieved from https://apha.confex.com/apha/134am/techprogram/paper_130086.htm
- Baum A, Grunberg N (1995). Measurement of stress hormones. Measuring Stress: In A Guide for Health and Social Scientists. New York, pp.175–192. [Google Scholar]
- Vyncke V, De Clercq B, Stevens V et al. (2013). Does neighbourhood social capital aid in levelling the social gradient in the health and well-being of children and adolescents? A literature review. BMC Public Health, 13(1): 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo J, Laub J (1978). The fear of crime: Broadening our perspective. Victimology, 3(3–4): 242–253. [Google Scholar]
- Boardman JD, Finch BK, Ellison CG et al. (2001). Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav, 42(2): 151–165. [PubMed] [Google Scholar]
- Kliewer W (2006). Violence exposure and cortisol responses in urban youth. Int J Behav Med, 13(2): 109–120. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW (2004). Seeing disorder: Neighborhood stigma and the social construction of “broken windows”. Soc Psychol Quart, 67(4): 319–342. [Google Scholar]
- Holt JB, Lo C (2008). The geography of mortality in the Atlanta metropolitan area. Comput Environ Urban, 32(2): 149–164. [Google Scholar]
- Coulton C, Korbin J, Su M (1996). Measuring neighborhood context for young children in an urban area. Am J Commun Psychol, 24(1): 5–32. [Google Scholar]
- Schaefer-McDaniel N (2009). Neighborhood stressors, perceived neighborhood quality, and child mental health in New York City. Health Place, 15(1): 148–155. [DOI] [PubMed] [Google Scholar]
- Rudolph KE, Gary SW, Stuart EA et al. (2013). The association between cortisol characteristics and neighborhood disadvantage in a US population-based sample of adolescents. AM J Epidemiol, 177: 32–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen A, Aber MS, Bhana A (2004). Adolescent coping and neighborhood violence: perceptions, exposure, and urban youths’ efforts to deal with danger. AM J Commun Psychol, 33(1–2): 61–75. [DOI] [PubMed] [Google Scholar]
- Chen E, Fisher EB, Bacharier LB, Strunk RC (2003). Socioeconomic status, stress, and immune markers in adolescents with asthma. Psychosom Med, 65(6): 984–992. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C (2010). Neighborhoods and health. Ann Ny Acad Sci, 1186(1): 125–145. [DOI] [PubMed] [Google Scholar]
- Browning CR, Cagney KA, Iveniuk J (2012). Neighborhood stressors and cardiovascular health: Crime and C-reactive protein in Dallas, USA. Soc Sci Med, 75(7): 1271–1279. [DOI] [PubMed] [Google Scholar]
- Dubow EF, Edwards S, Ippolito MF (1997). Life stressors, neighborhood disadvantage, and resources: A focus on inner-city children’s adjustment. J Clin Child Psychol, 26(2): 130–144. [DOI] [PubMed] [Google Scholar]
- Ellen IG, Mijanovich T, Dillman KN (2001). Neighborhood effects on health: exploring the links and assessing the evidence. J Urban Aff, 23(3‐4): 391–408. [Google Scholar]
- Elliott M (2000). The stress process in neighborhood context. Health Place, 6(4): 287–299. [DOI] [PubMed] [Google Scholar]
- Ewart CK, Suchday S (2002). Discovering how urban poverty and violence affect health: development and validation of a Neighborhood Stress Index. Health Psychol, 21(3): 254. [DOI] [PubMed] [Google Scholar]
- Hill TD, Angel RJ (2005). Neighborhood disorder, psychological distress, and heavy drinking. Soc Sci Med, 61(5): 965–975. [DOI] [PubMed] [Google Scholar]
- Johns LE, Aiello AE, Cheng C et al. (2012). Neighborhood social cohesion and posttraumatic stress disorder in a community-based sample: findings from the Detroit Neighborhood Health Study. Soc Psych Psych Epid, 47(12): 1899–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernald LC, Gunnar MR (2009). Poverty-alleviation program participation and salivary cortisol in very low-income children. Soc Sci Med, 68(12): 2180–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington WE. Neighborhood environment, stress, and obesogenic behaviors among adults [PhD Thesis]. University of Washington, 2012. [Google Scholar]
- Brenner AB, Zimmerman MA, Bauermeister JA, Caldwell CH (2013). The physiological expression of living in disadvantaged neighborhoods for youth. J Youth Adolescence, 42(6): 792–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Curry AD (2003). Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav, 44: 34–44. [PubMed] [Google Scholar]
- Do DP, Diez Roux AV, Hajat A et al. (2011). Circadian rhythm of cortisol and neighborhood characteristics in a population-based sample: the Multi-Ethnic Study of Atherosclerosis. Health Place, 17(2): 625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulin-Keita A, Casazza K, Fernandez JR et al. (2012). Do neighbourhoods matter? Neighbourhood disorder and long-term trends in serum cortisol levels. J Epidemiol Commun H, 66(1): 24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackman DA, Betancourt LM, Brodsky NL et al. (2012). Neighborhood disadvantage and adolescent stress reactivity. Front Hum Neurosci, 6: 277–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karb RA, Elliott MR, Dowd JB, Morenoff JD (2012). Neighborhood-level stressors, social support, and diurnal patterns of cortisol: the Chicago Community Adult Health Study. Soc Sci Med, 75(6): 1038–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Procidano M, Heller K (1983). Measures of perceived social support from friends and from family: Three validation studies. Am J Commun Psychol, 11(1): 1–24. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R (1983). A global measure of perceived stress. J Health Soc Behav, 24(4): 385–396. [PubMed] [Google Scholar]
- Hollingshead AB (1975). Four factor index of social status. Yale J Soc, 8: 21–51. [Google Scholar]
- Evans BE, Greaves-Lord K, Euser AS et al. (2013). Determinants of Physiological and Perceived Physiological Stress Reactivity in Children and Adolescents. PLoS ONE, 8(4): e61724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F (1997). Neighborhoods and violent crime: a multilevel study of collective efficacy. Science, 277(5328): 918–924. [DOI] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Kawachi I, et al. (2001). Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics, 108: e3. [DOI] [PubMed] [Google Scholar]
- Chen E, Paterson LQ (2006). Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychol, 25(6): 704–714. [DOI] [PubMed] [Google Scholar]
- Dulin-Keita A, Casazza K, Fernandez JR et al. (2012). Do neighbourhoods matter? Neighbourhood disorder and long-term trends in serum cortisol levels. J Epidemiol Commun H, 66(1): 24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Lercher P, Meis M et al. (2001). Community noise exposure and stress in children. J Acoust Soc Am, 109(3): 1023–1027. [DOI] [PubMed] [Google Scholar]
- Karb RA (2012). Neighborhood-level stressors, social support, and diurnal patterns of cortisol: The Chicago Community Adult Health Study. Soc Sci Med, 75(6): 1038–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]