Abstract
Background
This study aimed to assess factors affecting substandard care and probable medical errors associated with obstetric hemorrhage and HDP at a Northwestern Iranian health care system.
Methods
In a community-based descriptive cross-sectional study, data on all maternal deaths occurred at West Azerbaijan Province, Iran during a period of 10 years from March 21, 2002 to March 20, 2011 was analyzed. The principal cause of death, main contributory factors, nature of care, main responsible staff for sub-standard care and medical error were determined. The data on maternal deaths was obtained from the national Maternal Mortality Surveillance System (MMSS) which were covered all maternal deaths. The “Three delays model” was used to recognize contributing factors of maternal deaths due to obstetric hemorrhage and HDP.
Results
There were 183 maternal deaths, therefore the Mean Maternal Mortality Ratio (MMR) in the province was 32.8 per 100 000 live births (95% CI, 32.64—32.88). The most common causes of maternal deaths were obstetric hemorrhage in 36.6% of cases and HDP in 25.7%. The factors that most contributed to the deaths were all types of medical errors and substandard care with different proportions in management of obstetric hemorrhage and HDP.
Conclusion
A substandard care and medical error was the major contributing factor in both obstetric hemorrhage and HDP leading to maternal mortality, therefore, it is necessary to improve the quality of health care at all levels especially hospitals.
Keywords: Maternal mortality, Substandard care, Medical error, Iran
Introduction
Maternal mortality is an expression of the social, cultural and gender equity disadvantages that women experience and the capacity of a health system to respond maternal health needs. Reduction of the Maternal Mortality Ratio (MMR) by three quarters between 1990 and 2015 is one of the indicators used to evaluate the progress of 5th Millennium Development Goal (1). Latest WHO estimates show that an estimated 287000 tragic loss of mothers occurred worldwide in 2010 (2).
Recent researches on maternal mortality trend analysis confirm that the MMR would be decreasing if governments take a strategic plan to quality safe motherhood care and providing obstetrics emergency care, but there is more work to be done (3). The four major direct causes of maternal mortality are obstetric hemorrhage, Hypertensive Disorders of Pregnancy (HDP), complications of unsafe abortion, and puerperal-related sepsis (4).
Despite marked decreases during the past three decades, maternal deaths remain devastating women’s health in Iran. However, the precise level of maternal mortality is not accurately known. Based on official reports, MMR in Iran is significantly decreasing, i.e. it reduced from 90.6 maternal deaths per 100,000 live births in 1988 to 24.6 in 2005 and to 22.8 in 2008, but with remarkable differences between provinces (5). However, the accuracy of MMR is uncertain, since the reported statistics is based on the country level MMSS which is highly prone to under-registration. The WHO reported that Iran achieved an average annual decline of 5.5% or more in MMR between 1990 and 2008 and reached to estimated level of 30 (from 18 to 50) maternal deaths per 100000 live births so are “on track” (6). Because of lacking well complete registration data in Iran, this estimation has been done based on a model using the three selected covariates: the Gross Domestic Product per capita (GDP), the Total Fertility Rate (TFR), and the proportion of Skilled Attendants at Birth (SAB). At least two of them were improved dramatically during recent two decades, (TFR was decreased from 5.5 in 1988 to around 1.7 in 2012 and SAB increased from 70% to around 97.3% from 1989 to 2007) (7, 8). However in Iran, MMR is lower than in neighboring countries but it is elevated when compared with other national indicators (low TFR, high coverage of prenatal care and high percentage of hospital deliveries).
In recognition of the need to reduce maternal mortality in Iran, national MMSS has been implemented in to the national health system throughout the country since 2001 (9). The MMSS provides ongoing surveillance of all pregnancy-related deaths reported through individual health care settings, hospitals, and individual providers. Maternal deaths continue to be evaluated by a trained medical team to complete the surveillance system questionnaire form to determine any defect in health delivery system and then intervention is planned with the hope that it leads to avoid similar error in the future.
The majority of deaths occur in hospitals as expected, since over 97% of births are hospital deliveries. Postpartum hemorrhage and HDP as the major traditional cause of maternal mortality remain prominent in hospital settings. However, the preventability of these conditions has led to an increasing importance of quality of hospital setting cares. A previous study was investigated epidem-iologic features of maternal death in the West Azerbaijan Province during 2001-2005, which showed most of deaths were preventable and the most important contributing factor was health care provider failure, however; there is no clear image about common medical errors affecting maternal health (10). The MMR in the study setting has been decreased from 88 per 100,000 live births in 1996 to 42.4 in 2008, although it is felt still too many preventable maternal deaths occur (11). It is expected that the majority of maternal deaths occur in this province be related to sub-standard and medical errors, since over 98.2% of births were hospital deliveries and 98.5% of women had at least one prenatal visit in 2010 (12).
The main aims of this study were to determine the maternal mortality ratio for 2002—2011, preventability of maternal deaths, and the substandard cares and possible medical errors contributed to maternal mortality.
Materials and Methods
Design and setting
This was a community-based descriptive cross-sectional study of maternal deaths at West Azerbaijan Province, Iran during 10 years from March 21, 2002 to March 20, 2011. This northwestern province of Iran has higher fertility, lower level of socio-economic development than other provinces and is populated mainly by two large ethnic and religious groups namely Turks (Shiite Muslims) and Kurds (Sunni Muslims). Having more than three million populations, an average of 60,000 births per year and MMR level ranked among the highest in the country. Over 98.2% of births were hospital deliveries and 98.5% of women had at least one prenatal visit (the main provider were gynecologists for about 40% of women) in 2010 (11). Permission to carry out the study was ob tained from the Ethical Committee of the Urmia University of Medical Sciences.
Data collection
The data on maternal deaths was obtained from the national MMSS. This surveillance system provides the most qualitative information regarding inpatient and outpatient on all of the women who died. This involved a visit to the home and all levels of health facilities where of the deceased sought care. Key people were interviewed such as the deceased’s husband and her relatives, health care and hospital staff who participated in the provision of care to the deceased during one week after the death. The principal cause and category of death, main contributing factors, nature of care, main responsible staff for substandard care and medical error (if any) were determined. To ensure quality control of data collection, all data was gathered by an expert maternal mortality survey team. Then each maternal mortality case evaluated by a larger professional committee consisted of at least a maternal & child health specialist, a gynecologist, an anesthesiologist, a midwife and a nurse, thus the likelihood of information bias was reduced. We used all maternal mortality cases obtained from the national NMSS, so sample size estimation was not required. Using community-based data for the entire West Azerbaijan Province helped ensure the reliability of our analysis.
Data were collected using the national MMSS form consisted of the following parts: demographic, socio-cultural, present, past medical and obstetric history, quantity and quality of pre-preg-nancy, pregnancy, delivery and post-delivery cares. Since maternal mortality cases detected from several references such as hospitals, health system, Forensic Medicine Department and Organization for Civil Registration, authors believe that the MMSS was covered all maternal deaths cases. To recognize the different barriers women face in achieving the effective medical care needed to prevent deaths related to obstetric hemorrhage and HDP as the major causes of maternal mortality, the “Three delays model” was used (12): delay 1, delay in decision to request care when experiencing an obstetric emergency; delay 2, delay in reaching an appropriate obstetric facility; and delay 3, delay in receiving adequate treatment. Delay 1, indicated socio- cultural and financial barriers; delay 2, was related to availability of care and geographical variables; and delay 3, referred to the quality of care received once an obstetric care facility was reached. Quality care included some key elements relevant to any level facility, including provider competence, receiving adequate treatment, mechanisms ensuring continuity of care and interpersonal relations.
Medical errors were determined based on the Indiana Medical Error Reporting System definitions (13). In this system, medical error was happened if a maternal death has been associated with labor or delivery or within 42 days post-delivery in a low-risk pregnancy while being cared for in the facility. Excluded were deaths from any of the following: pulmonary or amniotic fluid embolism, acute fatty liver of pregnancy and cardiomyopathy.
After explaining the study and obtaining informed consent, the relatives of deceased women and medical staffs being interviewed.
Statistical analysis
A database was created and analyzed using SPSS software ver. 20 (IBM, Armonk, NY, USA). After the data were reviewed and coded, maternal mortality ratios were calculated. Cases meeting the 9th revision of the International Classification of Diseases (ICD-9) qualified for this investigation. According to the ICD-9 codes 630-676, a maternal death was defined as “The death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.” (5). The MMR was defined as the number of maternal deaths divided by the number of live births in the same category per 100,000. The study employed the “Three delays model” framework to analyze a sample of 114 maternal deaths related to obstetric hemorrhage and HDP. The framework uses three major and several minor delay related indicators to evaluate a range of barriers women face in achieving the effective medical care needed to prevent deaths. All qualitative variables are presented as number and percentage. Denominators indicate the number of patients known as having had the relevant characteristic. All maternal deaths identified were deemed either preventable or non-preventable and presence of any medical error by a professional committee consisting at least ten related specialists based on national standards of care. Preventability of each cases of maternal mortality assigned to one of the four categories by this committee: (a) no chance to prevent, (b) some chance to prevent, (c) good chance to prevent, and (d) strong chance to prevent.
Results
Maternal Mortality Ratio
Based on the provincial vital statistics system, 558600 live births happened in the West Azerbaijan Province from March 21, 2002, through March 20, 2011. In the same period, 183 maternal deaths evaluated by MMSS teams, therefore the mean MMR in the province was 32.8 per 100 000 live births (95% CI, 32.64-32.88) from 2002 until 2011, based on the ICD-9 classification system.
Obstetrical Characteristics
The obstetrical characteristics of 183 maternal deaths are shown in Table 1. More than half of women (55.2%) did not receive regular or any prenatal care. and 33.9% of pregnancies were terminated using cesarean section. About 40% of the maternal deaths were the outcome of unwanted pregnancies and most of the deaths (75.8%) occurred during delivery or after delivery.
Table 1.
Obstetrical characteristics of maternal deaths, West Azerbaijan Province, Iran, 2002-2011 (N=183)
| Characteristic | n (%) |
|---|---|
| Prenatal care | |
| Regular | 82 (44.8) |
| Some | 64 (35.0) |
| None | 37 (20.2) |
| Gravidity | |
| Primiparous | 53 (29.0) |
| Multiparous | 130 (71.0) |
| Pregnancy interval more than two years | 93 |
| Pregnancy interval lower than two years | 37 |
| Mode of delivery | |
| Vaginal | 77 (42.1) |
| Hospital | 41 |
| Home birth (or at the road) | 36 |
| Cesarean | 62 (33.9) |
| Emergent | 44 |
| Elective | 18 |
| Died prior to delivery | 44 (24.0) |
| Pregnancy intentions | |
| Wanted | 112 (61.2) |
| Unwanted pregnancy | 71 (38.8) |
| Time of death relative to delivery | |
| Before | 44 (24.0) |
| Within 24 hours postpartum | 66 (36.1) |
| 2-24 days postpartum | 73 (39.9) |
Causes of Maternal Deaths
Figure 1 presents the flowchart of study design. It shows that most of the maternal deaths were occurred in the medical facilities (77.6%). Causes of maternal deaths are represented in Table 2 according to the place of death. Of the 183 maternal deaths, 67 (36.6%) were due to obstetric hemorrhage, making it the most common cause of maternal mortality.
Fig. 1.
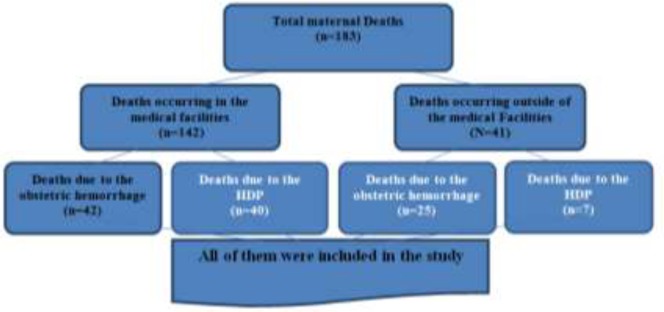
Flowchart of study design
Table 2.
Causes of maternal deaths, West Azerbaijan Provinces, Iran, 2002-2011
| Deaths occurring in medical facilities (n=142) | n (%) |
|---|---|
| Obstetric Hemorrhage | 42 (29.6) |
| Uterine atony | 15 |
| Hemorrhage following cesarean section | 13 |
| Lacerations and uterine rupture | 10 |
| Placental abruption | 3 |
| Ruptured ectopic pregnancy | 1 |
| Hypertensive Disorders of Pregnancy | 40 (28.2) |
| HELLP syndrome | 21 |
| Acute pulmonary edema | 11 |
| Acute fatty liver | 4 |
| Cerebrovascular disease | 3 |
| Eclampsia | 1 |
| Infection | 20 (14.1) |
| Obstetrics | 18 |
| Non obstetrics | 2 |
| Heart Diseases | 9 (6.3) |
| Pulmonary Thromboembolism | 7 (4.9) |
| Intracranial Hemorrhage | 7 (4.9) |
| Anesthesia Related | 5 (3.5) |
| Others and Unknown | 12 (8.4) |
| Deaths occurring outside of medical Facilities (N=41) | |
| Post-partum hemorrhage | 25 |
| Hypertensive Disorders of Pregnancy | 7 |
| Infection | 4 |
| Heart diseases | 2 |
| Pulmonary thromboembolism | 1 |
| Unknown | 2 |
The main cause of obstetric hemorrhage was uterine atony (n=20 [29.8%]). Hypertensive disorders of pregnancy was the second most common cause of maternal mortality, with 47 (25.7%) out of the 183 deaths occurred in the study period. The major complication associated with HDP was hemolysis, elevated liver enzymes, and low platelet count (HELLP syndrome) (n=21 [52.5%]). Other causes of death were infection in 20 women (13.1%), cardiac disease in nine women (6.0%), pulmonary thromboembolism in seven women (4.4%), intracranial hemorrhage in seven women (3.8%), anesthesia complications in five woman (2.7%), and 14 (7.6%) were from other and unknown causes.
Contributing Factors of Deaths and Medical Errors
Tables 3 and 4 illustrate the medical errors and contributing factors of the maternal deaths because of obstetric hemorrhage and HDP according to the types and subtypes of delays, respectively. Only medical errors, substandard cares and those factors the MMSS committee considered to have contributed to the maternal deaths were noted.
Table 3.
Distribution of the contributing factors of maternal deaths associated with obstetric hemorrhage according to the “Three delays model”, West Azerbaijan Province, Iran, 2002-2011
| Contributing factor of obstetric hemorrhage | n (%) |
|---|---|
| DELAY 1: Deciding to request care | |
| No delay 1 | 43/67 (64.2) |
| Delay for cultural reasons (women’s status & autonomy and husband’s permission) | 14/67 (20.9) |
| Inability to recognize the obstetric hemorrhage as a life-threatening complication | 11/67 (16.4) |
| Health care services perceived negative by pregnant women and their families | 4/67 (6.0) |
| DELAY 2: Reaching a medical facility | |
| No delay 2 | 48/67 (71.6) |
| Delay for geographic reasons (distance) | 9/67 (13.4) |
| Delay for transportation reasons (availability and efficiency) | 5/67 (7.5) |
| Delay for economic reasons | 4/67 (6.0) |
| DELAY 3: Receiving adequate treatment | |
| Not reducing risk factors of obstetric hemorrhage | |
| Not correcting anemia antenatal | 11/28 (39.3) |
| Not preventing prolonged labor using the active management of the third stage | 31/47 (66.0) |
| Not actively managing twin deliveries | 4/7 (57.1) |
| Not doing CBC test | 15/54 (27.8) |
| Medical errors in diagnosis of obstetric hemorrhage | |
| Mistake in classifying obstetric hemorrhage | 30/56 (53.6) |
| Delay in suspecting obstetric hemorrhage | 21/56 (37.5) |
| Delay in performing laboratory tests | 18/33 (54.5) |
| Substandard physical examination | 35/56 (62.5) |
| Medical errors in clinical monitoring (Not having sufficient skills available) | |
| Not recognizing the severity of the bleeding | 44/58 (75.9) |
| Not giving sufficient fluids in resuscitation | 23/36 (63.9) |
| Delay in stopping the bleeding | 41/58 (70/7) |
| Not follow-up observations in the woman after initially stopping the bleeding | 17/33 (51.5) |
| Medical errors in treatment | |
| Delay in stopping the bleeding | 24/34 (70.6) |
| Inadequate replacement of blood and blood components | 17/21 (80.9) |
| Substandard treatment of placenta accrete | 12/15 ((80.0) |
| Administrative and health care management problems | |
| Lack of appropriate medication and blood appropriate to the facility’s level of complexity | 21/37 (56.7) |
| Inadequate referral conditions | 31/45 (71.1) |
| Substandard teamwork | 29/41 (70.7) |
| Administrative difficulties that hampered care | 29/37 (78.4) |
Table 4.
Distribution of the contributing factors of maternal deaths associated with HDP according to the “Three delays model”, West Azerbaijan Province, Iran, 2002-2011
| Contributing factor of HDP | n(%) |
|---|---|
| DELAY 1: Deciding to request care | |
| No delay 1 | 32/47 (68.1) |
| Delay for cultural reasons (women’s status & autonomy and husband’s permission) | 7/47 (14.9) |
| Inability to recognize the HDP as a life-threatening complication | 5/47 (10.6) |
| Negative attitude of the woman toward healthcare services | 2/47 (4.3) |
| DELAY 2: Reaching a medical facility | |
| No delay 2 | 30/47 (63.8) |
| Delay for geographic reasons (distance) | 7/47 (14.9) |
| Delay for transportation reasons (availability and efficiency) | 5/47 (10.6) |
| Delay for economic reasons | 4/47 (8.5) |
| DELAY 3: Receiving adequate treatment | |
| Medical errors in diagnosis of HDP | |
| Delay in suspecting HDP | 23/42 (54.8) |
| Delay in performing laboratory tests | 26/39 (66.7) |
| Substandard physical examination | 25/35 (71.4) |
| Medical errors in clinical monitoring | |
| Inadequate monitoring of the HDP’s signs in the postpartum period | 18/38 (47.4) |
| Incomplete laboratory tests | 22/40 (55.0) |
| Postpartum bleeding not quantified | 9/16 (56/2) |
| Failure to recognize and treat pulmonary edema | 8/10 (80.0) |
| Medical errors in treatment | |
| Lack of emergency administration of antihypertensive drugs | 26/42 (61.9) |
| Inadequate administration of prophylactic mag. sulfate to prevent eclampsia | 15/40 (37.5) |
| Inadequate administration of mag. sulfate in a patient with eclampsia | 8/17 (47.1) |
| Inadequate management of intravenous fluids | 24/42 (57.1) |
| Non-admission to an intensive care unit when indicated | 21/35 (60.0) |
| Inadequate administration of prophylactic mag. sulfate to prevent eclampsia in the postpartum | 16/41 (39.0) |
| Medical errors in clinical decisions | |
| Retaining the patient at a health facility which was inappropriate for her condition | 9/24 (37.5) |
| Untimely referral | 18/33 (54.5) |
| Discharge before 48 hours | 6/38 (15.8) |
| Administrative and health care management errors | |
| Inadequate resources at the health facility | 17/42 (40.5) |
| Inadequate referral conditions | 16/33 (48.5) |
| Substandard teamwork | 17/40 (42.5) |
| Administrative difficulties that hampered care | 22/42 (52.4) |
Preventability of Deaths
Eighteen cases (9.8%) met the criteria for being no chance to prevent (unpreventable). Of pre ventable deaths, 54 cases (29.5%) had some chance to prevent, 45 women (24.6%) had good chance and finally, 66 cases (36.1%) had strong chance to prevent death.
Discussion
Maternal mortality rate
For the decade spanning 2002-2012, the average maternal mortality ratio in the study area found 32.8 per 100,000 live births, which is lower than the average MMR of developing regions (13), but greater than that officially reported for Iran as a whole (4). This regional difference in MMR may be attributed to the socio-economic variables and inequalities factors in Iran (14). While data in this study were not population-based, the MMR we are reporting is clearly under the real magnitude, so this is a limitation for this study.
A probable explanation for this could be related to the target population and definitional challenges. Data in this study were based on the cases of maternal deaths reported from hospitals and health care facilities using national active surveillance system. This method is known to miss a significant proportion of actual cases because events in early pregnancy related to for example, ectopic pregnancy or unsafe induced abortion are particularly prone to underreporting by relatives and providers. The absence of accurate mortality data as in other developing countries is of concern in Iran, however, our study design mainly aimed to identify the factors related to substandard care and possible errors contributing to the maternal mortality.
This study uncovers some common problems encountered in the quantity and quality of maternal care in a sample of developing country setting. Substandard care (all degrees) was common. We observed more than half of women did not receive regular or any prenatal care and about 40% of unwanted pregnancies among maternal deaths as causes of substandard care in pre-pregnancy and pregnancy care, a situation also noted by others (15).
Contributing factors of death related to the obstetric hemorrhage
As births moved to hospitals in Iran, it was expected the common causes of maternal deaths change from hemorrhage and sepsis to a greater incidence of indirect causes or embolism. We found hemorrhage remains the most common cause of maternal mortality (61.0% of deaths occurring outside of the medical facilities and 29.6% of cases in the medical facilities). About 64% and 71% of the patients who died from obstetric hemorrhage reached to the hospitals without type one and type two delays respectively, but they did not receive the standard care. Based on other researches, obstetric hemorrhage, which formerly was an important cause of maternal mortality, is less common today in developed countries (16), but remains as the leading cause of death in low-income countries (4). In addition, most of the hemorrhage related mortality occur at home or at lower levels of health care facilities (17, 18), and the active management of the third stage of the labor would be associated with a significant reduction in the occurrence of post-partum hemorrhage (19). In the present study, all types of medical errors and substandard care with different proportions in management of obstetric hemorrhage were detected. Not having sufficient skills available and errors in active management of the third stage of labor were the most common avoidable factors related to deaths contributed by obstetric hemorrhage. However, maternal mortality caused by hemorrhage at hospital has more incidents of medical errors and substandard care than other reasons of women’s death. A systematic review showed that all maternal deaths related to hemorrhage potentially could be prevented by care improvement (20). These findings emphasize that all in-hospital women’s death with obstetric hemorrhage, even in low risk pregnancies could be related to medical errors in our study setting. Since obstetric hemorrhage is the leading cause of maternal mortality in our research area and in Iran, we are confident that avoidance of the errors outlined in Table 3, will allow us to reduce the maternal mortality rate in the coming years.
Contributing factors of death related to the HDP
The findings of this analysis reveal that HDP were responsible for 40 out of 142 (28.2%) in-hospital mortality and 17.1% of deaths outside of hospitals, making it the second most common cause of maternal mortality. Overall, HDP is responsible for 10%-15% of direct maternal mortality in developing countries and is the leading cause of deaths in Latin America and the Caribbean, with the incidence estimated as 25.7% of deaths (4). Although HDP include conditions that are categorically unavoidable and unpreventable, such as preeclampsia and eclampsia (21), high quality care may prevent individual deaths in most of the patients (22). Common avoidable medical errors and substandard cares leading to maternal deaths related to HDP are outlined in Table 4. Medical error is detected to consist of diagnostic errors or delays, failure to monitor clinically and appreciate the severity of the condition and failure to refer patients to high-level disciplines. The most common medical errors in HDP management involved failure to recognize and treat pulmonary edema, substandard physical examination, and lack of emergency administration of antihyperten sive drugs. In the literature the suggestion is made that HDP cases of maternal deaths are associated with some degree of substandard care, even in the developed countries settings (23, 24).
The data of Tables 3 and 4, show that multiple factors influenced obstetric care utilization by the Iranian women. In most of the cases, death could not be attributed to a single delay. A significant number of women were not instructed to seek the care of a physician when obstetric emergency presented, a situation also noted by others (15, 25). The most common type one and two delays were attributed to cultural reasons, inability to recognize the severity of the symptoms, geographical and transport problems. In some of the cases, the relatives made no effort to transport the patients because their husbands were absent to allow or home delivery under supervision of a local uneducated midwife was a routine procedure in some regions.
Strength and limitations
The present study has at least two strengths. First, findings of this study highlighted substandard care and medical error as a less recognized critical component of maternal mortality. Few studies have examined the link between medical errors and substandard cares in health system to maternal mortality. The second strength of this study is that it used the “Three delay model” to analyze the medical care factors that directly contribute to maternal mortality from HDP which introduced by Zuleta-Tobon et al. (15). We modified this model to identify health care factors related to deaths from obstetric hemorrhage.
While the findings of this study are encouraging, there are a number of limitations to consider. First, the most important limitation was our cross-sectional design, because we could not identify maternal mortality risk factors based on our findings. A second limitation is that this study was conducted in a province having only four percent of the total country population; therefore, it seems that our results cannot be generalized to the overall country. On the other hand, following facts regarding health system governance in Iran shows a stereotypy in country level health system: the Ministry of Health and Medical Education (MOHME) is the primary body responsible for oversight of the health system; and most of the other supervisory, regulatory and planning functions are conducted by MOHME itself or by the Universities of Medical Sciences on its behalf in the provinces. Therefore, authors believe that our findings may be applicable to the general health system of Iran. Another limitation is that the study does not rely on a baseline number of obstetric hemorrhage and HDP cases in the West-Azerbaijan Province to calculate the incidence and lethality of these conditions.
Recommendations
Obstetric hemorrhage and HDP remains a major contributor to maternal morbidity in Iran. It is clear that doing further research in other settings will contribute to the understanding of the possible causes and the best treatment modalities.
This study identifies several practical points that are critical for health policy makers who aim to decrease MMR. Efforts to prevent substandard care and medical errors should focus on standardizing the maternal care in all levels of the health care system, especially the hospital systems that should have comprehensive programs directed at the prevention of maternal mortality. Reduction of variability in the provision of care using standard protocols and elimination of errors in the management of obstetric hemorrhage and HDP will contribute significantly to a reduction in maternal mortality.
Conclusion
In conclusion, because substandard care and medical errors are the major contributing factor in both obstetric hemorrhage and HDP leading to maternal mortality, it is necessary to improve the quality of care at all levels especially in hospitals to respond obstetric emergencies in the study area and may be in other similar developing countries.
Ethical consideration
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication, double publication and/or submission, etc.) have been checked by the authors and Urmia University of Medical Sciences (UMSU).
Acknowledgement
We would like to acknowledge Urmia University of Medical Sciences (UMSU), all interviewers, interviewees and the professional committee members for their sincere collaboration in development of this research.
The authors declare that this study was not supported by any specific financial source and they have no competing interests.
References
- Ronsmans C, Graham WJ (2006). Maternal mortality: who, when, where, and why. Lancet, 368: 1189–1200. [DOI] [PubMed] [Google Scholar]
- World Health Organization, UNICEF, UNFPA, Bank tW (2010). Trends in maternal mortality: 1990–2008. Estimates developed by WHO, UNICEF, UNFPA, and the World Bank. ed. WHO Geneva. [Google Scholar]
- UNFPA, UNICEF, WHO, World Bank (2012). Trends in Maternal Mortality: 1990–2010. ed. World Health Organization, Geneva. [Google Scholar]
- Khan KS, Wojdyla D, Say L, Gulmezoglu A M, Van Look PF (2006). WHO analysis of causes of maternal death: a systematic review. Lancet, 367: 1066–1074. [DOI] [PubMed] [Google Scholar]
- Heidari GhR, RN H (2009). Iran Millennium Development Goal’s in a Glance. Iran J Public Health, 38: 63–64. [Google Scholar]
- Abbasi Shavazi MJ, McDonald P, HosseiniChavoshi M (2008). Modernization and the cultural practice of consanguineous marriage: Case study in four province of Iran. J Biosoc Sci: 1–23. [DOI] [PubMed] [Google Scholar]
- Zemikhah A, Amirkhani MA, Jalilvand P, EmamiAfshar N, Radpooyan LNC (2009). A National Maternal Mortality Surveillance System in Iran. Iran J Public Health, 38: 90–92. [Google Scholar]
- Vakilian K, Mirzaii K (2011). Reproductive health in iran: international conference on population and development goals. Oman Med J, 26: 143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrokh-Eslamlou H, Nanbakhsh F, Heshmati F (2006). Epidemiology of Maternal Mortality in the West Azerbaijan Province (2001–2005). Urmia Medical Journal 17: 23–31(in Persian) [Google Scholar]
- Ministry of Health and Medical Education (2006). Islamic Republic of Iran, National Maternal Mortality Surveillance System. ed. Ministry of Health, Tehran. [Google Scholar]
- Rashidian A (2010). Health Observatory: First Report I.R. Iran Multiple-Indicator Demographic and Health Survey, 2010 ed. Ministry of Health and Medical Education. [Google Scholar]
- Maine D, Akalin MZ, Ward VM, Kamara A. (1997). The Design and Evaluation of MaternalMortality Programs. ed. Center for Population and Family Health School of Public Health Columbia University, Center for Population and Family Health School of Public Health Columbia University. [Google Scholar]
- Mbizvo MT, Say L (2012). Global progress and potentially effective policy responses to reduce maternal mortality. Int J Gynaecol Obstet, 119 Suppl 1:S9–12. [DOI] [PubMed] [Google Scholar]
- Tajik P, Nedjat S, Afshar NE, Changizi N, Yazdizadeh B, Azemikhah A, Aamrolalaei S, Majdzadeh R (2012). Inequality in maternal mortality in iran: an ecologic study. Int J Prev Med, 3: 116–121. [PMC free article] [PubMed] [Google Scholar]
- Zuleta-Tobon JJ, Pandales-Perez H, Sanchez S, Velez-Alvarez GA, Velasquez-Penagos JA (2013). Errors in the treatment of hypertensive disorders of pregnancy and their impact on maternal mortality. Int J Gynaecol Obstet, 121: 78–81. [DOI] [PubMed] [Google Scholar]
- Clark SL (2009). Reducing Maternal Mortality in the 21st Century. The Female Patient, 34: 40–42. [Google Scholar]
- Fawcus S, Mbombo N F, Hofmeyr J Obstetric haemorrhage. In: Pattinson RC (ed.) Saving mothers 2005–2007: Fourth report on Confidential enquiries into maternal deaths in South Africa, Goverment Prinyter Pretoria, in press. [Google Scholar]
- Prendiville WJ, Elbourne D, McDonaldSJ (2009). WITHDRAWN: Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev:CD000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begley CM, Gyte GM, Devane D, McGuire W, Weeks A (2011). Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev:CD007412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark SL, Belfort MA, Dildy GA, Herbst MA, Meyers JA, Hankins GD (2008). Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery. Am J Obstet Gynecol, 199: 36 e1–5; discussion 91,–92 e 7–11. [DOI] [PubMed] [Google Scholar]
- Duley L (2009). The global impact of pre-eclampsia and eclampsia. Semin Perinatol, 33: 130–137. [DOI] [PubMed] [Google Scholar]
- Ronsmans C, Campbell O (2011). Quantifying the fall in mortality associated with interventions related to hypertensive diseases of pregnancy. BMC Public Health, 11 Suppl 3:S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagaarachchi PT, Fernando L (2002). Trends in maternal mortality and assessment of substandard care in a tertiary care hospital. Eur J Obstet Gynecol Reprod Biol, 101: 36–40. [DOI] [PubMed] [Google Scholar]
- Goldenberg RL, McClure EM, Macguire ER, Kamath BD, Jobe AH (2011). Lessons for low-income regions following the reduction in hypertension-related maternal mortality in high-income countries. Int J Gynaecol Obstet, 113: 91–95. [DOI] [PubMed] [Google Scholar]
- Tsu VD, Shane B (2004). New and underutilized technologies to reduce maternal mortality: call to action from a Bellagio workshop. Int J Gynaecol Obstet, 85 Suppl 1:S83–93. [DOI] [PubMed] [Google Scholar]


