Abstract
Background
Social determinants, similar to equity, have been considered by policymakers in many countries. However, there is not a correct and complete understanding of them. This study aimed to analyze the systematic relationships among social determinants of health (SDH) and identify their prioritization in Iran.
Methods
This cross-sectional descriptive-analytical study was conducted in 2012. The target population consisted of 30 experts on SDH. Required data was collected using a questionnaire, as well as, nominal group technique (NGT). Then collected data were analyzed using MATLAB 7.9.0 and SPSS 18.0.
Results
Determinants of early life (EL), social gradient (SG), unemployment (U), stress (S) and addiction (A) were certainly affecting determinants on the system, which were placed in the cause group and ranked as the first to fifth priorities, respectively. While social exclusion (SE), food (F), social support (SS), work (W) and transport (T) were partially affected determinants and were placed in the effect group and ranked as the sixth to tenth priorities, respectively. Early life and transport were identified as the most affecting and affected determinants with the coordinates (2.16 and 0.75) and (1.68 and -0.47) on the SDH diagram, respectively.
Conclusion
Improving the social and economic status, considering the early life, increasing the quality of education, and reducing unemployment and stress have effects on the other social determinants of health and provide opportunities for increasing equity.
Keywords: Social determinants of health (SDH), DEMATEL, Iran
Introduction
Health, as a fundamental human right, is considered as one of the development factors in every society because every society development is basically measured by its quality of public health, fair distribution of health services among different social classes, as well as, the level of support of disadvantaged people against factors which are harmful to health (1–3). Although the health indicators have been improved in most countries, there are still major inequities among and within countries. Therefore, to increase fairness, there is a need for measures that go beyond the immediate causes of diseases and it is required to give special attention to the social determinants because these factors not only improve people’s health for participation in the community but also may lead to increased labor productivity and economic growth. Health and social determinants refer to “the economic, social and political structures and resources” which impact on the health outputs (4–7). Economic and social status has important effects on health. In other words, there is a social gradient in health which moves from top to down the socio-economic spectrum and each upper class has the better health status than the lower one. In most parts of the world, the poor and disadvantaged have more morbidity ratio than others; it means that the more disadvantaged groups both suffer from diseases more than others and suffer more from chronic diseases as well as disabilities at their lower ages. Differences between their psychological indicators, cardiov-ascular disease rates, and the level of accessibility and the quality of health care services received are grate and need more attention (8–10). The important reason for the differences between their health status, which are considered to be unfair, are largely outside the direct control of individuals; in that the poor due to lack of or limited resources have less choices, live in crowded and unsafe places, have less jobs and more risk of unemployment (9, 11, 12).
The increasing tendency to wellbeing and consumerism and its outcomes resulted in significant changes in the majority of life processes (13), people were given many tools, and gradually reduced mobility and changed physical activity to mental concerns (14). Following these changes, the health problems, which have been one of the biggest human concerns, have been worse in terms of personal, cultural, social, political, economic and national aspects by establishing development boundaries (15, 16) and transformed into one of the necessities of today’s societies which had a high priority and should be given more attention (13, 17).
Social determinants of health are classified in three categories: 1) The personal health behaviors within the family environment; 2) the social organizations and methods to deal with group health which are outside of the family environment; and 3) the social structure for planning and providing health services. These determinants have more effects on public health than the health system performance, and inequality in them can cause equity problems in health. Therefore, understanding the importance of these determinants by the policymakers has an important role in increasing the equity. Considering the importance of social determinants of health in reducing the inequalities and promoting health, the World Health Organization (WHO) established the Commission on Social Determinants of Health (CSDH) in 2005 and has taken the basic steps to reduce health inequalities (18). Also, these determinants have attracted special attention of policymakers (14, 19); because their management can be considered as a key tool for controlling the emerging diseases (20).
Social determinants, similar to equity, have been considered by policymakers in many countries. However, there is not a correct and complete understanding of them. Therefore, some researchers seek to provide conceptual models for understanding these factors (21). People who have less social protection, do not have proper health status, too (22). Also, some researchers have considered the improvement of living conditions as the basic principle of individual and population health (23, 24).
Riley and colleagues in a research studied the heart health promoting activities from an environmental perspective and concluded that the patterns of integrating social, environmental and organizational theories helped implement such programs (25). Rasanathan and colleagues studied the social determinants and their role in reducing inequities in the community access to health services (20). Viner and colleagues in their study considered the social determinants of health as the major problems of the youths in comparison with others (26), Wallace, also, in a similar study concluded that health problems in different age groups were due to ignoring these determinants (27), and Wallerstein and colleagues in their research studied the influence of social determinants of health on inequity in providing health care and diseases control (16).
In Iran, also, the improvement of health indicators such as reducing mortality and increasing life expectancy can clearly be seen and more efforts have been focused on increasing the equity in health (28). However, few studies have been conducted on the social determinants of health. Hos-seinpour and colleagues studied the outpatients’ utilization level of health services by reviewing some social factors including poverty and insurance status (29). The results of studies conducted in Iran show the effects of social determinants on health (30).
The WHO Commission on Social Determinants of Health has put a great emphasis on research in the field of SDH in the World Health Report 2010 (31). The researches conducted in this regard, have more taken researchers’ interests into consideration and are one-dimensional studies, and also have more reviewed the role of social determinants on health. Therefore, providing a conceptual model of social determinants of health will contribute greatly in understanding the relationships among the social determinants.
This study aimed to analyze the systematic relationships among social determinants of health and identify their cause and effect relationships and prioritization in Iran using one of the mathematical and operations research techniques.
Methods
This cross-sectional descriptive-analytical study was conducted in 2012 to analyze the systematic relationship among social determinants of health (SDH) in Iran using one of the mathematical and operations research techniques, DEMATEL. The target population consisted of 30 experts on social determinants of health (SDH). Required data was collected using a questionnaire, as well as, nominal group technique. Firstly, based on literature review, a model proposed by the WHO Commission on Social Determinants of Health members included 10 determinants such as early life, social gradient, unemployment, stress, addiction, social exclusion, food, social support, work, and transport was selected as the basic model (32). According to this model, a questionnaire was designed. This questionnaire along with a schematic diagram of the proposed model and its description were given to the experts to provide their advice about the proposed model. This questionnaire was a Likert scale questionnaire, in that each questions had a 5-choice answer, included completely disagreed, disagreed, no comment, agreed, and completely agreed. Finally, collected data was analyzed by t-test using SPSS 18.0.
Having approved the model, the experts were asked to specify the relationships among the determinants using nominal group technique (NGT) which means they should write their viewpoints on a paper without any consultation with each other. Then, the scores of every relationship were written on the white board. In order to clarify the inconsistencies, the scores which had large deviations from each other were reviewed and a final vote was taken. To determine the relationships among the determinants, scores of 0, 1, 2, 3 and 4 were given to the “very high impact, high impact, low impact, very low impact and no impact” responses, respectively. The final scores were analyzed using MATLAB 7.9.0.
The process of using DEMATEL technique
Identifying the social determinants influencing health
Determining the relationships among these determinants using a paired comparisons matrix by the experts
Forming the matrix of the intensity of relationships (M matrix)
Forming the matrix of the relative intensity of the direct relationships (M = α * M, The maximum sums of matrix rows = Μα)
Forming the matrix of the available relative intensity of direct and indirect relationships (matrix M(1-M)-1)
Identifying the determinants hierarchy (with diagram)
Results
All of the experts were agreed with the recommended determinants by the WHO Commission SDH members, including social gradient, stress, early life, social exclusion, work, unemployment, social support, addiction, food and transport (P=0.001) (Table 1).
Table 1:
The results of the experts ‘ viewpoints on the Social Determinants of Health
| Components | Experts’ Responses | ||||||
|---|---|---|---|---|---|---|---|
| Completely agreed | agreed | No Comment | Disagreed | Completely Disagreed | Mean | SD | |
| Social gradient | 20 | 10 | 0 | 0 | 0 | 4.67 | 0.46 |
| Stress | 21 | 8 | 1 | 0 | 0 | 4.63 | 0.66 |
| Early Life | 10 | 18 | 2 | 0 | 0 | 4.27 | 0.58 |
| Social Exclusion | 22 | 8 | 0 | 0 | 0 | 4.73 | 0.45 |
| Work | 13 | 17 | 0 | 0 | 0 | 4.43 | 0.50 |
| Unemployment | 23 | 7 | 0 | 0 | 0 | 4.77 | 0.43 |
| Social Support | 7 | 21 | 2 | 0 | 0 | 4.17 | 0.53 |
| Addiction | 25 | 5 | 0 | 0 | 0 | 4.83 | 0.37 |
| Food | 18 | 12 | 0 | 0 | 0 | 4.60 | 0.49 |
| Transport | 10 | 20 | 0 | 0 | 0 | 4.33 | 0.47 |
Besides, the present study findings showed that early life (EL), social gradient (SG), unemployment (U), stress (S) and addiction (A) were certainly affecting determinants on the system, which were placed in the cause group and ranked as the first to fifth priorities. While social exclusion (SE), food (F), social support (SS), work (W) and transport (T) were partially affected, which were placed in the effect group and ranked as sixth to tenth priorities (Table 2 and Fig. 1).
Table 2:
The hierarchy of affecting and affected Social Determinants of Health
| Determinants | R | J | R+J | R-J |
|---|---|---|---|---|
| Social gradient | 1.63 | 1.26 | 2.89 | 0.36 |
| Stress | 1.37 | 1.31 | 2.69 | 0.05 |
| Early Life | 1.45 | 0.70 | 2.16 | 0.75 |
| Social Exclusion | 1.40 | 1.47 | 2.88 | -0.06 |
| Work | 0.92 | 1.35 | 2.27 | -0.42 |
| Unemployment | 1.29 | 1.14 | 2.43 | 0.15 |
| Social Support | 1.23 | 1.46 | 3.12 | -0.23 |
| Addiction | 1.66 | 1.65 | 3.31 | 0.00 |
| Food | 0.97 | 1.11 | 2.09 | -0.13 |
| Transport | 0.60 | 1.08 | 1.68 | -0.47 |
Fig. 1:
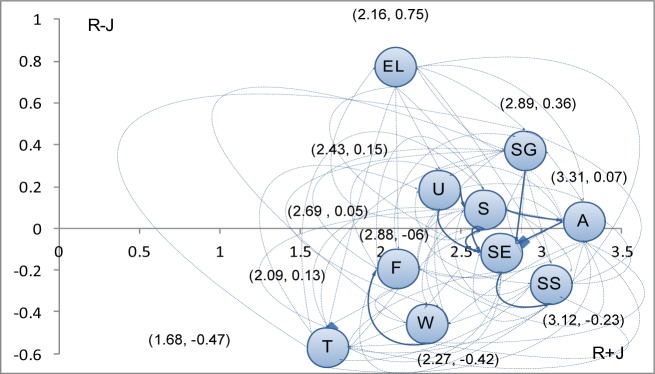
The prioritization of the Social Determinants of Health/(El: Early Life, SG: Social gradient, U: Unemployment, S: Stress, A: Addiction, SE: Social Exclusion, F: Food, SS: Social Support, W: Work, T: Transport)
Early life and transport were identified as the most affecting and affected determinants with the coordinates (2.16 and 0.75) and (1.68 and -0.47) on the SDH diagram, respectively.
Discussion
This study aimed to analyze the systematic relationships among social determinants of health and identify their cause and effect relationships and prioritization in Iran. Given the role of the environment and social structure in health promotion, the social determinants have been considered. On the other hand, the reasons of many premature deaths are social determinants such as the social gradient, unemployment, poor working and living conditions and social exclusion (33). “Social justice is defined as providing opportunities for health through economic, social and political structures and social values”. Also, equity in health refers to “the absence of systematic disparities in health or in major social determinants”. Therefore, the social-economic inequalities are the important factors affecting health, and the health problems in social disadvantaged classes can only be solved by policy makers through taking these inequalities into consideration (34).
International Centre for Health and Society has introduced some determinants such as stress, early life, nutrition, transport, addiction, employment, work, social support and social exclusion as the most important social determinants of health (35). In the present study, also, these factors have been confirmed by the experts as the important social determinants affecting health. The results of this study showed that most of social determinants of health have an impact on each other so that “early life” was identified as the most affecting determinant and has been affected the least by others. On the other hand, “transport” took the greatest effect from other determinants and was placed in the effect group. Therefore, in structuring the social determinants of health, considering the cause and effect relationships can help to make the right decisions.
The results of the current study also showed that poor early life could affect some determinants such as addiction, social exclusion, unemployment, etc. According to the results of a study, violence in childhood has the significant relationships with adulthood health, depression, and smoking, which means it has a major role in health in adulthood and should be considered and, generally, investments in early life has the greatest impact on increasing equity in health over many years and generations (36). This result confirms the current study results
“Social gradient”, as one of the social determinants of health, has been located after “early life”. Poverty is one of the most important social problems of countries. Dealing with this component as an indicator of the social gradient, can improve people’s health. In most countries, poverty has increased the exposure to infectious diseases, malnutrition, micronutrient deficiency, and maternal and child mortality (37).
Education is the other indicator of social gradient and a predictor of better health. Also, factors such as the household per capita expenditure and non-food costs, education level, social-economic subgroups and family size are significantly associated with some health indicators. There has been a direct correlation between family income and mammography screening (38). According to the present study results, the social gradient was a high priority, considering the role of its indicators, as well as, its effects on the other social determinants (39, 40).
There is evidence indicating that diseases may be both the causes and the consequences of unemployment. Unemployment may be due to the social gradient and affect the person’s life. Results of this study showed that “unemployment” has been located after “early life” and “social gradient” and strongly affect health. Unemployment has effects on the other determinants of the model (41).
Pawar and colleagues after controlling economic, social and demographic factors concluded that stress, social exclusion and lack of social support had significant relationships with morbidity (35). Also, people who had no access to social support were suffering from lower health outcomes (22). In the present study, “stress” was one of the social determinants of health which was affected by social gradient, unemployment, addiction, as well as, the effect group determinants.
From researchers’ perspective, some determinants such as food and transport are lifestyle components, and several tools and methods should be used to change the behavior in these determinants. This change in behavior can be both directly by individuals themselves and indirectly by government public and social policies. The results of some studies show that lifestyle change from driving to walking and cycling has a positive impact on health. Also, good nutrition has effect on increasing the life expectancy (42–44). In the current study, two mentioned determinants, food and transport, were placed in the effect group and affected by the other determinants of the model. These determinants are directly affected by the cause group determinants and their indicators such as preventive services programs and comprehensive health education programs. It is quite clear that determinants such as unemployment, stress, social support and social exclusion have effects on the desirable health behaviors including food and transport (45, 46).
Proper working conditions, such as control over work, public participation of employees, health and safety regulations and work shifts have great effects on improving health. In this study, “work” and its conditions, as one of the social determinants of health, was placed in the effect group and affected by other determinants. Generally, the effect of work and its conditions on health has strongly been confirmed (47–50).
The results of this study showed that health is a multi-sectoral issue and the growth of its indicators not only is affected by the performance of Department of Health and Medical Education but also requires the cooperation, coordination and interaction of all the social and economic organizations. Legal and political organizations involved in the policymaking process have a great role in improving health which perform this role through equitable distribution of services and making appropriate policies. Government attitude to the health issues is a key component to the success of any movement towards the social determinants. The government tools are to avoid any centralization in resource allocation and to implement financial and systematic reforms. Improving the social and economic status, considering the early life, increasing the quality of education, and reducing unemployment and stress have effects on the other social determinants of health and provide opportunities for increasing equity.
Conclusion
Improving the social and economic status, considering the early life, increasing the quality of education, and reducing unemployment and stress have effects on the other social determinants of health and provide opportunities for increasing equity.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
We thank faculty members of Medical Sciences Universities of Tehran, Baqiyatallah, Shahid Beheshti for their kind cooperation. The authors declare that there is no conflict of interests.
References
- Marmot MG, Wilkinson RG (2005). Social determinants of health. Second ed. Oxford University Press, USA. [Google Scholar]
- Raphael D (2004). Social determinants of health: Canadian perspectives. Second ed. Canadian Scholars Pr. [Google Scholar]
- Williams A, Cookson R (2000). Equity in health. In: Handbook of health economics. Eds, Culyer, A. J. and Newhouse, J. P. Elsevier, Amsterdam, 1: 1863–1910. [Google Scholar]
- Irwin A, Valentine N, Brown C, Loewenson R, Solar O, Brown H, et al. (2006). The Commission on Social Determinants of Health: Tackling the social roots of health inequities. PLoS Med, 3(6):e106, 749–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic D (2000). Essay: Rediscovering the social determinants of health. Health Aff, 19(3): 269–276. [Google Scholar]
- Starfield B (2002). Equity in health. J Epidemiol Community Health, 56(7): 483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett E, Casper M (2001). A definition of “social environment”. Am J Public Health, 91: 465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney G (1993). Equity in the finance and delivery of health care, an international perspective. J Epidemiol Community Health, 47(4): 338–339. [Google Scholar]
- Whitehead M, Dahlgren G, Evans T (2001). Equity and health sector reforms: can low-income countries escape the medical poverty trap? Lancet, 358(9284): 833–836. [DOI] [PubMed] [Google Scholar]
- Braveman P, Gruskin S (2003). Poverty, equity, human rights and health. Bull World Health Organ, 81(7): 539–545. [PMC free article] [PubMed] [Google Scholar]
- Braveman P, Starfield B, Geiger HJ, Murray CJL (2001). World Health Report 2000: how it removes equity from the agenda for public health monitoring and policyCommentary: comprehensive approaches are needed for full understanding. BMJ, 323(7314): 678–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poland B, Coburn D, Robertson A (1998). Wealth, equity and health care: a critique of a “population health” perspective on the determinants of health. Soc Sci Med, 46(7): 785–798. [DOI] [PubMed] [Google Scholar]
- Marmot M (2005). Social determinants of health inequalities. The Lancet, 365(9464): 1099–1104. [DOI] [PubMed] [Google Scholar]
- Riva M, Bambra C, Curtis S, Gauvin L (2011). Collective resources or local social inequalities? Examining the social determinants of mental health in rural areas. Eur J Public Health, 21(2): 197–203. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Egerter SA, Woolf SH, Marks JS (2011). When do we know enough to recommend action on the social determinants of health? Am J Prev Med, 40(1): 58–66. [DOI] [PubMed] [Google Scholar]
- Wallerstein NB, Yen IH, Syme SL (2011). Integration of social epidemiology and community-engaged interventions to improve health equity. Am J Public Health, 101(5): 822–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M (2011). Global action on social determinants of health. Bull World Health Organ, 89(10): 702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymus (2012). Interim Statement of the Commission on Social Determinants of Health 2007. WHO. [cited 2012. July, 1]; Available from: http://www.who.int/social_determinants/publications/commission.
- Rasanathan K, Montesinos EV, Matheson D, Etienne C, Evans T (2011). Primary health care and the social determinants of health: essential and complementary approaches for reducing inequities in health. J Epidemiol Community Health, 65(8): 656–660. [DOI] [PubMed] [Google Scholar]
- Rasanathan K, Sivasankara Kurup A, Jaramillo E, Lonnroth K (2011). The social determinants of health: key to global tuberculosis control. Int J Tuberc Lung Dis, 15 Suppl 2: S30–S6. [DOI] [PubMed] [Google Scholar]
- Exworthy M (2008). Policy to tackle the social determinants of health: using conceptual models to understand the policy process. Health Policy Plan, 23(5): 318–327. [DOI] [PubMed] [Google Scholar]
- Richmond CAM (2009). The social determinants of Inuit health: A focus on social support in the Canadian Arctic. Int J Circumpolar Health, 68(5): 471. [DOI] [PubMed] [Google Scholar]
- Raphael D (2006). The social determinants of health: what are the three key roles for health promotion? Health Promot J Austr, 17(3): 167. [PubMed] [Google Scholar]
- Raphael D (2009). Escaping from the Phantom Zone: social determinants of health, public health units and public policy in Canada. Health Promot Int, 24(2): 193–198. [DOI] [PubMed] [Google Scholar]
- Riley BL, Taylor SM, Elliott SJ (2001). Determinants of implementing heart health promotion activities in Ontario public health units: a social ecological perspective. Health Educ Res, 16(4): 425–441. [DOI] [PubMed] [Google Scholar]
- Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. (2012). Adolescence and the social determinants of health. The Lancet, 379(9826): 1641–1652. [DOI] [PubMed] [Google Scholar]
- Wallace SP (2012). Social determinants of health inequities and healthcare in old age. Public health for an aging society, In: Prohaska T, Anderson L, Binstock R, Eds, Public Health for an Aging Society. Baltimore, MD: Johns Hopkins University Press: 99–118. [Google Scholar]
- Etemadi A (2007). Social Determinants of Health: Theme Issue on Poverty and Human Development. Arch Iran Med, 10(4): 433–434. [PubMed] [Google Scholar]
- Hosseinpoor AR, Naghavi M, Alavian SM, Speybroeck N, Jamshidi H, Vega J (2007). Determinants of seeking needed outpatient care in Iran: results from a national health services utilization survey. Arch Iran Med, 10(4): 439–445. [PubMed] [Google Scholar]
- Moradi-Lakeh M, Ramezani M, Naghavi M (2007). Equality in safe delivery and its determinants in Iran. Arch Iran Med, 10(4): 446–451. [PubMed] [Google Scholar]
- Baum F (2010). Overcoming barriers to improved research on the social determinants of health. MEDICC Rev, 12(3): 36–38. [DOI] [PubMed] [Google Scholar]
- Wilkinson R, Marmot M (2003). The Social Determinants of Health: The Solid Facts, Second ed. World Health Organization. [Google Scholar]
- Anonymous (2008). Addressing Social Determinants of Health: Accelerating the Prevention and Control of HIV/AIDS, Viral Hepatitis, STD and TB. External Consultation Meeting Report. Atlanta: U.S. Department of Health and Human Services Centers for Disease Control and Prevention-National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention [cited 2012. June, 2]; Available from: http://www.cdc.gov/socialdeterminants.
- Cohen BE, Gregory D (2009). Community Health Clinical Education in Canada: Part 1-” State of the Art”. Int J Nurs Educ Scholarsh, 6(1): 1–17. [DOI] [PubMed] [Google Scholar]
- Pawar AB, Mohan PVTK, Bansal RK (2008). Social determinants, suboptimal health behavior, and morbidity in urban slum population: an Indian perspective. J Urban Health, 85(4): 607–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foege WH (2010). Social determinants of health and health-care solutions. Public Health Rep, 125(4): 8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler M (2007). Social determinants of health: what, how, why, and now. Prev Chronic Dis, 4(4): 1–4. [PMC free article] [PubMed] [Google Scholar]
- Wilcox LS (2007). Onions and bubbles: models of the social determinants of health. Prev Chronic Dis, 4(4): 1–4. [PMC free article] [PubMed] [Google Scholar]
- Braveman P (2007). Do we have real poverty in the United States of America?, Prev Chronic Dis, 4(4): 4–6. [PMC free article] [PubMed] [Google Scholar]
- Holt JB (2007). The topography of poverty in the United States: a spatial analysis using county-level data from the Community Health Status Indicators project, Prev Chronic Dis, 4(4): 12. [PMC free article] [PubMed] [Google Scholar]
- Bartley M, Ferrie J, Montgomery SM (2005). Health and labour market disadvantage: unemployment, non-employment, and job insecurity. In: Social Determinants of Health, Eds, Marmot M and Wilkinson R. Oxford University Press: Oxford, 2: 78–96. [Google Scholar]
- Egan M, Petticrew M, Ogilvie D, Hamilton V (2003). New roads and human health: A systematic review. Am J Public Health, 93(9): 1463–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogilvie D, Egan M, Hamilton V, Petticrew M (2004). Promoting walking and cycling as an alternative to using cars: systematic review. BMJ, 329(7469): 763–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall J, Mhurchu CN, Blakely T, Rodgers A, Wilton J (2006). Effectiveness of monetary incentives in modifying dietary behavior: A review of randomized, controlled trials. Nutr Rev, 64(12): 518–531. [DOI] [PubMed] [Google Scholar]
- Bierman AS, Dunn JR. Swimming upstream (2006). J Gen Intern Med, 21(1): 99–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberg N (2007). From lifestyle to social determinants: new directions for community health promotion research and practice. Prev Chronic Dis, 4(3): 1–2. [PMC free article] [PubMed] [Google Scholar]
- Aust B, Ducki A (2004). Comprehensive health promotion interventions at the workplace: experiences with health circles in Germany. J Occup Health Psychol, 9(3): 258–270. [DOI] [PubMed] [Google Scholar]
- Bambra C, Egan M, Thomas S, Petticrew M, Whitehead M (2007). The psychosocial and health effects of workplace reorganisation. 2. A systematic review of task restructuring interventions. J Epidemiol Community Health, 61(12): 1028–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambra C, Whitehead M, Sowden A, Akers J, Petticrew M (2008). “A hard day’s night?” The effects of Compressed Working Week interventions on the health and work-life balance of shift workers: a systematic review. J Epidemiol Community Health, 62(9): 764–777. [DOI] [PubMed] [Google Scholar]
- Egan M, Bambra C, Thomas S, Petticrew M, Whitehead M, Thomson H (2007). The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J Epidemiol Community Health, 61(11): 945–954. [DOI] [PMC free article] [PubMed] [Google Scholar]


