Abstract
Background
To investigate through a two-stage clinic-based screening, the frequency and clinical features of risk for psychosis syndromes in a Chinese help-seeking sample.
Method
2101 consecutive new patients ages 15–45 were recruited at their first visit to the Shanghai Mental Health Center (SMHC) and screened with the Prodromal Questionnaire -brief version (PQ-B) and questions about genetic risk. The Structured Interview for Prodromal Syndromes (SIPS) was administered to a sub-sample to estimate rates of psychosis and clinical high risk (CHR) for psychosis syndromes.
Results
The frequency estimate of CHR syndromes in the total sample was 4.2%. Among 89 CHR patients, more than two-thirds met criteria for Attenuated Positive Symptom Syndrome (APSS); and nearly a quarter met the criteria for Genetic Risk and Deterioration Syndrome (GRDS). The frequency of CHR syndromes peaked between the ages of 16–21 years and declined with subsequent age. The mean total and distress scores on the PQ-B in subjects with APSS and psychosis were significantly higher than in individuals with GDRS and patients without psychosis or CHR. High frequencies and strong correlations were found among some positive and non-specific symptoms in SIPS interviews. Among the 53 CHR participants who were followed-up for two years, 14 (26.4%) converted to psychosis. Of the non-converters, 53.8% were diagnosed with Axis I disorders.
Conclusions
This two stage screening method can enhance detection of Chinese CHR patients in clinical settings. The validity of the procedures for detecting CHR is supported by rates of transition to psychosis and of non-converter Axis I disorders that are comparable to those reported in meta-analyses.
Keywords: Ultra-high risk, Early detection, Clinical high risk, Epidemiology, Help-seeking
1. Introduction
In order to predict the occurrence of schizophrenia and other related psychotic disorders, many studies in the past two decades have explored potential clinical features (Klosterkotter et al., 2001; Schultze-Lutter et al., 2010; Yung et al., 1998; Yung et al., 2005), and laboratory markers (Borgwardt et al., 2007; Bramon et al., 2008; Brockhaus-Dumke et al., 2008; Fusar-Poli et al., 2012; Giuliano et al., 2012; Seidman et al., 2010; van Rijn et al., 2011) of the period just preceding or associated with the onset of psychosis. Biomarkers to date, whether considered individually or in combination, are insufficient predictors of psychosis (Klosterkotter et al., 2011). However, clinical criteria and instruments have been designed to identify young people likely to be in the prodromal psychosis stage, also known as ultra high risk (UHR), clinical high risk (CHR) or in an at risk mental state (ARMS). Positive symptoms in the prodromal stage often manifest as an attenuated or transient form in which some reality testing is preserved. Nevertheless, they provide a reliable indicator of increased risk for later conversion to psychosis. Researchers in Melbourne, Australia, were the first to translate the clinical symptoms of the prodromal phase of psychosis into UHR criteria (Yung et al., 1996). In early studies up to 50% of subjects meeting these criteria developed psychosis within 2.5 years (Mason et al., 2004; Woods et al., 2009; Yung et al., 2008; Yung et al., 2004; Yung et al., 2006) although recent rates are more modest (Pusar-Foli et a., 2013), closer to 35% over three years. Subsequently, Miller et al. (Miller et al., 2002; Miller et al., 1999) in the United States developed a structured interview based on very similar criteria for predicting the development of psychosis. Thus, trained clinicians are able to identify the help-seeking individuals who are at high risk of developing a psychotic disorder based on attenuated (lack of conviction in the reality of the symptom) or transient psychotic symptoms or a combination of genetic risk and functional deterioration.
Identifying CHR subjects in time is crucial for preventing or delaying the development of psychosis. Both pharmacological and psychological treatments (Miller et al., 2003b; Morrison et al., 2007; Morrison et al., 2004; Phillips et al., 2007; Ruhrmann et al., 2005) have demonstrated promise in improving symptoms in CHR subjects in recent years. A meta-analysis suggests rates of transition to psychosis can be reduced significantly in CHR youth with specialized interventions (Preti and Cella, 2010). However, the criteria for formal diagnosis of prodomal psychosis are still unavailable for clinicians (Raballo and Laroi, 2011). Identification of individuals in the prodromal stage of psychosis remains largely reliant on research communities, criteria, and assessment methods worldwide. The predictive validity of current criteria in different cultures and contexts needs to be better characterized before standardized criteria and treatment guidelines for this population can be developed and disseminated. Clinical characteristics and patterns of help-seeking may vary by cultural context and clinical setting. Given the limited social support and the pressure of social discrimination, psychological counseling may be an important channel for CHR subjects in China to talk about the distress caused by their symptoms. Thus, this setting may be particularly relevant for evaluating CHR criteria in China.
No doubt, much of the extant focus has been on establishing the percentage of CHR individuals participating in specialized research programs who end up developing psychosis over the course of follow-up. Yet, there is a lack of epidemiologic data regarding the prevalence and clinical features of CHR syndromes in people seeking help in general outpatient mental health clinics. Most putatively prodromal samples have been referred to researchers by clinicians. The question remains as to the number of CHR subjects in the broader clinic population from which these were selected. Furthermore, what was the clinical status of these individuals at initial contact with clinical services? These findings will be helpful to policy makers in planning early detection and intervention strategies. An epidemiological study on prodromal psychosis based on a clinical population is taken as the first step for both research and implementation of the new criteria of a high risk for psychosis syndrome. It will also highlight to Chinese clinicians the importance of the psychosis prodrome, a concept that may currently be relatively unfamiliar to psychiatrists in many regions of China.
The goal of the present study is to examine the presence of possibly prodromal symptoms of psychosis in a representative sample of individuals seeking psychological help for a broad range of psychopathology. The primary aim is to report the frequency of CHR syndromes in patients arriving for their first visit to a busy Chinese outpatient clinic. The second aim is to profile the clinical features of prodromal psychosis in Chinese clinical practice. We explore the relationship between positive symptoms and other non-specific symptoms. Finally, we report on the validity of the identified syndrome by comparing rates of transition to psychosis and presence of Axis I disorders to those of comparable samples worldwide. Findings are expected to inform the potential of implementing diagnostic criteria and assessment of prodromal psychosis in both the clinical and research community, and broader early intervention strategies for CHR subjects.
2. Method
2.1. Participants
The Research Ethics Committee at the Shanghai Mental Health Centre (SMHC) approved the study in 2011. The study sample comprised of patients attending their initial outpatient assessment in the SMHC, the largest mental health clinic in Shanghai, China. Inclusion criteria were: (i) age of 15 - 45 years; (ii) individuals younger than 18 years had to be accompanied by either a parent or legal guardian; (iii) capacity to provide informed consent or assent if under 18; and (iv) must have completed at least six years of primary education. Exclusion criteria were: (i) severe somatic diseases, for example, pneumonia, cancer or heart failure, (ii) mental retardation, or (iii) dementia. Subjects approached were a consecutive series of those seeking an initial appointment at the psychological counseling service center according to the hospital register form.
2.2. Setting
The Shanghai Psychotherapy and Psychological Counseling Center (SPCC) at SMHC, is the largest outpatient mental health clinic offering medication management and psychotherapy in China. The outpatients are from different parts of the country. The SPCC serves over 300 outpatients of all ages per day. There are approximately 1,000 professional staff who provide care for the patients at the center. Among them, 258 are psychiatrists and psychologists and 541 are psychiatric nurses, along with other support staff. The SPCC provides comprehensive clinical services, including psychological assessment and counseling as well medical management. Patients come seeking help for issues ranging from general psychological problems (e.g., interpersonal adaptation, marriage and learning difficulties) to more severe psychological disorders and mental illnesses (e.g., schizophrenia and bipolar disorder).
2.3. Measures
2.3.1. Screening
The Prodromal Questionnaire -Brief version (PQ-B, Loewy et al., 2011) is a 21-item self-report measure derived from the 92-item Prodromal Questionnaire (Loewy et al., 2005). The PQ-B is designed to screen for possible prodromal symptoms. Respondents indicate the presence or absence of each symptom item with a “Yes/No”. The total score is the number of items marked “Yes”. For each symptom endorsed, the respondent indicates whether the symptom causes distress on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree). Loewy et al. (Loewy et al., 2011) found the PQ-B to be an effective, efficient self-report screening instrument for putatively prodromal syndromes in help-seeking populations with high sensitivity (89%) and medium specificity (58%) (a total score of 3 or more endorsed in PQ-B items, with the specificity of 68% and sensitivity of 88% while the distress score of 6 or more endorsed). The English version of the PQ-B was translated by the first and second authors (Zhang and Li), under the supervision of the corresponding authors (Wang and Xiao).
Genetic risk information was assessed with one question about family history of mental disorders and questions probing DSM-IV schizotypal personality disorder (SPD). Subjects listed family members with mental disorders in response to an item querying a history of mental disorders in family members. Nine items were selected from the SPD subscale in PDQ-4+ (Personality diagnostic questionnaire 4th edition plus) (Yang et al., 2002). Subjects were asked to think about their behavioral patterns in the last 2 years and check the “Yes/No” checkbox.
2.3.2. CHR and Psychosis Assessment
The Structured Interview for Prodromal Symptoms (SIPS) and Scale of Prodromal Syndromes (SOPS, thus SIPS/SOPS, (Miller et al., 2003a) were used to determine whether subjects met criteria for a putatively prodromal syndrome (CHR status) or the Presence of a Psychotic Syndrome (POPS). The SIPS consists of 19 items assessing four symptom domains: positive symptoms (Scales P1-P5, Unusual Thought Content, Suspiciousness, Grandiosity, Perceptual Abnormalities, and Disorganized Communication), Negative Symptoms (Scales N1-N6), Disorganized Symptoms (Scales D1-D4), and General Symptoms (Scales G1-G4). The Criteria of Prodrome Syndromes (COPS) outline three syndromes: Brief Intermittent Psychotic Syndrome (BIPS), Attenuated Positive Symptom Syndrome (APSS), and Genetic Risk and Deterioration Syndrome (GRDS). Each item is rated on a 1–6 scale with 6 indicating “severe and psychotic” and 3–5 indicating a prodromal range symptom. POPS is determined by the presence of a 6 level P symptom that is either 1) dangerous or disorganizing or 2) occurring at least an hour a day on average four days a week for at least a month. BIPS is indicated by the recent onset of P symptoms rated at a 6 level and occurring at least a few minutes a day at least once a month but not at sufficient frequency or duration to meet criteria for the POPS. APSS criteria are met by at least one P symptom rated 3–5, present at least once a week on average in the last month, and either new within the past year or rated at least one point higher (indicating worsening) than 1 year prior. GRDS is indicated by a functional deterioration (30% drop in Global Assessment of Functioning, GAF, score relative to 12 months prior) in the context of either schizotypal personality disorder or at least one first-degree relative with psychosis.
The English version SIPS/SOPS has demonstrated acceptable inter-rater reliability and predictive validity (Miller et al., 2003a; Miller et al., 2002). Agreement on P1-P5 scales differentiating prodromal from non-prodromal or psychotic patients after training workshops provided by Dr. Miller and other Yale University trainers has been satisfactory (kappa=0.81, 95% CI=0.55–0.93)(Miller et al., 2002). The first and second authors were both certified on the SIPS at Yale University-sponsored SIPS/SOPS trainings.
With written permission from the Yale authors, the SIPS/SOPS (Version 5) was translated into Chinese by our team and according to the strict international translation standard (Zheng et al., 2012). First, the SIPS was translated into Chinese. The translators were bilingual and bicultural and were familiar with the instrument. Second, the translation was reviewed by a panel of individuals fluent in both English and Chinese and knowledgeable about both cultures. The panel reviewed and compared each translated item with the original English version. Third, the translation was revised reflecting the best judgment of the panel. Fourth, the second revision was then translated back into English by a native Chinese speaker who was fluent in English, but unfamiliar with the purpose of the study. Fifth, the back translation was compared to the original version. In particular, the second author (Li) facilitated appropriate attention to linguistic nuance and culturally-specific aspects of symptom presentation in the Chinese version of the SIPS. Preliminary SIPS data collected at SMHC ({Miller, 2003 #26}) show good inter-rater reliability (r=0.96, p<0.01 on the SOPS score). Expressed as the kappa value, the agreement rate between the four psychiatrists was 0.81–0.95. The inter-rater reliability (ICC) for the SIPS/SOPS positive symptoms ranged from ICC 0.86 (P5) to 0.98 (P4) within four raters. The Cronbach’s α for all SOPS items was 0.71, and the total SOPS score correlated significantly with the Chinese PANSS total score (r=0.63, p<0.01).
2.3.3. Clinical Diagnoses
The clinical diagnostic information of participants reported in this paper was from their outpatient medical records. All of the participants had received a clinical diagnosis of mental disorder from our psychiatrists using criteria established in the third edition of the Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD-3; Chinese Society of Psychiatry, 2001). This is a clinical guide used in China for routine practice. Diagnoses defined in CCMD-3 are intentionally identical or similar in structure and categorization to international classifications (DSM-IV or ICD-10). The CCMD-3 consists of 10 main diagnostic categories such as schizophrenia and other psychotic disorders, affective disorders, neurosis (phobia, anxiety disorder, obsession, and somatoform disorders), stress-related disorders (acute stress disorders, post-traumatic stress disorders, adjustment disorders) and so on.
2.4. Procedures
Similar to recruitment conducted at SMHC by this research team in 2006 (Zhang et al., 2012a; Zhang et al., 2012b), all new patients seeking treatment at the SPCC between March and September 2011 were invited to participate in the study by a psychiatric triage nurse. After obtaining informed consent, the nurse gave participants the PQ-B. Participants meeting the following criteria were referred for a same-day SIPS/SOPS interview: (i) A total score of 3 or higher on the PQ-B; (ii) A PQ-B distress score of 6 or higher, and/or (iii) one or more first-degree relatives with affective or non-affective psychosis. To assess the false negative rate of PQ-B, we also randomly selected 20% of patients who did not meet these criteria to receive the SIPS/SOPS interview. SIPS interviews were conducted by four experienced psychiatrists who have received SIPS interview training (with a minimum of three years of psychiatric practice experience). Supervision of SIPS/SOPS interviews was conducted on a weekly or fortnightly basis by two senior psychiatrists.
2.5. Statistical analyses
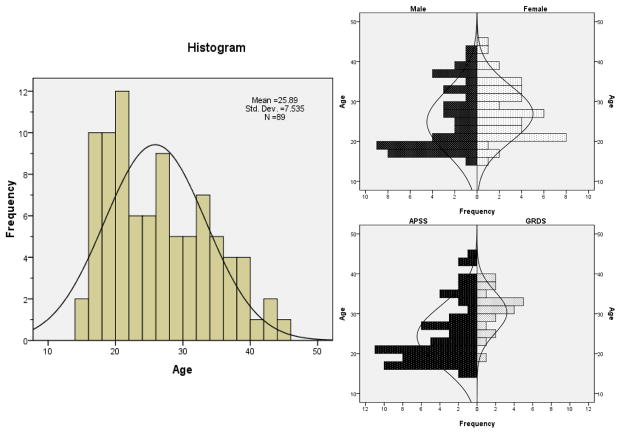
Data were summarized using standard descriptive statistics in SPSS version 16.0 (SPSS, Inc., Chicago, IL, USA) statistical software. Independent-samples t-tests were used to test between group comparisons, as applicable. Significance was determined by p < 0.05 (two-tailed). For further graphical representation of the age distributions in the total sample, male/female groups and APSS/GRDS groups, bar diagrams showing the number of prodromal subjects by single year of age were prepared. A box-plot-diagram (Min, 25% Quartile, Median, 75% Quartile, Max) was created by SPSS software showing the difference in PQ-B total and distress scores among four groups divided as APSS, GDRS, POPS and control group. Statistically significant differences among those CHR syndrome and psychosis groups were evaluated by one-way analysis of variance (ANOVA) followed by post hoc Fisher’s LSD multiple comparison tests. The correlation between positive symptoms and other subscales was calculated by nonparametric Spearman’s rank-correlation analysis.
3. Results
3.1. Overall Sample Characteristics
Of the 2,705 patients seeking treatment within the study period, 2,101 subjects met the study entry inclusion criteria and consented to be screened. This sample consisted of 935 males (44.5%) and 1,166 females (55.5%) with an average age of 27.1 years (SD =7.4). Of these, 1681 subjects were screened as positive with the PQ-B, 1,384 (82.3%) of whom completed the SIPS/SOPS interviews. Of the 420 subjects screened as negative, 77 (18.3%) completed the SIPS/SOPS interviews. A total of 89 subjects (4.2% of the initial 2101) met the criteria for a CHR syndrome, 87 patients who were initially screened positive, and 2 of those screened negative. A total of 105 subjects (5.0% of the initial 2101 subjects) met the criteria for POPS. The investigated 1907 sample who did not meet the criteria of APSS, GRDS and POPS (control group) included 835 males and 1072 females, with an average age of 27.4 years (SD=7.3) (see Figure 1 for a flow chart of the study sample).
Fig. 1.
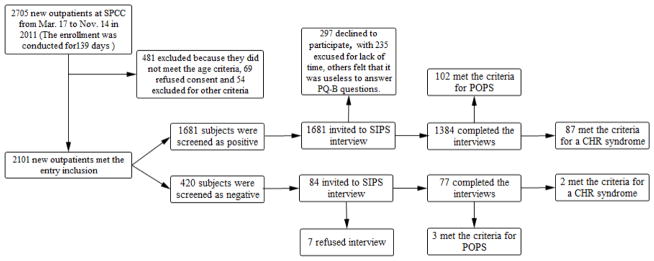
Sample Flowchart.
More than two-thirds of the CHR patients met criteria for APSS, while nearly a quarter met criteria for GRDS and only three met criteria for BIPS (see Table 1). The GRDS sample was significantly older than the APSS group (t=−4.008, p<0.01). The majority of CHR subjects (58.4%) was considered as having or was diagnosed with mood or anxiety disorders according to their medical records. Only a small minority who met criteria for APSS was diagnosed as having schizophrenia by their clinicians. The mean percentage drop in GAF score over the past year in prodromal subjects was 26.4%, with GRDS patients having significantly larger GAF drops than APSS patients, partly by syndrome definition (t=−7.108, p<0.01; See Table 1).
Table 1.
Age, Sex, Clinical Diagnoses and Drop in GAF Score by CHR Syndrome
| Type | N (%) | Age Mean (SD) | Male | Psychosis | Suspected Psychosis | Mood or Anxiety Disorder | Suspected Mood or Anxiety Disorder | Stress related disorder | Other Disorders or not yet determined | % Drop in GAF Mean (SD) |
|---|---|---|---|---|---|---|---|---|---|---|
| APSS | 62 (69.7%) | 24.34 (7.654) | 31 (50.0%) | 7 (11.3%) | 17 (27.4%) | 14 (22.6%) | 18 (29.0%) | 2 (3.2%) | 4 (6.5%) | 23.9% (8.8%) |
| GRDS | 21 (23.6%) | 30.33 (5.209) | 12 (57.1%) | 0 | 0 | 8 (38.1%) | 10 (47.6%) | 1 (4.8%) | 2 (9.5%) | 32.7% (2.5%) |
| BIPS | 2 (2.2%) | 20 41 |
1 | 1 | 1 | 0 | 0 | 0 | 0 | 22.2% 31.4% |
| GRDS & APSS | 3 (3.4%) | 24 27 27 |
0 | 0 | 0 | 0 | 2 | 0 | 1 | 31.3% 30.7% 31.3% |
| GRDS & BIPS | 1 (1.1%) | 19 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 37.8% |
| Total | 89 (100%) | 25.89 (7.535) | 45 (50.6%) | 8 (9.0%) | 19 (21.3%) | 22 (24.7%) | 30 (33.7) | 3 (3.4%) | 7 (7.9%) | 26.4% (8.5%) |
Note. The number of cases in BIPS, GRDS & APSS and GRDS & BIPS were no more than 3, so the individual data from subjects were listed. All the diagnostic information was collected from outpatients’ medical records which were created by their attending doctors according to the Chinese mental health diagnostic manual. Here, “suspected” indicates a nonconclusive diagnosis. Take “suspected psychosis” as an example, when a clinician gives the diagnosis of “suspected schizophrenia” or “state of suspiciousness,” we classify them into the “Suspected Psychosis” group.
3.2. Age at CHR Identification
The relationship between CHR syndrome and age is shown in Fig 2. The frequency of putatively prodromal psychosis or CHR in this sample peaked in early adulthood (16–21 years old) and declined with subsequent age. Compared to males, females presented with CHR syndromes during a broader age range (20–35 years old), with a slightly older age of peak frequency. Unlike males or patients in the APSS group for whom the peak frequency of CHR syndromes was in young adulthood, patients who met criteria of GRDS were identified at highest frequency over 30 years old.
Fig. 2.
Age Distribution for the Total Sample, Males, Females, APSS, and GRDS groups.
3.3. PQ-B Scores and Subsequent CHR Syndrome Identification
Perhaps not surprisingly, individuals with APSS and POPS endorsed significantly more symptoms on the PQ-B than either the GRDS or control group and both APSS and POPS groups reported significantly higher distress scores than the control group (see Table 2 and Fig. 3). The PQ-B cutoff point of total score of 3 or higher, distress score of 6 or higher for diagnosis of CHR yielded a sensitivity of 97.8% and a specificity of 20.8%. This cutoff point yielded a sensitivity of 97.4% and a specificity of 21.8% for identifying subjects with CHR or POPS.
Table 2.
Comparison of Total and Distress Scores of PQ-B
| Groups | Total score of PQ-B
|
Distress score of PQ-B
|
|||||
|---|---|---|---|---|---|---|---|
| N | Mean ± SD | p Value (Control) | p Value (GRDS) | Mean ± SD | p Value (Control) | p Value (GRDS) | |
|
|
|
||||||
| APSS | 62 | 11.21 ± 4.491 | 0.000 | 0.028 | 43.39 ± 19.507 | 0.000 | 0.059 |
| GRDS | 21 | 8.48 ± 5.810 | 0.142 | - | 34.19 ± 26.940 | 0.023 | - |
| POPS | 105 | 10.26 ± 4.895 | 0.000 | 0.131 | 37.96 ± 21.148 | 0.000 | 0.414 |
| Control Group | 1907 | 6.89 ± 4.931 | - | 0.142 | 24.55 ± 19.082 | 0.023 | |
Note. p Value (Control): p Value for comparison between Control Group and APSS, GDRS, POPS by one-way ANOVA and Fisher’s LSD post hoc test. p Value (GRDS) is the same. Control Group was composed of subjects consented who did not meet the criteria of APSS, GDRS and POPS) screened by PQ-B.
Fig. 3.
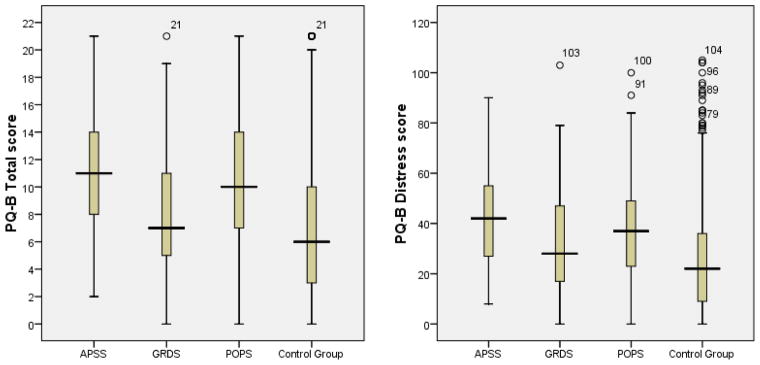
Total and Distress Score of PQ-B Distribution for APSS, GRDS, POPS, and Control Group.
3.4. SIPS/SOPS Symptoms in Chinese Help-Seeking Outpatients
Table 3 shows the frequency of positive symptoms endorsed in the SIPS/SOPS interviews. The most frequent positive symptoms reported by CHR subjects were unusual thought content and suspiciousness, followed by perceptual abnormalities (see Table 3 for details). Social anhedonia, avolition and occupational functioning in negative symptoms, trouble with focus and attention in disorganized symptoms, sleep disturbance, dysphoric mood and impaired tolerance to normal stress in general symptoms were the most frequently identified negative, disorganized, and general symptoms.
Table 3.
Frequency Profiles for CHR Subjects on SIPS/SOPS Subscales
| SOPS Items | Positive (N)
|
Median | IQR | Range | |||
|---|---|---|---|---|---|---|---|
| Total (N=89) | APSS (N=65) | GRDS (N=25) | BIPS (N=3) | ||||
| P. POSITIVE SYMPTOMS (Number, N, with a rating of 3 or higher) | |||||||
| P1 Unusual Thought Content/Delusional Ideas | 42 | 40 | 0 | 2 | 2 | 4 | 0 – 5 |
| P2 Suspiciousness/Persecutory Ideas | 36 | 33 | 3 | 3 | 2 | 4 | 0 – 5 |
| P3 Grandiose Ideas | 1 | 1 | 0 | 0 | 0 | 0 | 0 – 4 |
| P4 Perceptual Abnormalities/Hallucinations | 30

|
29 | 2

|
3

|
0 | 4 | 0 – 6 |
| P5 Disorganized Communication | 7 | 7 | 0 | 0 | 0 | 2 | 0 – 4 |
| N. NEGATIVE SYMPTOMS | Value (MODE) | ||||||
| N1 Social Anhedonia | 2 | 2 | 3 | 1,1,2 | 2 | 2 | 0 – 5 |
| N2 Avolition | 2 | 2 | 3 | 1,1,3 | 2 | 2 | 0 – 5 |
| N3 Expression of Emotion | 0 | 0 | 0 | 1,1,2 | 0 | 1 | 0 – 4 |
| N4 Experience of Emotions and Self | 0 | 0 | 0 | 1,2,2 | 0 | 2 | 0 – 4 |
| N5 Ideational Richness | 0 | 0 | 0 | 1,1,2 | 0 | 0 | 0 – 6 |
| N6 Occupational Functioning | 3 | 2 | 3 | 3,3,5 | 3 | 1 | 0 – 6 |
| D. DISORGANIZATION SYMPTOMS (MODE) | |||||||
| D1 Odd Behavior of Appearance | 0 | 0 | 0 | 0,1,2 | 0 | 0 | 0 – 3 |
| D2 Bizarre Thinking | 0 | 0 | 0 | 0,2,3 | 0 | 1 | 0 – 3 |
| D3 Trouble with Focus and Attention | 2 | 2 | 2 | 2,2,3 | 2 | 2 | 0 – 5 |
| D4 Impairment in Personal Hygiene | 0 | 0 | 0 | 0,0,2 | 0 | 0 | 0 – 3 |
| G. GENERAL SYMPTOMS (MODE) | |||||||
| G1 Sleep Disturbance | 3 | 3 | 3 | 0,2,3 | 3 | 2 | 0 – 6 |
| G2 Dysphoric Mood | 2 | 2 | 5 | 2,2,3 | 3 | 3 | 0 – 6 |
| G3 Motor Disturbances | 0 | 0 | 0 | 0,0,1 | 0 | 0 | 0 – 3 |
| G4 Impaired Tolerance to Normal Stress | 2 | 2 | 2 | 2,2,3 | 2 | 1 | 0 – 5 |
Note. Comorbid prodromal syndromes were not considered in this table. IQR: Inter quartile range. The mode is the value that appears most often in a set of data.
 : one case was scored 6 (met the criteria of current psychosis). The number of cases in BIPS was only 3, so the raw data from BIPS for negative symptoms, disorganized symptoms and general symptoms were listed.
: one case was scored 6 (met the criteria of current psychosis). The number of cases in BIPS was only 3, so the raw data from BIPS for negative symptoms, disorganized symptoms and general symptoms were listed.
3.5. Correlation of Symptoms and Functioning
Table 4 shows the Spearman’s rank correlation coefficients between positive symptoms, percentage drop of GAF and other subscales for 65 subjects with APSS (APSS criteria are met by at least one P symptom). There was a statistically significant unadjusted positive correlation (p<0.01) between P1 and N6, P4 and N4, P5 and N1-6, and D4, and between a drop in GAF and N6 and G4. The strongest correlation (r = 0.517) was observed between a drop in GAF and G4.
Table 4.
Spearman’s Rank Correlation among SIPS/SOPS Subscales in Subjects with APSS (N=65)
| N1 | N2 | N3 | N4 | N5 | N6 | D1 | D2 | D3 | D4 | G1 | G2 | G3 | G4 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | 0.248* | 0.157 | 0.306* | 0.331** | 0.259* | 0.320** | 0.191 | 0.384** | 0.056 | 0.112 | −0.176 | −0.257* | 0.133 | 0.100 |
| P2 | 0.053 | 0.114 | 0.069 | 0.101 | 0.236 | 0.076 | 0.177 | 0.088 | −0.225 | 0.143 | −0.076 | 0.121 | 0.077 | 0.027 |
| P3 | 0.228 | 0.046 | 0.191 | 0.183 | −0.089 | 0.133 | −0.084 | 0.297* | 0.078 | 0.153 | −0.046 | −0.057 | −0.046 | 0.203 |
| P4 | 0.315* | 0.208 | 0.280* | 0.371** | 0.134 | 0.104 | 0.088 | −0.039 | 0.087 | 0.209 | 0.169 | 0.216 | 0.012 | 0.217 |
| P5 | 0.486** | 0.462** | 0.469** | 0.482** | 0.383** | 0.258* | 0.183 | 0.217 | 0.105 | 0.334** | −0.153 | −0.070 | 0.230 | 0.195 |
| Drop GAF | 0.297* | 0.142 | 0.061 | 0.112 | 0.114 | 0.442** | 0.121 | 0.236 | −0.091 | 0.055 | 0.148 | 0.170 | 0.193 | 0.517** |
Note.
Correlation is significant at the 0.05 level (2-tailed).
Correlation is significant at the 0.01 level (2-tailed).
3.6. Transition to Psychosis outcomes
Through October 2013, 53/89 (59.6%) CHR subjects completed a two years follow-up assessment, 11 (12.4%) subjects withdrew from study and 25 (28.1%) could not be reached by phone or mail. At follow-up, 12 out of the 53 subjects were available for face-to-face interview and the remaining 41 were available for telephone contact. SMHC medical records were available as well. Information on the CHR subjects was updated and recorded in the research files every year. Among the 53 CHR cases, 14 (26.4%) converted to psychosis. Specifically, 4 were hospitalized in psychiatric units and diagnosed with schizophrenia, 8 were diagnosed with schizophrenia at the outpatient clinic in last two years, and 2 met POPS criteria on interview. Among the 39 subjects who did not convert to full-blown psychosis, 21 were diagnosed with an Axis I disorder and had received treatment during the follow-up period. Ten out of the 39 remitted and no longer met CHR criteria, 8 had not converted but reported some attenuated psychotic symptoms at follow-up and were taking anti-psychotic medicine irregularly.
4. Discussion
There is a growing body of research into the early detection of prodromal psychosis in clinical samples worldwide (Addington et al., 2007; Broome et al., 2005; Cannon et al., 2008; Green et al., 2011; Ruhrmann et al., 2009; Yung et al., 2008; Yung et al., 2006). However, most putatively prodromal samples are clinician-referred (Addington et al., 2008; Simon et al., 2006; Simon and Umbricht, 2010). As reported in previous studies, nearly one third of such referrals meet putatively prodromal criteria (Fusar-Poli et al., 2013b). Thus, training clinicians would appear to be a more efficient early detection strategy than a clinic-wide screening. However, referrals to a third party (such as a research team) rarely occur in Chinese clinical practice and some cultural factors need to be considered. Patients experience being “kicked around” to different parts of the hospital, especially in a first visit, if sent for research. Doctors may worry that other clinicians or researchers will have different opinions about the diagnosis or treatment. Even the “referral” concept itself could lead patients to lose confidence in their doctors in China (Li et al., 2009).
Whereas the concept of an “At Risk Mental State” had initially been used by Lam et al. (2006) in Hong Kong, China, the term of prodromal psychosis had not been formally researched and implemented in mainland China. Lam et al found that about 29% of symptomatic individuals would transition to frank psychosis within a 6 month period of time. Such a high transition rate warrants attention from Chinese clinicians. However, the concept of “clinical high risk” is still largely unfamiliar in mainland China. Lack of standardized tools may partially account for this pattern. To our knowledge, our research group is one of the first to investigate the distribution of the CHR subjects in an epidemiological way in a clinical setting in mainland China. Examination of the clinical diagnoses of CHR subjects through clinic-based screening offers an additional perspective on the degree to which Chinese clinicians are currently recognizing psychosis and psychosis risk. Only one-fifth of CHR subjects detected through the broad clinic screening were considered to be possibly psychotic (e.g. schizophrenia was suspected) by Chinese clinicians, and less than one third were considered related to psychosis (including both the diagnosis of psychosis and suspected psychosis). Most CHR subjects were treated for mood or anxiety disorders, which is not surprising, given high rates of comorbid anxiety and depressive disorders in CHR samples (Fusar-Poli et al., in press; Salokangas et al., 2012). It is reasonable that non-psychotic symptoms are more often of concern to both patients and clinicians. However, clinicians without sufficient training in the subtle pre-psychotic symptoms, particularly those with a genetic risk and significant drop in functioning, may miss identifying young people at risk (Rietdijk et al., 2012). Extensive effort and significant resources are needed to recruit samples by clinical referral (Addington et al., 2008; McGlashan et al., 2007). Screening for early symptoms of emerging psychosis in help-seeking populations may be more effective for research recruitment and early intervention in China. The two-stage detection strategy described above, although involving intensive effort, identified 89 patients meeting CHR status within just seven months, a significant recruitment rate compared to longstanding early intervention programs worldwide (Addington et al., 2007; Fusar-Poli et al., 2013b; Phillips et al., 2002). It thus holds promise, not only for facilitating early intervention in China, but for more rapidly advancing worldwide research with this population.
The effects of age and sex have been postulated to play a role in the onset of psychosis. We found that the peak age range of new patients meeting prodromal syndrome criteria was between the 16 and 21 years, which is largely consistent with other studies (Fusar-Poli et al., 2013b; Miller et al., 2002; Morrison et al., 2011; Yung et al., 2007a; Yung et al., 2007b). The mean age of our sample at 25.9 years was consistent with some clinical trials in adult cohorts (Allen et al., 2012; Koutsouleris et al., 2012) but it was older than the sample (N=370) of the North American Prodrome Longitudinal Study (NAPLS), where the mean age is 18.2 (SD=4.7) years) (Addington et al., 2007). Two things may account for this age difference. Firstly, we included subjects between 15 and 45 years of age, while the NAPLS recruited subjects 12 to 35 years of age. Secondly, our study recruited subjects who were not referred by clinicians.
We found an early and steep increase in frequency of prodromal syndromes between the age of 16 to 21 in males, and a delayed and gradual increase by age in females. Research indicates that male patients with schizophrenia have an earlier age of onset than females (Faraone et al., 1994; Hafner et al., 1993). This phenomenon highlights the potential importance of differential screening by age and gender (e.g., expanding screening to older females). In addition, APSS subjects were younger than GRDS, and made up the majority of the CHR sample (70%). BIPS subjects were rare. Previous findings (Kelleher et al., 2012; Woods et al., 2009) have also found APSS to be the most common of the three prodromal syndromes according to the COPS criteria, with very low rates of BIPS in most CHR samples. Further research is needed to determine the relative predictive value of syndromes identified through screening in Chinese and other clinic samples will require follow-up over time. Findings from such studies could further inform best strategies for clinician training.
The results of the PQ-B are timely given that Chinese researchers have proposed the screening method as a better option for recruitment. Our preliminary data showed that the PQ-B could be a very useful tool for discriminating subjects with potentially psychotic symptoms from other help-seeking clients. The sensitivity of the PQ-B was excellent in this study. In fact, this clinic screening strategy detected over three times the typical rates of CHR subjects obtained via more traditional clinician referral methods. However, specificity of the traditional PQ-B cut-off in this sample was low. Outpatients seeking help in the hospital, may be likely to report high rates of “false positive” symptoms (the false positive rate in this study was 79.2%) on this screening questionnaire. For example, the question in the PQ-B “Do you worry at times that something may be wrong with your mind?” was responded positively for 72.8% subjects. And the question of “Have you felt that you are not in control of your own ideas or thoughts?” was responded positively by 62.8% subjects. With a higher cut-off point on the PQ-B, a two-stage screening process combining the PQ-B and SIPS may result in a highly efficient recruitment method. High rates of GRDS detection in this study support the additional inclusion of a brief screening for genetic risk and schizotypal personality disorder. As other researchers have previously proposed (Broome et al., 2005; Rietdijk et al., 2012), self-report screening measures can be quite useful to identifying a substantial subset of the CHR population.
Our investigation showed that “Unusual Thought Content”, “Suspiciousness” and “Perceptual Abnormalities” were prevalent in CHR individuals with positive symptoms. However, very few cases with “Grandiose Ideas” were identified in this sample. We suppose that grandiosity may be difficult to detect or less frequent in a help-seeking population (Hsiao et al., 1999), especially in a first time meeting. In traditional Chinese culture, being modest is particularly valued, making it particularly unacceptable to share “Grandiose Ideas” with people on initial meeting (Oyserman and Lee, 2008).
Although prodromal symptoms rely primarily on the presence of positive symptoms, non-specific symptoms such as negative symptoms, disorganizing symptoms, and general symptoms are quite common in CHR subjects. Indeed, our results suggest that some common non-specific symptoms may be secondary to prodromal psychosis. Particularly, most negative symptoms were positively related with P1, P4 and P5. Based on published reports (Blanchard et al., 2005; Piskulic et al., 2012), those non-specific symptoms may be vulnerability factors for developing psychosis. However, as the term “non-specific” suggests, these symptoms may predict other mental disorders such as depression and anxiety disorder as well (Addington et al., 2011) as suggested by the relatively high rates of comorbid Axis I disorders among CHR subjects (Fusar-Poli et al., in press; Myles-Worsley et al., 2007). More research is needed to determine if these non-specific symptoms reflect secondary effects of positive symptoms or core symptoms in the early stage of psychosis.
The present findings may also help direct clinicians to ask a more questions about subtle psychotic symptoms (mainly P1, unusual Thought Content, P2, Suspiciousness, and P4, Perceptual Abnormalities) during initial visits, even when the patients’ complaints are about depressive or anxious symptoms. The assessment of role function (such as school or work performance) should be a focus for identifying CHR subjects, especially for adolescents and young adults ages 16–21 years old or individuals with familial risk. Although there are no established guidelines for CHR treatment, a special team (for either research or service purpose) to better stratify the intervention activities and strategies is urgently needed in Chinese psychiatric or psychological medicine departments.
Finally, although the recruitment of a large sample of CHR is on-going and the longitudinal follow-up has not been fully completed, there are preliminary 2 year follow-up conversion rate data. Among the 53 CHR participants who were followed-up for two years, 14 (26.4%) converted to psychosis, relatively consistent with the rates summarized in Fusar Poli (Fusar-Poli et al., 2013a). Of the non-converters, 53.8% were diagnosed with Axis I disorders, also consistent with reports from other centers.
A further limitation is that, due to resource limitations, only a small proportion of those being screened negative by PQ-B received the more definitive SIPS/SOPS interviews. In fact, 2 out of the 77 screened negative subjects turned out to meet the criteria for a CHR syndrome. So it is possible that there were yet other undetected CHR cases among the 343 screened negative cases. This could lead to a significant underestimation of the true prevalence rate of CHR in the study population.
A final limitation of this study is that subjects were outpatients of the largest psychological counseling clinic in Shanghai, which is one of the mostly highly developed cities in China, limiting the generality of our finding to rural settings in China. Despite these limitations, the fact that this two stage screening method led to detection of Chinese CHR patients, for whom the rates of transition to psychosis and of Axis I disorders were comparable to those reported in meta-analyses, supports its validity in a large, urban, mental health center in China.
References
- Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, Seidman LJ, Tsuang M, Walker EF, Woods SW, Heinssen R. North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33(3):665–672. doi: 10.1093/schbul/sbl075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Cornblatt BA, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Heinssen R. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011;168(8):800–805. doi: 10.1176/appi.ajp.2011.10081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Epstein I, Reynolds A, Furimsky I, Rudy L, Mancini B, McMillan S, Kirsopp D, Zipursky RB. Early detection of psychosis: finding those at clinical high risk. Early Interv Psychiatry. 2008;2(3):147–153. doi: 10.1111/j.1751-7893.2008.00078.x. [DOI] [PubMed] [Google Scholar]
- Allen P, Chaddock CA, Howes OD, Egerton A, Seal ML, Fusar-Poli P, Valli I, Day F, McGuire PK. Abnormal relationship between medial temporal lobe and subcortical dopamine function in people with an ultra high risk for psychosis. Schizophr Bull. 2012;38(5):1040–1049. doi: 10.1093/schbul/sbr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard JJ, Horan WP, Collins LM. Examining the latent structure of negative symptoms: is there a distinct subtype of negative symptom schizophrenia? Schizophr Res. 2005;77(2–3):151–165. doi: 10.1016/j.schres.2005.03.022. [DOI] [PubMed] [Google Scholar]
- Borgwardt SJ, McGuire PK, Aston J, Berger G, Dazzan P, Gschwandtner U, Pfluger M, D’Souza M, Radue EW, Riecher-Rossler A. Structural brain abnormalities in individuals with an at-risk mental state who later develop psychosis. Br J Psychiatry Suppl. 2007;51:s69–75. doi: 10.1192/bjp.191.51.s69. [DOI] [PubMed] [Google Scholar]
- Bramon E, Shaikh M, Broome M, Lappin J, Berge D, Day F, Woolley J, Tabraham P, Madre M, Johns L, Howes O, Valmaggia L, Perez V, Sham P, Murray RM, McGuire P. Abnormal P300 in people with high risk of developing psychosis. Neuroimage. 2008;41(2):553–560. doi: 10.1016/j.neuroimage.2007.12.038. [DOI] [PubMed] [Google Scholar]
- Brockhaus-Dumke A, Schultze-Lutter F, Mueller R, Tendolkar I, Bechdolf A, Pukrop R, Klosterkoetter J, Ruhrmann S. Sensory gating in schizophrenia: P50 and N100 gating in antipsychotic-free subjects at risk, first-episode, and chronic patients. Biol Psychiatry. 2008;64(5):376–384. doi: 10.1016/j.biopsych.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Broome MR, Woolley JB, Johns LC, Valmaggia LR, Tabraham P, Gafoor R, Bramon E, McGuire PK. Outreach and support in south London (OASIS): implementation of a clinical service for prodromal psychosis and the at risk mental state. Eur Psychiatry. 2005;20(5–6):372–378. doi: 10.1016/j.eurpsy.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65(1):28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Chen WJ, Goldstein JM, Tsuang MT. Gender differences in age at onset of schizophrenia. Br J Psychiatry. 1994;164(5):625–629. doi: 10.1192/bjp.164.5.625. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rossler A, Schultze-Lutter F, Keshavan M, Wood S, Ruhrmann S, Seidman LJ, Valmaggia L, Cannon T, Velthorst E, De Haan L, Cornblatt B, Bonoldi I, Birchwood M, McGlashan T, Carpenter W, McGorry P, Klosterkotter J, McGuire P, Yung A. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013a;70(1):107–120. doi: 10.1001/jamapsychiatry.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Byrne M, Badger S, Valmaggia LR, McGuire PK. Outreach and support in South London (OASIS), 2001–2011: Ten years of early diagnosis and treatment for young individuals at high clinical risk for psychosis. Eur Psychiatry. 2013b;28(5):315–26. doi: 10.1016/j.eurpsy.2012.08.002. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Deste G, Smieskova R, Barlati S, Yung AR, Howes O, Stieglitz RD, Vita A, McGuire P, Borgwardt S. Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry. 2012;69(6):562–571. doi: 10.1001/archgenpsychiatry.2011.1592. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid Depressive and Anxiety Disorders in 509 Individuals With an At-Risk Mental State: Impact on Psychopathology and Transition to Psychosis. Schizophr Bull. doi: 10.1093/schbul/sbs136. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano AJ, Li H, Mesholam-Gately RI, Sorenson SM, Woodberry KA, Seidman LJ. Neurocognition in the psychosis risk syndrome: a quantitative and qualitative review. Curr Pharm Des. 2012;18(4):399–415. doi: 10.2174/138161212799316019. [DOI] [PubMed] [Google Scholar]
- Green CE, McGuire PK, Ashworth M, Valmaggia LR. Outreach and Support in South London (OASIS). Outcomes of non-attenders to a service for people at high risk of psychosis: the case for a more assertive approach to assessment. Psychol Med. 2011;41(2):243–250. doi: 10.1017/S0033291710000723. [DOI] [PubMed] [Google Scholar]
- Hafner H, Maurer K, Loffler W, Riecher-Rossler A. The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry. 1993;162:80–86. doi: 10.1192/bjp.162.1.80. [DOI] [PubMed] [Google Scholar]
- Hsiao MC, Liu CY, Yang YY, Yeh EK. Delusional disorder: retrospective analysis of 86 Chinese outpatients. Psychiatry Clin Neurosci. 1999;53(6):673–676. doi: 10.1046/j.1440-1819.1999.00624.x. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Murtagh A, Molloy C, Roddy S, Clarke MC, Harley M, Cannon M. Identification and characterization of prodromal risk syndromes in young adolescents in the community: a population-based clinical interview study. Schizophr Bull. 2012;38(2):239–246. doi: 10.1093/schbul/sbr164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klosterkotter J, Hellmich M, Steinmeyer EM, Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Arch Gen Psychiatry. 2001;58(2):158–164. doi: 10.1001/archpsyc.58.2.158. [DOI] [PubMed] [Google Scholar]
- Klosterkotter J, Schultze-Lutter F, Bechdolf A, Ruhrmann S. Prediction and prevention of schizophrenia: what has been achieved and where to go next? World Psychiatry. 2011;10(3):165–174. doi: 10.1002/j.2051-5545.2011.tb00044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koutsouleris N, Davatzikos C, Bottlender R, Patschurek-Kliche K, Scheuerecker J, Decker P, Gaser C, Moller HJ, Meisenzahl EM. Early recognition and disease prediction in the at-risk mental states for psychosis using neurocognitive pattern classification. Schizophr Bull. 2012;38(6):1200–1215. doi: 10.1093/schbul/sbr037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam MM, Hung SF, Chen EY. Transition to psychosis: 6-month follow-up of a Chinese high-risk group in Hong Kong. Aust N Z J Psychiatry. 2006;40(5):414–420. doi: 10.1080/j.1440-1614.2006.01817.x. [DOI] [PubMed] [Google Scholar]
- Li X, Zhang X, Wang Q. The Research on Misunderstanding to Consultation and Referral of Counseling Psychologist. China Journal of Health Psychology. 2009;19(2):245–247. [Google Scholar]
- Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD. The prodromal questionnaire (PQ): preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr Res. 2005;79(1):117–125. [PubMed] [Google Scholar]
- Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD. Psychosis risk screening with the Prodromal Questionnaire--brief version (PQ-B) Schizophr Res. 2011;129(1):42–46. doi: 10.1016/j.schres.2011.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason O, Startup M, Halpin S, Schall U, Conrad A, Carr V. Risk factors for transition to first episode psychosis among individuals with ‘at-risk mental states’. Schizophr Res. 2004;71(2–3):227–237. doi: 10.1016/j.schres.2004.04.006. [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Addington J, Cannon T, Heinimaa M, McGorry P, O’Brien M, Penn D, Perkins D, Salokangas RK, Walsh B, Woods SW, Yung A. Recruitment and treatment practices for help-seeking “prodromal” patients. Schizophr Bull. 2007;33(3):715–726. doi: 10.1093/schbul/sbm025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003a;29(4):703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, Woods SW. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159(5):863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Woods SW, Stein K, Driesen N, Corcoran CM, Hoffman R, Davidson L. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70(4):273–287. doi: 10.1023/a:1022034115078. [DOI] [PubMed] [Google Scholar]
- Miller TJ, Zipursky RB, Perkins D, Addington J, Woods SW, Hawkins KA, Hoffman R, Preda A, Epstein I, Addington D, Lindborg S, Marquez E, Tohen M, Breier A, McGlashan TH. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis. II. Baseline characteristics of the “prodromal” sample. Schizophr Res. 2003b;61(1):19–30. doi: 10.1016/s0920-9964(02)00440-1. [DOI] [PubMed] [Google Scholar]
- Morrison AP, French P, Parker S, Roberts M, Stevens H, Bentall RP, Lewis SW. Three-year follow-up of a randomized controlled trial of cognitive therapy for the prevention of psychosis in people at ultrahigh risk. Schizophr Bull. 2007;33(3):682–687. doi: 10.1093/schbul/sbl042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, Parker S, Bentall RP. Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomised controlled trial. Br J Psychiatry. 2004;185:291–297. doi: 10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- Morrison AP, Stewart SL, French P, Bentall RP, Birchwood M, Byrne R, Davies LM, Fowler D, Gumley AI, Jones PB, Lewis SW, Murray GK, Patterson P, Dunn G. Early detection and intervention evaluation for people at high-risk of psychosis-2 (EDIE-2): trial rationale, design and baseline characteristics. Early Interv Psychiatry. 2011;5(1):24–32. doi: 10.1111/j.1751-7893.2010.00254.x. [DOI] [PubMed] [Google Scholar]
- Oyserman D, Lee SW. Does culture influence what and how we think? Effects of priming individualism and collectivism. Psychol Bull. 2008;134(2):311–342. doi: 10.1037/0033-2909.134.2.311. [DOI] [PubMed] [Google Scholar]
- Phillips LJ, Leicester SB, O’Dwyer LE, Francey SM, Koutsogiannis J, Abdel-Baki A, Kelly D, Jones S, Vay C, Yung AR, McGorry PD. The PACE Clinic: identification and management of young people at “ultra” high risk of psychosis. J Psychiatr Pract. 2002;8(5):255–269. doi: 10.1097/00131746-200209000-00002. [DOI] [PubMed] [Google Scholar]
- Phillips LJ, McGorry PD, Yuen HP, Ward J, Donovan K, Kelly D, Francey SM, Yung AR. Medium term follow-up of a randomized controlled trial of interventions for young people at ultra high risk of psychosis. Schizophr Res. 2007;96(1–3):25–33. doi: 10.1016/j.schres.2007.05.018. [DOI] [PubMed] [Google Scholar]
- Piskulic D, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, McGlashan TH. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res. 2012;196(2–3):220–224. doi: 10.1016/j.psychres.2012.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raballo A, Laroi F. Psychosis risk syndrome and DSM-5: time for a dimensional approach to at-risk mental states? Clin Schizophr Relat Psychoses. 2011;5(3):155–158. doi: 10.3371/CSRP.5.3.6. [DOI] [PubMed] [Google Scholar]
- Rietdijk J, Klaassen R, Ising H, Dragt S, Nieman DH, van de Kamp J, Cuijpers P, Linszen D, van der Gaag M. Detection of people at risk of developing a first psychosis: comparison of two recruitment strategies. Acta Psychiatr Scand. 2012;126(1):21–30. doi: 10.1111/j.1600-0447.2012.01839.x. [DOI] [PubMed] [Google Scholar]
- Ruhrmann S, Schultze-Lutter F, Maier W, Klosterkotter J. Pharmacological intervention in the initial prodromal phase of psychosis. Eur Psychiatry. 2005;20(1):1–6. doi: 10.1016/j.eurpsy.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Ruhrmann S, Schultze-Lutter F, Salokangas RK, Heinimaa M, Linszen D, Dingemans P, Birchwood M, Patterson P, Juckel G, Heinz A, Morrison A, Lewis S, von Reventlow HG, Klosterkotter J. Prediction of psychosis in adolescents and young adults at high risk: results from the prospective European prediction of psychosis study. Arch Gen Psychiatry. 2009;67(3):241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- Salokangas RK, Ruhrmann S, von Reventlow HG, Heinimaa M, Svirskis T, From T, Luutonen S, Juckel G, Linszen D, Dingemans P, Birchwood M, Patterson P, Schultze-Lutter F, Klosterkotter J. Axis I diagnoses and transition to psychosis in clinical high-risk patients EPOS project: prospective follow-up of 245 clinical high-risk outpatients in four countries. Schizophr Res. 2012;138(2–3):192–197. doi: 10.1016/j.schres.2012.03.008. [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter F, Ruhrmann S, Berning J, Maier W, Klosterkotter J. Basic symptoms and ultrahigh risk criteria: symptom development in the initial prodromal state. Schizophr Bull. 2010;36(1):182–191. doi: 10.1093/schbul/sbn072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidman LJ, Giuliano AJ, Meyer EC, Addington J, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, Woods SW, Bearden CE, Christensen BK, Hawkins K, Heaton R, Keefe RS, Heinssen R, Cornblatt BA. Neuropsychology of the prodrome to psychosis in the NAPLS consortium: relationship to family history and conversion to psychosis. Arch Gen Psychiatry. 2010;67(6):578–588. doi: 10.1001/archgenpsychiatry.2010.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon AE, Dvorsky DN, Boesch J, Roth B, Isler E, Schueler P, Petralli C, Umbricht D. Defining subjects at risk for psychosis: a comparison of two approaches. Schizophr Res. 2006;81(1):83–90. doi: 10.1016/j.schres.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Simon AE, Umbricht D. High remission rates from an initial ultra-high risk state for psychosis. Schizophr Res. 2010;116(2–3):168–172. doi: 10.1016/j.schres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- van Rijn S, Aleman A, de Sonneville L, Sprong M, Ziermans T, Schothorst P, van Engeland H, Swaab H. Neuroendocrine markers of high risk for psychosis: salivary testosterone in adolescent boys with prodromal symptoms. Psychol Med. 2011;41(9):1815–1822. doi: 10.1017/S0033291710002576. [DOI] [PubMed] [Google Scholar]
- Woods SW, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, McGlashan TH. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009;35(5):894–908. doi: 10.1093/schbul/sbp027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YP, Shen DY, Wang JY, Yang J. The reliability and validity of PDQ-4+ in China. Chin J Clin Psychol. 2002;10:165–168. [Google Scholar]
- Yung AR, Buckby JA, Cosgrave EM, Killackey EJ, Baker K, Cotton SM, McGorry PD. Association between psychotic experiences and depression in a clinical sample over 6 months. Schizophr Res. 2007a;91(1–3):246–253. doi: 10.1016/j.schres.2006.11.026. [DOI] [PubMed] [Google Scholar]
- Yung AR, McGorry PD, Francey SM, Nelson B, Baker K, Phillips LJ, Berger G, Amminger GP. PACE: a specialised service for young people at risk of psychotic disorders. Med J Aust. 2007b;187(7 Suppl):S43–46. doi: 10.5694/j.1326-5377.2007.tb01336.x. [DOI] [PubMed] [Google Scholar]
- Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC, Rakkar A. Monitoring and care of young people at incipient risk of psychosis. Schizophr Bull. 1996;22(2):283–303. doi: 10.1093/schbul/22.2.283. [DOI] [PubMed] [Google Scholar]
- Yung AR, Nelson B, Stanford C, Simmons MB, Cosgrave EM, Killackey E, Phillips LJ, Bechdolf A, Buckby J, McGorry PD. Validation of “prodromal” criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophr Res. 2008;105(1–3):10–17. doi: 10.1016/j.schres.2008.07.012. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, McGorry PD, McFarlane CA, Francey S, Harrigan S, Patton GC, Jackson HJ. Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br J Psychiatry Suppl. 1998;172(33):14–20. [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004;67(2–3):131–142. doi: 10.1016/S0920-9964(03)00192-0. [DOI] [PubMed] [Google Scholar]
- Yung AR, Stanford C, Cosgrave E, Killackey E, Phillips L, Nelson B, McGorry PD. Testing the Ultra High Risk (prodromal) criteria for the prediction of psychosis in a clinical sample of young people. Schizophr Res. 2006;84(1):57–66. doi: 10.1016/j.schres.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell’Olio M, Francey SM, Cosgrave EM, Killackey E, Stanford C, Godfrey K, Buckby J. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39(11–12):964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]
- Zhang T, Chow A, Wang L, Dai Y, Xiao Z. Role of childhood traumatic experience in personality disorders in China. Compr Psychiatry. 2012a;53(6):829–836. doi: 10.1016/j.comppsych.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T, Wang L, Good MJ, Good BJ, Chow A, Dai Y, Yu J, Zhang H, Xiao Z. Prevalence of personality disorders using two diagnostic systems in psychiatric outpatients in Shanghai, China: a comparison of uni-axial and multi-axial formulation. Soc Psychiatry Psychiatr Epidemiol. 2012b;47(9):1409–1417. doi: 10.1007/s00127-011-0445-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng L, Wang J, Zhang T, Li H, Li C, Jiang K. The Chinese version of the SIPS/SOPS: a pilot study of reliability and validity. Chinese Mental Health Journal. 2012;26(8):571–576. [Google Scholar]