Abstract
Background:
A recent study indicates that the incidence of smoking cessation varies with age. Although nicotine dependence (ND) has been regarded as one of the most significant barriers of successful smoking cessation, few researches have focused on the relationship between nicotine dependence and age.
Methods:
A cross-sectional study (conducted in 2013) with 596 Chinese rural male current smokers was performed to study the relationship between ND and age. The ND level was assessed using the Fagerström Test for Nicotine Dependence (FTND) scale. The univariate two-degree fractional polynomials (FPs) regression was used to explore the relation of ND to age.
Results:
The mean of FTND scores in the middle-aged group (45–64 yr old) was higher than that in the younger (<45 yr old) and older groups (≥65 yr old). The FPs regression showed an inverse U-shaped relationship between ND and age.
Conclusion:
The middle-aged current smokers had higher degree of ND than the younger and the older groups, which showed an inverse U-shaped relationship between ND and age. This finding needs to be confirmed by further researches.
Keywords: Age, Nicotine dependence, Smoking, Tobacco, China
Introduction
Tobacco use remains to be the leading cause of preventable death around the world (1). It is associated with an increased risk of various diseases, including respiratory problems, cardiovascular disorders and cancers (2, 3). Being the key determinant of tobacco addiction, nicotine dependence (ND) is one of the major barriers of successful smoking cessation (4–6). The incidence of smoking cessation varies with age (7). The quitting ratio in young (21–31 years old) and old (51–60 years old) adults appears to be greater than that in middle aged (31–50 years old) group. Previous studies conducted in South Korea (8) and China (9) demonstrate that ND has an inverse U-shaped relationship with age, with the peak at 50 years of age. That supports and may partially account for what underlies the cessation-age trend found by Fidler et al. (7).
However, the number of studies on the relationship between ND and age is very limited. Furthermore, almost all participants in previous researches live in cities. Many characteristics such as income, occupation, educational etc. are different between urban and rural dwellers (10–12). Therefore, that whether the above-mentioned cessation-age trend is suitable for the rural residents needs to be further explored.
In this study, we used Fagerström Test for Nicotine Dependence (FTND) to assess the degree of ND among rural male current smokers in China and investigated the relationship between ND and age, which will provide evidence needed to better-informed education for tobacco control intervention.
Materials and Methods
Related definitions
According to the WHO (13), some definitions are as follows. Smokers: Those who have/had smoked 100 or more cigarettes (or the equivalent amount of tobacco) during their lifetime. Current smokers: Those who meet the criterion of smokers, and smoke any tobacco product at the time of the survey. Current daily smokers: Those who meet the criterion of smokers, and smoke at least once a day at the time of the survey. Current occasional smokers: Those who meet the criterion of smokers, and smoke but not every day at the time of the survey. Ex-smokers: Those who meet the criterion of smokers, but do not smoke at all at the time of the survey.
Subjects
This cross-sectional study was conducted from April to May, 2013, among persons residing in 17 villages of three counties (Pingyin, Junan, and Liangshan) in Shandong, China. Male persons aged 18 years or more and ever spontaneous quitted smoking was face-to-face interviewed by the well-trained investigators to complete a questionnaire that was designed based on the Global Adult Tobacco Survey (GATS) Core Questionnaire with Optional Questions. The total amount of valid questionnaires was 1429, among which, 596 were for current smokers (including 509 for current daily smokers and 87 for current occasional smokers) and 833 were for ex-smokers.
In this analysis, the 596 current smokers were included. This study was approved by the Ethics Review Committee of Shandong University and all subjects provided informed consent.
Measure of nicotine dependence
Participants’ level of ND was assessed using the fagerström test for nicotine dependence (FTND) scale (14), which measured both physical and psychological tobacco dependence (15). This FTND scale consists of six items. The total scores range from 0 to 10, with higher scores showing greater dependence. The total scale showed good internal consistency reliability in this study (Cronbach’s alpha=0.689).
Statistical analysis
The frequency and percent of categorical variables, as well as the mean and standard deviation of metric variables were calculated to describe the demographic characteristics of participants. If the variance between groups was homogeneous, one-way analysis of variance was used to test the difference of means of metric variables between groups; otherwise, the Kruskal-Wallis equality-of-populations rank test was used. Multiple linear regression was performed to adjust for the potential confounders. The adjusted means of the analyzed independent variables were calculated at the means of the other covariates. The association of FTND scores with age was analyzed using univariate two-degree fractional polynomials (FPs) regression model, whose best power was chosen from candidates: −2, −1, −0.5, 0, 0.5, 1, 2, 3 (16, 17). The best model is that with the lowest deviance. All statistical analyses were carried out using STATA version 13.1 (Stata Corporation, College Station, TX, USA). All reported probabilities (P-value) were two-sided, and that less than 0.05 were considered statistically significant.
Results
Subjects Characteristics
The age of subjects ranged from 23 to 80 years old, with an average of 55.08 years. Totally, 444 (74.50%) participants were engaged in farming work. Overall, 378 (63.42%) participants had a middle level of education (primary and middle school). The mean of pack-year was 26.824±22.450. The mean of FTND scores was 3.062±2.589. Other characteristics of the subjects are presented in Table 1.
Table 1:
The characteristics of the subjects
| Variable | Current smokers (n=596) |
|---|---|
| Age (year) | 55.077 ± 12.177 |
| Age group (young/middle/old) | 115(19.30) / 345(57.89) / 136(22.82) |
| FTND score | 3.062 ± 2.589 |
| Occupation (farmer/others) | 444(74.50) / 152(25.50) |
| Marital status (married/unmarried/others) | 562(94.30) / 5(0.84) / 29(4.87) |
| Education (low/middle/high) | 119(19.97) / 378(63.42) / 99(16.61) |
| Age of smoking onset (year) | 22.210 ± 6.702 |
| CPD | 17.068 ± 12.297 |
| Pack-year | 26.824 ± 22.450 |
| Smoking duration (year) | 31.346 ± 12.660 |
Note: Values are expressed as mean ± SD or frequency (%). Age group: young=age <45, middle=45≤age <65, old=age≥65. FTND: Fagerström Test of Nicotine Dependence. Education: low=below primary school, middle = primary and middle school, high= high school or more. CPD: cigarettes per day. Pack-year=CPD/20× number of years smoked
Relationship between nicotine dependence and age
The FTND scores in different age groups (the mean ± SD in <45, 45–64, and ≥65 years of age were 2.522 ± 2.429, 3.281 ± 2.663, and 2.963 ± 2.472, respectively) analyzed using one-way analysis of variance were significant (P=0.021) with the biggest in 45–64 age group.
Multiple linear regression, with FTND score as dependent variable, age as independent variable, and potential confounders including categorical variables of occupation, marital status, educational level and metric variables of tertiles of smoking duration and age of smoking onset as the covariates, showed that the adjusted FTND scores in different age groups (the adjusted mean ± SE in <45, 45–64, and ≥65 years of age were 3.033 ± 0.317, 3.257 ± 0.138, and 2.592 ± 0.284, respectively) were no longer significant (P=0.068), but the distributional trend of the FTND scores in different age groups was just similar to that before the adjustment. We used univariate two-degree FPs regression to explore the relation of ND to age. The best FPs model was that with the powers of 0.5 and 1, which showed an inverse U-shaped association of ND with age. After adjusting for the above-mentioned potential confounders, the results were not altered significantly (Table 2 & Fig. 1).
Table 2:
The relation of FTND score to age estimated by FPs with powers of 0.5 and 1
| Variables | β | SE | t | P | 95%CI | |
|---|---|---|---|---|---|---|
| Age (yr) | ||||||
| 1 | 4.591 | 1.632 | 2.813 | 0.005 | 1.385 | 7.796 |
| 2 | −0.339 | 0.114 | −2.959 | 0.003 | −0.564 | −0.114 |
| Marital status | ||||||
| Unmarried | 0.090 | 1.146 | 0.079 | 0.937 | −2.160 | 2.341 |
| Others | −0.407 | 0.503 | −0.808 | 0.420 | −1.395 | 0.582 |
| Occupation | −0.427 | 0.258 | −1.652 | 0.099 | −0.934 | 0.081 |
| Education | ||||||
| Middle | −0.041 | 0.285 | −0.143 | 0.887 | −0.600 | 0.519 |
| High | 0.335 | 0.373 | 0.900 | 0.368 | −0.396 | 1.067 |
| Smoking duration | 0.665 | 0.249 | 2.674 | 0.008 | 0.177 | 1.154 |
| Age of smoking onset | −0.166 | 0.162 | −1.021 | 0.308 | −0.485 | 0.153 |
| Constant | −13.046 | 5.842 | −2.233 | 0.026 | −24.519 | −1.572 |
Notes: FTND: score for Fagerström Test of Nicotine Dependence; FPs: fractional polynomials regression; Education: middle = primary and middle school, high = high school or more.
Fig. 1:
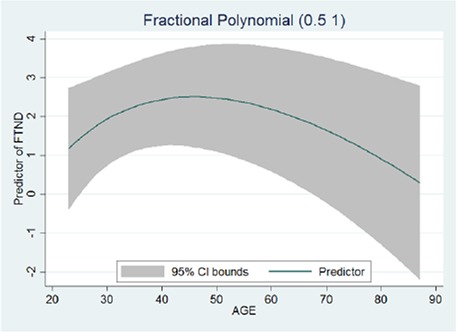
The adjusted curve of relation of FTND score to age estimated by the univariate two-degree fractional polynomials regression with the best-fit powers (0.5, 1). FTND: Fagerström test of nicotine dependence. CI: confidence interval. Adjusting for occupation, marital status, education, smoking duration, and age of smoking onset
In our study, we also analyzed the effects of age on cigarettes per day (CPD) and pack-year. Results were just similar to the relationship between ND and age (data not show).
Discussion
Our study indicated that ND level in the middle aged Chinese rural current smokers was significantly higher than that in the younger and the older, which showed an inverse U-shaped association. This is consistent with the previous studies conducted in the urban population (8, 9).
The definite mechanism of the aforementioned relationship between ND and age is not fully understood. Desensitization of nicotinic receptors and effects of psychosocial factors are probably the primary drivers. Data demonstrate that the availability of the central nicotinic cholinergic receptor could decline significantly with age (18, 19). Desensitization of nicotinic cholinergic receptors due to the long time exposure to nicotine will result in the onset of the symptoms of craving or withdrawal of smoking (2). Therefore, in order to alleviate the craving or avoid torturous withdrawal symptoms, smokers have to use more and more tobacco products to maintain the comparatively high level of plasma nicotine and the sufficient binding ratio of nicotinic receptors, which will aggravate continuously the severity of dependence (20). In addition, middle-aged smokers are facing more smoking-related cues from their surroundings than other age groups, such as specific moods (delighted or depressed emotion, enormous pressures of life and work), initiation of social interaction, situations (working with colleagues, dining together, drinking, driving or being with smoking friends), etc. Those could reinforce their psychological dependence on nicotine (6, 21–23). Furthermore, comparing with the middle-aged group, younger smokers (<45 years) have higher perceived self-efficacy for quitting and older smokers are less likely to be reactive to psychological cues for the desire to smoke (24, 25).
There may be also a variety of factors associated with the descending tendency of ND among the older smokers. Firstly, total clearance of nicotine is decreased by 23%, and renal clearance decreased by 49% in the elderly (age>65 years) compared to young adults (26). As the speed of delivering nicotine to the brain is slow in elderly, lower nicotine metabolism contributes to reduce their urge to smoke, which resulted in decreasing tobacco consumption and the level of ND (2, 26). Secondly, owing to the age-related decline in physical function, illness or fear of being ill make the older smokers be more careful about their physical conditions than other age groups (21). They, especially those who are suffering from some serious smoking-caused diseases, may spontaneously reduce their daily intake of nicotine from cigarettes and attempt to quit smoking (27–29). Finally, the descending tendency appears due to the survivorship bias brought by the higher death rate among heavier smokers. Smokers with higher ND level have an increased susceptibility to dying at younger age than lighter or non-smokers (30, 31). All smoking-induced excess mortality increases with age (32), thus resulting probably in leaving individuals with lower ND in the older group.
Several potential limitations of our study should be considered while interpreting the results. Firstly, our results are based on a relatively small sample. Secondly, since ND has a complex etiology generated by many factors, other uninvestigated potential confounders may alter the results. Finally, this was only a cross-sectional study, some biases, e.g. selected and recalls bias, might exist and could distort the results.
Conclusion
The middle-aged current smokers had higher degree of ND than the younger and the older groups, which showed an inverse U-shaped relationship between ND and age. This finding needs to be confirmed by further researches.
Ethical Considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgments
This study is sponsored by a grant from the National Natural Science Foundation of China (No: 81273150). We thank the local Health Bureau, local Center for Disease Control and Prevention, other relevant governments and persons, the investigators, and respondents for their support to this research. The authors declare that there is no conflict of interests.
Reference
- 1. World Health Organization (2013). WHO report on the global tobacco epidemic, 2013: enforcing bans on tobacco advertising, promotion and sponsorship. WHO, Geneva, Available from: http://apps.who.int/iris/bitstream/10665/85380/1/9789241505871_eng.pdf?ua=1 [Google Scholar]
- 2. Benowitz NL. (2010). Nicotine addiction. New Engl J Med, 362( 24), 2295. 10.1056/NEJMra0809890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nilsson S, Carstensen JM, Pershagen G. (2001). Mortality among male and female smokers in Sweden: a 33 year follow up. J Epidemiol Community Health, 55( 11), 825–830. 10.1136/jech.55.11.825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Asfar T, Weg MV, Maziak W, et al. (2008). Outcomes and adherence in Syria’s first smoking cessation trial. Am J Health Behav, 32( 2), 146–156. 10.5993/AJHB.32.2.4 [DOI] [PubMed] [Google Scholar]
- 5. Hagimoto A, Nakamura M, Morita T, et al. (2010). Smoking cessation patterns and predictors of quitting smoking among the Japanese general population: a 1-year follow-up study. Addiction, 105( 1), 164–173. 10.1111/j.1360-0443.2009.02735.x [DOI] [PubMed] [Google Scholar]
- 6. Gruder CL, Trinidad DR, Palmer PH, et al. (2013). Tobacco smoking, quitting, and relapsing among adult males in Mainland China: The China seven cities study. Nicotine Tob Res, 15( 1), 223–230. 10.1093/ntr/nts116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fidler J, Ferguson SG, Brown J, et al. (2013). How does rate of smoking cessation vary by age, gender and social grade? Findings from a population survey in England. Addiction. 10.1111/add.12241 [DOI] [PubMed] [Google Scholar]
- 8. Park S, Lee JY, Song TM, et al. (2012). Age-associated changes in nicotine dependence. Public Health, 126( 6), 482–489. 10.1016/j.puhe.2012.02.007 [DOI] [PubMed] [Google Scholar]
- 9. Chen J, Cui Z, Li C, et al. (2012). Relationships between nicotine dependence and age-associated factors. Chinese J Health Educ, 28( 10), 802–805. [Google Scholar]
- 10. Reid JL, Hammond D, Boudreau C, et al. (2010). Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res, 12( suppl 1), S20–S33. 10.1093/ntr/ntq051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wu J, Yang T, Rockett IR, et al. (2011). Nicotine dependence among rural-urban migrants in China. BMC public health, 11( 1), 296. 10.1186/1471-2458-11-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yang T, Abdullah ASM, Mustafa J, et al. (2009). Factors associated with smoking cessation among Chinese adults in rural China. Am J Health Behav, 33( 2), 125–134. 10.5993/AJHB.33.2.2 [DOI] [PubMed] [Google Scholar]
- 13. World Health Organization (1998). Guidelines for controlling and monitoring the tobacco epidemic. WHO, Geneva, Available from http://apps.who.int/bookorders/anglais/detart1.jsp?sesslan=1&codlan=1&codcol=15&codcch=468# [Google Scholar]
- 14. Heatherton TF, Kozlowski LT, Frecker RC, et al. (1991). The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict, 86( 9), 1119–1127. [DOI] [PubMed] [Google Scholar]
- 15. Dijkstra A, Tromp D. (2002). Is the FTND a measure of physical as well as psychological tobacco dependence? J Subst Abus Treat, 23( 4), 367–374. 10.1016/S0740-5472(02)00300-8 [DOI] [PubMed] [Google Scholar]
- 16. Royston P, Altman DG. (1994). Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling. Applied Statistics, 429–467. 10.2307/2986270 [DOI] [Google Scholar]
- 17. Royston P, Ambler G, Sauerbrei W. (1999). The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol, 28( 5), 964–974. 10.1093/ije/28.5.964 [DOI] [PubMed] [Google Scholar]
- 18. Mitsis EM, Cosgrove KP, Staley JK, et al. (2009). Age-related decline in nicotinic receptor availability with [< sup> 123</sup> I] 5-IA-85380 SPECT. Neurobiol of aging, 30( 9), 1490–1497. 10.1016/j.neurobiolaging.2007.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang H, Sun X. (2005). Desensitized nicotinic receptors in brain. Brain Res Rev, 48( 3), 420–437. 10.1016/j.brainresrev.2004.09.003 [DOI] [PubMed] [Google Scholar]
- 20. Brody AL, Mandelkern MA, London ED, et al. (2006). Cigarette Smoking Saturates Brain {alpha} 4beta2 Nicotinic Acetylcholine Receptors. Arch Gen Psychiat, 63( 8), 907. 10.1001/archpsyc.63.8.907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim SS, Son H, Nam KA. (2005). Personal factors influencing Korean American men’s smoking behavior: addiction, health, and age. Arch Psychiat Nurs, 19( 1), 35–41. 10.1016/j.apnu.2004.11.005 [DOI] [PubMed] [Google Scholar]
- 22. Chu C, Zhang L, Yang C. (2010). Effects of social-psychological factors on smoking behavior in male adults Chinese J Public Health, 2010; 7: 026. [Google Scholar]
- 23. Jayakrishnan R, Mathew A, Lekshmi K, et al. (2012). Assessment of Nicotine Dependence among Smokers in a Selected Rural Population in Kerala, India. Asian Pac J Cancer Prev, 13( 6), 2663–2667. 10.7314/APJCP.2012.13.6.2663 [DOI] [PubMed] [Google Scholar]
- 24. Ma GX, Fang CY, Knauer CA, et al. (2006). Tobacco dependence, risk perceptions and self-efficacy among Korean American smokers. Addictive behaviors, 31( 10), 1776–1784. 10.1016/j.addbeh.2005.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tsai Y-W, Wen Y-W, Tsai C-R, et al. (2009). Peer pressure, psychological distress and the urge to smoke. Int J Environ Res Public Health, 6( 6), 1799–1811. 10.3390/ijerph6061799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Benowitz NL, Hukkanen J, Jacob P., III (2009). Nicotine chemistry, metabolism, kinetics and biomarkers Handb Exp Pharmacol, ( 192), 29–60. 10.1007/978-3-540-69248-5_2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Allen SC. (2009). Tobacco smoking in older people. Rev Clin Gerontol, 19( 03), 185–192. 10.1017/S0959259809990256 [DOI] [Google Scholar]
- 28. Qian J, Cai M, Gao J, et al. (2010). Trends in smoking and quitting in China from 1993 to 2003: National Health Service Survey data. Bull World Health Organ, 88( 10), 769–776. 10.2471/BLT.09.064709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lugo A, La Vecchia C, Boccia S, et al. (2013). Patterns of Smoking Prevalence among the Elderly in Europe. Int J Environ Res Public Health, 10( 9), 4418–4431. 10.3390/ijerph10094418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. John U, Hanke M. (2003). Tobacco- and alcohol-attributable mortality and years of potential life lost in Germany. Eur J Public Health, 13( 3), 275–277. 10.1093/eurpub/13.3.275 [DOI] [PubMed] [Google Scholar]
- 31. Doll R, Peto R, Boreham J, et al. (2004). Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ, 328( 7455), 1519. 10.1136/bmj.38142.554479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gellert C, Schöttker B, Brenner H. (2012). Smoking and All-Cause Mortality in Older PeopleSystematic Review and Meta-analysis. Arch Intern Med, 172( 11), 837–844. 10.1001/archinternmed.2012.1397 [DOI] [PubMed] [Google Scholar]


