We report 2 brothers who presented at young age with multiple lacunar strokes, inflammatory skin rash, and a range of neurologic symptoms.
Case reports.
Patient 1 had a history of premature birth, congenital chylothorax, splenomegaly, and chronic anemia post Epstein-Barr virus infection. At age 3 years, he had an episode of lowered consciousness, behavioral regression, and ataxia, with spontaneous recovery within 24 hours. At age 8 years, he experienced speech disturbances, disorientation, left-sided sixth nerve palsy, and right-sided hemiparesis with total recovery after 1 week. MRI revealed a hyperintense lesion in the ventrolateral thalamus, consistent with lacunar infarction (figure, A and B). Magnetic resonance angiography results were normal. On his 11th birthday, he was admitted to the hospital with nausea, vertigo, right-sided hearing loss, and nystagmus. Further clinical details are lacking. The episode was interpreted as labyrinthitis. Repeated MRI showed no new abnormalities. Right-sided hearing loss persisted. A new ischemic left-sided lacunar pontine infarct caused a sixth nerve palsy at age 17 years. Two years later, he developed acute left-sided ptosis, without other abnormalities on physical examination or new imaging findings, which almost completely recovered within 1 month. Ancillary investigations over the years failed to reveal a cardioembolic source or prothrombotic condition. CSF showed an increased leukocyte count. In addition, since 4 years of age, he episodically experienced non-itching red noduli and maculae over his face, arms, and lower legs (figure, D). Skin biopsies revealed deep-reaching angiocentric lymphohistiocytic inflammatory infiltrates, consistent with polyarteritis nodosa (figure, E–G). Immunologic analysis showed no evidence of systemic vasculitis.
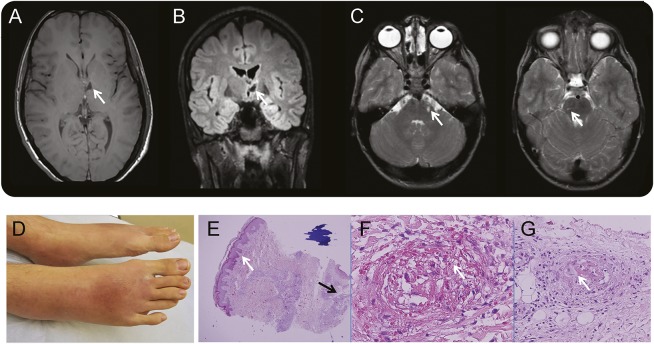
Figure. Clinical features in 2 brothers with adenosine deaminase 2 deficiency.
3T T1-weighted (A) and fluid-attenuated inversion recovery (B) MRI of patient 1, performed at age 21 years, show thalamic infarction (arrows). (C) 1.5T T2-weighted MRI of patient 2 performed at age 7 years with arrows indicating left and right lacunar pontine infarcts. (D) Bilateral erythematous swelling of both feet at age 21 years. (E–G) Hematoxylin & eosin stain of skin biopsy of foot with intact epidermis (E, white arrow) and including subcutaneous fat (E, black arrow) reveals necrotizing vasculitis with necrosis (arrow in F) and multiple thrombi and fibrin (arrow in G).
His younger brother, patient 2, was diagnosed with autism and attention-deficit/hyperactivity disorder. He experienced an acute episode with inability to stand and walk with exotropia of the right eye at age 2 years, without CT abnormalities. All symptoms, except strabismus, resolved within 24 hours. At age 7 years, a partial nasal visual field defect of the right eye and a right-sided optic nerve atrophy were diagnosed. Subsequent MRI of the brain revealed 3 old lacunar infarcts in the pons and left internal capsule (figure, C). He was admitted at age 9 years because of an acute episode with vertigo, nausea and vomiting, nystagmus, and an inability to abduct the right eye. At that time, a red skin rash was noticed, which he had had more often in the past. Extensive laboratory investigations revealed a mildly elevated CSF cell count. MRI revealed no new lesions. No cardioembolic, prothrombotic, or metabolic abnormalities were found. This episode was at that time interpreted as vestibular neuritis. He did not experience new events in the past 11 years.
Both parents are healthy. The mother experienced one epileptic seizure as an adult without known cause and migraine is common in both families. The father's father died at age 66 years due to hemorrhagic stroke.
The remarkable medical history of both siblings, including multiple lacunar strokes at young age in association with the inflammatory skin lesions, prompted genetic testing for mutations in the CECR1 gene that were recently described in patients with deficiency of adenosine deaminase 2 (ADA2). Sanger sequencing of all 10 exons of CECR1 revealed that both patients were homozygous for the previously described pathogenic mutation p.Arg169Gln (p.R169Q; c.506G>A) variant in the CECR1 gene, encoding ADA2.
Discussion.
Recently, 9 patients were described with ADA2 deficiency, caused by loss of function mutations in the CECR1 gene.1 ADA2 is a secreted growth factor that is important for the development and differentiation of hematopoietic and endothelial cells and maintenance of vascular integrity. Mutations in CECR1 are associated with a range of vascular and inflammatory phenotypes including young-onset ischemic stroke, ophthalmologic involvement, livedo racemosa, hepatosplenomegaly, and a low serum immunoglobulin M. Also, patients were described who met the criteria for polyarteritis nodosa and were homozygous for the p. Gly47Arg mutation, which is associated with highly variable clinical expression, sometimes without neurologic features.2
We report 2 Dutch siblings with a homozygous p.Arg169Gln mutation in CECR1. Their symptoms of early-onset stroke, skin abnormalities, splenomegaly, and ophthalmologic involvement overlap with previously described cases. However, the unexplained early-onset acute episode with ataxia resolving spontaneously, a labyrinthitis-like episode with vertigo and nausea, and the cranial nerve palsies, e.g., acute hearing loss in the eldest brother and optic nerve involvement in the youngest, have not yet been reported.
In patients with unexplained young-onset lacunar stroke accompanied by systemic inflammation and a positive family history suspicious of recessively inherited disease (i.e., affected sibling), ADA2 deficiency needs to be considered in the differential diagnosis.
Footnotes
Author contributions: W.F.W. wrote the manuscript together with P.J.N. and K.P.J.B. I.A., A.E.H., and K.D.L. commented on the manuscript. All authors agreed to the final version.
Study funding: No targeted funding reported.
Disclosure: The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
References
- 1.Zhou Q, Yang D, Ombrello AK, et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med 2014;370:911–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Navon EP, Pierce SB, Segel R, et al. Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N Engl J Med 2014;370:921–931. [DOI] [PubMed] [Google Scholar]