Abstract
Objective
Vaccine against human papillomavirus (HPV) has been offered free of charge to all 12-year-old girls in Norway since 2009. Nevertheless, the uptake of HPV vaccine is lower than for other childhood vaccines. The aim of this study was to examine whether parental education and income are associated with initiation and completion of HPV vaccination.
Design
Nationwide register-based study.
Setting
Publicly funded childhood immunisation programme in Norway.
Participants
91 405 girls born between 1997 and 1999 and registered in the Norwegian Central Population Registry were offered HPV vaccine during the first 3 programme years. Of these, 84 139 had complete information on all variables and were included in the study.
Measurements
Information on HPV-vaccination status was obtained from the Norwegian Immunisation Registry. Data on socioeconomic factors were extracted from Statistics Norway. Risk differences (RDs) and CIs were estimated with Poisson regression.
Results
In the study sample, 78.3% received at least one dose of HPV vaccine and 73.6% received all three doses. High maternal education was significantly associated with lower probability of initiating HPV vaccination (multivariable RD=−5.5% (95% CI −7.0% to −4.0%) for highest compared with lowest education level). In contrast, high maternal income was significantly associated with higher probability of initiating vaccination (multivariable RD=10.1% (95% CI 9.0% to 11.3%) for highest compared with lowest quintile). Paternal education and income showed similar, but weaker, associations. The negative association between education and initiation was only seen for incomes below the median value.
Conclusions
In spite of the presumably equal access to HPV vaccine in Norway, we found socioeconomic disparities in vaccine uptake. More studies are needed to explain the underlying factors responsible for the observed socioeconomic differences. Insight into these factors is necessary to target information and increase vaccination coverage to ultimately reduce HPV-related disease across socioeconomic barriers.
Keywords: EPIDEMIOLOGY, PREVENTIVE MEDICINE, PUBLIC HEALTH
Strengths and limitations of this study.
The strengths of this study include a large sample size. The study is nationwide and includes all girls offered vaccination against human papillomavirus (HPV) during the first 3 years of the publicly funded HPV immunisation programme in Norway.
Individual data on vaccination and socioeconomic factors from different national registries, covering the entire Norwegian population, were linked. This allowed us to study the associations of maternal and paternal education, and income, with the uptake of HPV vaccine, while controlling for numerous possible confounders.
Missing information on parental education and income was disproportionately distributed, with more missing numbers for immigrant parents.
Introduction
Vaccine against human papillomavirus (HPV) was introduced in the Norwegian Childhood Immunisation Programme in 2009. The vaccine is offered through a school-based programme to all 12-year-old girls. The aim is to provide cervical cancer protection to all women and thereby overcome potential socioeconomic differences in cervical cancer incidence. About 50% of cervical cancer cases in Norway arise from the 20% of the population who, for different reasons, do not attend screening.1
The Norwegian healthcare system is built on the principle of equal access to service for all citizens, reflected in the delivery of vaccines in the Childhood Immunisation Programme. All vaccines in the programme, including the HPV vaccine, are offered free of charge within the public health service. The HPV vaccine is given at school, during school hours, by public health nurses, without parents present. Thus, there are no obvious barriers to vaccination, such as cost or access to the programme.
Vaccination coverage is well above 90% for all vaccines in the programme provided during the first 2 years of life. Furthermore, the proportion of 16-year-olds in 2013 (born 1997) who had received all recommended doses, including school age boosters, was 91% for diphtheria vaccine and 94% for vaccine against polio, measles, mumps and rubella.2 The uptake of HPV vaccine has, however, not yet reached the same level as the other childhood vaccines.3 In spite of the presumably equal access to HPV vaccine in Norway, we speculate that socioeconomic disparities in vaccine uptake may still exist. The association between socioeconomic factors and vaccine uptake has not earlier been studied in Norway.
Associations between deprivation and uptake of HPV vaccine have previously been investigated in other countries with publicly funded immunisation programmes.4–9 However, these studies have used aggregates of socioeconomic conditions such as deprivation indices based on postcodes of residence, and results are inconsistent. Population based studies with individual data on socioeconomic factors are few. Moreover, to the best of our knowledge, no previous studies have aimed to assess the associations between specific socioeconomic factors, such as education and income, and the uptake of HPV vaccine. Furthermore, the differential associations of maternal versus paternal education and income are unknown.
We had the unique opportunity to link individual data from several national sources: The Norwegian Central Population Registry, Statistics Norway and the Norwegian Immunisation Registry. This allowed us to estimate the association between specific socioeconomic measures, namely maternal and paternal education and income, and initiation and completion of HPV vaccination, while controlling for a number of possible confounders, in a large cohort comprising all girls offered the HPV vaccine during the 3 first years of the HPV vaccination programme in Norway.
Methods
HPV vaccination programme
The HPV vaccine is offered free of charge in a three-dose schedule to 12-year-old girls during seventh grade. Parents provide consent to vaccination, usually by returning a signed informed consent form to the school nurse. Although the girls do not consent to HPV vaccination themselves, the parents are encouraged to discuss with their daughters and take their views into consideration when deciding whether to consent to HPV vaccination. Each programme year corresponds to an academic year, starting 20 August and ending 20 June the following year. Programme years 1, 2 and 3 included girls born in 1997, 1998 and 1999, respectively. In addition, due to the coinciding of the start of the HPV vaccination programme and the H1N1 influenza pandemic in the autumn of 2009, girls born in 1997 were also offered the vaccine during programme year 2.
Data sources
The Norwegian Central Population Registry was used to define the study population, namely all girls born between 1997 and 1999, residing in Norway as of 31 December 2012, or previously. Information on emigration, immigration or death was also obtained from the Norwegian Central Population Registry.
Dates of HPV vaccinations were extracted from the Norwegian Immunisation Registry on 22 August 2013. Notification to the Norwegian Immunisation Registry of all vaccinations within the childhood immunisation programme is mandatory and does not require consent from either the vaccinated child or the parents. The transfer of data is electronic from the electronic patient journal to the register, thus the register is continuously updated.10
Information on maternal and paternal highest attained education level (as of 31 December 2012), maternal and paternal income in 2011, maternal and paternal employment status in 2012, municipality and county of residence (as of 31 December 2012), country of birth of the girls and their parents, number of siblings and maternal age at birth of daughter, was retrieved from Statistics Norway and includes data from the National Education Data Base and the National Tax Registry. The data in the National Education Database is compiled by Statistics Norway, and is based on information from all schools and institutions of higher education in Norway. Information on education completed abroad is obtained from the Norwegian State Educational Loan Fund and the Health Personnel Register, as well as from surveys among immigrants performed by Statistics Norway, the latest in 2011–2012. The data in the Tax Registry are obtained by Statistics Norway from The Directorate of Taxes. The data from Statistics Norway are updated yearly.
The unique identification number allocated to all Norwegian residents was used to link the national registries.
Outcome variables
The main outcome variable was initiation of HPV vaccination, defined as receipt of at least one dose.
The secondary outcome variable was completion of the HPV-vaccination series, defined as receipt of all three doses with time intervals of at least 30 days between the first and second dose, and at least 90 days between the second and third dose, in accordance with the minimum intervals specified in the Summary of Product Characteristics (SPC) for Gardasil, the vaccine used in Norway. No restrictions on maximum intervals between the doses were applied.
Main exposure variables
Maternal and paternal levels of education were categorised in five groupings: compulsory education (comprising primary and lower secondary education, ≤10 years of schooling), upper secondary levels 1 and 2 (11–12 years of schooling), completed upper secondary education (including tertiary vocational education, 13–14 years of schooling), higher education, undergraduate level (14–17 years of schooling) and higher education, graduate level (≥18 years of schooling).11
Maternal and paternal incomes were each divided into quintiles.
Other covariates
Maternal and paternal employment status was categorised as ‘employed’ (including self-employed) or ‘unemployed’ (including those outside the labour force and those within the labour force who were unemployed).
Country of origin was defined as ‘Norway’ for girls with at least one Norwegian-born parent. Otherwise, country of origin was defined as the girl's country of birth if she was foreign born, or as her mother's country of birth if the girl was born in Norway. Countries of origin other than Norway were grouped into the following categories: Western Europe, Eastern Europe (including former Soviet Republics), Middle East/North Africa, South Asia, East/Southeast Asia, sub-Saharan Africa and America/Oceania (see online supplementary table S1 for list of countries in each category).
Municipality of residence was categorised according to number of inhabitants: rural (<10 000 inhabitants), semiurban (10 000–49 999 inhabitants) and urban (≥50 000 inhabitants).
Maternal age at birth of daughter was categorised as ≤25, 26–30, 31–35 and ≥36 years.
Number of siblings was categorised as 0, 1, 2, 3 and ≥4.
Study sample
A total of 96 692 girls born between 1997 and 1999 were registered in the Norwegian Central Population Registry (figure 1). Dates of immigration, emigration and death were used to determine residency in Norway. Girls who were not residents of Norway during the entire programme year in which their birth cohort was offered HPV vaccination were excluded. A total of 91 405 girls were considered eligible for vaccination in the period.
Figure 1.
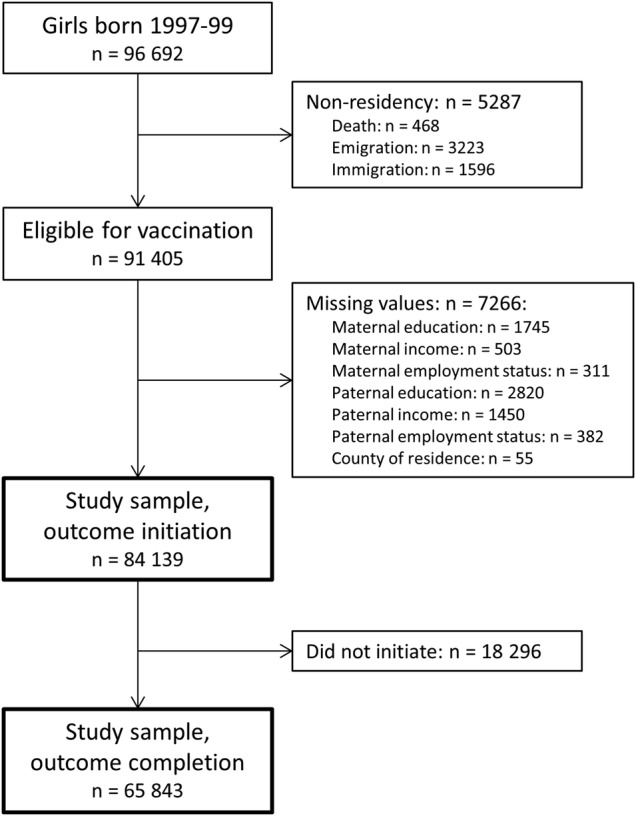
Flow diagram of the study population.
We excluded 7266 girls with missing information on maternal or paternal education, income or employment status, or county of residence (figure 1). The remaining 84 139 girls had complete information on all variables, and were included in analyses with initiation of HPV vaccination as the outcome. Siblings (8.9% of the study sample) were not excluded, since earlier studies have found number of siblings and maternal age at birth of daughter to be associated with HPV vaccination.12 13 In analyses with completion of HPV-vaccination as the outcome, girls who did not initiate vaccination were excluded, leaving 65 843 girls for analyses.
Statistical analysis
We used Poisson regression to estimate risk differences (RDs) and CIs.14 To account for correlation between siblings, we used a robust variance estimator for cluster-correlated data where each cluster contained girls with the same mother.15 The maternal multivariable model (model 1) included maternal education, income and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence and year of birth. In the paternal model (model 2) we removed maternal education, income and employment status, and included paternal education, income and employment status. The covariates other than the main exposures were included because they have previously been reported to be associated with uptake of HPV vaccine.12 We used a Wald test to examine whether the coefficients corresponding to a main variable were simultaneously equal to zero. We examined whether income modified the effect of education, by including interaction terms between education and income (categorised as below or above median income). The interaction terms were evaluated with a Wald test. The same models were used for both initiation and completion of the HPV vaccination schedule as outcomes.
All tests were two sided, and p<0.05 were considered statistically significant. The data were analysed with Stata/SE V.12.1 (StataCorp, College Station, Texas, USA).
Results
Of the 84 139 girls in the study sample, 78.3% initiated HPV vaccination (table 1). Among those who initiated vaccination, 94.1% completed the vaccination series, resulting in a vaccine uptake with three doses of 73.6%. Initiation of HPV vaccination increased from 71.8% among girls in the 1997 birth cohort to 82.6% among girls born in 1999.
Table 1.
Characteristics of the study sample, N=84 139
| n (%) | |
|---|---|
| Vaccine uptake | |
| Initiated HPV vaccination | 65 843 (78.3) |
| Completed HPV vaccination | 61 951 (73.6) |
| Maternal education (years of schooling) | |
| Compulsory (≤10) | 14 803 (17.6) |
| Upper secondary, levels 1 and 2 (11–12) | 6669 (7.9) |
| Upper secondary, completed (13–14) | 26 755 (31.8) |
| Higher, undergraduate level (14–17) | 29 352 (34.9) |
| Higher, graduate level (≥18) | 6560 (7.8) |
| Maternal income (NOK*), median | 396 149 |
| Maternal employment status | |
| Employed | 71 467 (84.9) |
| Unemployed | 12 672 (15.1) |
| Paternal education (years of schooling) | |
| Compulsory (≤10) | 15 716 (18.7) |
| Upper secondary, levels 1 and 2 (11–12) | 6234 (7.4) |
| Upper secondary, completed (13–14) | 34 564 (41.1) |
| Higher, undergraduate level (14–17) | 18 493 (22.0) |
| Higher, graduate level (≥18) | 9132 (10.9) |
| Paternal income (NOK*), median | 525 861 |
| Paternal employment status | |
| Employed | 75 076 (89.2) |
| Unemployed | 9 063 (10.8) |
| Country of origin† | |
| Norway | 77 683 (92.3) |
| Western Europe | 695 (0.8) |
| Eastern Europe | 1 258 (1.5) |
| Middle East/North Africa | 1 417 (1.7) |
| South Asia | 1 426 (1.7) |
| East/Southeast Asia | 689 (0.8) |
| Sub-Saharan Africa | 793 (0.9) |
| America/Oceania | 178 (0.2) |
| Urbanity | |
| Rural (<10 000 inhabitants) | 20 772 (24.7) |
| Semiurban (10 000–49 999 inhabitants) | 35 766 (42.5) |
| Urban (≥50 000 inhabitants) | 27 601 (32.8) |
| Maternal age at birth of daughter (years) | |
| ≤25 | 18 822 (22.4) |
| 26–30 | 31 553 (37.5) |
| 31–35 | 23 967 (28.5) |
| >35 | 9 797 (11.6) |
| Number of siblings | |
| 0 | 3 076 (3.7) |
| 1 | 30 811 (36.6) |
| 2 | 30 507 (36.3) |
| 3 | 12 122 (14.4) |
| ≥4 | 7623 (9.1) |
*NOK=Norwegian kroner (€1 EUR≈8.5 NOK).
†List of countries in each category is supplied in the supplementary table S1.
HPV, human papillomavirus.
The proportion of girls with mothers in the highest education level was 7.8%, whereas 10.9% of the girls had fathers in the highest education level (table 1). Median maternal and paternal income was NOK 396 149 and NOK 525 861, respectively. The proportion of girls with employed mothers was 84.9%, while 89.2% had employed fathers.
Initiation of HPV-vaccination
Girls with mothers in the highest education category were significantly less likely to initiate HPV vaccination as compared to girls whose mothers had only compulsory education (table 2). The difference was small, but when adjusting for maternal income and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence and year of birth, the association was strengthened, RD=−5.5% (95% CI−7.0% to −4.0%), and a clear negative trend was observed.
Table 2.
Initiation of HPV vaccination and RDs according to parental education and income, N=84 139
| Initiated HPV vaccination |
Univariable model |
Multivariable model 1* |
Multivariable model 2† |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | RD | 95% CI | RD | 95% CI | RD | 95% CI | |
| Maternal education (years of schooling) | ||||||||
| Compulsory (≤ 10) | 11 600 | 78.4 | 0 | Ref | 0 | Ref | ||
| Upper secondary, levels 1 and 2 (11–12) | 5174 | 77.6 | −0.8 | −2.0 to 0.5 | −1.7 | −3.0 to −0.4 | ||
| Upper secondary, completed (13–14) | 21 128 | 79.0 | 0.6 | −0.2 to 1.5 | −1.9 | −2.8 to −1.0 | ||
| Higher, undergraduate level (14–17) | 22 907 | 78.0 | −0.3 | −1.2 to 0.5 | −4.1 | −5.1 to −3.1 | ||
| Higher, graduate level (≥18) | 5034 | 76.7 | −1.6 | −2.9 to −0.4 | −5.5 | −7.0 to −4.0 | ||
| p=0.001 | p<0.0001 | |||||||
| Maternal income quintile (NOK)‡ | ||||||||
| 1 (≤278 599) | 12 294 | 73.1 | 0 | Ref | 0 | Ref | ||
| 2 (278 600–361 617) | 13 223 | 78.6 | 5.5 | 4.6 to 6.5 | 5.1 | 4.1 to 6.1 | ||
| 3 (361 620–433 172) | 13 375 | 79.5 | 6.4 | 5.5 to 7.4 | 6.5 | 5.5 to 7.5 | ||
| 4 (433 179–524 224) | 13 433 | 79.8 | 6.8 | 5.8 to 7.7 | 7.8 | 6.7 to 8.8 | ||
| 5 (≥524 242) | 13 518 | 80.3 | 7.3 | 6.3 to 8.2 | 10.1 | 9.0 to 11.3 | ||
| p<0.0001 | p<0.0001 | |||||||
| Paternal education (years of schooling) | ||||||||
| Compulsory (≤10) | 12 374 | 78.7 | 0 | Ref | 0 | Ref | ||
| Upper secondary, levels 1 and 2 (11–12) | 4 840 | 77.6 | −1.1 | −2.4 to 0.2 | −0.6 | −1.9 to 0.6 | ||
| Upper secondary, completed (13–14) | 27 370 | 79.2 | 0.5 | −0.3 to 1.2 | −0.4 | −1.3 to 0.4 | ||
| Higher, undergraduate level (14–17) | 14 214 | 76.9 | −1.9 | −2.8 to −1.0 | −2.5 | −3.5 to −1.5 | ||
| Higher, graduate level (≥18) | 7 045 | 77.1 | −1.6 | −2.7 to −0.5 | −1.4 | −2.6 to −0.1 | ||
| p<0.0001 | p<0.0001 | |||||||
| Paternal income quintile (NOK)‡ | ||||||||
| 1 (≤ 374 466) | 12 867 | 76.5 | 0 | Ref | 0 | Ref | ||
| 2 (374 478–476 519) | 13 207 | 78.5 | 2.0 | 1.1 to 2.9 | 2.0 | 0.9 to 3.0 | ||
| 3 (476 523–585 410) | 13 353 | 79.3 | 2.9 | 2.0 to 3.8 | 3.4 | 2.4 to 4.5 | ||
| 4 (585 412–796 067) | 13 242 | 78.7 | 2.2 | 1.3 to 3.1 | 3.2 | 2.1 to 4.2 | ||
| 5 (≥796 072) | 13 174 | 78.3 | 1.8 | 0.9 to 2.8 | 3.9 | 2.8 to 5.0 | ||
| p<0.0001 | p<0.0001 | |||||||
*This model included maternal income, education and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence and year of birth.
†This model included paternal income, education and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence and year of birth.
‡NOK=Norwegian kroner (€1 EUR≈8.5 NOK).
HPV, human papillomavirus; RD, risk difference.
The proportion of girls initiating vaccination increased with increasing maternal income, from 73.1% in the lowest to 80.3% in the highest income quintile (table 2). The association became stronger after adjustment, and girls with mothers in the highest income quintile had 10.1 percentage points higher probability (95% CI 9.0% to 11.3%) of initiating HPV vaccination as compared to daughters of mothers in the lowest quintile.
Paternal education and income followed patterns similar to maternal education and income, although the associations were weaker and the differences between the groups were smaller (table 2). In the multivariable analysis, having a father with higher education was associated with lower probability of initiating vaccination, multivariable RD=−1.4% (95% CI −2.6% to −0.1%) for highest compared with lowest education level. Furthermore, girls with fathers in the highest income quintile had 3.9 percentage points higher probability (95% CI 2.8% to 5.0%) of initiating vaccination as compared to daughters of fathers in the lowest quintile.
We found significant interaction between maternal education and income, pinteraction<0.0001 (table 3). High education was negatively associated with initiation of HPV vaccination only in girls whose mothers had income below median value, multivariable RD=−11.4% (95% CI −14.7% to −8.0%) for highest compared with lowest education level. Significant interaction was also found between paternal education and income, pinteraction=0.0004, and the association between initiation of HPV vaccination and education was only observed if the father had below median income, multivariable RD=−5.4% (95% CI −8.0% to −2.9%) for highest compared with lowest education level.
Table 3.
Initiation of HPV vaccination and RDs according to parental education by income level, N=84 139
| Income below median value* |
Income above median value* |
|||||||
|---|---|---|---|---|---|---|---|---|
| Initiated HPV vaccination |
Multivariable model† |
Initiated HPV vaccination |
Multivariable model† |
|||||
| n | % | RD | 95% CI | n | % | RD | 95% CI | |
| Maternal education (years of schooling) | ||||||||
| Compulsory (≤10) | 9169 | 77.9 | 0 | Ref | 2431 | 80.1 | 0 | Ref |
| Upper secondary, levels 1 and 2 (11–12) | 3557 | 77.0 | −1.3 | −2.8 to 0.2 | 1 617 | 78.8 | −0.9 | −3.3 to 1.5 |
| Upper secondary, completed (13–14) | 12 452 | 78.0 | −1.3 | −2.4 to −0.2 | 8676 | 80.4 | −0.5 | −2.2 to 1.2 |
| Higher, undergraduate level (14–17) | 6463 | 73.2 | −5.6 | −6.9 to −4.3 | 16 444 | 80.1 | −0.6 | −2.2 to 1.1 |
| Higher, graduate level (≥18) | 588 | 65.7 | −11.4 | −14.7 to −8.0 | 4446 | 78.5 | −1.0 | −2.9 to 0.9 |
| p<0.0001 | p=0.88 | |||||||
| Paternal education (years of schooling) | ||||||||
| Compulsory (≤10) | 9257 | 78.6 | 0 | Ref | 3117 | 79.2 | 0 | Ref |
| Upper secondary, levels 1 and 2 (11–12) | 3170 | 77.5 | −0.5 | −2.0 to 1.1 | 1670 | 78.0 | −0.4 | −2.7 to 1.8 |
| Upper secondary, completed (13–14) | 14 140 | 78.7 | −0.2 | −1.3 to 0.8 | 13 230 | 79.7 | 0.5 | −1.0 to 1.9 |
| Higher, undergraduate level (14–17) | 5103 | 75.4 | −3.1 | −4.5 to −1.8 | 9111 | 77.7 | −0.9 | −2.4 to 0.7 |
| Higher, graduate level (≥18) | 1049 | 72.1 | −5.4 | −8.0 to −2.9 | 5996 | 78.1 | 0.7 | −0.9 to 2.4 |
| p<0.0001 | p=0.054 | |||||||
*Median maternal income=NOK 396 149. Median paternal income=NOK 525 861. NOK=Norwegian kroner (€1 EUR≈8.5 NOK).
†The maternal model included maternal income (categorised as below or above median income), education and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence, year of birth, and interaction terms between maternal education and income. The paternal model included paternal income (categorised as below or above median income), education and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence, year of birth, and interaction terms between paternal education and income.
HPV, human papillomavirus; RD, risk difference.
Mutual adjustment for maternal and paternal education, income and employment status did not change the results (not shown).
Completion of HPV vaccination
We observed weak, but statistically significant positive associations between maternal and paternal education and income, and completion of the three-dose vaccination series in the univariable analyses (table 4). After adjustment, only the association with paternal income remained significant.
Table 4.
Completion of HPV vaccination and RDs according to parental education and income, N=65 843
| Completed HPV vaccination |
Univariable model |
Multivariable model 1* |
Multivariable model 2† |
|||||
|---|---|---|---|---|---|---|---|---|
| n | %‡ | RD | 95% CI | RD | 95% CI | RD | 95% CI | |
| Maternal education (years of schooling) | ||||||||
| Compulsory (≤10) | 10 845 | 93.5 | 0 | Ref | 0 | Ref | ||
| Upper secondary, levels 1 and 2 (11–12) | 4841 | 93.6 | 0.1 | −0.7 to 0.9 | 0.0 | −0.8 to 0.8 | ||
| Upper secondary, completed (13–14) | 19 813 | 93.8 | 0.3 | −0.3 to 0.8 | 0.0 | −0.6 to 0.6 | ||
| Higher, undergraduate level (14–17) | 21 675 | 94.6 | 1.1 | 0.6 to 1.7 | 0.4 | −0.2 to 1.0 | ||
| Higher, graduate level (≥18) | 4777 | 94.9 | 1.4 | 0.6 to 2.2 | 0.0 | −0.9 to 0.9 | ||
| p<0.0001 | p=0.39 | |||||||
| Maternal income quintile (NOK)§ | ||||||||
| 1 (≤278 599) | 11 465 | 93.3 | 0 | Ref | 0 | Ref | ||
| 2 (278 600–361 617) | 12 391 | 93.7 | 0.5 | −0.2 to 1.1 | 0.3 | −0.4 to 0.9 | ||
| 3 (361 620–433 172) | 12 575 | 94.0 | 0.8 | 0.2 to 1.4 | 0.3 | −0.3 to 1.0 | ||
| 4 (433 179–524 224) | 12 691 | 94.5 | 1.2 | 0.6 to 1.8 | 0.6 | −0.1 to 1.2 | ||
| 5 (≥524 242) | 12 829 | 94.9 | 1.6 | 1.1 to 2.2 | 0.6 | −0.1 to 1.2 | ||
| p<0.0001 | p=0.51 | |||||||
| Paternal education (years of schooling) | ||||||||
| Compulsory (≤10) | 11 578 | 93.6 | 0 | Ref | 0 | Ref | ||
| Upper secondary, levels 1 and 2 (11–12) | 4523 | 93.5 | −0.1 | −0.9 to 0.7 | −0.3 | −1.1 to 0.6 | ||
| Upper secondary, completed (13–14) | 25 719 | 94.0 | 0.4 | −0.1 to 0.9 | 0.0 | −0.5 to 0.6 | ||
| Higher, undergraduate (14–17) | 13 438 | 94.5 | 1.0 | 0.4 to 1.5 | 0.1 | −0.6 to 0.7 | ||
| Higher, graduate level (≥18) | 6693 | 95.0 | 1.4 | 0.8 to 2.1 | 0.0 | −0.7 to 0.8 | ||
| p<0.0001 | p=0.96 | |||||||
| Paternal income quintile (NOK)§ | ||||||||
| 1 (≤374 466) | 11 961 | 93.0 | 0 | Ref | 0 | Ref | ||
| 2 (374 478–476 519) | 12 385 | 93.8 | 0.8 | 0.2 to 1.4 | 0.7 | 0.0 to 1.3 | ||
| 3 (476 523–585 410) | 12 600 | 94.4 | 1.4 | 0.8 to 2.0 | 1.1 | 0.4 to 1.8 | ||
| 4 (585 412–796 067) | 12 516 | 94.5 | 1.6 | 1.0 to 2.2 | 1.1 | 0.4 to 1.8 | ||
| 5 (≥796 072) | 12 489 | 94.8 | 1.8 | 1.3 to 2.4 | 0.9 | 0.2 to 1.6 | ||
| p<0.0001 | p=0.01 | |||||||
*This model included maternal income, education and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence and year of birth.
†This model included paternal income, education and employment status, country of origin, urbanity, maternal age at birth of daughter, number of siblings, county of residence and year of birth.
‡Percentage of those who initiated HPV vaccination.
§NOK=Norwegian kroner (€1 EUR≈8.5 NOK).
HPV, human papillomavirus; RD, risk difference.
No interaction was found between maternal education and income (pinteraction=0.59), or between paternal education and income (pinteraction=0.97).
Mutual adjustment for maternal and paternal education, income and employment status did not change the results (not shown).
Discussion
We have assessed parents’ socioeconomic factors in relation to uptake of HPV vaccination in their seventh grade daughters. In spite of the presumably equal access to HPV vaccine in Norway, we found socioeconomic disparities in initiation of the HPV-vaccination series. Overall, maternal income was positively associated with initiation of HPV vaccination, whereas education was negatively associated with initiation of HPV vaccination. Paternal income and education showed similar, but weaker, associations. The association with parental education was restricted to girls with low-income parents. More than 94% of all girls who initiate the HPV-vaccination series complete the schedule and receive all three doses as recommended. Parental socioeconomic status had little influence on completion of the three-dose series.
In our study, maternal income was associated with initiation of HPV vaccination. Studies from publicly funded school-based programmes in Scotland and Canada have reported associations between deprivation and completion of the vaccination series in the routine programme, but not with initiation.5 6 A study from England found no association between deprivation and uptake of HPV vaccine.4 However, the exposure measure in these studies are hardly comparable to ours, as they have used deprivation indices, made up of several dimensions of deprivation and related to post code of residence, as compared to the individual income data in our study.
The negative association observed between maternal education level and initiation of HPV vaccination was weak, but increased after adjustment. Our results are in line with a Canadian study reporting decreased likelihood of HPV vaccination with increasing parental education level in a publicly funded school-based programme.13 The opposite was, however, found in a Swedish study of on-demand HPV vaccination.16 This inconsistency in findings could be explained by differences in vaccine delivery systems, and may suggest that highly educated parents make more active choices on whether to vaccinate their daughters or not, as compared to parents at lower education levels. Highly educated parents have earlier been reported to have more negative attitudes towards vaccines in general than less educated parents.17
Maternal education and income were more strongly associated with initiation of HPV vaccination than paternal education and income. This is in line with previous Swedish results.16 We are, however, unable to draw conclusions on whether these findings reflect that underlying maternal factors in general are more important than paternal in deciding about HPV vaccination based on the data in our study.
Several factors, including maternal health-related beliefs, attitudes and sociopsychological factors as well as knowledge of HPV, safety concerns and media reports, have been reported by others to be important determinants for mothers’ decisions to vaccinate daughters against HPV.13 18–20 Extensive media attention and debate among central health officials, disputing the effectiveness and safety of the vaccine, preceded the implementation of the HPV vaccination programme in Norway.21–23 In addition to the influenza pandemic and pandemic vaccination coinciding with the start of the HPV vaccination programme, this public debate may be a possible explanation why the uptake of HPV vaccine was off to a low start in the first vaccinated birth cohort. The controversy was especially pronounced in the county of Sør-Trøndelag,24 where the lowest uptake of HPV vaccine was observed.25 One might also hypothesise that this debate may have influenced the parental opinion on HPV vaccination selectively. More highly educated mothers may have followed the debate more closely and thereby been more reluctant to vaccinate their daughters than less educated mothers. However, the current data set does not enable assessment of parental beliefs or attitudes.
The negative association between maternal education level and initiation of HPV vaccination was only seen in daughters of mothers with income below median value. This finding is hard to explain. However, we speculate that highly educated mothers with low incomes are more likely to work part-time than highly educated mothers with high income. The same underlying factors may influence both the choice to work part-time and the attitudes towards HPV vaccination. We have no available data on part-time work in our study population. However, about 30% of all employed women in the age group 30–54 in Norway are working part-time.26 Our results may suggest that higher income mothers have a greater awareness of cervical cancer or less scepticism about HPV vaccination than lower income mothers, regardless of education level.
The HPV vaccination programme in Norway is publicly funded, and the vaccine is provided at school during school hours. It was therefore surprising to find that maternal income was positively related to the uptake of HPV vaccine. The inverse association between maternal education level and initiation of HPV vaccination is also interesting. There are generally limited wage differences according to education level in Norway.27 This is reflected in the moderate correlation we observed between education and income (Spearman's correlation coefficient 0.47 and 0.41, for mothers and fathers, respectively). It seems likely that different underlying mechanisms explain the findings on education and income.
The observed associations between parental education and income, and completion of the HPV vaccination, were small and unlikely to be of clinical relevance. This may indicate that factors important for completion of the HPV vaccination series are different from those associated with initiation. The proportion of girls completing the vaccination series once they have started was, however, high. Thus, to increase the overall uptake with three doses, efforts should focus on increasing initiation of HPV vaccination.
In this large data set we may detect statistically significant associations even for clinically insignificant differences. Hence, results should be interpreted with caution and in relation to their public health relevance. Most of the observed unadjusted differences in HPV vaccine uptake between the socioeconomic groups were small. However, the adjusted associations observed for maternal education and income may, in our opinion, be considered meaningful in a public health perspective. A health technology assessment recently performed by The Norwegian Knowledge Centre for the Health Services found that increasing the uptake of the first dose of HPV vaccine by 10 percentage points to the same level as the other vaccines in the Childhood Immunisation Programme in Norway, would result in an additional reduction of between 3 and 4 cases of cervical cancer and approximately 35 less cases of severe precancerous cervical lesions yearly.28 In a Norwegian setting, with about 300 cases of cervical cancer and approximately 3000 cases of severe precancerous cervical lesions yearly,29 30 we find this to be of clinical importance.
The major strength of our study is the use of individual data from different population-based registries, covering the total population. This allowed us to include all girls eligible for HPV vaccination during the first 3 years of the HPV immunisation programme in Norway, limiting selection bias while controlling for numerous possible confounders. The quality of the information on vaccination in the Norwegian Immunisation Registry is considered to be high, as there is mandatory notification to the immunisation registry. Moreover, extensive quality assurance systems are implemented to secure the accuracy of the data.10 The statistics compiled and provided by Statistics Norway are based on several nationwide administrative registries. These data are widely used in epidemiological research and are generally considered to be of high quality. The information on immigrants’ education obtained abroad may, however, be less precise as it is mainly based on surveys among immigrants.
The study is limited by incomplete information on some of the variables that were included (mainly education and income). The 7266 girls excluded due to missing information were less likely to have initiated HPV vaccination than the girls in the study sample (74.8% vs 78.3%, respectively). Moreover, a larger proportion of them did not have Norway as country of origin, as compared to the study sample (50.0% vs 7.8%, respectively). However, sensitivity analyses where girls with missing values were assigned values corresponding to the lowest and highest parental education level, and income, respectively, gave similar results. The effect estimates in the sensitivity analysis did not differ from our results, with more than 0.5 percentage points for any of the variables, with the exception of paternal education level, where the difference in one of the sensitivity analyses was 1.2 percentage points. Thus, it seems unlikely that exclusion of girls with missing information has biased the results.
Conclusion
In the current study, we observed inequalities in the uptake of HPV vaccine related to socioeconomic factors in the publicly funded school-based programme in Norway. Maternal income was positively associated with vaccine uptake in daughters. In contrast, maternal education was negatively associated with HPV vaccination. The findings were unexpected in a setting with presumably equal access to HPV vaccination. More studies are needed to explain the underlying factors responsible for the observed socioeconomic differences in HPV vaccine uptake. Insight into these factors is necessary in targeting information with the overall aim to increase vaccination coverage to the same high level as other childhood vaccines, and to ultimately reduce HPV-related precancerous lesion and cancers across socioeconomic barriers.
Footnotes
Contributors: BF contributed to conception and design of the study, acquisition of the data, analysis and interpretation of the data, and drafting the article. IL contributed to design of the study, preparation of the data files, analysis and interpretation of the data, and drafting the article. TM and BHS contributed to design of the study, analysis and interpretation of the data and revising the article critically for important intellectual content. IC, SEH, PM, OAS and JS contributed to design of the study, interpretation of the data and revising the article critically for important intellectual content. LT contributed to conception and design of the study, acquisition of the data, interpretation of the data and drafting the article. All authors gave final approval of the version to be published.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: The study was approved by the Regional Committee for Medical and Health Research Ethics, South East Norway.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Nygard M. Screening for cervical cancer: when theory meets reality. BMC Cancer 2011;11:240 10.1186/1471-2407-11-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Norwegian Institute of Public Health. Barnevaksinasjon—statistikk [Statistics on childhood vaccination] 2014. Norwegian. http://www.fhi.no/artikler/?id=84900 (accessed 11 Feb 2015).
- 3.Bergsaker M, Feiring B, Hagerup-Jenssen M et al. . Barnevaksinasjonsprogrammet i Norge. Rapport for 2012 [The Childhood Immunisation Programme in Norway. Report for 2012]. Norwegian Institute of Public Health, 2013. Norwegian. [Google Scholar]
- 4.Fisher H, Audrey S, Mytton JA et al. . Examining inequalities in the uptake of the school-based HPV vaccination programme in England: a retrospective cohort study. J Public Health (Oxf) 2013;36:36–45. 10.1093/pubmed/fdt042 [DOI] [PubMed] [Google Scholar]
- 5.Sinka K, Kavanagh K, Gordon R et al. . Achieving high and equitable coverage of adolescent HPV vaccine in Scotland. J Epidemiol Community Health 2014;68:57–63. 10.1136/jech-2013-202620 [DOI] [PubMed] [Google Scholar]
- 6.Smith LM, Brassard P, Kwong JC et al. . Factors associated with initiation and completion of the quadrivalent human papillomavirus vaccine series in an Ontario cohort of grade 8 girls. BMC Public Health 2011;11:645 10.1186/1471-2458-11-645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rondy M, van Lier A, van de Kassteele J et al. . Determinants for HPV vaccine uptake in the Netherlands: a multilevel study. Vaccine 2010;28:2070–5. 10.1016/j.vaccine.2009.12.042 [DOI] [PubMed] [Google Scholar]
- 8.Poole T, Goodyear-Smith F, Petousis-Harris H et al. . Human papillomavirus vaccination in Auckland: reducing ethnic and socioeconomic inequities. Vaccine 2012;31:84–8. 10.1016/j.vaccine.2012.10.099 [DOI] [PubMed] [Google Scholar]
- 9.Spencer AM, Roberts SA, Brabin L et al. . Sociodemographic factors predicting mother's cervical screening and daughter's HPV vaccination uptake. J Epidemiol Community Health 2014;68:571–7. 10.1136/jech-2013-202629 [DOI] [PubMed] [Google Scholar]
- 10.Trogstad L, Ung G, Hagerup-Jenssen M et al. . The Norwegian immunisation register—SYSVAK. Euro Surveill 2012;17:pii: 20147 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20147 [PubMed] [Google Scholar]
- 11.Nygård G. Facts about education in Norway 2015—key figures 2013. Statistics Norway 2014. http://www.ssb.no/en/utdanning/artikler-og-publikasjoner/facts-about-education-in-norway-2015?fane=om (accessed 11 Feb 2015).
- 12.Widgren K, Simonsen J, Valentiner-Branth P et al. . Uptake of the human papillomavirus-vaccination within the free-of-charge childhood vaccination programme in Denmark. Vaccine 2011;29:9663–7. 10.1016/j.vaccine.2011.10.021 [DOI] [PubMed] [Google Scholar]
- 13.Ogilvie G, Anderson M, Marra F et al. . A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med 2010;7:e1000270 10.1371/journal.pmed.1000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–6. 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 15.Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res 2011;22:661–70. 10.1177/0962280211427759 [DOI] [PubMed] [Google Scholar]
- 16.Leval A, Herweijer E, Ploner A et al. . Quadrivalent human papillomavirus vaccine effectiveness: a Swedish national cohort study. J Natl Cancer Inst 2013;105:469–74. 10.1093/jnci/djt032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hak E, Schonbeck Y, De Melker H et al. . Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine 2005;23:3103–7. 10.1016/j.vaccine.2005.01.074 [DOI] [PubMed] [Google Scholar]
- 18.Griffioen AM, Glynn S, Mullins TK et al. . Perspectives on decision making about human papillomavirus vaccination among 11- to 12-year-old girls and their mothers. Clin Pediatr (Phila) 2012;51:560–8. 10.1177/0009922812443732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Keulen HM, Otten W, Ruiter RA et al. . Determinants of HPV vaccination intentions among Dutch girls and their mothers: a cross-sectional study. BMC Public Health 2013;13:111 10.1186/1471-2458-13-111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stokley S, Jeyarajah J, Yankey D et al. . Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014—United States. MMWR Morb Mortal Wkly Rep 2014;63:620–4. [PMC free article] [PubMed] [Google Scholar]
- 21.Haug C. [Too good to be true]. Tidsskr Nor Laegeforen 2006;126:1891 Norwegian. [PubMed] [Google Scholar]
- 22.Haug C. [From uncertainty to anxiety]. Tidsskr Nor Laegeforen 2007;127:1763 Norwegian. [PubMed] [Google Scholar]
- 23.Haug C. [The HPV vaccine—still no answers to important questions]. Tidsskr Nor Laegeforen 2007;127:1625 Norwegian. [PubMed] [Google Scholar]
- 24.Dommerud T. Færre enn 30 prosent vil HPV-vaksineres [Less than 30 percent wants to be vaccinated against HPV]. Dagens medisin. 12 Nov 2009. Norwegian. http://www.dagensmedisin.np/nyheter/farre-enn-30-prosent-vil-hpv-vaksineres/
- 25.Trogstad L, Stålcrantz J, Hagerup-Jenssen M et al. . Årsrapport for HPV-vaksine i barnevaksinasjonsprogrammet 2009/2010 [Report for HPV vaccine in the Childhood Immunisation Programme 2009/2010]. Norwegian Institute of Public Health, 2011. Norwegian. [Google Scholar]
- 26.Næsheim H, Villund O. Deltidsarbeid—blir forskjellene utjevnet [Part-time employment—are the inequalitites reduced]. Samfunnsspeilet 2013;2:24–7. Norwegian. [Google Scholar]
- 27.OECD. Education at a glance 2013: OECD Indicators. OECD Publishing, 2013. 10.178/eag-2013-en [DOI] [Google Scholar]
- 28.Jiménez E, Torkilseng EB, Klemp M. Cost-effectiveness of HPV-vaccination of boys aged 12 in a Norwegian setting. Report from Kunnskapssenteret no 2–2015 Oslo: Norwegian Knowledge Centre for the Health Services, 2015. [PubMed] [Google Scholar]
- 29.Cancer Registry of Norway. Cancer in Norway 2012—Cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway, 2014. [Google Scholar]
- 30.Cancer Registry of Norway. Masseundersøkelsen mot livmorhalskreft. Årsrapport 2012. [The Cervical Cancer Screening Programme. Report for 2012]. Oslo: Cancer Registry of Norway, 2014. Norwegian. [Google Scholar]


