Abstract
Objective
To investigate the relationship between Ankle-Brachial Index (ABI) and renal function progression in patients with atrial fibrillation (AF).
Design
Observational prospective multicentre cohort study.
Setting
Atherothrombosis Center of I Clinica Medica of ‘Sapienza’ University of Rome; Department of Medical and Surgical Sciences of University Magna Græcia of Catanzaro; Atrial Fibrillation Registry for Ankle-Brachial Index Prevalence Assessment-Collaborative Italian Study.
Participants
897 AF patients on treatment with vitamin K antagonists.
Main outcome measures
The relationship between basal ABI and renal function progression, assessed by the estimated Glomerular Filtration Rate (eGFR) calculated with the CKD-EPI formula at baseline and after 2 years of follow-up. The rapid decline in eGFR, defined as a decline in eGFR >5 mL/min/1.73 m2/year, and incident eGFR<60 mL/min/1.73 m2 were primary and secondary end points, respectively.
Results
Mean age was 71.8±9.0 years and 41.8% were women. Low ABI (ie, ≤0.90) was present in 194 (21.6%) patients. Baseline median eGFR was 72.7 mL/min/1.73 m2, and 28.7% patients had an eGFR<60 mL/min/1.73 m2. Annual decline of eGFR was −2.0 (IQR −7.4/−0.4) mL/min/1.73 m2/year, and 32.4% patients had a rapid decline in eGFR. Multivariable logistic regression analysis showed that ABI ≤0.90 (OR 1.516 (95% CI 1.075 to 2.139), p=0.018) and arterial hypertension (OR 1.830 95% CI 1.113 to 3.009, p=0.017) predicted a rapid eGFR decline, with an inverse association for angiotensin converting enzyme (ACE) inhibitors/angiotensin receptor blockers (OR 0.662 95% CI 0.464 to 0.944, p=0.023). Among the 639 patients with AF with eGFR >60 mL/min/1.73 m2, 153 (23.9%) had a reduction of the eGFR <60 mL/min/1.73 m2. ABI ≤0.90 was also an independent predictor for incident eGFR<60 mL/min/1.73 m2 (HR 1.851, 95% CI 1.205 to 2.845, p=0.005).
Conclusions
In patients with AF, an ABI ≤0.90 is independently associated with a rapid decline in renal function and incident eGFR<60 mL/min/1.73 m2. ABI measurement may help identify patients with AF at risk of renal function deterioration.
Trial registration number
Strengths and limitations of this study.
Measurement of Ankle-Brachial Index (ABI) is a simple, inexpensive and standardised method to explore systemic atherosclerosis.
Renal function assessment and deterioration were assessed using international definitions.
ABI measurement may help identify patients with atrial fibrillation (AF) who are at high risk of renal function deterioration, and eventually require serum creatinine monitoring.
Our findings may turn particularly useful in the era of non-vitamin K antagonist oral anticoagulants, whose dosage requires to be tailored in AF patients with renal impairment.
Our analysis was performed only in a Caucasian population from the same country (Italy), limiting the generalisability of the findings.
Introduction
Atrial fibrillation (AF) is the most common arrhythmia encountered in daily clinical practice, accounting for approximately one-third of all hospitalisations for a cardiac rhythm abnormality. It is associated with a fivefold increase in the risk for stroke, and is estimated to be the cause of almost 15% of all strokes.1
Chronic kidney disease (CKD) is a frequent feature of patients with AF having an important impact on clinical outcomes, as it predisposes to both ischaemic stroke and bleeding.2–4 Diagnosis and evaluation of CKD progression is a part of comprehensive AF management, not only to prevent adverse clinical events, but also to aid decision-making on oral anticoagulation. In fact, evaluation of renal function is a key aspect when prescribing of non-vitamin K antagonist oral anticoagulants (NOACs), especially dabigatran.5
Ankle-Brachial Index (ABI) is a simple, inexpensive and non-invasive marker of peripheral artery disease and systemic atherosclerosis, which is associated with an increased risk of cardiovascular events.6 7 Prior studies have reported that a low ABI (ie, ≤0.90) is present in patients with CKD and predicts a rapid decline in renal function in the general population.8 We have recently reported that low ABI can be detected in about 20% of the AF population,9 suggesting that systemic atherosclerosis is a frequent feature in this setting.10 No prior studies have reported on the relationship between low ABI and rapid decline in renal function in patients with AF.
We hypothesised that low ABI may predict a rapid decline in renal function and may represent a useful, rapid and simple clinical tool to risk-stratify those patients at risk of renal impairment. Thus, we analysed the relationship between low ABI and the occurrence of rapid renal function decline, and incident CKD as assessed by renal function <60 mL/min/1.73 m2 during a follow-up of approximately 2 years in a large population affected by AF.
Methods
This was an observational prospective multicentre study including patients with AF recruited from the Atherothrombosis Center of I Clinica Medica of ‘Sapienza’ University of Rome, from the Department of Medical and Surgical Sciences, University Magna Græcia of Catanzaro, Italy, and from those included in the cohort of the Atrial Fibrillation Registry for Ankle-Brachial Index Prevalence Assessment-Collaborative Italian Study (see online supplementary appendix) who had a double determination of serum creatinine.
All patients with non-valvular AF aged >18 years and with a follow-up of at least 1 year were included in this prospective study. Exclusion criteria were the presence of valvular diseases (prosthetic heart valves or any severe valvulopathy), chronic infectious diseases (ie, HIV infection, hepatitis C virus, hepatitis B virus) or autoimmune systemic disease. Subjects were also excluded from the study if they had active cancer or liver insufficiency (eg, cirrhosis). At baseline, anthropometric data as well as comorbidities and concomitant therapies were collected. The presence of cardiovascular risk factors were defined as previously described.11
At baseline, serum creatinine (mg/dL) was obtained for all patients. Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula.12 Patients were classified in eGFR categories according to Kidney Disease: Improving Global Outcomes (KDIGO) guidelines:13 normal eGFR (>90 mL/min/1.73 m2, Stage G1), mildly decreased eGFR (89–60 mL/min/1.73 m2, Stage G2), moderately decreased eGFR (59–30 mL/min/1.73 m2, Stage G3) and severely decreased eGFR (<30 mL/min/1.73 m2, Stage G4). A second serum creatinine was collected during follow-up. The primary end point of the study was to evaluate the rapid decline in eGFR defined as a loss in glomerular filtration >5 mL/min/1.73 m2/year.13 The secondary end point of the study was incident CKD as defined as an eGFR<60 mL/min/1.73 m2.
ABI measurement
At baseline, trained clinical staff measured the ABI in all patients using an 8 MHz CW Vascular Doppler (Risingmed Model:RFD-B). ABI was calculated as the ratio of systolic blood pressure obtained from the ankle and brachial arteries. Ankle and brachial systolic blood pressures were measured separately for the right and left sides, and ABI was assessed separately for the right and left legs using the highest arm pressure as the denominator. Patients were categorised into 2 groups according to their ABI value: (1) normal, if both left and right ABI values were normal (ABI >0.90) and (2) low, if at least one of the two values of ABI was ≤0.90.
The local ethical boards approved the protocol study. The study was conducted according to the principles embodied in the Declaration of Helsinki, and all patients included in the present study provided written informed consent at enrolment.
Statistical analyses
Categorical variables are reported as counts (percentage). Continuous variables are expressed as mean±SD or median and interquartile range (IQR) (IQR; 25th–75th percentile), as appropriate. Two-sided t tests or the Wilcoxon rank sum test, depending on the shape of the distribution curve, was used to compare means. Pearson χ2 test was used to compare proportions. Bivariate analysis was performed with Pearson’s linear correlation. Appropriate non-parametric tests (Mann-Whitney U test and Spearman rank correlation test) were employed for all the other variables.
We calculated the annual absolute decline in eGFR, expressed as the difference between the two eGFR values (follow-up eGFR—basal eGFR/years of follow-up).
We divided the population according to the presence or absence of a rapid decline in eGFR (>5 mL/min/1.73 m2/year), to analyse clinical characteristics of patients with renal function deterioration. We performed a multivariable logistic regression analysis to calculate the adjusted ORs of factors associated with the annual rapid decline in kidney function.
The multivariate analysis was determined including all variables that could potentially affect renal function. In particular, we included as covariates the following variables: age, gender, ABI≤0.90, type of AF (persistent/permanent vs paroxysmal AF), presence of arterial hypertension, diabetes, heart failure, history of ischaemic stroke/transient ischaemic attack (TIA), history of myocardial infarction/cardiac revascularisation, as well as the use of angiotensin converting enzyme (ACE) inhibitors/angiotensin receptor blockers (ARBs), β blockers, calcium channel antagonists, statins, antiplatelet therapy and body mass index.
We also analysed the clinical characteristics of patients with AF developing incident eGFR<60 mL/min/1.73 m2. Considering that the second creatinine was not collected at the same time during follow-up for all patients with AF, we used a Cox proportional hazard regression analysis to calculate the relative adjusted hazard ratios (HRs) of factors associated with incident eGFR<60 mL/min/1.73 m2, using the same variables listed above with the addition of baseline eGFR, which has been shown to be predictive of incident eGFR<60 mL/min/1.73 m2.14
All tests were two-tailed and analyses were performed using computer software packages (SPSS-V.18.0, SPSS). Only p values <0.05 were considered as statistically significant.
Results
Clinical characteristics of 897 patients with AF included in the study are described in table 1. Mean age was 71.8±9.0 years, and 41.8% were women. The median CHA2DS2-VASc score was 3.0 (2.0–4.0).
Table 1.
Baseline characteristics of entire cohort, according to the presence or absence of renal impairment (eGFR<60 mL/min)
| Overall | Baseline eGFR <60 mL/min/1.73 m2 |
p Value | ||
|---|---|---|---|---|
| (n=897) | No (n=639) | Yes (n=258) | ||
| Age (years) | 71.8±9.0 | 69.8±8.9 | 76.7±7.3 | <0.001 |
| Women (%) | 41.8 | 36.9 | 53.9 | <0.001 |
| Permanent AF (%) | 43.1 | 40.7 | 49.2 | 0.021 |
| Body mass index (kg/m2) | 27.9±4.6 | 28.1±4.6 | 27.7±4.5 | 0.300 |
| Ankle-Brachial Index ≤0.90 (%) | 21.6 | 16.6 | 34.1 | <0.001 |
| CHA2DS2-VASc score | 3.0 (2.0–4.0) | 3.0 (2.0–4.0) | 4.0 (3.0–5.0) | <0.001 |
| Arterial hypertension (%) | 86.3 | 85.4 | 88.4 | 0.284 |
| Diabetes mellitus (%) | 24.1 | 22.7 | 27.5 | 0.075 |
| History of MI/CHD (%) | 18.4 | 16.7 | 22.5 | 0.029 |
| Heart failure (%) | 19.0 | 16.4 | 25.2 | 0.003 |
| History of stroke/TIA (%) | 11.3 | 11.1 | 11.6 | 0.816 |
| ACE inhibitor/ARBs (%) | 72.8 | 71.4 | 76.4 | 0.074 |
| β blockers (%) | 48.6 | 47.1 | 52.3 | 0.090 |
| Calcium channel antagonists (%) | 27.2 | 26.0 | 30.2 | 0.195 |
| Statins (%) | 44.4 | 43.3 | 46.9 | 0.336 |
| Antiplatelets (%) | 19.6 | 20.5 | 17.4 | 0.309 |
ACE, angiotensin converting enzyme; AF, atrial fibrillation; ARBs, angiotensin receptor blockers; CHD, coronary heart disease; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; TIA, transient ischaemic attack.
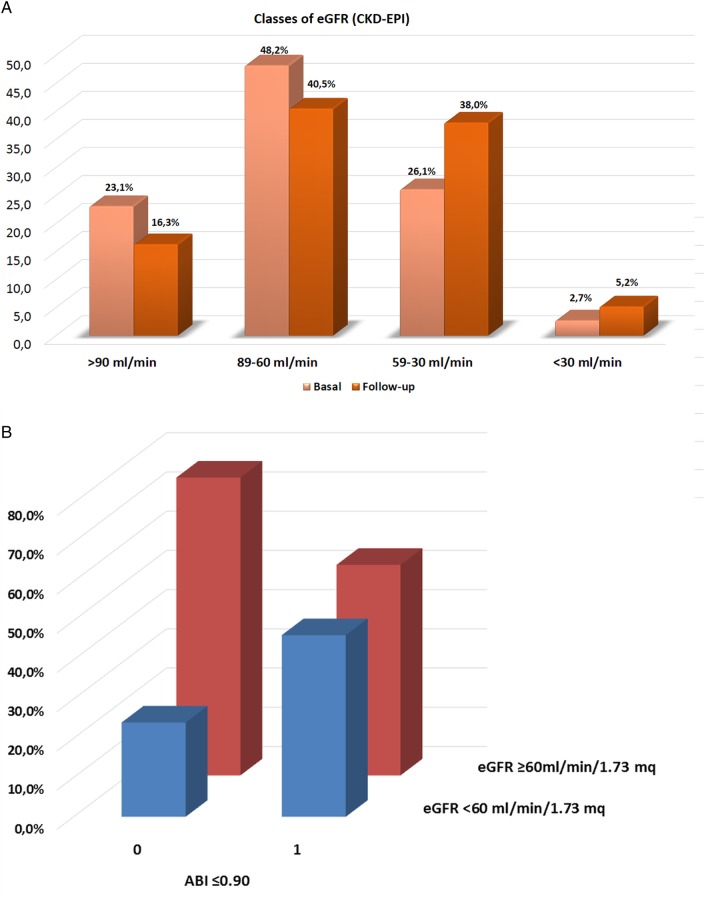
In the whole population, the baseline median eGFR was 72.7 mL/min/1.73 m2 (56.8–88.8), and 258 (28.7%) had an eGFR<60 mL/min/1.73 m2. Distribution of classes of eGFR in the whole cohort is reported in figure 1A. Prevalence of normal, mild, moderate and severe eGFR was 23.1%, 48.2%, 26.1% and 2.7%, respectively. Using 60 mL/min/1.73 m2 as a cut-off to define the CKD, we found that patients with renal disease were older, more frequently women, with a clinical history more complicated by heart failure and myocardial infarction/coronary heart disease and with a higher CHA2DS2-VASc score (table 1). Moreover, a higher prevalence of permanent AF was found in patients with baseline eGFR<60 mL/min/1.73 m2 (table 1).
Figure 1.
(A) Distribution of classes of estimated glomerular filtration rate (eGFR) in the whole cohort of patients with atrial fibrillation (AF) at baseline and during follow-up. (B) Prevalence of Ankle-Brachial Index (ABI) >0.90 (Row: 0) ABI ≤0.90 (Row: 1) in patients with eGFR ≥60 mL/min/1.73 m2 (Red columns) or <60 mL/min/1.73 m2 (Blue columns).
In the whole cohort, 194 (21.6%) had a value of ABI ≤0.90. No significant differences of low ABI were found between paroxysmal/persistent and permanent AF (19.6 vs 24.3%, p=0.102). The prevalence of reduced eGFR (<60 mL/min/1.73 m2) was significantly higher in patients with ABI ≤0.90 compared with those with ABI >0.90 (45.4 vs 24.2%, p<0.001) (figure 1B). Thus, patients with ABI ≤0.90 had a median eGFR of 65.0 (46.9–82.4) vs 74.1 (60.1–90.1) mL/min/1.73 m2 in those with normal ABI (p<0.001).
A second measurement of serum creatinine was obtained for all patients after a median of 2.0 (1.0–3.4) years. During follow-up, median eGFR decreased significantly from a baseline of 72.7 to 63.6 (48.8–82.0) mL/min/1.73 m2 (p<0.001) with a parallel increase in the prevalence of impaired renal function (figure 1A). Overall, the annual median decline in eGFR was −2.0 (IQR −7.4/−0.4) mL/min/1.73 m2/year, with no differences between paroxysmal/persistent and permanent AF (−2.1 (−7.5/−0.45) vs −2.0 (−7.1/−0.30), p=0.453).
Patients with AF with ABI ≤0.90 showed a significantly higher deterioration of renal function compared with those with normal ABI (−3.2 (−8.3 to −0.5) vs −1.9 (−6.8 to −0.4) mL/min/1.73 m2, p=0.020).
Rapid decline in renal function
Analysis of rapid deterioration in renal function showed that 291 (32.4%) patients with AF had a rapid decline in eGFR. The clinical characteristics of these patients are reported in table 2.
Table 2.
Clinical characteristics of patients with a rapid decline in renal function (>5 mL/min/1.73 m2/year)
| Rapid decline in eGFR (n=291) |
No decline in eGFR (n=606) |
p Value | |
|---|---|---|---|
| Age (years) | 72.1±8.4 | 71.6±9.3 | 0.486 |
| Body mass index (kg/m2) | 27.5±4.5 | 28.2±4.6 | 0.039 |
| Women (%) | 41.9 | 41.7 | 0.960 |
| Permanent AF (%) | 42.3 | 43.6 | 0.720 |
| Ankle-Brachial Index ≤0.90 (%) | 26.5 | 19.3 | 0.015 |
| Arterial hypertension (%) | 88.7 | 85.1 | 0.152 |
| Diabetes (%) | 23.0 | 24.6 | 0.608 |
| Heart failure (%) | 19.6 | 18.6 | 0.736 |
| History of stroke/TIA (%) | 10.0 | 11.9 | 0.396 |
| History of MI/CHD (%) | 19.6 | 17.8 | 0.523 |
| Antiplatelet (%) | 18.2 | 20.3 | 0.462 |
| ACE inhibitors/ARBs (%) | 69.4 | 74.4 | 0.068 |
| β blockers (%) | 51.5 | 47.2 | 0.222 |
| Calcium channel antagonists (%) | 27.8 | 26.9 | 0.768 |
| Statins (%) | 43.6 | 44.7 | 0.761 |
ACE, angiotensin converting enzyme; AF, atrial fibrillation; ARBs, angiotensin receptor blockers; CHD, coronary heart disease; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; TIA, transient ischaemic attack.
The rapid decline in renal function was detected in 97 (33.3%) patients with AF and normal eGFR at baseline, 148 (50.9%) with mildly decreased eGFR, 44 (15.1%) with moderately decreased eGFR and in 2 (0.7%) patients with baseline eGFR severely decreased.
A multivariable logistic regression analysis (table 3) showed that factors independently predicting rapid eGFR decline were ABI ≤0.90 (OR 1.516 (1.075 to 2.139), p=0.018) and arterial hypertension (OR 1.830 (1.113 to 3.009), p=0.017), while the use of ACE inhibitors/ARBs showed a protective effect (OR 0.662 (0.464 to 0.944), p=0.023).
Table 3.
Multivariable-adjusted ORs of factors associated with a rapid decline in kidney function (eGFR decrease >5 mL/min/1.73 m2/year)
| p Value | OR | 95% CI | |
|---|---|---|---|
| Age (years) | 0.988 | 0.998 | 0.741 to 1.344 |
| Women (%) | 0.819 | 0.998 | 0.981 to 1.015 |
| Body mass index (kg/m2) | 0.080 | 0.955 | 0.938 to 1.004 |
| Persistent/permanent AF (%) | 0.573 | 0.919 | 0.687 to 1.231 |
| Ankle-Brachial Index ≤0.90 (%) | 0.018 | 1.516 | 1.075 to 2.139 |
| Arterial hypertension (%) | 0.017 | 1.830 | 1.113 to 3.009 |
| Diabetes (%) | 0.485 | 0.883 | 0.622 to 1.253 |
| Heart failure (%) | 0.969 | 0.993 | 0.683 to 1.443 |
| History of stroke/TIA (%) | 0.176 | 0.723 | 0.452 to 1.156 |
| History of MI/CHD (%) | 0.800 | 1.052 | 0.708 to 1.564 |
| ACE inhibitors/ARBs (%) | 0.023 | 0.662 | 0.464 to 0.944 |
| β blockers (%) | 0.215 | 1.206 | 0.897 to 1.621 |
| Calcium channel antagonists (%) | 0.673 | 1.074 | 0.771 to 1.497 |
| Statins (%) | 0.848 | 0.971 | 0.720 to 1.311 |
| Antiplatelet (%) | 0.464 | 0.870 | 0.600 to 1.262 |
ACE, angiotensin converting enzyme; AF, atrial fibrillation; ARBs, angiotensin receptor blockers; CHD, coronary heart disease; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; TIA, transient ischaemic attack.
Incident eGFR<60 mL/min/1.73 m2
At baseline, 639 (71.2%) patients with AF had an eGFR >60 mL/min/1.73 m2; during the follow-up, 153 (23.9%) patients with an eGFR >60 mL/min/1.73 m2 had an eGFR<60 mL/min/1.73 m2. As shown in table 4, patients with AF with incident eGFR<60 mL/min/1.73 m2 were older, more frequently women, and affected by arterial hypertension compared with those with stable renal function. Low ABI was more frequent in patients with AF with incident eGFR<60 mL/min/1.73 m2 (table 4).
Table 4.
Characteristics of patients developing incident eGFR<60 mL/min/1.73 m2
| Incident eGFR<60 mL/min/1.73 m2 |
|||
|---|---|---|---|
| Yes (n=153) | No (n=486) | p Value | |
| Age (years) | 73.2±8.2 | 68.7±8.8 | <0.001 |
| Body mass index (kg/m2) | 27.5±4.5 | 28.2±4.7 | 0.090 |
| Women (%) | 45.1 | 34.4 | 0.016 |
| Permanent AF (%) | 39.2 | 41.2 | 0.760 |
| Ankle-Brachial Index ≤0.90 (%) | 23.5 | 14.4 | 0.008 |
| Arterial hypertension (%) | 90.8 | 83.7 | 0.030 |
| Diabetes (%) | 18.3 | 24.1 | 0.137 |
| Heart failure (%) | 12.4 | 17.7 | 0.124 |
| History of stroke/TIA (%) | 11.1 | 11.1 | 1.000 |
| History of MI/CHD (%) | 17.0 | 16.7 | 0.925 |
| Antiplatelet (%) | 16.3 | 21.8 | 0.087 |
| ACE inhibitors/ARBs (%) | 72.5 | 71.0 | 0.759 |
| β blockers (%) | 49.0 | 46.5 | 0.586 |
| Calcium channel antagonists (%) | 28.1 | 25.3 | 0.492 |
| Statins (%) | 44.4 | 43.0 | 0.754 |
ACE, angiotensin converting enzyme; AF, atrial fibrillation; ARBs, angiotensin receptor blockers; CHD, coronary heart disease; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; TIA, transient ischaemic attack.
A Cox regression analysis found a positive association of ABI ≤0.90 and age with incident eGFR<60 mL/min/1.73 m2, while baseline eGFR and the use of calcium channel antagonists were inversely associated (table 5).
Table 5.
Adjusted HRs, based on a Cox proportional hazards analysis of factors associated with incident eGFR<60 mL/min/1.73 m2
| p Value | HR | 95% CI |
||
|---|---|---|---|---|
| Age (years) | 0.019 | 1.030 | 1.005 | 1.056 |
| Baseline eGFR (mL/min/1.73 m2) | <0.001 | 0.957 | 0.944 | 0.971 |
| Body mass index (kg/m2) | 0.777 | 1.006 | 0.967 | 1.045 |
| Women (%) | 0.994 | 1.001 | 0.711 | 1.409 |
| Permanent AF (%) | 0.395 | 0.862 | 0.611 | 1.214 |
| Ankle-Brachial Index ≤0.90 (%) | 0.005 | 1.851 | 1.205 | 2.845 |
| Arterial hypertension (%) | 0.052 | 1.860 | 0.994 | 3.481 |
| Diabetes (%) | 0.151 | 0.713 | 0.449 | 1.132 |
| Heart failure (%) | 0.841 | 1.055 | 0.627 | 1.774 |
| History of stroke/TIA (%) | 0.867 | 1.046 | 0.619 | 1.767 |
| History of MI/CHD (%) | 0.172 | 0.725 | 0.457 | 1.150 |
| Antiplatelet (%) | 0.518 | 0.864 | 0.555 | 1.346 |
| ACE inhibitors/ARBs (%) | 0.442 | 0.842 | 0.543 | 1.306 |
| β blockers (%) | 0.788 | 1.052 | 0.728 | 1.521 |
| Calcium channel antagonists (%) | 0.029 | 0.640 | 0.429 | 0.954 |
| Statins (%) | 0.434 | 1.148 | 0.812 | 1.622 |
ACE, angiotensin converting enzyme; AF, atrial fibrillation; ARBs, angiotensin receptor blockers; CHD, coronary heart disease; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; TIA, transient ischaemic attack.
Discussion
This report shows that low ABI (ie ≤0.90) is associated with rapid deterioration of renal function and with an increased risk of incident kidney disease in a population affected by AF. The baseline analysis of our population showed that renal impairment was common in the AF population, as only 23% of patients have a normal renal function (eGFR >90 mL/min), while moderate renal impairment (eGFR<60 mL/min) was detected in approximately 30% of patients. Similar findings were seen by Roldan et al,3 who found 28% with moderate renal impairment in 978 patients affected by AF.3 Furthermore, patients with AF had an annual decline in renal function of approximately 2–5 mL/min, which is consistent with previous data in a very old AF population.15
To the best of our knowledge, only one previous study analysed the rate and predictors of rapid renal disease progression in AF. Roldan et al3 demonstrated a progression of CKD ≥10 mL/min in 21% of patients with AF at 2 years of follow-up, with age, female gender and arterial hypertension being significantly associated with a decline in renal function. This study, using the general definition of rapid decline in renal function >5 mL/min per year,13 shows a rapid function deterioration in 32.4% of patients with AF. Rapid deterioration was more evident in patients with AF with normal or mildly decreased renal function at baseline.
The novelty of this study is in the analysis of the interplay between low ABI and the rapid renal function deterioration in a population affected by AF. Thus far, only one study has explored this interplay in the general population, by comparing 51 participants with ABI ≤0.90 vs 2541 with ABI >0.90, and demonstrated that over a follow-up of 9 years, ABI ≤0.90 independently predicted a rapid decline in eGFR.8 In our cohort, which included 194 (21.6%) patients with AF with ABI ≤0.90, we confirm that ABI ≤0.90, along with hypertension, was significantly associated with a rapid decline in renal function, while the use of ACE/ARB inhibitors was protective.
This would suggest that low ABI, in addition to being a marker of systemic atherosclerosis, represents a marker of vascular damage occurring not only in the coronary or cerebral tree, but also in the circulation of other organs such as the kidney. Unfortunately, we cannot determine if the association between low ABI and rapid decline in renal function is a reflection of atherosclerotic burden in the micro-circulation and/or macro-circulation, but this issue deserves further investigation. However, our data are in keeping with other methods exploring atherosclerosis disease, such as pulse wave velocity, which have been shown to be predictive of renal function decline in different clinical settings.16 17
Analysis of incident eGFR<60 mL/min/1.73 m2 showed that approximately 24% of AF with baseline values >60 mL/min/1.73 m2 had renal function impairment. Further support for the role of ABI as a predictor of renal function deterioration was provided by the significant association between low ABI and incident eGFR<60 mL/min. This is in contrast to Foster et al,8 who found only a trend between low ABI and incident CKD, but their small sample size may perhaps account for the different findings.
This study has implications and limitations. Patients with AF have a relatively high prevalence and incidence of renal impairment which is related to ABI, a marker of systemic atherosclerosis. This finding may turn useful particularly in the era of NOACs which are excreted, even if to a different degree by the kidney, and whose dosage requires to be tailored in case of patients with AF with moderate renal function.18
In this context, ABI measurement could be particularly useful in identifying patients who are at high risk of renal function deterioration, and will eventually require serum creatinine monitoring.
Furthermore, identification of patients at high risk of renal disease progression may be of use to identify patients who are at higher risk of cardiovascular events. Our analysis performed only in a Caucasian population is a study limitation, as it cannot be translated to other race or ethnic groups. Another limitation of the study is represented by the lack of data on proteinuria or haematuria, which can be associated with an abnormality in the urinary tract even with a preserved eGFR (>90 mL/min) and with ABI<0.9.19 Finally, in our study, a decline in renal function has been assessed using only a second value of serum creatinine during follow-up; the analysis of renal function progression would be more appropriate by assessing more than two values of creatinine.
In conclusion, the study provides evidence that in patients with AF, an ABI ≤0.90 is independently associated with a rapid decline in renal function. ABI measurement may help identify patients with AF at risk of renal function deterioration.
Footnotes
Collaborators: ARAPACIS (Atrial Fibrillation Registry for Ankle-Brachial Index Prevalence Assessment-Collaborative Italian Study) study group: see online supplementary appendix.
Contributors: FV is responsible for the study concept and design, drafting of the manuscript and critical revision of the manuscript. DP and PP are responsible for the study concept and design, acquisition, analysis and interpretation of data and drafting of the manuscript. FP, WRH, GRC and GYHL are responsible for the interpretation of data, drafting of the manuscript and critical revision of the manuscript. AS, SB and MP are responsible for the acquisition, analysis and interpretation of data and critical revision of the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Local Ethical Board of Sapienza University of Rome.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983–8. 10.1161/01.STR.22.8.983 [DOI] [PubMed] [Google Scholar]
- 2.Marinigh R, Lane DA, Lip GY. Severe renal impairment and stroke prevention in atrial fibrillation: implications for thromboprophylaxis and bleeding risk. J Am Coll Cardiol 2011;57:1339–48. 10.1016/j.jacc.2010.12.013 [DOI] [PubMed] [Google Scholar]
- 3.Roldan V, Marin F, Fernandez H et al. Renal impairment in a “real-life” cohort of anticoagulated patients with atrial fibrillation (implications for thromboembolism and bleeding). Am J Cardiol 2013;111:1159–64. 10.1016/j.amjcard.2012.12.045 [DOI] [PubMed] [Google Scholar]
- 4.Apostolakis S, Guo Y, Lane DA et al. Renal function and outcomes in anticoagulated patients with non-valvular atrial fibrillation: the AMADEUS trial. Eur Heart J 2013;34:3572–9. 10.1093/eurheartj/eht328 [DOI] [PubMed] [Google Scholar]
- 5.Huisman MV, Lip GY, Diener HC et al. Dabigatran etexilate for stroke prevention in patients with atrial fibrillation: resolving uncertainties in routine practice. Thromb Haemost 2012;107:838–47. 10.1160/TH11-10-0718 [DOI] [PubMed] [Google Scholar]
- 6.Kojima I, Ninomiya T, Hata J et al. A low ankle brachial index is associated with an increased risk of cardiovascular disease: the Hisayama study. J Atheroscler Thromb 2014;21:966–73. 10.5551/jat.22608 [DOI] [PubMed] [Google Scholar]
- 7.Alzamora MT, Fores R, Pera G et al. Ankle-brachial index and the incidence of cardiovascular events in the Mediterranean low cardiovascular risk population ARTPER cohort. BMC Cardiovasc Disord 2013;13:119 10.1186/1471-2261-13-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foster MC, Ghuman N, Hwang SJ et al. Low ankle-brachial index and the development of rapid estimated GFR decline and CKD. Am J Kidney Dis 2013;61:204–10. 10.1053/j.ajkd.2012.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Violi F, Davi G, Hiatt W et al. Prevalence of peripheral artery disease by abnormal ankle-brachial index in atrial fibrillation: implications for risk and therapy. J Am Coll Cardiol 2013;62:2255–6. 10.1016/j.jacc.2013.07.035 [DOI] [PubMed] [Google Scholar]
- 10.Masanauskiene E, Naudziunas A. Comparison of ankle-brachial index in patients with and without atrial fibrillation. Medicina 2011;47:641–5. [PubMed] [Google Scholar]
- 11.Pastori D, Pignatelli P, Angelico F et al. Incidence of myocardial infarction and vascular death in anticoagulated elderly patients with atrial fibrillation: Relation to atherosclerotic risk factors. Chest 2014. Published Online First 27 November 2014. doi:10.1378/chest.14-2414. 10.1378/chest.14-2414 [DOI] [PubMed] [Google Scholar]
- 12.Levey AS, Stevens LA, Schmid CH et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 2013;158:825–30. 10.7326/0003-4819-158-11-201306040-00007 [DOI] [PubMed] [Google Scholar]
- 14.Tohidi M, Hasheminia M, Mohebi R et al. Incidence of chronic kidney disease and its risk factors, results of over 10 year follow up in an Iranian cohort. PLoS ONE 2012;7:e45304 10.1371/journal.pone.0045304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo Y, Wang H, Zhao X et al. Sequential changes in renal function and the risk of stroke and death in patients with atrial fibrillation. Int J Cardiol 2013;168:4678–84. 10.1016/j.ijcard.2013.07.179 [DOI] [PubMed] [Google Scholar]
- 16.Su HM, Lin TH, Hsu PC et al. Brachial-ankle pulse wave velocity and systolic time intervals in risk stratification for progression of renal function decline. Am J Hypertens 2012;25:1002–10. 10.1038/ajh.2012.77 [DOI] [PubMed] [Google Scholar]
- 17.Yoon HE, Shin DI, Kim SJ et al. Brachial-ankle pulse wave velocity predicts decline in renal function and cardiovascular events in early stages of chronic kidney disease. Int J Med Sci 2013;10:1430–6. 10.7150/ijms.6645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reilly PA, Lehr T, Haertter S et al. The effect of dabigatran plasma concentrations and patient characteristics on the frequency of ischemic stroke and major bleeding in atrial fibrillation patients: the RE-LY Trial (Randomized Evaluation of Long-Term Anticoagulation Therapy). J Am Coll Cardiol 2014;63:321–8. 10.1016/j.jacc.2013.07.104 [DOI] [PubMed] [Google Scholar]
- 19.Wattanakit K, Folsom AR, Criqui MH et al. Albuminuria and peripheral arterial disease: results from the multi-ethnic study of atherosclerosis (MESA). Atherosclerosis 2008;201:212–16. 10.1016/j.atherosclerosis.2007.12.044 [DOI] [PMC free article] [PubMed] [Google Scholar]