Abstract
Study Objective:
Recent studies report a link between obstructive sleep apnea (OSA) syndrome, low vitamin D levels, and high parathyroid hormone (PTH) concentrations. The aim of the current study is to evaluate the effect of 7-night continuous positive airway pressure (CPAP) therapy on serum vitamin D, PTH, and calcium levels in patients with severe OSA syndrome.
Methods:
Patients with severe OSA were enrolled into the study and compared to control subjects. Patients with OSA underwent CPAP therapy for 7 nights and were consequently divided into responders (OSA-R, mean residual AHI < 5/h) and nonresponders (OSA-nR, mean residual AHI > 5/h). Serum vitamin D, PTH, and calcium levels were measured at baseline in patients with severe OSA (apnea-hypopnea index > 30/h) and control subjects. Patients with OSA underwent a final morning blood sample after 7-night CPAP therapy.
Results:
We enrolled 90 patients with OSA into the study (65 OSA-R and 25 OSA-nR) compared to 32 control subjects. At baseline, lower vitamin D and higher PTH levels were detected in the OSA group compared to controls. After 7-night CPAP therapy, male OSA-R patients showed a significant increase in vitamin D levels. Conversely, female OSA-R patients did not show the same increase in vitamin D levels. It was also observed that OSA-nR subjects did not show modifications of serum markers after nCPAP-therapy.
Conclusions:
The study demonstrates that short-term nCPAP treatment is able to promote the recovery of vitamin D homeostasis in male patients with OSA. The mediation of sexual hormones in regulating vitamin D is a possible explanation of the lack of recovery of vitamin D homeostasis in female patients with OSA as it often affects postmenopausal women.
Citation:
Liguori C, Romigi A, Izzi F, Mercuri NB, Cordella A, Tarquini E, Giambrone MP, Marciani MG, Placidi F. Continuous positive airway pressure treatment increases serum vitamin D levels in male patients with obstructive sleep apnea. J Clin Sleep Med 2015;11(6):603–607.
Keywords: calcium, CPAP, OSA, PTH, vitamin D
Obstructive sleep apnea (OSA) syndrome is a condition characterized by the occurrence of repetitive episodes of partial or complete obstruction of the upper airway, intermittent hypoxia, and fragmentation of sleep.1 The prevalence of this syndrome in the population is between 3.1% and 7.5% in males and 1.2% and 4.5% in females.2 Nasal continuous positive airway pressure (nCPAP) represents the most suitable treatment of OSA.
Recent studies confirm the evidence of a link between OSA syndrome and abnormally low vitamin D and high parathyroid hormone (PTH) serum levels.3–6 Vitamin D and PTH participate in bone metabolism and calcium homeostasis. Additionally, vitamin D has pleiotropic effects, modulating numerous metabolic processes in multiple tissues throughout the body.7 Moreover, vitamin D deficiency has been recently associated with diabetes, hypertension, and incident stroke.7,8
Therefore, the aim of the current study is to verify whether short-term nCPAP treatment may influence serum vitamin D, PTH and calcium levels in patients with severe OSA syndrome.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Vitamin D not only participates in bone metabolism and regulates calcium homeostasis, but also has pleiotropic effects, modulating numerous metabolic processes. Considering that patients with obstructive sleep apnea (OSA) suffer from vitamin D deficiency and show high serum parathyroid hormone (PTH) levels, we tested the effects of short-term continuous positive airway pressure (CPAP) on serum vitamin D and PTH levels.
Study Impact: These findings suggest that short-term CPAP therapy in male patients with OSA determines an increase of serum vitamin D levels. Therefore, the current study provides evidence that OSA seems to be an etiopathogenetic factor involved in vitamin D deficiency, which may recover after CPAP therapy in male patients.
METHODS
In our study we included consecutive patients with OSA undergoing polygraphic cardiorespiratory monitoring diagnosed according to American Academy of Sleep Medicine (AASM) criteria.9 The recording montage included: an oronasal pressure cannula to record airflow and snoring sound, piezoelectric belts to detect thoracic and abdominal respiratory efforts, finger pulse oximetry, and sensors of heart rate and body positioning. The following oxygen saturation (SaO2) parameters were calculated: mean SaO2, lowest SaO2, time spent with SaO2 < 90% (T < 90), and oxygen desaturation index (ODI) (number of oxygen desaturations ≥ 3%/h). Apnea-hypopnea index (AHI) is defined as the sum of all apneas (> 90% reduction in airflow for > 10 seconds) and all hypopneas (> 30% reduction in airflow > 10 sec) associated with ≥ 3% O2 desaturation.10 Patients with OSA were selected based on an AHI ≥ 30/h, because such patients are candidates for nCPAP therapy. Patients underwent nCPAP therapy using a home autotitrating CPAP device with a mask pressure 5–15 cmH2O for 7 nights.11
The control group was selected from a population of volunteers with low sun exposure (indoor workers), and similar to patients with OSA in terms of age, sex, and body mass index (BMI). Inclusion criterion for controls was the absence of sleep disorders, evaluated by means of both a structured interview and a polygraphic cardiorespiratory monitoring (AHI < 5/h).
Exclusion criteria for patients with OSA and controls were: chronic liver disease or chronic renal failure; diabetes mellitus; thyroid dysfunction; malignancies; use of corticosteroids or antibiotics over the 4 w preceding recruitment in the study; autoimmune or neuromuscular disorders; symptoms or signs of acute or chronic inflammation disorders or recent infections; calcium or vitamin D supplements; and diuretic treatments.
At baseline, we took venous blood samples from patients with OSA and controls between 08:00 and 09:00 am after overnight fasting. Patients with OSA underwent a final morning blood sample after a 7-night period of nCPAP treatment.
Based on compliance and efficacy of the 7-night nCPAP home titration treatment documented by the ventilator software report, we divided patients with OSA in two subgroups: responders (OSA-R) who showed a mean residual AHI < 5/h during nCPAP therapy, with a usage > 4 h per night; and nonresponders (OSA-nR) who showed a residual AHI > 5/h. Moreover, the OSA-nR group also included patients who did not use their devices regularly (nCPAP usage < 4 h/night).
Serum vitamin D, PTH and calcium levels were quantified by routine clinical laboratory methods (Vista, Centaur, and Immulite Siemens Healthcare Diagnostic, Milan, Italy). To avoid seasonal variability, vitamin D levels in patients with OSA and controls were measured during the same season.
We also evaluated excessive daytime somnolence in patients with OSA and controls by means of the Epworth Sleepiness Scale (ESS).12,13
Patients and controls provided informed consent, which was approved by the Independent Ethical Committee of the University Hospital of Rome “Tor Vergata”.
We used the Statistica 10.0 program (Statsoft Inc, Tulsa, OK, USA) for the statistical analysis. One-way analysis of variance (ANOVA) was applied to compare clinical and cardiorespiratory polygraphic data as well as serum markers between patients with OSA and controls. We used three-way ANOVA with repeated measures counting treatment efficacy (OSA-R versus OSA-nR) and sex (male versus female) as “between” factors and serum markers levels (pre- versus post-nCPAP treatment) as “within” factors. Significant results were further analyzed using the post hoc Sheffè test.
Among the OSA patient groups, correlations between all the serum data, BMI, ESS, and polygraphic scores were separately performed through the nonparametric Spearman rank-order test. An additional multiple regression analysis was used after variable transformation (square root or logarithmic) when appropriate. The significance level was set at p < 0.05 for all statistical analyses.
RESULTS
Demographic, Clinical, and Polygraphic Data of Patients and Controls
Ninety patients with OSA completed the study between October 2013 and March 2014 (65 OSA-R and 25 OSA-nR). The control population consisted of 32 subjects of similar age, sex, and BMI to that of patients with OSA.
In the OSA-R group, the mean residual AHI was 3.21 ± 1.42/h and the mean nCPAP usage was 5.53 ± 1.12/h. In contrast, OSA-nR patients showed a mean residual AHI of 11.85 ± 4.91/h with a mean nCPAP usage of 4.78 ± 1.44 hours per night.
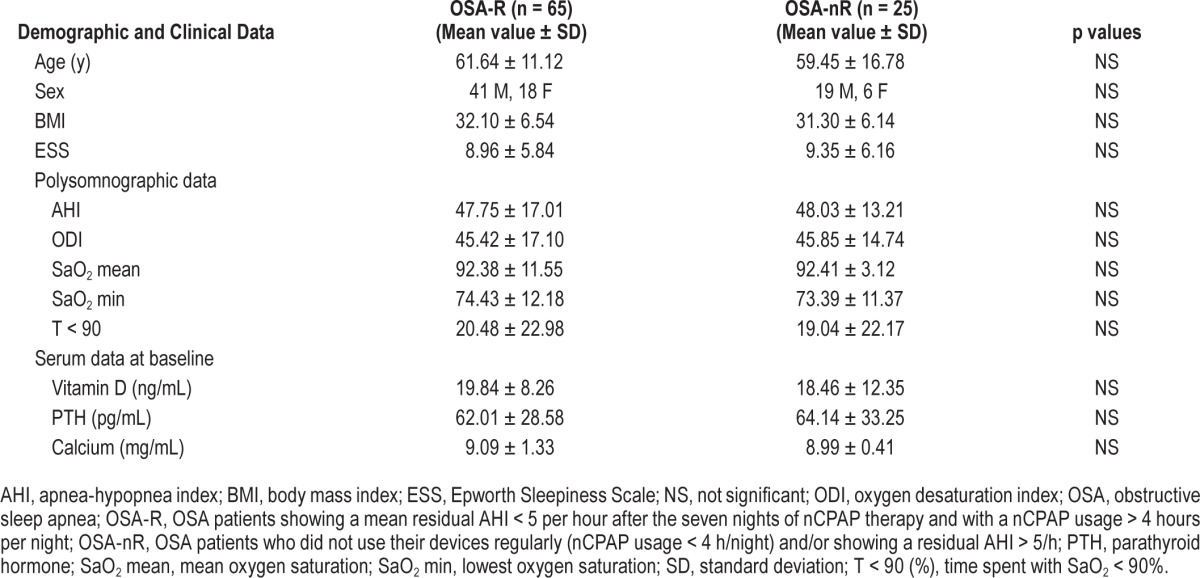
Demographic, clinical and polygraphic features of OSA patient groups and controls are summarized in Tables 1 and 2.
Table 1.
Demographic, clinical, polygraphic, and serum data of patients with obstructive sleep apnea and controls.
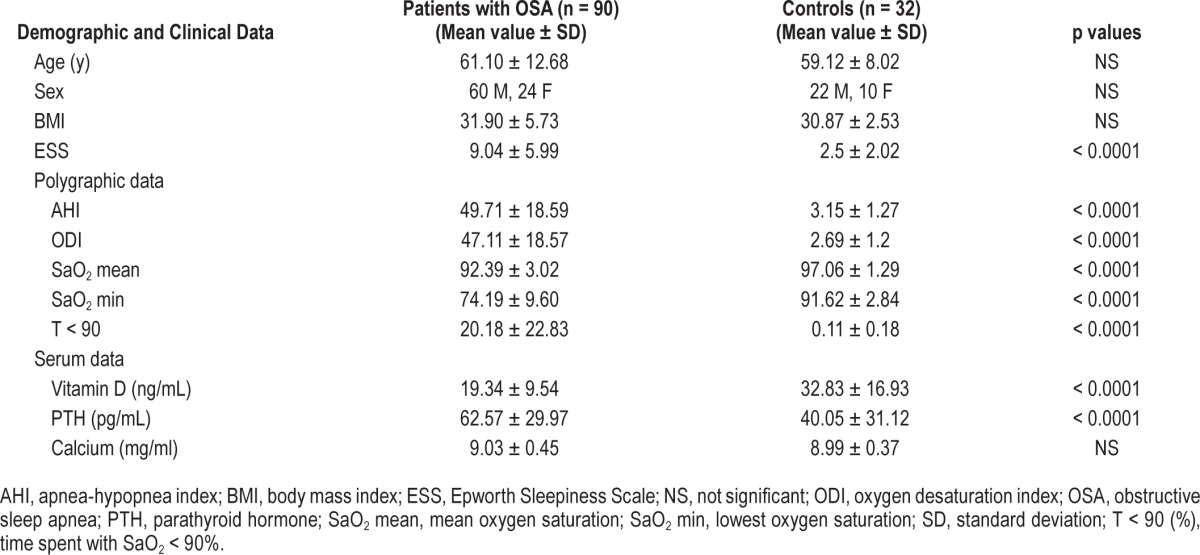
Table 2.
Demographic, clinical, polysomnographic, and serum data of obstructive sleep apnea patient subgroups at baseline.
Vitamin D, PTH and Calcium Levels in OSA Patient Group and Controls
We found lower vitamin D and higher PTH levels in patients with OSA compared to controls (Table 1). Serum calcium concentrations did not differ between patients with OSA and controls.
Correlations Between Clinical, Polygraphic, and Serum Data in Patients With OSA
The Spearman rank-order test showed that BMI correlated positively with PTH levels (R = 0.42, p < 0.001) and negatively with vitamin D levels (R = −0.32, p < 0.01) in the entire OSA group. ESS value correlated negatively with minimum oxygen saturation (R = −0.27, p = 0.039). Moreover, we found a significant negative correlation between serum PTH levels and both vitamin D and calcium levels (R = −0.26 and p < 0.05, R = −0.29 and p < 0.05; respectively). No other correlations between the aforementioned parameters emerged. The additional multivariate regression analysis revealed the association between serum vitamin D levels and lowest SaO2 (β = 1.37, p = 0.04).
Vitamin D, PTH, and Calcium Levels in Patient Groups After nCPAP Therapy
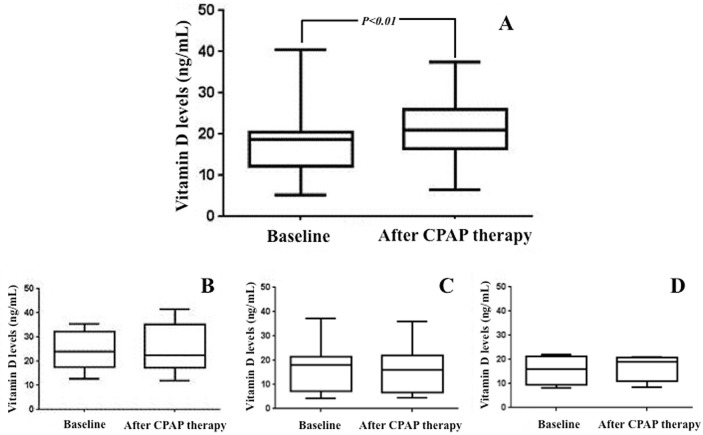
We observed a significant nCPAP treatment effect with the increase of serum vitamin D concentrations in the global OSA population (19.21 ± 9.45 versus 21.03 ± 9.50, F = 8.32, p < 0.01). In addition, we found a significant interaction between OSA subgroups, sex, and nCPAP treatment (F = 10.03, p < 0.01). In particular, the post hoc analysis showed the significant increase of serum vitamin D levels after 7-night nCPAP therapy compared to baseline in male OSA-R (Figure 1, p < 0.01). This increase was not observed in female OSA-R patients or in OSA-nR subgroups (Figure 1, p > 0.05). No significant effect of nCPAP therapy on serum calcium and PTH levels was observed in OSA-R and OSA-nR subgroups.
Figure 1. Vitamin D levels in obstructive sleep apnea (OSA) patient subgroups at baseline and after continuous positive airway pressure (CPAP) therapy [mean ± standard deviation (min-max)].
We observed the significant increment of serum vitamin D levels uniquely in male OSA responders (A), whereas this increase was not evident in female OSA responder (B), male OSA nonresponder (C), and female OSA nonresponder (D) subgroups.
DISCUSSION
These results confirm the emerging lines of evidence that patients with OSA suffer from low vitamin D and high PTH levels.3–6 The novel contribution of the current study lies in the observation that a short-term treatment with nCPAP promotes the improvement of the vitamin D homeostasis in male patients with OSA. In fact, nCPAP is the treatment of choice to improve several internal parameters in patients with OSA.14–18
Vitamin D has pleiotropic effects and plays major roles in an extended range of organ functions and disorders.7 Vitamin D is a fat-soluble secosteroid hormone which undergoes two hydroxylation reactions, first in the liver and second in the kidney.7 Hydroxylations are regulated by complex feedback loops involving PTH and calcium serum levels.7
We confirmed in our population of patients with OSA the high prevalence of low vitamin D levels coupled with high PTH concentrations. Consistently, it is well known that vitamin D deficiency causes a compensatory increase of PTH levels in order to maintain serum calcium homeostasis.19 Obesity, frequently associated with OSA,20 is also linked to vita-min D deficiency and PTH increase.21,22 Congruously, in the OSA patient group, BMI correlated negatively with vitamin D levels and positively with PTH concentrations. However, we found that patients with OSA showed lower vitamin D and higher PTH levels with respect to BMI-matched controls. On this basis, it can be hypothesized that OSA represents a risk factor for vitamin D deficiency independently of obesity and it is plausible that OSA coupled with obesity may cause a more severe vitamin D-deficient status, which seems to improve after short-term nCPAP therapy. Furthermore, the association found between lowest SaO2 and serum vitamin D levels could suggest that hypoxia is a putative factor involved in vitamin D deficiency in patients with OSA, as reported in chronic obstructive pulmonary diseases.23 However, considering that vitamin D binding-protein (VDBP) changes its serum level in response to chronic hypoxia,24 further investigation of VDBP serum levels in patients with OSA before and after CPAP treatment would be necessary in the future.
Interestingly, the increase in vitamin D levels was observed only in male OSA-R patients. This differential effect of nCPAP treatment may be related to the observation that vitamin D deficiency is frequently reported in postmenopausal women,25 as were those included in this study. Consistently, it is well known that sex hormone secretions affect bone mineralization, calcium homeostasis, and both vitamin D and PTH levels.
Developing evidence suggests that low vitamin D levels increase the risk of cardiovascular and cerebrovascular diseases, diabetes, autoimmune diseases, chronic rhinitis, and tonsillar hypertrophy.8,26 Additionally, vitamin D deficiency may also elevate the risk of development of OSA via various mechanisms.26 Therefore, ensuring normal serum vitamin D levels in patients with OSA may reduce the worsening of OSA syndrome and prevent cardiovascular and cerebrovascular risk and diabetes.
In conclusion, this study has demonstrated that short-term nCPAP treatment is able to promote the recovery of vitamin D homeostasis in male patients with OSA. The mediation of sex hormones in regulating vitamin D is a possible explanation of the lack of recovery of vitamin D homeostasis in female patients with OSA as it often affects postmenopausal women. Further studies investigating the effect of long-term nCPAP on vitamin D and PTH levels would be beneficial in the near future.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Ryan CM, Bradley TD. Pathogenesis of obstructive sleep apnea. J Appl Physiol. 2005;99:2440–50. doi: 10.1152/japplphysiol.00772.2005. [DOI] [PubMed] [Google Scholar]
- 2.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barcelo A, Esquinas C, Pierola J, et al. Vitamin D status and parathyroid hormone levels in patients with obstructive sleep apnea. Respiration. 2013;86:295–301. doi: 10.1159/000342748. [DOI] [PubMed] [Google Scholar]
- 4.Erden ES, Genc S, Motor S, et al. Investigation of serum bisphenol A, vitamin D, and parathyroid hormone levels in patients with obstructive sleep apnea syndrome. Endocrine. 2014;45:311–8. doi: 10.1007/s12020-013-0022-z. [DOI] [PubMed] [Google Scholar]
- 5.Bozkurt NC, Cakal E, Sahin M, Ozkaya EC, Firat H, Delibasi T. The relation of serum 25-hydroxyvitamin-D levels with severity of obstructive sleep apnea and glucose metabolism abnormalities. Endocrine. 2012;41:518–25. doi: 10.1007/s12020-012-9595-1. [DOI] [PubMed] [Google Scholar]
- 6.Mete T, Yalcin Y, Berker D, et al. Obstructive sleep apnea syndrome and its association with vitamin D deficiency. J Endocrinol Invest. 2013;36:681–5. doi: 10.3275/8923. [DOI] [PubMed] [Google Scholar]
- 7.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 8.Michos ED, Carson KA, Schneider AL, et al. Vitamin D and subclinical cerebrovascular disease: The Atherosclerosis Risk in Communities Brain Magnetic Resonance Imaging Study. JAMA Neurol. 2014;71:863–71. doi: 10.1001/jamaneurol.2014.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 10.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuna ST, Gurubhagavatula I, Maislin G. Non inferiority of functional outcome in ambulatory management of obstructive sleep apnea. Am J Respir Crit Care Med. 2011;183:1238–44. doi: 10.1164/rccm.201011-1770OC. [DOI] [PubMed] [Google Scholar]
- 12.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 13.Vignatelli L, Plazzi G, Barbato A, et al. Italian version of the Epworth sleepiness scale: external validity. Neurol Sci. 2003;23:295–300. doi: 10.1007/s100720300004. [DOI] [PubMed] [Google Scholar]
- 14.Diomedi M, Placidi F, Cupini LM, Bernardi G, Silvestrini M. Cerebral hemodynamic changes in sleep apnea syndrome and effect of continuous positive airway pressure treatment. Neurology. 1998;51:1051–6. doi: 10.1212/wnl.51.4.1051. [DOI] [PubMed] [Google Scholar]
- 15.Entzian P, Linnemann K, Schlaak M, Zabel P. Obstructive sleep apnea syndrome and circadian rhythms of hormones and cytokines. Am J Respir Crit Care Med. 1996;153:1080–6. doi: 10.1164/ajrccm.153.3.8630548. [DOI] [PubMed] [Google Scholar]
- 16.Chin K, Shimizu K, Nakamura T, et al. Changes in intra-abdominal visceral fat and serum leptin levels in patients with obstructive sleep apnea syndrome following nasal continuous positive airway pressure therapy. Circulation. 1999;100:706–12. doi: 10.1161/01.cir.100.7.706. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura T, Chin K, Shimizu K, et al. Acute effect of nasal continuous positive airway pressure therapy on the systemic immunity of patients with obstructive sleep apnea syndrome. Sleep. 2001;24:545–53. doi: 10.1093/sleep/24.5.545. [DOI] [PubMed] [Google Scholar]
- 18.Christou K, Kostikas K, Pastaka C, Tanou K, Antoniadou I, Gourgoulianis KI. Nasal continuous positive airway pressure treatment reduces systemic oxidative stress in patients with severe obstructive sleep apnea syndrome. Sleep Med. 2009;10:87–94. doi: 10.1016/j.sleep.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 19.McCarty MF, Thomas CA. PTH excess may promote weight gain by impeding catecholamine-induced lipolysis-implications for the impact of calcium, vitamin D, and alcohol on body weight. Med Hypotheses. 2003;61:535–42. doi: 10.1016/s0306-9877(03)00227-5. [DOI] [PubMed] [Google Scholar]
- 20.Vgontzas AN, Bixler EO, Chrousos GP, Pejovic S. Obesity and sleep disturbances: meaningful sub-typing of obesity. Arch Physiol Biochem. 2008;114:224–36. doi: 10.1080/13813450802521507. [DOI] [PubMed] [Google Scholar]
- 21.Snijder MB, van Dam RM, Visser M, et al. Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women. J Clin Endocrinol Metab. 2005;90:4119–23. doi: 10.1210/jc.2005-0216. [DOI] [PubMed] [Google Scholar]
- 22.Young T. Rationale, design and findings from the Wisconsin Sleep Cohort Study: toward understanding the total societal burden of sleep disordered breathing. Sleep Med Clin. 2009;4:37–46. doi: 10.1016/j.jsmc.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Persson LJ, Aanerud M, Hiemstra PS, Hardie JA, Bakke PS, Eagan TM. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One. 2012;7:e38934. doi: 10.1371/journal.pone.0038934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmad Y, Sharma NK, Garg I, Ahmad MF, Sharma M, Bhargava K. An insight into the changes in human plasma proteome on adaptation to hypobaric hypoxia. PLoS One. 2013;8:3e67548. doi: 10.1371/journal.pone.0067548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mata-Granados JM, Cuenca-Acevedo JR, Luque de Castro MD, Holick MF, Quesada-Gomez JM. Vitamin D insufficiency together with high serum levels of vitamin A increases the risk for osteoporosis in postmenopausal women. Arch Osteoporos. 2013;8:124. doi: 10.1007/s11657-013-0124-5. [DOI] [PubMed] [Google Scholar]
- 26.McCarty DE, Chesson AL, Jr., Jain SK, Marino AA. The link between vitamin D metabolism and sleep medicine. Sleep Med Rev. 2014;18:311–9. doi: 10.1016/j.smrv.2013.07.001. [DOI] [PubMed] [Google Scholar]