Abstract
Study Objectives:
Although a substantial number of pregnant women report symptoms of insomnia, few studies have used a validated instrument to determine the prevalence in early gestation. Identification of insomnia in pregnancy is vital given the strong connection between insomnia and the incidence of depression, cardiovascular disease, or immune dysregulation. The goal of this paper is to provide additional psychometric evaluation and validation of the Insomnia Symptom Questionnaire (ISQ) and to establish prevalence rates of insomnia among a cohort of pregnant women during early gestation.
Methods:
The ISQ was evaluated in 143 pregnant women at 12 weeks gestation. The internal consistency and criterion validity of the dichotomized ISQ were compared to traditional measures of sleep from sleep diaries, actigraphy, and the Pittsburgh Sleep Quality Index using indices of sensitivity, specificity, positive and negative predictive value (PPV, NPV), and likelihood ratio (LR) tests.
Results:
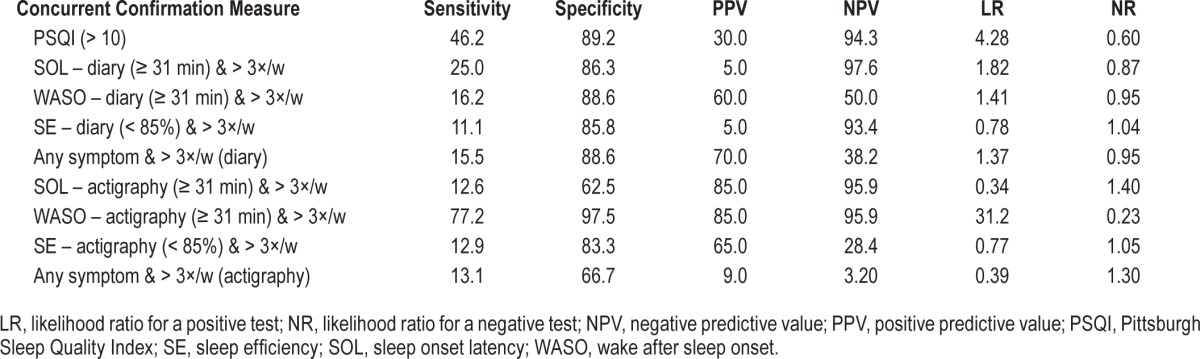
The ISQ identified 12.6% of the sample as meeting a case definition of insomnia, consistent with established diagnostic criteria. Good reliability was established with Cronbach α = 0.86. The ISQ had high specificity (most > 85%), but sensitivity, PPV, NPV, and LRs varied according to which sleep measure was used as the validating criterion.
Conclusions:
Insomnia is a health problem for many pregnant women at all stages in pregnancy. These data support the validity and reliability of the ISQ to identify insomnia in pregnant women. The ISQ is a short and cost-effective tool that can be quickly employed in large observational studies or in clinical practice where perinatal women are seen.
Commentary:
A commentary on this article appears in this issue on page 593.
Citation:
Okun ML, Buysse DJ, Hall MH. Identifying insomnia in early pregnancy: validation of the insomnia symptoms questionnaire (ISQ) in pregnant women. J Clin Sleep Med 2015;11(6):645–654.
Keywords: actigraphy, insomnia, pregnancy, sleep, validity
Pregnant women report substantial sleep disturbances beginning as early as 10 weeks.1 Among the many sleep complaints associated with pregnancy, difficulty initiating or maintaining sleep or unrefreshing sleep, are the most frequently reported issues .1,2 Collectively these sleep symptoms comprise only one aspect of clinical insomnia. According to diagnostic criteria for insomnia, one must have: (1) a difficulty initiating or maintaining sleep, and/or unrefreshing sleep despite adequate opportunity for sleep; (2) the duration of the sleep complaint is at least 1 mo; and (3) complaints of significant impairment in social, occupational, or daily functioning.3,4 Insomnia is associated with activation of the stress system resulting in autonomic hyperarousal.5,6 It is also linked to various morbidities including depression.7–12 Emerging evidence implicates autonomic hyperarousal as a pathway through which the risk of depression is augmented.13 This association is particularly relevant for pregnant women because there is evidence that depression is associated with an increased risk for preterm birth (PTB),14 and prenatal depression negatively impairs maternal-child bonding and neurocognitive development.14–17 Having a simple diagnostic tool to identify clinical insomnia in pregnant women could be a first step in reducing the incidence of depression, autonomic hyperarousal, as well as adverse pregnancy outcomes, such as PTB.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Pregnant women are at increased risk for insomnia. Insomnia is associated with an increased risk for adverse health outcomes. Identifying insomnia in pregnant women using a diagnostically valid instrument could assist with the diagnosis of insomnia. Early identification may lead to early intervention, and a subsequent amelioration of risk.
Study Impact: The ISQ provides useful clinical information regarding degree and severity of insomnia symptoms. Given what we know about sleep and adverse pregnancy outcomes, use of the ISQ could help with the dissemination of the importance of sleep and sleep problems during pregnancy.
Pregnant women are attracting greater attention with regard to insomnia. Evidence supports the conviction that an increasing number of women report insomnia symptoms following conc eption.18–20 Although the majority of the evidence indicates that the third trimester confers the greatest risk for developing i nsomnia,19,21 few studies have assessed sleep in early pregnancy and none have evaluated the prevalence of a case definition of insomnia. We contend that a substantial number of women are at risk of developing insomnia in early pregnancy based on the myriad physiological and psychological changes that occur. The first weeks of conception are characterized by marked fluctuations in immune and endocrine markers22–26 known to directly and indirectly affect sleep. Physical symptoms, such as increased need to urinate, backache, and nausea, are recognized disruptors of sleep.27,28 Psychological factors, including pregnancy-related anxiety and distress, can also impair a woman's ability to effectively return to sleep.1,29 We recently reported that about 30% of nonde-pressed pregnant women endorsed symptoms of insomnia at 20 w.20 We believe that early pregnancy may be a critical period in which to identify insomnia, given the vast physiological adaptations that occur during this time,30–32 as well as the links between symptoms of insomnia and adverse pregnancy outcomes.33,34
Various symptom severity questionnaires have been incorporated into studies of sleep in pregnancy in order to assess the prevalence of insomnia. Several of these correspond to specific diagnostic criteria by assessing sleep complaints, duration and/ or daytime consequences. Kizilirmak and colleagues19 used the Women's Health Initiative Insomnia Rating Scale (WHIRS)35 to identify the prevalence of insomnia in 486 women during pregnancy. Although they found that > 50% of the women scored positive for insomnia sleep symptoms,19 the WHIRS only assesses the frequency of the sleep symptoms in the past 4 w, but not the daytime impairment which is a key component of diagnostic criteria. Dorheim et al.18 used the Bergen Insomnia Scale (BIS) in 2,816 women at two times during pregnancy. Similarly, they found that about 61% of women met Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) criteria for insomnia at 32 w gestation.18 Although the BIS adequately assesses diagnostic insomnia criteria, it does not capture the duration that one has experienced insomnia. Thus, insomnia may be overdiagnosed with this scale. Others have used the Pittsburgh Sleep Quality Index (PSQI)36,37 to indicate prevalence of sleep disturbance and/or insomnia in pregnancy. Although the PSQI may reliably quantify subjective sleep quality in pregnant women,38–40 it was not designed to identify insomnia per se. The most commonly used measure of insomnia symptoms in pregnant women has been the Insomnia Severity Index (ISI).41 Several studies of pregnant women report high rates of insomnia symptoms. Swanson et al.42 reported that 45% of pregnant women scored above the threshold value, and Fernandez-Alonso et al.43 identified more than 73% in late pregnancy. Manber and colleagues,44 however, reported that only 17% of Latina women, across all trimesters, met criteria for insomnia (≥ 10) and that there was no difference across trimesters.
The Insomnia Symptom Questionnaire (ISQ) is a validated 13-item self-report instrument designed to identify insomnia.45 However, it has only been validated in a cohort of perimenopausal and postmenopausal women.45 The extent to which pregnant women experience insomnia differentially or to a varying degree than other groups of women has not been evaluated. In the current paper, we psychometrically evaluate the ISQ in comparison to sleep data ascertained by frequently used collection methods utilized in pregnant women. Additionally, in light of the goals of the Healthy People 2020 initiative,46,47 this tool may be exceptionally valuable in the clinical setting. Both prenatal health care visits and sleep health are highlighted as areas of opportunity in which to reduce present and future morbidity. We further sought to estimate the prevalence of insomnia in early pregnancy, given evidence that insomnia contributes to pregnancy-related morbidity.10,48,49
METHODS
Participants
Study participants were 160 pregnant women between age 18 and 45 y who were recruited from the greater Pittsburgh area from October 2008 through December 2012 as part of a larger study evaluating pregnancy-related sleep disturbances in relation to perinatal outcomes.1,50 The women were identified through self-referral, physician referral, local advertising, or enrollment in University research registries. Potential participants were excluded it they self-reported a diagnosis of a mental disorder, sleep disorder, had chronic diseases, including diabetes, human immunodeficiency virus, or uterine abnormalities, or were actively taking antidepressants or receiving other treatments for mental disorders, i.e., therapy. Women were not objectively tested for sleep disturbances, such as obstructive sleep apnea/sleep disordered breathing. Nor were they clinically assessed for restless legs. Data from women who miscarried (n = 7) or did not have complete sleep data at 10–12 weeks or ISQ data (n = 10) were not included in the current analyses, leaving a final sample of 143 women. All participants provided written consent. Approval was received from the University of Pittsburgh Institutional Review Board.
Procedures
The research design was a prospective observational study, examining daily indices of sleep in early gestation. Participants recorded subjective sleep and daily activity in the Pittsburgh Sleep Diary53 and wore a wrist actigraph (Mini Mitter, Philips Respironics, Bend, OR) on their nondominant arm for 2 w during 10–12 weeks gestation. The assessment period enabled collection of all sleep patterns for the entire time period, often including irregularities due to illness, travel, “on call” nights, etc. All available days with data were included in the descriptive analyses. Subsequent to the diary/actigraphy assessment period, participants completed a series of online questionnaires.
Measures
The ISQ is a 13-item self-report instrument designed to identify insomnia.45 ISQ questions are based on DSM-IV criteria for primary insomnia4 and are consistent with the American Academy of Sleep Medicine's (AASM) Research Diagnostic Criteria (RDC).51 The ISQ does not assess whether the sleep disturbance occurs exclusive of another sleep disorder, mental disorder, or substance or general medical condition (criteria C-E in DSM-IV for primary insomnia) that allows clinicians to diagnose other DSM-IV insomnia subtypes. However, in the current sample, women were excluded if they reported a diagnosis of a sleep disorder or major medical condition. Hence, it is likely that the women in whom insomnia was diagnosed via the ISQ have primary insomnia. The ISQ and its psychometric properties have been characterized in a cohort of midlife women going through the menopausal transition. Compared to traditionally used methods to identify insomnia, the ISQ has good internal reliability, Cronbach α = 0.89, modest sensitivity (50–66.7%), and excellent specificity (90.8–91.0%).
The PSQI36 is an 18-item questionnaire used to measure sleep quality complaints. Seven component scores assess habitual duration of sleep, nocturnal sleep disturbances, sleep latency, sleep quality, daytime dysfunction, sleep medication usage, and sleep efficiency. The seven components (range 0–3) are summed to yield a measure of global sleep quality with a range of 0 (good sleep quality) to 21 (poor sleep quality). The PSQI and its psychometric properties have been characterized in various populations, including patients with insomnia, depression, and pregnant women.39,52 These reports have documented adequate sensitivity and specificity using a cutoff score > 5 to identify those with poor sleep quality in depressed and pregnant women, and a cutoff score > 10 to identify poor sleep quality among people with insomnia.
Other measures are self-reported and actigraphy-assessed sleep variables. Symptoms of insomnia include difficulty falling asleep, difficulty staying asleep, and unrefreshing sleep. Three resultant variables are sleep onset latency (SOL), wake after sleep onset (WASO), and sleep efficiency (SE). These variables are used to quantify the first two symptoms of insomnia. Unrefreshing sleep is defined from a subjective perspective. SOL is circumscribed as the interval between when one “tried to go to sleep” to the onset of sleep. WASO is circumscribed as the total number of minutes spent awake following sleep onset. Time in bed (TIB) is circumscribed as the total amount of time from reported “time tried to go to sleep” to the time of the reported final awakening from sleep. Total sleep time (TST) is circumscribed as minutes of time spent asleep between sleep onset and offset. SE is circumscribed as the ratio of TST to TIB, multiplied by 100.
Sleep diaries53 were used to describe daily measures of self-reported sleep parameters at both a morning and evening recording time. Variables included mean values for SOL, WASO, TST, TIB, and SE calculated from all available sleep diary data.
Wrist actigraphy data (Mini Mitter Actiwatch 64; Philips Respironics) were collected for 14 continuous days via an actigraph worn on the nondominant wrist. Participants were instructed to press the event marker button when “I tried to go to sleep” and when “I got out of bed.” Data were analyzed in 1-min epochs with Actiware version 5.04 software (Philips Respironics) using sleep diary data to corroborate bedtime and wake time. On download, each record was visually inspected for collection quality (i.e., correct number of days and watch removals). The Auto Interval option was set to identify one primary Rest Interval per 24-h period, using the markers as anchor points. This method saves processing time but does not eliminate the need for some manual editing. Periods of time where the watch was not worn during the protocol were excluded from the record prior to export. Sleep parameters calculated from the sleep diary and actigraphy data included SOL, WASO, and SE. These variables were chosen as they are validated actigraphy parameters or have been conventionally used in reports examining quantitative criteria for insomnia: SOL ≥ 31 min; WASO ≥ 31 min; and SE ≤ 85%.54–57
Statistical Analyses
Descriptive statistics were used to characterize the subjective (questionnaires and diary) and actigraphy-assessed sleep measures. Pearson correlations were conducted to assess the discriminant validity between the ISQ and three measures of different constructs: the Inventory of Depressive Symptoms,58 the Perceived Stress Questionnaire,59 and the Revised Prenatal Distress Questionnaire.60 Traditional psychometric characteristics including internal validity and criterion (concurrent) validity were then examined. Internal reliability was characterized using Cronbach α statistic.61 Because we did not have the gold standard of a clinical interview, concurrent validity and indicators of diagnostic accuracy (e.g., sensitivity, specificity, and predictive value) were estimated by comparing the dichotomized ISQ to widely used indicators of insomnia (e.g., actigraphy and diary-assessed indicators of difficulty falling and staying asleep).54,56 Last, likelihood ratios (LR) were used to evaluate how effectively the ISQ performed as a diagnostic test. This approach has the advantage of being less likely to change with the prevalence of the disorder in different samples as compared to estimates of sensitivity and specificity.62 “LR positive” indicates how much more likely it would be to find a positive ISQ in those with insomnia compared to those without insomnia. Generally, LR values > 10 suggest a strongly positive result, ≥ 5–10 indicate a moderate result, ≥ 2–5 is a small result, and LR values of 1–2 suggest the questionnaire is noninformative.62
Insomnia estimates used to evaluate the validity of the ISQ were derived from three sources: PSQI, sleep diaries, and actigraphy. We dichotomized the PSQI global score at a cutoff of > 10 reflecting the values used in samples of insomnia subjects.63–65 The decision to use comparison values for SOL (≥ 31 min), WASO (≥ 31 min), and SE (< 85%) from the sleep diaries and PSG was based on assorted reports and suggestions for quantitative insomnia criteria.51,54,56 For the sleep diary and actigraphy data, the frequency of the sleep complaint was also gauged in accordance with the RDC: ≥ 3 times per week.51 These analyses were conducted with SPSS Version 21.0 (IBM SPSS Statistics for Windows, Version 21.0, IBM Corporation, Armonk, NY). A two-sided probability of < 0.05 was designated as a statistically significant association.
RESULTS
Sleep Characteristics
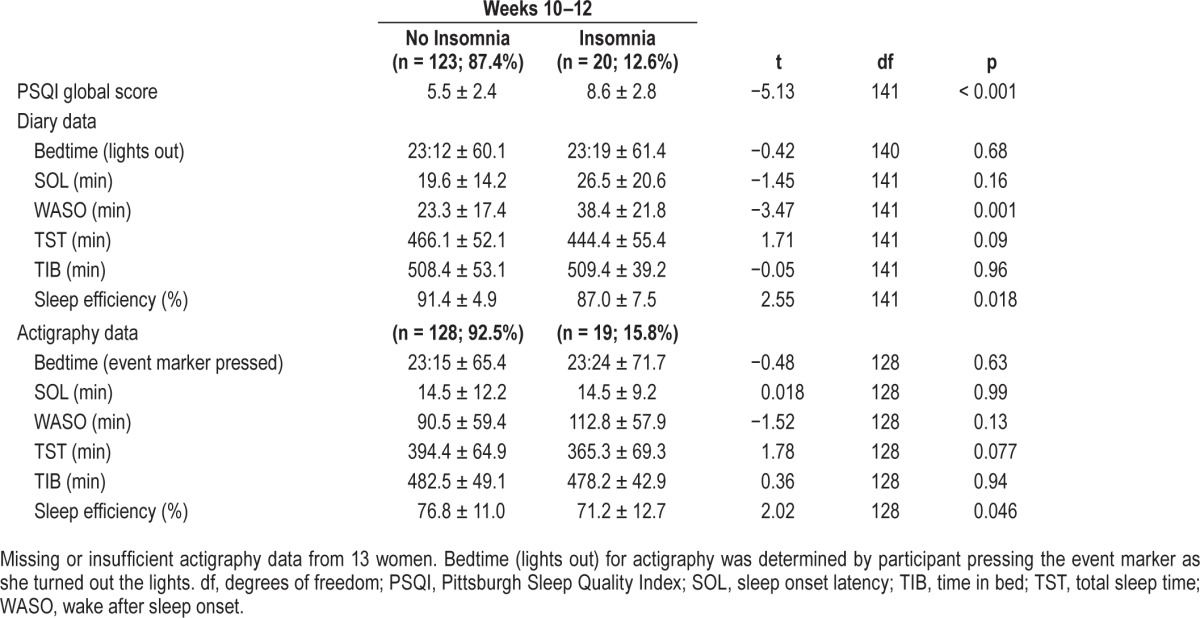
Participant characteristics are presented in Table 1. Twenty women (12.6%) women met diagnostic criteria for insomnia as defined by the ISQ. The women with insomnia were not statistically different from the women without insomnia on any of the participant characteristics. Upon further examination of the specific ISQ criteria, we observed 20 participants (14.0%) had one of the three sleep complaints at least three times per week, 81 (56.6%) with a sleep complaint indicated a duration of greater than 1 mo, and 27 (18.9%) noted significant daytime impairment as a result of the sleep complaint. The subjective and actigraphy-assessed sleep measures for participants by ISQ insomnia criteria are reported in Table 2. Women who were identified as having insomnia on the ISQ had higher PSQI scores, indicating poorer sleep quality (p < 0.001). They also had greater diary-assessed WASO (p = 0.001) and poorer diary and actigraphy-assessed SE (p = 0.018 and p = 0.046) than did women who were not identified as having insomnia on the ISQ.
Table 1.
Participant characteristics.
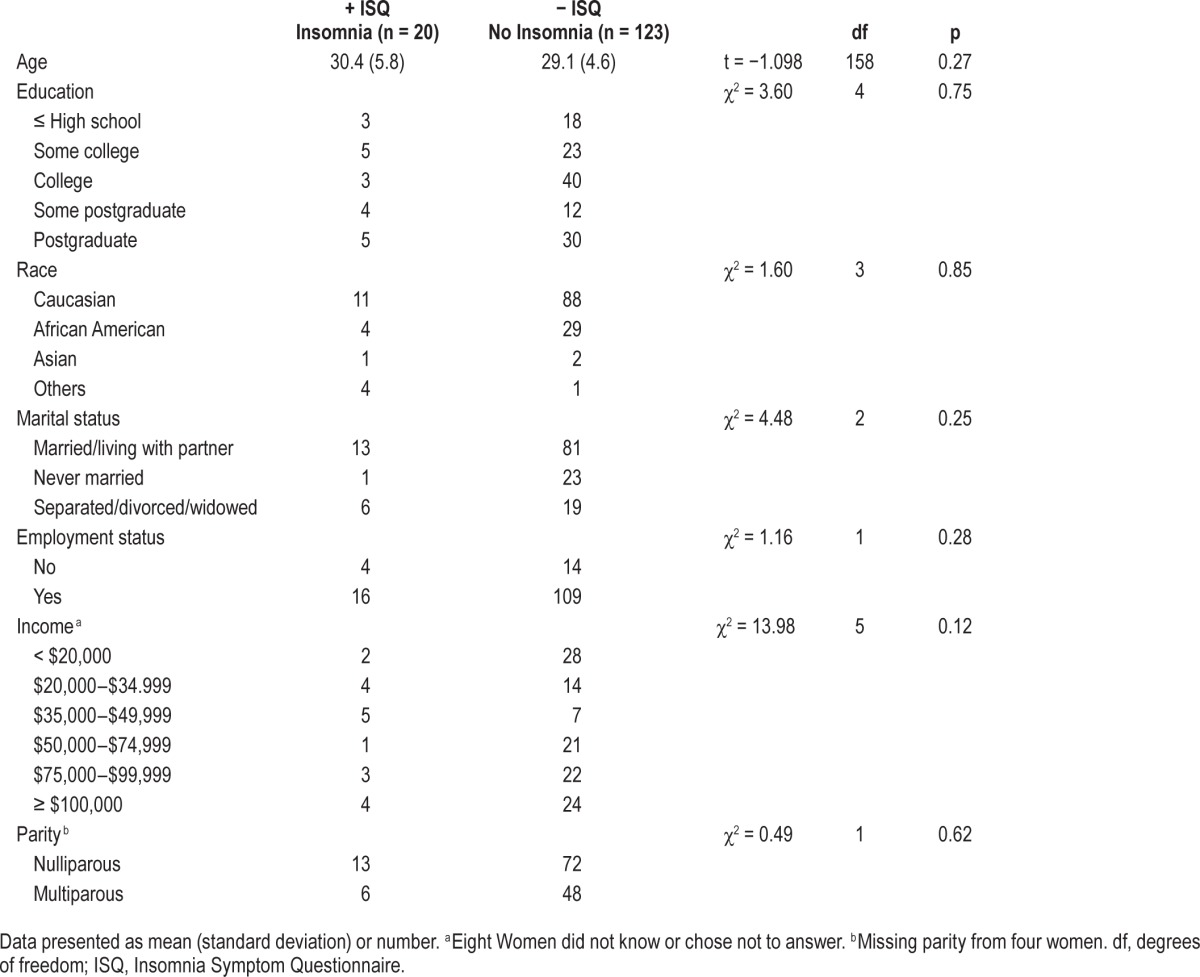
Table 2.
Subjective and actigraphic sleep characteristics for women who meet the case definition (insomnia) and women who do not meet the case definition (no insomnia) at 10–12 weeks gestation.
Psychometric and Test Characteristics
The 13-item ISQ had an overall reliability coefficient (Cronbach α) of 0.86 indicating a high degree of internal consistency.61 Correlations indicate modest discriminant validity as indicated by small magnitude, but significant correlations between the ISQ and the PSS (r = 0.14, p = 0.09), the New Prenatal Distress Questionnaire (NuPDQ) (r = 0.17, p = 0.06), and the IDS (minus the sleep items) (r = 0.20, p = 0.02). Although the goal would be to observe no significant correlations, given the high collinearity among the three constructs, the low discriminant validity is not surprising.
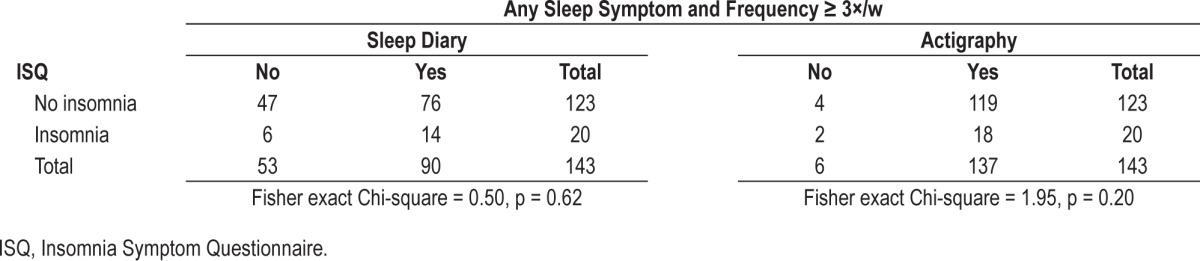
Criterion validity of the ISQ was assessed by examining the diagnostic accuracy of the ISQ outcome referenced to dichotomized PSQI scores and dichotomized estimates of SOL, WASO, and SE, and with and without frequency criteria considered, from sleep diary and actigraphy (Tables 3–7). Tables 4–7 indicate that the ISQ, when compared to a composite measure derived from the sleep diary consisting of SOL or WASO ≥ 31 min or SE < 85% and frequency of three or more times per week resulted in fewer true negatives. When comparing the dichotomized ISQ to other sleep measures, most specificities were high (all > 80%) except for diary-assessed SOL (≥ 31 min and three times per week = 62.5%) and any symptom derived from actigraphy (66.7%). Sensitivities (11.1–77.2%) were much more variable, indicating that the ISQ insomnia definition did not identify insomnia in the same manner in which the other sleep measures identify symptoms of insomnia. The wide range of positive predictive value similarly indicates that traditional sleep measures and methodologies differentially identified previously relied upon measures of insomnia (i.e. true and false positives).
Table 3.
Cross-tabulations between Pittsburgh Sleep Quality Index global score (cutoff > 10) and Insomnia Symptom Questionnaire classification of subjects who do and do not meet the case definition (insomnia) from 10–12 weeks.
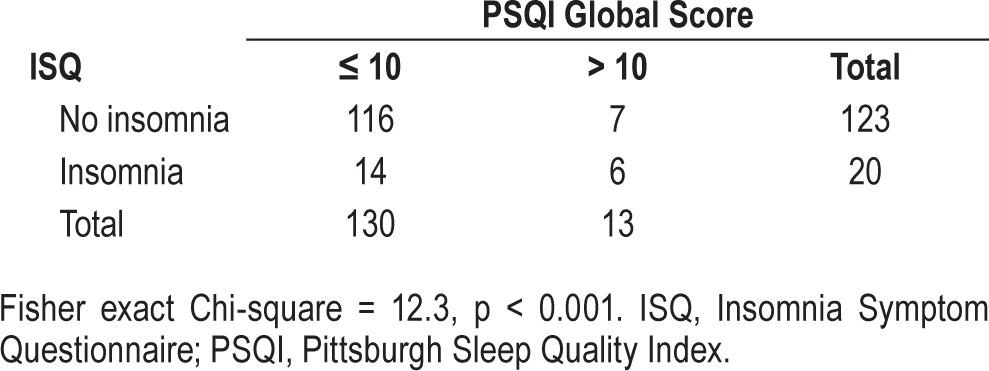
Table 4.
Cross-tabulations between sleep onset latency from sleep diary (≥ 31 minutes) and actigraphy (≥ 31 minutes) and Insomnia Symptom Questionnaire classification of subjects who do (insomnia) and do not meet the case definition (no insomnia) from 10–12 weeks.
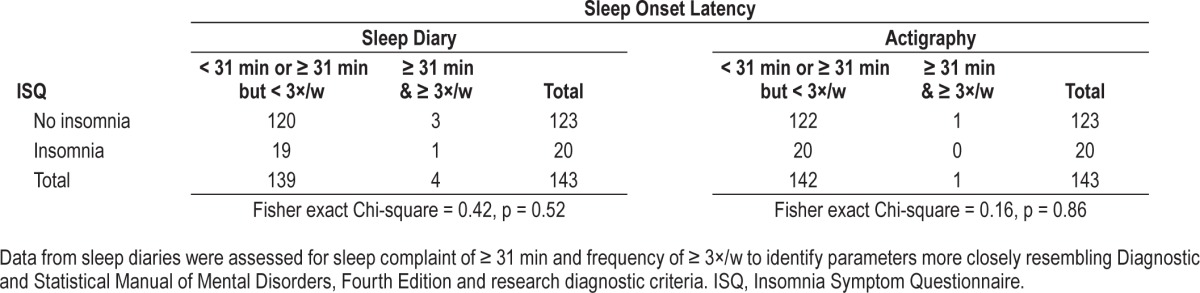
Table 5.
Cross-tabulations between wake after sleep onset from sleep diary (≥ 31 min) and actigraphy (≥ 31 min) and Insomnia Symptom Questionnaire classification of subjects who do (insomnia) and do not meet the case definition (no insomnia) at 10–12 weeks.
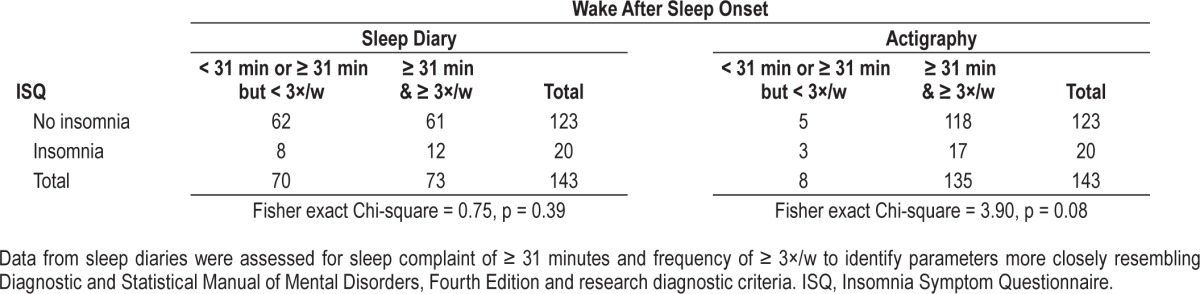
Table 6.
Cross-tabulations between sleep efficiency from sleep diary (≥ 85%) and actigraphy (≥ 85%) and Insomnia Symptom Questionnaire classification of subjects who do (insomnia) and do not meet the case definition (no insomnia).
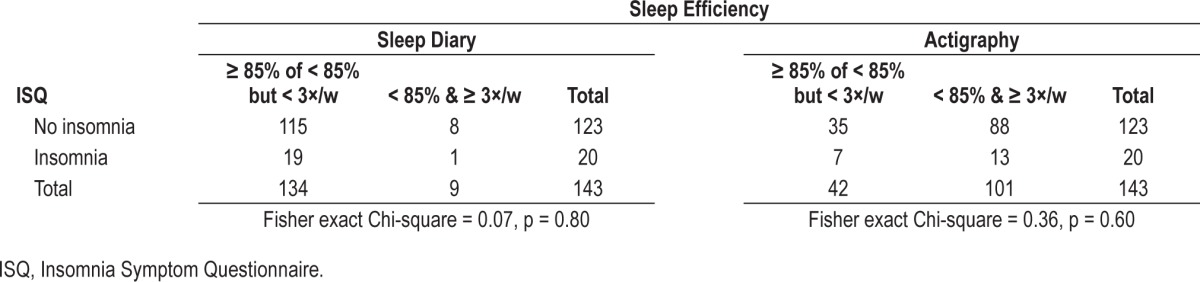
Table 7.
Cross-tabulations between any sleep symptom and Insomnia Symptom Questionnaire classifications of subjects who do (insomnia) and do not meet the case definition (no insomnia).
The LRs indicate that the ISQ is more similar to the PSQI and actigraphy-assessed WASO in its ability to identify who has insomnia (LRs > 5). The remaining measures based on the LRs ranging from 1 to 2 do not demonstrate the ISQ to be a useful measure for identifying insomnia as defined by the other methods (Table 8).
Table 8.
Evaluation of the Insomnia Symptom Questionnaire as a diagnostic screening tool.
DISCUSSION
In the current paper we psychometrically assessed the ISQ in pregnant women and identified the prevalence of insomnia in early gestation. The validation results were not as encouraging as we would have liked to observe. The validation criteria are not methods used to independently identify clinical insomnia; they are often used in conjunction with other measures or clinical interview. Thus, although sensitivities were low, this may be a function of the criteria. Our group previously validated this questionnaire in a cohort of midlife women45 with similar results. We identified 12.6% of pregnant women in early gestation, who self-reported no insomnia disorder upon enrollment, who subsequently met the diagnostic criteria for insomnia. These findings support previous evidence that pregnancy confers increased risk for the development of symptoms of insomnia that are analogous to a case-definition of insomnia.18,19,43 The utility of this tool in pregnancy may be to identify those with the most severe sleep problems that persist. This may be clinically relevant given the emerging evidence that sleep disturbance increases risk for adverse pregnancy outcomes.33,66,67
Insomnia is associated with significant morbidities including an increased risk for depression,18 stress,65,68 and inadequate or excessive gestational weight gain.69,70 Although depression and stress are well known consequences of insomnia, fewer studies have evaluated insomnia in relation to gestational weight gain. Women are expected to gain adequate weight to support the growing fetus.71 However, too little or too much weight gain can pose serious health threats, including gestational diabetes, hypertension, and metabolic irregularities, all of which can contribute to obesity.70,72,73 Each of these specific morbidities are important as they are independent risk factors for adverse pregnancy and infant outcomes, such as preterm birth, small- and large-for gestational-age infants, and future disease.14,74–77 Moreover, insomnia, depression,83,84 and stress85 are all independently associated with immune dysregulation. Several studies in the literature confirm that exaggerated inflammation, specifically chronic low-grade inflammation, is one biological pathway linked to adverse pregnancy outcomes.26,86–88
The majority of the research has focused on the third trimester when most women experience myriad physical and psychosocial changes. These include a dramatic increase in body size, physical discomfort, frequent need to urinate, nausea and backache, an increase in restless legs syndrome, as well as sleep disordered breathing.89,90 Psychosocially, a woman is often influenced by demands of life, work, and family. She may experience increased levels of stress and distress.44,91 All of these influences may disrupt sleep. However, we contend that an emphasis regarding sleep concerns should be placed on the first 20 w gestation. During this period, the consequences of insomnia, regardless of where they are derived, may have the most profound effect. Prior to 20 w a dominant proinflammatory profile is necessary for early pregnancy success. In vitro experiments in which cytokines inhibit trophoblast invasion, it is postulated that an exacerbated inflammatory response interferes with normal trophoblast invasion.92 This would result in subsequent disruption of the remodeling of the maternal vessels of the maternal vascular bed, an abnormality present in preeclampsia, preterm birth, and pregnancies with intrauterine growth restriction.33 These physiological processes are further affected by the remarkable fluctuations in immune and endocrine markers, especially inflammatory cytokines, progesterone, and estrogen, all of which have a substantial direct and indirect effect on sleep.93–100 We assert that there is a need to identify pregnant women with insomnia, especially in early pregnancy, because insomnia could increase the risk of adverse outcomes to the mother and to the developing fetus.33
The methods used to validate the ISQ (sleep diaries and/or actigraphy) are more commonly used than PSG when diagnosing insomnia, as well as when ascertaining sleep in pregnant women.66 Actigraphy is significantly correlated with PSG on most variables,101,102 but PSG only captures 1 to 2 nights of sleep which is insufficient to diagnose insomnia.103 Sleep diaries and actigraphy are commonly used to provide a detailed, prospective account about quantitative sleep disturbances and their variability.104 However, quantitative information alone is insufficient to diagnose insomnia as there must be concomitant daytime impairment.4 It is also well established that subjective and objective measures of sleep are often discrepant in patients with insomnia,105 which partially explains the low degree of agreement between the quantitative values derived from diary and actigraphy. The PSQI, however, has been validated to adequately identify insomnia even though it was not designed as a measure of insomnia.36 A benefit of the ISQ is that it incorporates criteria consistent with the DSM-IV and RDC criteria.
The presence of insomnia should not be viewed as an isolated symptom, especially in women. In many situations, insomnia may be the result of another primary disorder, such as obstructive sleep apnea, restless legs syndrome, or depression.106 The presence of comorbid sleep disorders may have negative consequences for outcomes.107 The identification of one or any of these disorders may require fundamentally different treatment options, such as pharmacologic treatment or behavioral intervention. A positive ISQ (indicating insomnia) might prompt the search for other comorbid conditions.
There are several strengths to this study. We have a large cohort of pregnant women recruited in early pregnancy who are ethnically and socioeconomically diverse. This increases the generalizability and utility of the ISQ. The short duration of the ISQ suggest that it could have substantial clinical applicability. Rather than collecting data over several weeks, identification could take place within a few minutes. The availability of 2 w of continuous sleep diary and actigraphy data afforded the opportunity to examine longer, more representative periods of sleep, compared to polysomnographic sleep studies, whose expense and participant burden limits data collection to fewer nights.103 A strength was the use of DSM-IV4 and RDC,104 which allowed for the identification of a case-definition of insomnia. However, since the inception of the ISQ new recommendations from DSM-5 and International Classification of Sleep Disorders, Third Edition have been published. This is particularly relevant to the duration of insomnia. The scoring algorithm will have to be revised to account for these changes.
We acknowledge limitations including the absence of a clinical diagnosis as a gold standard for further validation of the ISQ in pregnant women. A comparison of the ISQ with clinical interviews is needed. One such feasible comparison would be with the Brief Insomnia Questionnaire (BIQ), which is a 32-question fully structured interviewer-administered questionnaire developed using all diagnostic systems.108 Consistent with information gleaned during diagnostic interviews and from the BIQ, it might prove useful to include question(s) regarding opportunity/circumstances for sleep as the ISQ undergoes further refinement. This may become particularly salient when used in a postpartum sample. Inclusion of this item may improve its sensitivity since it is a criterion that is specific for the diagnosis of insomnia. The ISQ does not assess insomnia due to another medical or mental condition and because comorbidity was not evaluated in this report, it is possible that some of the women may have insomnia due to another medical or mental condition. Again, a positive ISQ could prompt a researcher or clinician to search for other conditions. We also acknowledge that the measures used to test for criterion and discriminant validity were insufficient because these constructs heavily overlap. Sleep diaries, the PSQI, and actigraphy only measure certain symptoms of insomnia. Thus, it is not surprising that the criterion validity was low. Likewise, stress and depression are predictors, as well as symptoms of insomnia, so we would expect discriminant validity to be poor.13 Additional instruments that are orthogonal to the ISQ are needed to further validate this measure in pregnant women.
In summary, we conducted a psychometric validation of the ISQ in a pregnancy cohort. We identified 12.6% of the sample as meeting diagnostic criteria for insomnia. Although the validation criteria were not as convincing as we might have liked, the data do suggest that in comparison with data collected from sleep diaries and actigraphy, the ISQ is a cost-effective self-report instrument with high utility for use in large observational studies as a screening instrument of insomnia.
Relevance to Clinical Practice
The incidence of insomnia varies depending on the strictness of the criteria used.109 Even when the most relaxed criteria are utilized, a strong association is detected between insomnia and adverse health outcomes.109 Given that pregnant women are at higher risk for experiencing insomnia,110 it is imperative to incorporate brief but accurate methods to identify insomnia in order to stave off additional risk for adverse pregnancy outcomes. In line with the Healthy People 2020 initiatives emphasizing prenatal care46 and sleep health,47 we contend that the ISQ would serve as ideal instrument and should be added to the prenatal care regiment. Ferraro and colleagues70 highlight that sleep may be a talking point for practitioners to assess and advise on during prenatal care. Currently, the allotted time for a new obstetrics patient, for example, is about 23 min, but in a survey of 705 obstetrics and gynecology physicians, the time they needed to adequately address sleep concerns, in addition to their other clinical responsibilities, was approximately 33 min.111 Currently, there is “no time” to talk about sleep in prenatal healthcare. If time were made, however, and a positive screen was ascertained, a clinician could provide a pamphlet on sleep and associated links for treatment options. This is already a standard practice for a variety of disorders, conditions, or procedures.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Buysse has served as a paid consultant on scientific advisory boards for Eisai, GlaxoSmithKline, Merck, Philips Respironics, Purdue Pharma, Sanofi-Aventis, and Takeda. He has also spoken at single-sponsored educational meetings for Sanofi-Aventis and Servier. The other authors have indicated no financial conflicts of interest. The work associated with this manuscript was conducted at the University of Pittsburgh, Pittsburgh, PA.
ABBREVIATIONS
- BIS
Bergen Insomnia Scale
- DSM-IV
Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition
- ISI
Insomnia Severity Index
- ISQ
Insomnia Symptom Questionnaire
- LR
likelihood ratio
- NuPDQ
New Prenatal Distress Questionnaire
- PNV
negative predictive value
- PPV
positive predictive value
- PTB
preterm birth
- PSQI
Pittsburgh Sleep Quality Index
- RDC
Research Diagnostic Criteria
- SE
sleep efficiency
- SOL
sleep onset latency
- TIB
time in bed
- TST
total sleep time
- WASO
wake time after sleep onset
- WHIRS
Women's Health Initiative Insomnia Rating Scale
REFERENCES
- 1.Okun ML, Kline CE, Roberts JM, Wettlaufer B, Glover K, Hall M. Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. J Womens Health (Larchmt) 2013;22:1028–37. doi: 10.1089/jwh.2013.4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okun ML, Coussons-Read ME. Sleep disruption during pregnancy: how does it influence serum cytokines? J Reprod Immunol. 2007;73:158–65. doi: 10.1016/j.jri.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Sleep Medicine. The International Classification of Sleep Disorders, Second Edition (ICSD-2): Diagnostic and Coding Manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 5.de Zambotti M., Covassin N, De Min TG, Sarlo M, Stegagno L. Sleep onset and cardiovascular activity in primary insomnia. J Sleep Res. 2011;20:318–25. doi: 10.1111/j.1365-2869.2010.00871.x. [DOI] [PubMed] [Google Scholar]
- 6.Farina B, Dittoni S, Colicchio S, et al. Heart rate and heart rate variability modification in chronic insomnia patients. Behav Sleep Med. 2014;12:290–306. doi: 10.1080/15402002.2013.801346. [DOI] [PubMed] [Google Scholar]
- 7.Althuis MD, Fredman L, Langenberg PW, Magaziner J. The relationship between insomnia and mortality among community-dwelling older women. J Am Geriatr Soc. 1998;46:1270–3. doi: 10.1111/j.1532-5415.1998.tb04544.x. [DOI] [PubMed] [Google Scholar]
- 8.Ancoli-Israel S. The impact and prevalence of chronic insomnia and other sleep disturbances associated with chronic illness. Am J Manag Care. 2006;12:S221–9. [PubMed] [Google Scholar]
- 9.Cheek RE, Shaver JL, Lentz MJ. Lifestyle practices and nocturnal sleep in midlife women with and without insomnia. Biol Res Nurs. 2004;6:46–58. doi: 10.1177/1099800404263763. [DOI] [PubMed] [Google Scholar]
- 10.Perlis ML, Smith LJ, Lyness JM, et al. Insomnia as a risk factor for onset of depression in the elderly. Behav Sleep Med. 2006;4:104–13. doi: 10.1207/s15402010bsm0402_3. [DOI] [PubMed] [Google Scholar]
- 11.Specchio LM, Prudenzano MP, de Tommaso M, et al. Insomnia, quality of life and psychopathological features. Brain Res Bull. 2004;63:385–91. doi: 10.1016/j.brainresbull.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Violani C, Lucidi F, Devoto A, Lombardo C, De Santo RM. Insomnia and its comorbidities in chronic kidney disease. Semin Nephrol. 2006;26:61–3. doi: 10.1016/j.semnephrol.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez-Mendoza J, Vgontzas AN. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep. 2013;15:418. doi: 10.1007/s11920-013-0418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009;166:557–66. doi: 10.1176/appi.ajp.2008.08081170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458–90. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 16.Graignic-Philippe R, Dayan J, Chokron S, Jacquet AY, Tordjman S. Effects of prenatal stress on fetal and child development: a critical literature review. Neurosci Biobehav Rev. 2014;43:137–62. doi: 10.1016/j.neubiorev.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 17.Lindgren K. Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health. 2001;24:203–17. doi: 10.1002/nur.1023. [DOI] [PubMed] [Google Scholar]
- 18.Dorheim SK, Bjorvatn B, Eberhard-Gran M. Insomnia and depressive symptoms in late pregnancy: a population-based study. Behav Sleep Med. 2012;10:152–66. doi: 10.1080/15402002.2012.660588. [DOI] [PubMed] [Google Scholar]
- 19.Kizilirmak A, Timur S, Kartal B. Insomnia in pregnancy and factors related to insomnia. Sci World J. 2012;2012:197093. doi: 10.1100/2012/197093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okun ML, Kiewra K, Luther JF, Wisniewski SR, Wisner KL. Sleep disturbances in depressed and nondepressed pregnant women. Depress Anxiety. 2011;28:676–85. doi: 10.1002/da.20828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krystal AD. Insomnia in women. Clin Cornerstone. 2003;5:41–50. doi: 10.1016/s1098-3597(03)90034-2. [DOI] [PubMed] [Google Scholar]
- 22.Gaunt G, Ramin K. Immunological tolerance of the human fetus. Am J Perinatol. 2001;18:299–312. doi: 10.1055/s-2001-17861. [DOI] [PubMed] [Google Scholar]
- 23.Hegde UC, Ranpura S, D'Souza S, Raghavan VP. Immunoregulatory pathways in pregnancy. Ind J Biochem Biophys. 2001;38:207–19. [PubMed] [Google Scholar]
- 24.Piccinni MP, Maggi E, Romagnani S. Role of hormone-controlled T-cell cytokines in the maintenance of pregnancy. Biochem Soc Trans. 2000;28:212–5. doi: 10.1042/bst0280212. [DOI] [PubMed] [Google Scholar]
- 25.Robinson DP, Klein SL. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Hormones Behav. 2012;62:263–71. doi: 10.1016/j.yhbeh.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wadhwa PD, Culhane JF, Rauh V, Barve SS. Stress and preterm birth: neuroendocrine, immune/inflammatory, and vascular mechanisms. Matern Child Health J. 2001;5:119–25. doi: 10.1023/a:1011353216619. [DOI] [PubMed] [Google Scholar]
- 27.Baratte-Beebe KR, Lee K. Sources of midsleep awakenings in childbearing women. Clin Nurs Res. 1999;8:386–97. doi: 10.1177/10547739922158377. [DOI] [PubMed] [Google Scholar]
- 28.Lee KA, Zaffke ME, McEnany G. Parity and sleep patterns during and after pregnancy. Obstet Gynecol. 2000;95:14–8. doi: 10.1016/s0029-7844(99)00486-x. [DOI] [PubMed] [Google Scholar]
- 29.Palagini L, Gemignani A, Banti S, Manconi M, Mauri M, Riemann D. Chronic sleep loss during pregnancy as a determinant of stress: impact on pregnancy outcome. Sleep Med. 2014;15:853–9. doi: 10.1016/j.sleep.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 30.Burton GJ, Woods AW, Jauniaux E, Kingdom JC. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta. 2009;30:473–82. doi: 10.1016/j.placenta.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Capeless EL, Clapp JF. Cardiovascular changes in early phase of pregnancy. Am J Obstet Gynecol. 1989;161:1449–53. doi: 10.1016/0002-9378(89)90902-2. [DOI] [PubMed] [Google Scholar]
- 32.Feinsilver SH, Hertz G. Respiration during sleep in pregnancy. Clin Chest Med. 1992;13:637–44. [PubMed] [Google Scholar]
- 33.Okun ML, Roberts JM, Marsland AL, Hall M. How disturbed sleep may be a risk factor for adverse pregnancy outcomes. Obstet Gynecol Surv. 2009;64:273–80. doi: 10.1097/OGX.0b013e318195160e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okun ML, Luther JF, Wisniewski SR, Sit D, Prairie BA, Wisner KL. Disturbed Sleep, a Novel Risk Factor for Preterm Birth? J Womens Health. 2011;21:54–60. doi: 10.1089/jwh.2010.2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levine DW, Kripke DF, Kaplan RM, et al. Reliability and validity of the Women's Health Initiative Insomnia Rating Scale. Psychol Assess. 2003;15:137–48. doi: 10.1037/1040-3590.15.2.137. [DOI] [PubMed] [Google Scholar]
- 36.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 37.Neau JP, Texier B, Ingrand P. Sleep and vigilance disorders in pregnancy. Eur Neurol. 2009;62:23–9. doi: 10.1159/000215877. [DOI] [PubMed] [Google Scholar]
- 38.Okun ML, Schetter CD, Glynn LM. Poor sleep quality is associated with preterm birth. Sleep. 2011;34:1493–8. doi: 10.5665/sleep.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Skouteris H, Wertheim EH, Germano C, Paxton SJ, Milgrom J. Assessing sleep during pregnancy: a study across two time points examining the Pittsburgh Sleep Quality Index and associations with depressive symptoms. Womens Health Issues. 2009;19:45–51. doi: 10.1016/j.whi.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 40.Strange LB, Parker KP, Moore ML, Strickland OL, Bliwise DL. Disturbed sleep and preterm birth: a potential relationship? Clin Exper Obstet Gynecol. 2009;36:166–8. [PubMed] [Google Scholar]
- 41.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 42.Swanson LM, Pickett SM, Flynn H, Armitage R. Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. J Womens Health (Larchmt) 2011;20:553–8. doi: 10.1089/jwh.2010.2371. [DOI] [PubMed] [Google Scholar]
- 43.Fernandez-Alonso AM, Trabalon-Pastor M, Chedraui P, Perez-Lopez FR. Factors related to insomnia and sleepiness in the late third trimester of pregnancy. Arch Gynecol Obstet. 2012;286:55–61. doi: 10.1007/s00404-012-2248-z. [DOI] [PubMed] [Google Scholar]
- 44.Manber R, Steidtmann D, Chambers AS, Ganger W, Horwitz S, Connelly CD. Factors associated with clinically significant insomnia among pregnant low-income Latinas. J Womens Health (Larchmt) 2013;22:694–701. doi: 10.1089/jwh.2012.4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Okun ML, Kravitz HM, Sowers MF, Moul DE, Buysse DJ, Hall M. Psychometric evaluation of the Insomnia Symptom Questionnaire: a self-report measure to identify chronic insomnia. J Clin. Sleep Med. 2009;5:41–51. [PMC free article] [PubMed] [Google Scholar]
- 46.US Department of Health and Human Services. Maternal, Infant, and Child Health. Washington, DC: US Department of Health and Human Services; 2014. http://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health. [Google Scholar]
- 47.US Department of Health and Human Services. Sleep Health. Washington, DC: US Department of Health and Human Services; 2014. http://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health. [DOI] [PubMed] [Google Scholar]
- 48.Grandner MA, Perlis ML. Insomnia as a cardiometabolic risk factor. Sleep. 2013;36:11–2. doi: 10.5665/sleep.2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I. Insomnia and the risk of incident heart failure: a population study. Eur Heart J. 2013;35:1382–93. doi: 10.1093/eurheartj/eht019. [DOI] [PubMed] [Google Scholar]
- 50.Okun ML, Tolge M, Hall M. Low socioeconomic status negatively affects sleep in pregnant women. J Obstet Gynecol Neonatal Nurs. 2014;43:160–7. doi: 10.1111/1552-6909.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27:1567–96. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 52.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 53.Monk TH, Reynolds CF, Kupfer DJ, et al. The Pittsburgh Sleep Diary. J Sleep Res. 1994;3:111–20. [PubMed] [Google Scholar]
- 54.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 55.Edinger JD. Classifying insomnia in a clinically useful way. J Clin Psychiatry. 2004;65:36–43. [PubMed] [Google Scholar]
- 56.Lineberger MD, Carney CE, Edinger JD, Means MK. Defining insomnia: quantitative criteria for insomnia severity and frequency. Sleep. 2006;29:479–85. doi: 10.1093/sleep/29.4.479. [DOI] [PubMed] [Google Scholar]
- 57.Natale V, Plazzi G, Martoni M. Actigraphy in the assessment of insomnia: a quantitative approach. Sleep. 2009;32:767–71. doi: 10.1093/sleep/32.6.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–83. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 59.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Social Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 60.Lobel M. State University of New York at Stony Brook; 1996. The Revised Prenatal Distress Questionnaire. [Google Scholar]
- 61.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–309. [Google Scholar]
- 62.Flemons WW, Whitelaw WA, Brant R, Remmers JE. Likelihood ratios for a sleep apnea clinical prediction rule. Am J Respir Crit Care Med. 1994;150:1279–85. doi: 10.1164/ajrccm.150.5.7952553. [DOI] [PubMed] [Google Scholar]
- 63.Backhaus J, Jughanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 64.Germain A, Moul DE, Franzen PL, et al. Effects of a brief behavioral treatment for late-life insomnia: preliminary findings. J Clin Sleep Med. 2006;2:403–6. [PubMed] [Google Scholar]
- 65.Hall M, Buysse DJ, Nowell PD, et al. Symptoms of stress and depression as correlates of sleep in primary insomnia. Psychosom Med. 2000;62:227–30. doi: 10.1097/00006842-200003000-00014. [DOI] [PubMed] [Google Scholar]
- 66.August EM, Salihu HM, Biroscak BJ, Rahman S, Bruder K, Whiteman VE. Systematic review on sleep disorders and obstetric outcomes: scope of current knowledge. Am J Perinatol. 2012;20:323–34. doi: 10.1055/s-0032-1324703. [DOI] [PubMed] [Google Scholar]
- 67.Haney A, Buysse DJ, Rosario BL, Chen YF, Okun ML. Sleep disturbance and cardiometabolic risk factors in early pregnancy: a preliminary study. Sleep Med. 2014;15:444–50. doi: 10.1016/j.sleep.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cuadros JL, Fernandez-Alonso AM, Cuadros-Celorrio AM, et al. Perceived stress, insomnia and related factors in women around the menopause. Maturitas. 2012;72:367–72. doi: 10.1016/j.maturitas.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 69.Abeysena C, Jayawardana P. Sleep deprivation, physical activity and low income are risk factors for inadequate weight gain during pregnancy: a cohort study. J Obstet Gynaecol Res. 2011;37:734–40. doi: 10.1111/j.1447-0756.2010.01421.x. [DOI] [PubMed] [Google Scholar]
- 70.Ferraro ZM, Chaput JP, Gruslin A, Adamo KB. The potential value of sleep hygiene for a healthy pregnancy: a brief review. ISRN Family Med. 2014;2014:928293. doi: 10.1155/2014/928293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Restall A, Taylor RS, Thompson JM, et al. Risk factors for excessive gestational weight gain in a healthy, nulliparous cohort. J Obes. 2014;2014:148391. doi: 10.1155/2014/148391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.American Congress of Obstetricians and Gynecologists (ACOG) Committee on Obstetric Practice; 2013. Obesity in Pregnancy. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Obesity-in-Pregnancy. [Google Scholar]
- 73.IOM. Weight Gain During Pregnancy. 2009. http://www.iom.edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines.aspx.
- 74.Austin MP, Leader L. Maternal stress and obstetric and infant outcomes: epidemiological findings and neuroendocrine mechanisms. Aust N Z J Obstet Gynaecol. 2000;40:331–7. doi: 10.1111/j.1479-828x.2000.tb03344.x. [DOI] [PubMed] [Google Scholar]
- 75.Djelantik AA, Kunst AE, van der Wal MF, Smit HA, Vrijkotte TG. Contribution of overweight and obesity to the occurrence of adverse pregnancy outcomes in a multi-ethnic cohort: population attributive fractions for Amsterdam. BJOG. 2012;119:283–90. doi: 10.1111/j.1471-0528.2011.03205.x. [DOI] [PubMed] [Google Scholar]
- 76.Field T, Diego M, Hernandez-Reif M, et al. Depressed pregnant black women have a greater incidence of prematurity and low birthweight outcomes. Infant Behav Dev. 2009;32:10–6. doi: 10.1016/j.infbeh.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Heude B, Thiebaugeorges O, Goua V, et al. Pre-pregnancy body mass index and weight gain during pregnancy: relations with gestational diabetes and hypertension, and birth outcomes. Matern Child Health J. 2012;16:355–63. doi: 10.1007/s10995-011-0741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cover H, Irwin M. Immunity and depression: insomnia, retardation, and reduction of natural killer cell activity. J Behav Med. 1994;17:217–23. doi: 10.1007/BF01858106. [DOI] [PubMed] [Google Scholar]
- 79.Irwin M, Clark C, Kennedy B, Christian GJ, Ziegler M. Nocturnal catecholamines and immune function in insomniacs, depressed patients, and control subjects. Brain Behav Immun. 2003;17:365–72. doi: 10.1016/s0889-1591(03)00031-x. [DOI] [PubMed] [Google Scholar]
- 80.Laugsand LE, Asvold BO, Vatten LJ, et al. Metabolic factors and high-sensitivity C-reactive protein: the HUNT study. Eur J Prev Cardiol. 2012;19:1101–10. doi: 10.1177/1741826711417758. [DOI] [PubMed] [Google Scholar]
- 81.Sakami S, Ishikawa T, Kawakami N, et al. Coemergence of insomnia and a shift in the Th1/Th2 balance toward Th2 dominance. Neuroimmunomodulation. 2002;10:337–43. doi: 10.1159/000071474. [DOI] [PubMed] [Google Scholar]
- 82.Savard J, Laroche L, Simard S, Ivers H, Morin CM. Chronic insomnia and immune functioning. Psychosom Med. 2003;65:211–21. doi: 10.1097/01.psy.0000033126.22740.f3. [DOI] [PubMed] [Google Scholar]
- 83.Benson S, Janssen OE, Hahn S, et al. Obesity, depression, and chronic low-grade inflammation in women with polycystic ovary syndrome. Brain Behav Immun. 2008;22:177–84. doi: 10.1016/j.bbi.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 84.Christian LM, Franco A, Glaser R, Iams JD. Depressive symptoms are associated with elevated serum proinflammatory cytokines among pregnant women. Brain Behav Immun. 2009;23:750–54. doi: 10.1016/j.bbi.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Coussons-Read ME, Okun ML, Nettles CD. Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain Behav Immun. 2007;21:343–50. doi: 10.1016/j.bbi.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 86.Challis JR, Lockwood CJ, Myatt L, Norman JE, Strauss JF, III, Petraglia F. Inflammation and pregnancy. Reprod Sci. 2009;16:206–15. doi: 10.1177/1933719108329095. [DOI] [PubMed] [Google Scholar]
- 87.El Shazly S, Makhseed M, Azizieh F, Raghupathy R. Increased expression of pro-inflammatory cytokines in placentas of women undergoing spontaneous preterm delivery or premature rupture of membranes. Am J Reprod Immunol. 2004;52:45–52. doi: 10.1111/j.1600-0897.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 88.Qiu C, Luthy DA, Zhang C, Walsh SW, Leisenring WM, Williams MA. A prospective study of maternal serum C-reactive protein concentrations and risk of preeclampsia. Am J Hypertens. 2004;17:154–60. doi: 10.1016/j.amjhyper.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 89.Facco FL. Sleep-disordered breathing and pregnancy. Semin Perinatol. 2011;35:335–9. doi: 10.1053/j.semperi.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 90.Lee KA. Sleep during pregnancy and postpartum. In: Lee-Chiong T, editor. Sleep Medicine: Essentials and Review. Oxford University Press; 2007. pp. 629–35. [Google Scholar]
- 91.Dorheim SK, Garthus-Niegel S, Bjorvatn B, Eberhard-Gran M. Personality and perinatal maternal insomnia: a study across childbirth. Behav Sleep Med. 2014 Aug 30; doi: 10.1080/15402002.2014.941063. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 92.Mor G. Inflammation and pregnancy: the tole of Toll-like teceptors in trophoblast-immune interaction. Ann N Y Acad Sci. 2008;1127:121–8. doi: 10.1196/annals.1434.006. [DOI] [PubMed] [Google Scholar]
- 93.Driver HS, Shapiro CM. A longitudinal study of sleep stages in young women during pregnancy and postpartum. Sleep. 1992;15:449–53. doi: 10.1093/sleep/15.5.449. [DOI] [PubMed] [Google Scholar]
- 94.Lancel M, Faulhaber J, Schiffelholz T, et al. Allopregnanolone affects sleep in a benzodiazepine-like fashion. J Pharmacol Exp Ther. 1997;282:1213–8. [PubMed] [Google Scholar]
- 95.Lancel M, Faulhaber J, Holsboer F, Rupprecht R. Progesterone induces changes in sleep comparable to those of agonistic GABAA receptor modulators. Am J Physiol. 1996;271:E763–72. doi: 10.1152/ajpendo.1996.271.4.E763. [DOI] [PubMed] [Google Scholar]
- 96.Luisi S, Petraglia F, Benedetto C, et al. Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients. J Clin Endocrinol Metab. 2000;85:2429–33. doi: 10.1210/jcem.85.7.6675. [DOI] [PubMed] [Google Scholar]
- 97.Pazos M, Sperling RS, Moran TM, Kraus TA. The influence of pregnancy on systemic immunity. Immunol Res. 2012;54:254–61. doi: 10.1007/s12026-012-8303-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Piccinni MP, Scaletti C, Maggi E, Romagnani S. Role of hormone-controlled Th1- and Th2-type cytokines in successful pregnancy. J Neuroimmunol. 2000;109:30–3. doi: 10.1016/s0165-5728(00)00299-x. [DOI] [PubMed] [Google Scholar]
- 99.Saaresranta T, Polo O. Hormones and breathing. Chest. 2002;122:2165–82. doi: 10.1378/chest.122.6.2165. [DOI] [PubMed] [Google Scholar]
- 100.Teran-Perez G, Arana-Lechuga Y, Esqueda-Leon E, Santana-Miranda R, Rojas-Zamorano JA, Velazquez MJ. Steroid hormones and sleep regulation. Mini Rev Med Chem. 2012;12:1040–8. doi: 10.2174/138955712802762167. [DOI] [PubMed] [Google Scholar]
- 101.McCall C, McCall WV. Objective vs. subjective measurements of sleep in depressed insomniacs: first night effect or reverse first night effect? J Clin Sleep Med. 2012;8:59–65. doi: 10.5664/jcsm.1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.McCall C, McCall WV. Comparison of actigraphy with polysomnography and sleep logs in depressed insomniacs. J Sleep Res. 2012;21:122–7. doi: 10.1111/j.1365-2869.2011.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.American Sleep Disorders Association. Practice parameters for the use of polysomnography in the evaluation of insomnia. Standards of Practice Committee of the American Sleep Disorders Association. Sleep. 1995;18:55–7. [PubMed] [Google Scholar]
- 104.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 105.Carskadon MA, Dement WC, Mitler MM, Guilleminault C, Zarcone VP, Spiegel R. Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. Am J Psychiatry. 1976;133:1382–8. doi: 10.1176/ajp.133.12.1382. [DOI] [PubMed] [Google Scholar]
- 106.Pavlova M, Sheikh LS. Sleep in women. Semin Neurol. 2011;31:397–403. doi: 10.1055/s-0031-1293539. [DOI] [PubMed] [Google Scholar]
- 107.Pien GW, Schwab RJ. Sleep disorders during pregnancy. Sleep. 2004;27:1405–7. doi: 10.1093/sleep/27.7.1405. [DOI] [PubMed] [Google Scholar]
- 108.Roth T, Coulouvrat C, Hajak G, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69:592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 109.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 110.Balserak BI, Lee K. Sleep disturbances and sleep-related disorders in pregnancy. In: Kryger MH, Roth T, Dement WC, editors. Principles and practices of sleep medicine. St. Louis: Elsevier; 2011. pp. 1572–86. [Google Scholar]
- 111.O'Connell VA, Youcha S, Pellegrini V. Physician burnout: the effect of time allotted for a patient visit on physician burnout among OB/GYN physicians. J Med PractManage. 2009;24:300–13. [PubMed] [Google Scholar]


