Sir,
Psychiatric morbidity is reported to be quite common in patients with diabetes mellitus (DM) and most of the studies have focused on depression. Diabetes and depression share a reciprocal relationship and it is suggested that these disorders often co-exist and one acts as a risk factor for development of the other1,2. Epidemiological data from uncontrolled studies suggest that 17.8 to 39 per cent of patients with type 2 diabetes mellitus (T2DM) suffer from depression3. Although there are variations across studies, data from controlled studies reveal that prevalence rate for depression in patients of T2DM is two-times more than that seen in those without diabetes mellitus3. The variations in the prevalence figures are mostly due to assessment methods used. Most studies have relied on self report questionnaire methods to ascertain the prevalence of depression4,5,6,7,8. Some studies have used scales like Hamilton Depression Rating scale (HDRS) for evaluation of depression and Hamilton Anxiety Rating scale for anxiety disorders6, which may not be appropriate scales for assessment of psychiatric morbidity in medically ill patients, considering the presence of higher somatic symptom load in patients with physical illnesses. Thus, there is a need to evaluate the presence of depression and other common mental disorders in patients with DM. There are little or no data available on the concordance in the diagnosis made on the basis of screening instruments and clinical assessment by a psychiatrist. With this background, this study was undertaken to evaluate the presence of common mental disorders in patients with diabetes mellitus by using a two - stage evaluation method, i.e.first evaluation as per the Patient Health Questionnaire (PHQ)9 and subsequently, as per ICD-10 (International Classification of Diseases - 10th revision) classification of mental and behavioural disorders10 based on a semi-structured interview by a qualified psychiatrist.
This study was conducted (in November-December 2011) in the Endocrinology Outpatient Clinic of Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, a tertiary care hospital in north India. Institute's ethics committee approved the study and the patients were recruited after obtaining written informed consent.
The inclusion criteria for the patients were age between 18-65 yr, established diagnosis of T2DM as per the criteria of American Diabetes Association11. Very sick patients and those who were not able to read Hindi were excluded.
Initially patients were assessed on the three page version of the PHQ9. The questionnaire has questions about symptoms and signs divided into eight diagnostic categories corresponding to specific DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, fourth edition) diagnoses12. These are threshold disorders corresponding to major depressive disorder, panic disorders, other anxiety disorders, bulimia nervosa and sub-threshold disorders such as other depressive disorders, probable alcohol abuse or dependence, somatoform and binge eating disorders. Patient's responses to the PHQ indicate to the physician of the diagnostic categories applicable to the patient. The evaluation by the physician can be done at any time during the encounter with the patient, but after the reasons for patient's visit are addressed to and before reviewing the PHQ, the physician notes whether the patient is new or established, types of current physical disorders and the physician's opinion about any current mental disorder in the patient. Before making a final diagnosis, the physician rules out any physical cause for psychiatric disorders9. For the study, Hindi translation of three-page questionnaire was used for screening as it covers the common mental disorders. This translated version of PHQ was developed at our centre using standardized methodology for translation13. ICD-10 classification of mental and behavioural disorders criteria were used by a qualified psychiatrist to make the possible axis-I psychiatric diagnosis in patients with diabetes mellitus10.
After documenting the socio-demographic and clinical data, patients with T2DM attending the Endocrinology Outpatient Clinic were initially asked to fill the Hindi version of the PHQ. Then these patients were evaluated by a qualified psychiatrist who was blind to the responses on the PHQ. Those found to have psychiatric disorder(s) as per the clinical assessment done by the psychiatrist were offered treatment for psychiatric morbidity.
Descriptive analysis was carried out using mean and standard deviation with range for continuous variables and in terms of frequency and percentages for discontinuous variables. For comparison of those with and without a psychiatric disorder, Pearson's Chi-square test or t test was used. Agreement between the diagnosis made by PHQ and the psychiatrist was studied by using kappa statistics.
The mean age of the patients was 50.5±9.6 yr with a range of 21-65 yr. The mean number of years of education was 10.2 ± 4.7 yr. There were nearly equal patients of either gender (male-48.9%; females-51.1%). Most of the patients were married (93.6%) and slightly more than two-third (69.6%) came from urban locality. The clinical profile of the patients is depicted in the Table.
Table I.
Psychiatric diagnosis as per patient Health Questionnaire (PHQ) and evaluation by psychiatrist in patients (n=280)
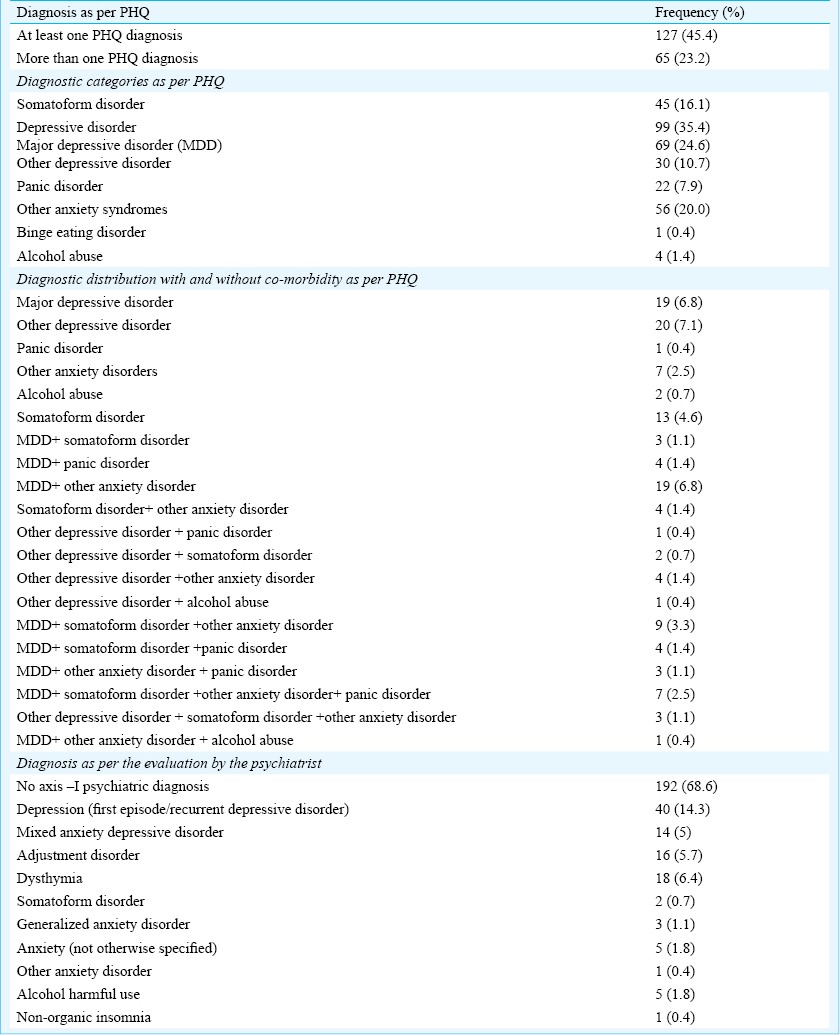
Of the 280 patients, both PHQ and the psychiatrist concurred for 143 patients having no psychiatric diagnosis, and for 95 cases having atleast one psychiatric diagnosis. However, in 10 patients no psychiatric diagnosis was made as per the PHQ, but the psychiatrist made a diagnosis. Conversely, for 32 cases who had a PHQ diagnosis, psychiatrist considered these patients to be free of any psychiatric morbidity. Overall, of the 280 cases, there was concurrence for 238 cases between the PHQ and the psychiatrist. The kappa value for measure of agreement between the two diagnostic methods was 0.693 (P<0.001).
When the diagnosis of depressive disorders (depressive episode, dysthymia, mixed depressive and anxiety disorder and adjustment disorder) as made by the psychiatrist was compared with PHQ diagnosis of major depressive disorder (MDD) and other anxiety disorders, the level of agreement was still high (Kappa value- 0.752; P<0.001).
The study sample was divided into two groups, i.e. those with and without psychiatric diagnosis as per the diagnosis made by the psychiatrist. Higher proportion of females had a psychiatric diagnosis (41.2% versus 21.2%; p<0.001). Those who had psychiatric illness had higher number of years of school education [10.7 ± 4.4 versus 9.0 ± 5.1; p<0.01] and heavier weight [71.8 ± 12.9 versus 67.8 ± 10.1; p<0.01]. Depression was more common in those with family income less than  19, 525 monthly (35.2 versus 18.8%; p<0.05).
19, 525 monthly (35.2 versus 18.8%; p<0.05).
When similar comparisons were made between those with depressive disorders (i.e. depressive episode, dysthymia, mixed depressive and anxiety disorder and adjustment disorder) and those with no psychiatric diagnosis, the two groups differed on the same variables, i.e. those with depressive disorders were more often females, had higher level of education and greater body weight.
Findings of the present study revealed that 31.4 to 45.4 per cent of patients with diabetes mellitus suffered from common mental disorders, depending on the assessment method used. Among the various psychiatric disorders, depressive disorders was most common and the rate of occurrence varied from 14.3 to 35.4 per cent, depending on the method used for making the diagnosis. These figures for depression were similar to that reported from other parts of the world11 and also from India4,5,6.
This study evaluated the concordance between the PHQ diagnosis and the diagnosis made by the qualified psychiatrists. A high level of concordance was found in this study between the PHQ diagnosis and the diagnosis made by the psychiatrist. This suggests that PHQ is a useful screening and diagnostic instrument in evaluating common mental disorders in patients with depression. In contrast to the multiple diagnoses on PHQ, the clinicians preferred to make a single diagnosis of mental disorder. Therefore, the clinicians (physicians) may use PHQ for screening, however, for confirmatory diagnosis they should rely on clinical interview. Lower percentage of psychiatric morbidity as per the psychiatrist's assessment suggests that there may be other clinical factors associated with glycaemic control which may mimic psychiatric symptoms and may be mistaken as symptoms of psychiatric disorders. Hence, careful assessment by the clinician and psychiatrist must be undertaken to reach to a psychiatric diagnosis in patients with diabetes mellitus. High psychiatric morbidity in females compared with males observed in this study was in concordance with the existing literature3,14.
To conclude, the present study demonstrated that about 30-45 per cent of patients with T2DM suffered from common mental disorders. Female gender and high body weight may be important risk factors for development of mental disorders. This study also showed that Hindi version of PHQ had good concordance for presence or absence of a psychiatric diagnosis with the ICD-10 diagnoses for group of depressive disorders made by a qualified psychiatrist. Therefore, PHQ can be used by busy physicians to screen patients of diabetes mellitus for common mental disorders. However, the psychiatrist should be consulted to confirm the diagnosis. The findings of the present study must be interpreted in the background of participants being recruited by purposive sampling.
References
- 1.Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49:837–45. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- 2.Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, et al. European Depression in Diabetes (EDID) Research Consortium. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53:2480–6. doi: 10.1007/s00125-010-1874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142(Suppl):S8–21. doi: 10.1016/S0165-0327(12)70004-6. [DOI] [PubMed] [Google Scholar]
- 4.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence & determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 5.Balhara YP, Sagar R. Correlates of anxiety and depression among patients with type 2 diabetes mellitus. Indian J Endocrinol Metab. 2011;15(Suppl 1):S50–4. doi: 10.4103/2230-8210.83057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaudhry R, Mishra P, Mishra J, Parminder S, Mishra BP. Psychiatric morbidity among diabetic patients: a hospital-based study. Indian Psychiatry J. 2010;19:47–9. doi: 10.4103/0972-6748.77637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaur G, Tee GH, Ariaratnam S, Krishnapillai AS, China K. Depression, anxiety and stress symptoms among diabetics in Malaysia: a cross sectional study in an urban primary care setting. BMC Fam Pract. 2013;14:69. doi: 10.1186/1471-2296-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Maier M, Wu J, Li W, Chen Y, Qin Y, et al. A descriptive and comparative study from China on patients with type-2 diabetes with and without depressive symptoms. J Community Health Nurs. 2013;30:106–15. doi: 10.1080/07370016.2013.778734. [DOI] [PubMed] [Google Scholar]
- 9.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care Evaluation of Mental Disorders. Patients Health Questionnaire JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization (WHO) Geneva: WHO; 1992. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. [Google Scholar]
- 11.Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–97. doi: 10.2337/diacare.20.7.1183. No author listed. [DOI] [PubMed] [Google Scholar]
- 12.American Psychiatric Association. 4th ed. Washington, DC: American Psychiatric Association; 1994. Diagnostic and statistical manual of mental disorders, DSM-IV. [Google Scholar]
- 13.Avasthi A, Varma SC, Kulhara P, Nehra R, Grover S, Sharma S. Diagnosis of common mental disorders by using PRIME-MD Patient Health Questionnaire. Indian J Med Res. 2008;127:159–64. [PubMed] [Google Scholar]
- 14.Leone T, Coast E, Narayanan S, de Graft Aikins A. Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): a mapping of the evidence. Global Health. 2012;8:39. doi: 10.1186/1744-8603-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]


