Abstract
Background
Recently a preoperative pain neuroscience education (NE) program was developed for lumbar surgery (LS) for radiculopathy as a means to decrease postoperative pain and disability. This study attempts to determine the short term effects, if any, of providing NE before surgery on patient outcomes.
Methods
A case series of 10 patients (female = 7) received preoperative one-on-one educational session by a physical therapist on the neuroscience of pain, accompanied by an evidence-based booklet, prior to LS for radiculopathy. Post-intervention data was gathered immediately after NE, as well as 1, 3 and 6 months following LS. Primary outcome measures were Pain Catastrophization Scale (PCS), forward flexion, straight leg raise (SLR) and beliefs regarding LS.
Results
Immediately following NE for LS for radiculopathy, all patients had lower PCS scores, with 5 patients exceeding the MDC score of 9.1 and 8 of the patients had PCS change scores exceeding the MDC by the 1, 3 and 6 month follow ups. Physical changes showed that fingertip-to-floor test in 6 patients had changes in beyond the MDC of 4.5 cm and 6 patients had changes in SLR beyond the MDC of 5.7°. The main finding, however, indicated a positive and more realistic shift in expectations regarding pain after the impending LS by all patients.
Conclusions
The results of the case series suggest that immediately after NE, patients scheduled for LS for radiculopathy had meaningful detectable changes in pain catastrophizing, fingertip-to-floor test, passive SLR and positive shifts in their beliefs about LS.
Keywords: pain, neuroscience, Education, Preoperative, Surgery
Introduction
It is estimated that between 10 – 40% of patients experience persistent pain and disability after lumbar discectomy for radiculopathy1–3 and postoperative rehabilitation has shown little effect on reducing the postoperative pain and disability. It has been proposed that preoperative education may decrease postoperative pain. The current preoperative counselling by orthopedic surgeons, including lumbar surgery (LS), utilize anatomical and biomechanical models for addressing pain and disability,7–11 which not only has shown limited efficacy, but may even increase patient fears, anxiety and stress, thus negatively impact their outcomes. Despite this, patients, including those with LS, are interested in knowing more about pain, and education strategies teaching patients about their pain have shown efficacy in easing pain and disability.
Recent research into educational strategies for patients with low back pain (LBP) shows an increased use of therapeutic neuroscience education (TNE). TNE aims to reduce pain and disability by helping patients gain an increased understanding of the biological and physiological processes involved in their pain experience. TNE differs from traditional education strategies by not focusing on anatomical or biomechanical explanations for pain, but rather on neurophysiology, neurobiology, processing and representation, and meaning of pain. It has been demonstrated that patients are capable of understanding the neurophysiology of pain, while professionals tend to underestimate their patient's ability to understand the “complex” issues related to pain.28 A recent systematic review suggests strong evidence for TNE addressing pain, disability and physical performance in musculoskeletal pain, particularly spinal disorders.20 Studies which utilized TNE have reported decreased fear and changes in patients’ perception of their pain;22 an immediate effect on improvements in patients’ attitudes about pain;29 improvements in pain, cognition and physical performance;9 increased pain thresholds during physical tasks;24 improved outcomes of therapeutic exercises;19 and significantly reduced widespread brain activity characteristic of a pain experience.23
Recently a preoperative neuroscience educational tool (PNET) was developed to explain LBP and lumbar radiculopathy to patients facing LS from a neurophysiological perspective.30 The PNET was based on previous TNE studies which have shown immediate post-education changes in cognitions regarding pain and threat, as well as physical performance in patients with chronic LBP. To date, no studies have assessed the ability of TNE to provide similar positive changes in patients following surgical management of their LBP. This case series sought to examine whether the PNET would result in immediate post-education changes in pain catastrophization, physical movements and expectations regarding the impending LS.
Materials and Methods
Subject Descriptions and Examinations
All patients provided written informed consent to participate in the study. This case series comprises data from 10 patients (7 female; average age 47.4 years) scheduled for non-instrumented lumbar decompressive surgery for lumbar radiculopathy with an average duration of leg pain of 7.3 months (range 2-23), average leg pain of 4.1 out of 10 on a numeric pain rating scale (NPRS) and average time to surgery of 9.5 days (range 2 – 28). Patient demographics can be found in Table 1.
Table 1.
Patient demographics prior to lumbar surgery for radiculopathy
| Patient | Age (years) | Gender | Duration of leg symptoms (months) | Leg pain rating (0-10 NPRS) | Wait time till surgery (days) |
|---|---|---|---|---|---|
| 1* | 50 | F | 4 | 6 | 6 |
| 2 | 70 | M | 2 | 8 | 7 |
| 3 | 51 | F | 8 | 9 | 2 |
| 4 | 24 | F | 12 | 3 | 9 |
| 5 | 47 | F | 23 | 4 | 2 |
| 6 | 70 | F | 8 | 6 | 28 |
| 7 | 27 | M | 3.5 | 2 | 8 |
| 8 | 55 | F | 3 | 2 | 8 |
| 9 | 30 | F | 3 | 0 | 15 |
| 10* | 50 | M | 6 | 1 | 10 |
| Average | 47.4 | 7.3 | 4.1 | 9.5 |
Indicates patient had previous lumbar surgery for radiculopathy
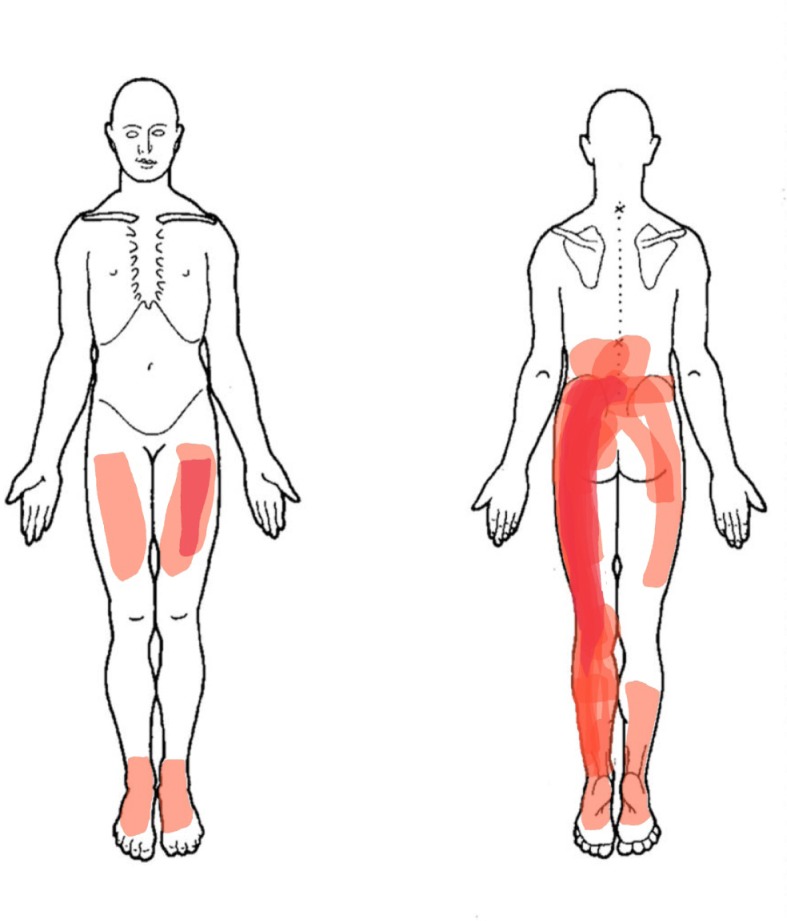
All patients presented with pain in the lower extremity (with radicular pain) with or without neurological symptoms such as numbness, pins and needles and weakness (Figure 1). Two patients (P1 and P10) had prior LS for radiculopathy (single-level discectomy).
Fig. 1.
Cumulative presentation of leg pain in the case series patient population.
Pre-education self-report measures
Prior to TNE and after completion of the consent and demographic intake forms, patients were asked to complete self-report surveys related to pain, function, fear avoidance, pain catastrophization, knowledge of pain and beliefs regarding surgical outcome.
Pain (Low Back and Leg) (Numeric Pain Rating Scale – NPRS): LBP and leg pain were measured with the use of a NPRS, as has been used in various RCTs for TNE and spinal pain. A change of 2.1 has been proposed as the minimal detectable change (MDC).33
Oswestry Disability Index (ODI): The ODI is a 10-item questionnaire that assesses different aspects of physical function. Each item is scored from 0 to 5, with higher values representing greater disability. The total score is multiplied by 2 and expressed as a percentage. The ODI has been shown to be a valid and reliable measure of disability related to LBP.34–36 A change of 5 points (10%) has been proposed as the minimal clinically important difference.37
Fear Avoidance Beliefs Questionnaire (FABQ): The FABQ is a 16-item questionnaire that was designed to quantify fear and avoidance beliefs in individuals with LBP. The FABQ has two subscales: 1) a 7-item scale to measure fear-avoidance beliefs about work and 2) a 4-item scale to measure fear avoidance beliefs about physical activity. Each item is scored from 0 to 6 with possible scores ranging between 0 and 24 and 0 and 42 for the physical activity and work subscales, respectively, with higher scores representing an increase in fear-avoidance beliefs. The FABQ has demonstrated acceptable levels of reliability and validity in previous LBP studies. Presence of avoidance behavior is associated with increased risk of prolonged disability and work loss. It is proposed that FABQ-W scores >34 and FABQ-PA >14 are associated with a higher likelihood of not returning to work.
Pain Catastrophization Scale (PCS): The PCS is a self-report questionnaire that assesses inappropriate coping strategies and catastrophic thinking about pain and injury. The PCS has been used in previous TNE studies for chronic LBP and demonstrated strong construct validity, reliability and stability.42 The PCS utilizes a 13-item, 5-point Likert scale with higher scores indicating elevated levels of catastrophizing. Previous studies utilizing the PCS have shown a median score of 18 that of healthy individuals and in patients with pain the PCS is generally higher.42 The minimal detectable change for the PCS is reported to be 9.1.43
Neurophysiology of Pain Questionnaire: Pain knowledge was measured by using a neurophysiology of pain questionnaire (NPQ), since it deals with the content of the TNE for this case series. The NPQ is based on a current pain science text 44 and was used in a previous study measuring the neurophysiology knowledge of patients and healthcare personnel.28 The NPQ is a 19-point questionnaire requesting ‘true’ or ‘false’ answers to statements, with the higher scores indicating more correct answers. The questionnaire used in this study is similar to the one used by Moseley28 and adapted slightly to make it easier for patients to understand, e.g., “nociception” was replaced with “danger messages.”
The results of the pre-education self-report measures are found in Table 2.
Table 2.
Patient self-report psychometric measures prior to therapeutic neuroscience education (TNE) and prior to lumbar surgery for radiculopathy
| Patient | ODI % | FABQ – W | FABQ – PA | PCS | NPQ |
|---|---|---|---|---|---|
| 1 | 44 | 0 | 23 | 27 | 13 |
| 2 | 44 | 10 | 10 | 21 | 15 |
| 3 | 48 | 31 | 17 | 47 | 12 |
| 4 | 48 | 23 | 22 | 22 | 13 |
| 5 | 18 | 12 | 18 | 11 | 12 |
| 6 | 48 | 10 | 15 | 24 | 12 |
| 7 | 36 | 38 | 23 | 28 | 12 |
| 8 | 74 | 0 | 24 | 47 | 15 |
| 9 | 26 | 19 | 22 | 23 | 10 |
| 10 | 22 | 15 | 13 | 4 | 15 |
| Average | 40.8 | 15.8 | 18.7 | 25.4 | 12.9 |
ODI: Oswestry Disability Index; FABQ-W: Fear Avoidance Beliefs
Questionnaire – Work Subscale; FABQ-PA: Fear Avoidance Beliefs
Questionnaire – Physical Activity Subscale; PCS: Pain Catastrophization
Scale; NPQ: Neurophysiology of Pain Questionnaire.
The pre-education measures revealed the patients in this series to have moderate LBP and leg pain; moderate disability (ODI > 40%);34–36 potential risk for not returning to work (FABQ-PA > 14); high levels of pain catastrophization (average PCS was 25.4); and limited knowledge of pain (NPQ).28
The 10 patients scheduled for LS for radiculopathy were also asked to rate their level of agreement on a 10-point scale (strongly disagree [0] – strongly agree [10]) with 7 statements regarding LS (Table 3). In response to the beliefs regarding LS, patients were ambivalent on 4 of the 7 questions (I am afraid of the upcoming surgery; I know what to expect after back surgery; back pain after surgery is expected; and I can control the amount of postoperative pain). Patients tended to agree that “back surgery will ‘fix my pain’; and “I feel prepared and ready for surgery.” They tended to disagree that “leg pain after surgery is to be expected.”
Table 3.
Patient self-report beliefs regarding lumbar surgery and their radiculopathy
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Average Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| I feel prepared and ready for surgery | 10 | 10 | 1 | 6 | 2 | 8 | 7 | 8 | 3 | 7 | 6.2 |
| I am afraid of the upcoming surgery | 2 | 6 | 4 | 9 | 10 | 1 | 3 | 8 | 5 | 5 | 5.3 |
| I know what to ex-pect after back surgery | 4 | 6 | 0 | 3 | 6 | 9 | 2 | 6 | 9 | 7 | 5.2 |
| Back pain after surgery is to be ex-pected | 5 | 2 | 0 | 8 | 8 | 8 | 8 | 6 | 2 | 7 | 5.4 |
| Leg pain after surgery is to be ex-pected | 5 | 2 | 0 | 7 | 7 | 2 | 7 | 0 | 0 | 4 | 3.4 |
| I can control the amount of post-op-erative pain | 5 | 8 | 3 | 8 | 6 | 8 | 3 | 2 | 5 | 7 | 5.5 |
| Back surgery will ‘fix my pain’ | 10 | 9 | 10 | 9 | 5 | 9 | 7 | 9 | 10 | 7 | 8.5 |
Scores are on a 10-point scale (strongly disagree [0] – strongly agree [10]) with each statement.
Pre-education physical performance
Prior to the preoperative TNE, 2 physical tests were performed: fingertip-to-floor test, measured from the longest finger on the dominant hand to the floor and passive straight leg raise (SLR), measured with an inclinometer placed on the tibial plateau 5cm distal to the inferior border of the patella on the most affected leg. Given the high levels of fear and potential provocative nature of forward flexion with herniated discs, active forward flexion was only performed once. The SLR measurements followed a standard protocol described previously. Physical measurement outcomes are shown in Table 4.
Table 4.
Physical examination findings prior to preoperative education.
| Patient | Fingertip-to-Floor (cm) | SLR (degrees) |
|---|---|---|
| 1 | 36.5 | 43 |
| 2 | 31.5 | 48 |
| 3 | 53 | 18 |
| 4 | 30 | 43 |
| 5 | 2 | 70 |
| 6 | 10.5 | 38 |
| 7 | 19.5 | 33 |
| 8 | 47 | 31 |
| 9 | −30* | 148* |
| 10 | 10 | 78 |
| Average | 21 | 55 |
Patient was a high-level professional dancer who could easily put her palms flat on the floor. A step was gradually increased until the patient had her longest finger, dominant hand just touch the floor. Step height (30 cm) was thus subtracted from a zero score (touching the floor).
Intervention: Preoperative Neuroscience Education
Details of the development of the PNET are described elsewhere;30 however, a brief description and more specifically, the delivery and content is described for this case series. After an extensive systematic review of the literature for RCTs, non-randomized clinical trials or case series evaluating the effect of TNE on pain, disability, anxiety and stress for musculoskeletal conditions, the evidence for TNE was established, and content and delivery methods were explored.20 The content of the TNE sessions, as found in the systematic review was used to develop appropriate messages for patients undergoing surgery for lumbar radiculopathy. The educational messages were designed to be delivered in one-on-one sessions to patients prior to LS for radiculopathy, along with the development of a patient booklet containing the same messages to provide patients with a written version of the content of the educational session.45 The primary focus of the preoperative TNE program was to help patients re-conceptualize their back, hip and leg pain as an increase in nerve sensitivity and up-regulation of the peripheral and central nervous system, at the same time defocusing attention from nociceptive input via the tissues from the affected areas. The TNE message thus aimed to reduce anxiety and uncertainty, and promote positive expectations and beliefs.
The structure of the developed TNE program consisted of six sections (Table 5). The PNET was designed to include prepared pictures, examples, and metaphors.46 The sensitivity of the nervous system metaphorically described as an alarm system46 accompanied with drawings of action potentials was used to describe peripheral sensitization, central sensitization, and plasticity of the nervous system. Face and content validity was established with an expert panel (spine surgeons, experts in TNE, pain management physicians, orthopedic nurses, physical therapists, psychologists and specialists in patient education), a convenience sample of patients who had recently undergone lumbar surgery for radiculopathy, as well as a convenience sample from the general population.47
Table 5.
Content of the Preoperative Neuroscience Educational Tool (PNET) program and booklet.
| Section | Topic | Main Theme |
|---|---|---|
| 1 | The decision to have back surgery | Several studies have shown that uncertainty prior to surgery is associated with poor outcomes. The purpose of the PNET is not to discourage surgery, but rather embrace the surgical decision and make positive choices associated with favorable recovery. |
| 2 | The nervous system's anatomy, physiology and pathways | The essence of TNE is explaining the biology and physiology of nerves to patients. The session aimed to make patients understand how nerves can be viewed as an alarm system aimed at providing information to the brain from the tissues. |
| 3 | Peripheral nerve sensitization | A key element of the preoperative neuroscience educational tool is for patients to understand that pain may be from faulty tissue but also (likely more so) from increased nerve sensitivity. The section aimed to have patients understand how the nervous system modulates sensitivity to protect when facing LBP, surgery, failed treatments, fear and anxiety. |
| 4 | Surgical experiences and environmental issues on nerve sensitivity | Several studies have indicated that the surgical experience is stressful, and this section aimed to make patients aware how surgery, hospital experiences, anxiety and interaction with medical personnel may increase sensitivity around the time of the surgery. |
| 5 | Calming the nervous system down | The patient is provided information on how the heightened nerve sensitivity can be decreased with the surgery, knowledge, movement and medication. Emphasis is placed on a knowledgeable brain down-regulating nociception and thus modulating the pain experience. |
| 6 | Recovery after back surgery | The last section summarized sections 1-5 with various explanations of what to expect during the recovery phase. |
| References | Scientific evidence for the booklet content | Patients were provided with a list of references titled as scientific evidence for the material in the preoperative neuroscience educational tool as a means to underscore the fact that the program is based on evidence and research. |
| Q & A Page | Questions to ask the surgeon prior to surgery | A Q & A page was provided at the end as a means to write down remaining questions to ask the surgeon prior to surgery. The fact that knowledge would help ease pain and uncertainty would likely increase pain was once again emphasized as a means to encourage patients to develop a greater understanding of what to expect before, during and after the surgical experience |
Table 5: Content of the Preoperative Neuroscience Educational Tool (PNET) program and booklet
Statistical Analysis
This was to a large degree a descriptive study. Descriptive statistics such as counts and percentages, frequency distributions, means, standard deviations and confidence intervals were used to describe variables. Some pre-specified comparisons were made between certain variables.
Results
Post-intervention data was gathered immediately after TNE (which lasted 30 minutes), as well as 1, 3 and 6 months following surgery. Two patients (patients P5 and P7) did not undergo surgery following the TNE session (P5 - medical complications; P7 - decided to opt out of surgery) but they were followed along with the other cases out to 6 months. One, 3 and 6 month data was collected via mailed, pre-paid postage envelopes containing surveys.
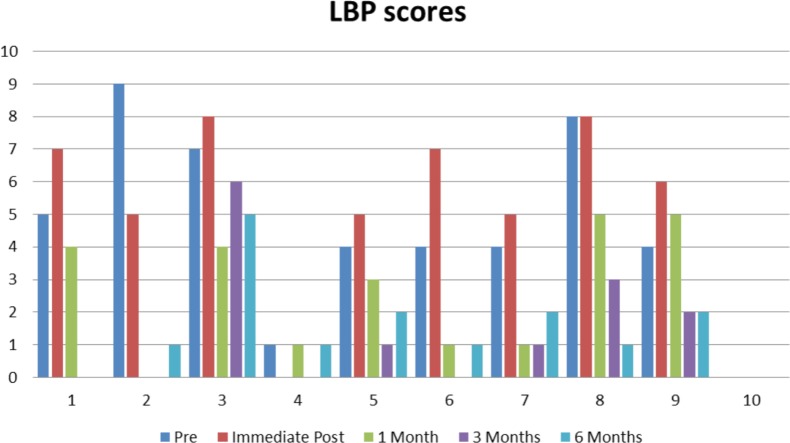
Low Back Pain
Six out of 10 patients reported higher pain scores for their low back immediately after the TNE; however, only one (patient P6) exceeded the minimally detectable change (MDC) of 2.1.33 (Figure 2) At the 1-month follow up, 8 patients reported less pain than at baseline and immediately following TNE, with 6 of them exceeding the MDC. At the 3 and 6 month follow ups, most patients (9 out of 10) had minimal to no back pain (≤ 2/10).
Fig. 2.
Low back pain (LBP) scores for all patients prior to therapeutic neuroscience education (TNE), immediately after and the 1, 3 and 6 month follow ups.
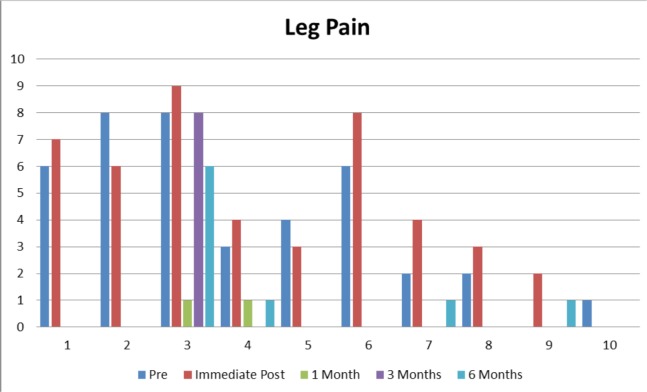
Leg Pain
Seven out of 10 patients reported higher pain scores for their leg (radiculopathy) immediately after the TNE; however, none exceeded the MDC (Figure 3). Most of the patients had no leg pain at the 1, 3 and 6 month follow ups.
Fig. 3.
Leg pain scores for all patients prior to therapeutic neuroscience education (TNE), immediately after and the 1, 3 and 6 month follow ups.
Fear Avoidance
For fear avoidance of physical activity (FABQ-PA), 7 patients reported an immediate decrease following TNE. Prior to TNE, 8 patients scored > 14 points associated with high likelihood not to return to work. Immediately after TNE 7 patients scored less than 14 points, while at 1, 3 and 6 months post-LS a 50% reduction on the high likelihood to not return to work due to FABQ-PA was reversed. For FABQ Work Subscale, pre-TNE scores were decreased by 25% immediately following TNE.
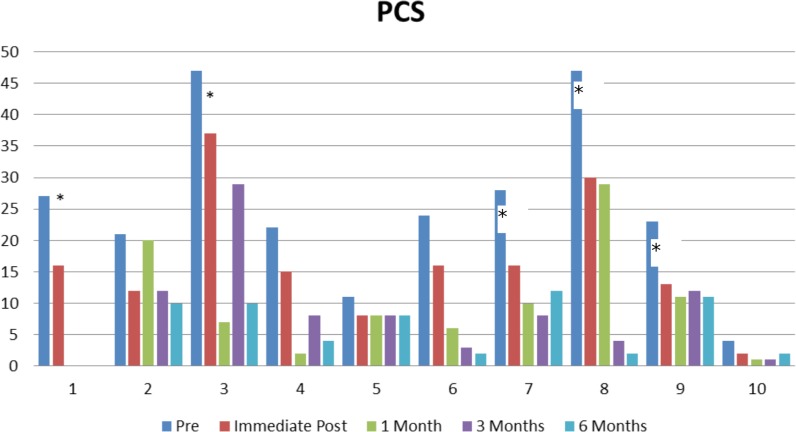
PCS
All patients had lower PCS scores immediately following the TNE, with 5 exceeding the MDC score of 9.1.43 (Figure 4) Eight of the 10 patients had PCS change scores exceeding the MDC by the 1, 3 and 6 month follow ups. Only patients 5 and 10, who started with low PCS scores (11 and 4 respectively) failed to show decreases in their scores beyond the MDC.
Fig. 4.
Pain Catastrophizing Scale (PCS) scores for all patients prior to therapeutic neuroscience education (TNE), immediately after and the 1, 3 and 6 month follow ups. * denotes change exceeded minimal detectable change (MDC) of 9.1 points.
NPQ
Immediately following TNE, patients improved their knowledge of the neurophysiology of pain from 12.9 out of 19 to 14.2, or an increase of 10%. This increase was maintained at 1, 3 and 6 months following LS.
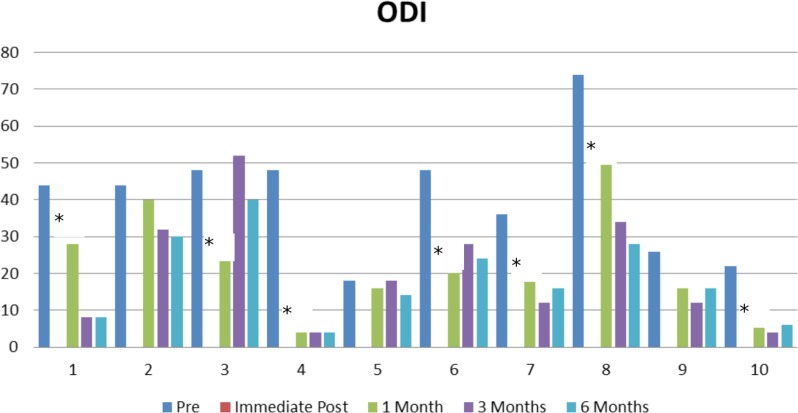
ODI
One month after surgery, 7 out of 8 patients had decreased ODI scores that exceeded the minimal detectable change of 10%. (Figure 5) Six of the patients continued improvement and reported ODI scores lower than 20% at 6 months post-surgery.
Fig. 5.
Oswestry Disability Index (ODI) scores for all patients prior to therapeutic neuroscience education (TNE), and at 1, 3 and 6 month follow ups. * denotes change exceeded minimal detectable change (MDC) of 10%.
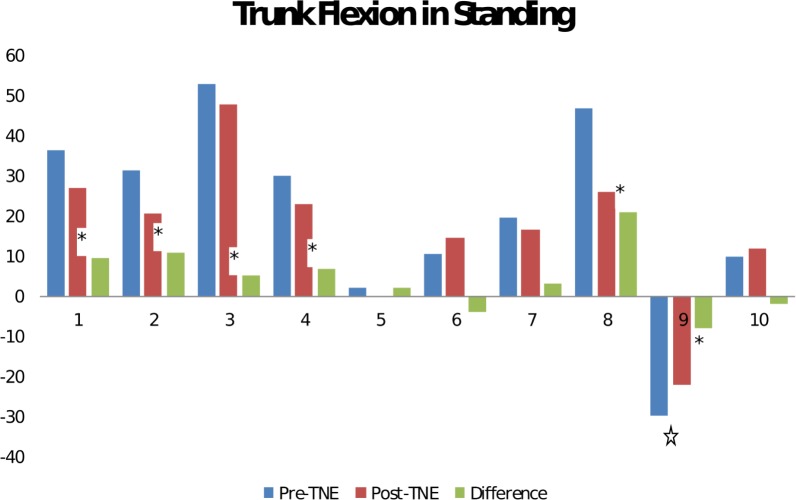
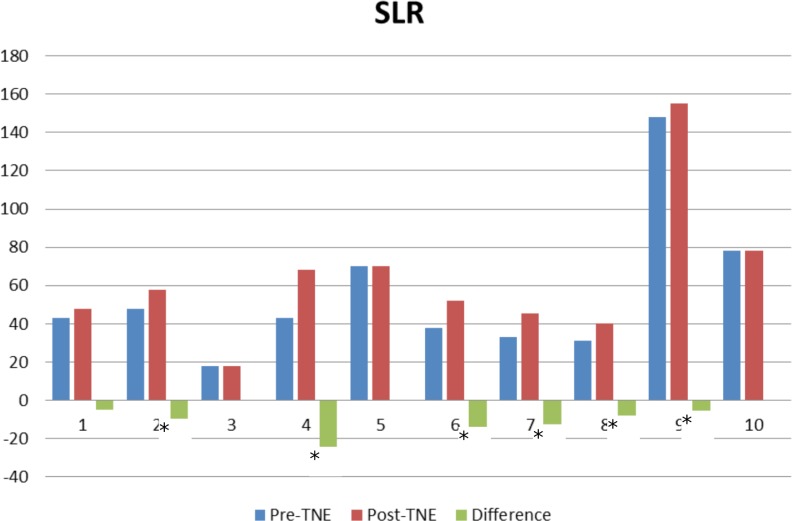
Physical Measurements
Physical changes were only measured before and immediately after TNE (30 minutes later). Six of the patients demonstrated changes in fingertip-to-floor test beyond the MDC of 4.5 cm.48 (Figure 6) Six of the patients demonstrated changes in SLR beyond the MDC of 5.7°(Figure 7).48
Fig. 6.
Fingertip-to-Floor Test measures for all patients prior to therapeutic neuroscience education (TNE), and immediately afterwards. * denotes change exceeded minimal detectable change (MDC) of 4.5 cm. Patient was a high-level professional dancer who could easily put her palms flat on the floor. A step was gradually increased until the patient had her longest finger, dominant hand just touch the floor. Step height (30 cm) was thus subtracted from a zero score (touching the floor).
Fig. 7.
Straight leg raise (SLR) for all patients prior to therapeutic neuroscience education (TNE), and immediately afterwards. * denotes change exceeded minimal detectable change (MDC) of 5.7 degrees.
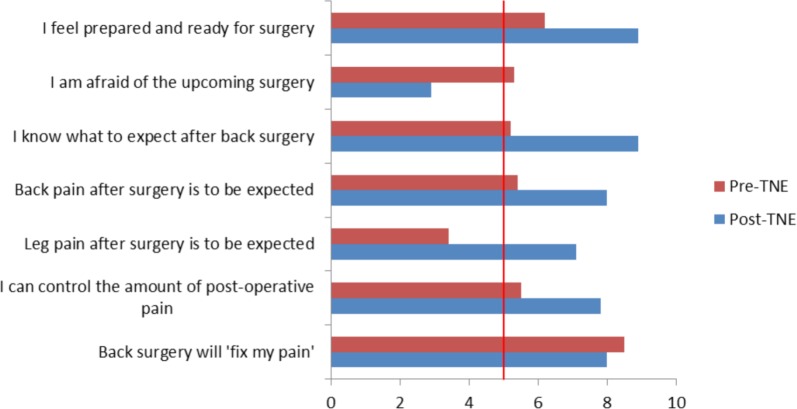
Beliefs and cognitions about surgery
The immediate changes in beliefs about lumbar surgery following TNE are presented in Figure 8. The results suggest positive shifts in patient beliefs about LS, and the impact of the surgery on their expected symptoms and recovery.
Fig. 8.
Patient self-report beliefs about lumbar surgery and their radiculopathy before and immediately after therapeutic neuroscience education (TNE). Scores below 5 indicate disagreement with the statements, whereas scores above 5 indicate agreement with the statements.
Discussion
The aim of this study was to measure the effects of preoperative TNE on symptoms, emotions and cognitions associated with lumbar radiculopathy. The results of this case series suggest that immediately after TNE, patients scheduled for LS for radiculopathy had detectable changes in pain catastrophizing, fingertip-to-floor test, passive SLR and positive shifts in their beliefs about LS. Although the majority of patients reported higher back and leg pain scores immediately after the TNE, most of the changes did not exceed the MDC and may not have represented true change. Previous studies have reported that TNE often produces no significant immediate changes in pain perception, although clinically, others have reported a slight increase in pain after TNE and attributed it to an increased awareness and discussion of pain, pain issues, and the word ‘pain’, which together may increase pain ratings.49
Although care should be taken in the analysis of a case series of patients with no control subjects, results demonstrated immediate positive changes following the application of TNE. The immediate changes in PCS and physical tests concur with previous studies using TNE for CLBP. At the core of TNE for patients with lumbar radiculopathy is a message to help patients realize the pain they experience is more likely due to nerve sensitization and the effect of various perioperative influences rather than a more mechanistic disc injury with resulting nerve irritation.
Disc herniation model descriptions have been associated with increased fear and anxiety,50–52 which has in turn been linked to limited movement and heightened increased irrational thoughts and coping strategies. Our results show that immediately after the TNE, all patients had lower scores for PCS which might be interpreted as them changing their catastrophic thinking about their pain and injury. This reconceptualization is further demonstrated by the ability of the patients to willfully engage in pushing further the fingertip-to-floor test, which has been shown to be very provocative in discogenic disorders and lumbar radiculopathy and also allow a clinician to move the involved lower extremity further (SLR). Both FABQ-W and FABQ-PA changed for the positive, while the PCS resulted in an immediate lowering of 6.5 points, which is similar to the statistically significant changes produced by Moseley et al. performing TNE in CLBP and measuring immediate post-education findings.24 Considering the PCS assesses inappropriate coping strategies and catastrophic thinking about pain and injury it could be argued that TNE aiming at re-conceptualizing pain cognitions are likely to have more of an immediate effect, whereas FABQ relates to physical tasks and work, which the newly acquired cognitions have not been able to be applied to. The one and three month data does show significant FABQ changes one and three months after surgery, which concurs with this possible explanation of the FABQ and PCS changes.
The largest effect however, occurred in patient beliefs regarding LS. Several studies have shown that beliefs and expected outcomes for surgery are highly correlated with predicting outcome following LS.55–58 The sample of patients in this case series displayed numerous poor beliefs regarding LS prior to TNE, associated with possible poor outcomes including beliefs of surgery “fixing” pain, expecting little to no pain after surgery, uncertainty about the surgery as well as unknown outcomes. Pain after surgery is to be expected and expectations of no pain after surgery are unrealistic.58 In a study interviewing patients one month after LS for radiculopathy, Louw et al. showed that patients who experienced pain after surgery expected to have some residual pain, and more than 50% indicated a true concern the pain would not go away, but rather increase.17 Immediately following the TNE, patients shifted their realistic expectations of back pain (back pain after surgery is to be expected), leg pain (leg pain after surgery is to be expected) and ability to control their own pain (I can control the amount of post-operative pain) by > 50%, thus preparing them for potential pain after surgery, which is more realistic. One and three month post-operative data indicated some patients were still experiencing pain, which coincided with persistent decreased psychometric measures of fear avoidance and pain catastrophizing.
The reconceptualization of pain and the pain experience is a key point. To date there have been several preoperative education studies used in orthopedic extremity surgery 12–14, 63 and spine surgery,59–61 mainly preparing patients for their surgery by explaining procedural information. Several RCT's and systematic reviews, however, have shown little to no effect in postoperative outcomes. The studies did show patients felt more prepared for the impending surgery, which concurs with the findings of this case series where patients feel more prepared for surgery (I feel prepared and ready for surgery; I know what to expect after surgery; and I am afraid of the upcoming surgery), but no postoperative changes in range of motion, pain, length of hospital stay or function. The one and three month postoperative data from this case series show a dramatic decrease in pain ratings and function. This addition of pain education to preoperative education concurs with the study by McDonald, where total joint arthroplasty patients were provided with pain science education and showed immediate postoperative pain reduction effects.21
Another very important potential implication of this case series is the delivery of preemptive TNE. To date TNE has been applied to various orthopedic and musculoskeletal patients, mainly CLBP.20 One weakness of a case series design is the lack of control patients. This case series, however, showed that patients who received TNE prior to LS had significant changes in LBP, leg pain, pain catastrophization, fear of work, fear of physical activity and function one month after surgery and these positive changes remain intact 2 months later (3 months after surgery). Given the fact that between 10 to 40% of patients following LS for radiculopathy experience persistent pain, loss of movement and disability,64 and postoperative rehabilitation has shown little effect in changing postoperative disability and pain TNE may provide a unique role for physical therapy and spine surgery patients. Furthermore, TNE may provide an additional lessening of pain and disability following LS for radiculopathy, with benefits for all stakeholders in the patient's outcome.
Limitations
Several limitations exist for this case series. Case series by design do not utilize a comparison group and the true effect of TNE compared to other interventions, or no intervention, is not known. The case series was specific to adults undergoing a selective surgical procedure for a specific condition. The possible effect of TNE on other kinds of surgery (i.e., fusions); younger patients; patients with other symptoms and indications for surgery are unknown.
Conclusion
In this case series, 10 patients scheduled for LS for radiculopathy underwent a preoperative TNE program resulting in immediate, 1 and 3 months postoperative clinically meaningful changes in pain, psychometric measures of pain catastrophizing and fear avoidance, function, physical movement and beliefs regarding LS. Although this case series does not suggest superior results to usual or no care, the intervention may be clinically effective in leading to preoperative and possible postoperative changes in lumbar radiculopathy patients undergoing surgery.
Disclosures
The authors report no financial disclosures.
References
- 1.Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine. 2003;28(6):616–620. doi: 10.1097/01.BRS.0000049927.37696.DC. [DOI] [PubMed] [Google Scholar]
- 2.Ostelo RW, de Vet HC, Waddell G, Kerckhoffs MR, Leffers P, van Tulder M. Rehabilitation following first-time lumbar disc surgery: a systematic review within the framework of the cochrane collaboration. Spine. 2003;28(3):209–218. doi: 10.1097/01.BRS.0000042520.62951.28. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296(20):2451–2459. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ostelo RW, Costa LO, Maher CG, de Vet HC, van Tulder MW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev. 2008;(4):CD003007. doi: 10.1002/14651858.CD003007.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Oshodi TO. The impact of preoperative education on postoperative pain. Part 1. Br J Nurs. 2007;16(12):706–710. doi: 10.12968/bjon.2007.16.12.23719. [DOI] [PubMed] [Google Scholar]
- 6.Oshodi TO. The impact of preoperative education on postoperative pain. Part 2. Br J Nurs. 2007;16(13):790–797. doi: 10.12968/bjon.2007.16.13.24244. [DOI] [PubMed] [Google Scholar]
- 7.Brox JI, Storheim K, Grotle M, Tveito TH, Indahl A, Eriksen HR. Systematic review of back schools, brief education, and fear-avoidance training for chronic low back pain. Spine J. 2008;8(6):948–958. doi: 10.1016/j.spinee.2007.07.389. [DOI] [PubMed] [Google Scholar]
- 8.Maier-Riehle B, Harter M. The effects of back schools--a meta-analysis. Int J Rehabil Res. 2001;24(3):199–206. doi: 10.1097/00004356-200109000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8(1):39–45. doi: 10.1016/S1090-3801(03)00063-6. [DOI] [PubMed] [Google Scholar]
- 10.Louw A, Butler DS, Diener I, Puentedura EJ. Preoperative education for lumbar radiculopathy: A Survey of US Spine Surgeons. International Journal of Spine Surgery. 2012;6:130–139. doi: 10.1016/j.ijsp.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Louw A, Diener I, Butler DS, Puentedura EJ. Preoperative education addressing postoperative pain in total joint arthroplasty: Review of content and educational delivery methods; Physiotherapy theory and practice; 2012. [DOI] [PubMed] [Google Scholar]
- 12.Koes BW, van Tulder MW, van der Windt WM, Bouter LM. The efficacy of back schools: a review of randomized clinical trials. J Clin Epidemiol. 1994;47(8):851–862. doi: 10.1016/0895-4356(94)90188-0. [DOI] [PubMed] [Google Scholar]
- 13.Waddell G. The Back Pain Revolution. Second ed. Edinburgh: Elsevier; 2004. [Google Scholar]
- 14.Nachemson AL. Newest knowledge of low back pain. A critical look. Clinical orthopaedics and related research. 1992;(279):8–20. [PubMed] [Google Scholar]
- 15.Poiraudeau S, Rannou F, Baron G, et al. Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain. 2006;124(3):305–311. doi: 10.1016/j.pain.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 16.Hirsch MS, Liebert RM. The physical and psychological experience of pain: the effects of labeling and cold pressor temperature on three pain measures in college women. Pain. 1998;77(1):41–48. doi: 10.1016/S0304-3959(98)00080-3. [DOI] [PubMed] [Google Scholar]
- 17.Louw A, Louw Q, Crous LCC. Preoperative Education for Lumbar Surgery for Radiculopathy. South African Journal of Physiotherapy. 2009;65(2):3–8. [Google Scholar]
- 18.Moseley GL, Hodges PW, Nicholas MK. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clinical Journal of Pain. 2004;20:324–330. doi: 10.1097/00002508-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297–302. doi: 10.1016/s0004-9514(14)60169-0. [DOI] [PubMed] [Google Scholar]
- 20.Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of physical medicine and rehabilitation. 2011;92(12):2041–2056. doi: 10.1016/j.apmr.2011.07.198. [DOI] [PubMed] [Google Scholar]
- 21.McDonald DD, Freeland M, Thomas G, Moore J. Testing a preoperative pain management intervention for elders. Res Nurs Health. 2001;24(5):402–409. doi: 10.1002/nur.1040. [DOI] [PubMed] [Google Scholar]
- 22.Moseley GL. Joining Forces - Combining Cognition-Targeted Motor Control Training with Group or Individual Pain Physiology Education: A Successful Treatment For Chronic Low Back Pain. Journal of Manual & Manipulative Therapy. 2003;11(2):88–94. [Google Scholar]
- 23.Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51(1):49–52. doi: 10.1016/s0004-9514(05)70053-2. [DOI] [PubMed] [Google Scholar]
- 24.Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–330. doi: 10.1097/00002508-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Ryan CG, Gray HG, Newton M, Granat MH. Pain biology education and exercise classes compared to pain biology education alone for individuals with chronic low back pain: a pilot randomised controlled trial. Man Ther. 2010;15(4):382–387. doi: 10.1016/j.math.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Louw A, Puentedura EL, Mintken P. Use of an abbreviated neuroscience education approach in the treatment of chronic low back pain: A case report; Physiotherapy theory and practice; 2011. [DOI] [PubMed] [Google Scholar]
- 27.Meeus M, Nijs J, Van Oosterwijck J, Van Alsenoy V, Truijen S. Pain Physiology Education Improves Pain Beliefs in Patients With Chronic Fatigue Syndrome Compared With Pacing and Self-Management Education: A Double-Blind Randomized Controlled Trial. Arch Phys Med Rehabil. 2010;91(8):1153–1159. doi: 10.1016/j.apmr.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 28.Moseley GL. Unraveling the barriers to reconceptualization of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. The Journal of Pain. 2003;4(4):184–189. doi: 10.1016/s1526-5900(03)00488-7. [DOI] [PubMed] [Google Scholar]
- 29.Moseley GL. A pain neuromatrix approach to patients with chronic pain. Man Ther. 2003;8(3):130–140. doi: 10.1016/s1356-689x(03)00051-1. [DOI] [PubMed] [Google Scholar]
- 30.Louw A, Butler DS, Diener I, Puentedura EJ. Development of a Preoperative Neuroscience Educational Program for Patients with Lumbar Radiculopathy; American journal of physical medicine & rehabilitation / Association of Academic Physiatrists; 2013. [DOI] [PubMed] [Google Scholar]
- 31.Louw A, Puentedura EJ, Mintken P. Use of an abbreviated neuroscience education approach in the treatment of chronic low back pain: A case report; Physiother Theory Pract; 2011. [DOI] [PubMed] [Google Scholar]
- 32.Moseley GL. Joining forces - combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap. 2003;11(2):88–94. [Google Scholar]
- 33.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89(1):69–74. doi: 10.1016/j.apmr.2007.08.126. [DOI] [PubMed] [Google Scholar]
- 34.Deyo RA, Battie M, Beurskens AJ, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976) 1998;23(18):2003–2013. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 35.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81(2):776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 36.Hakkinen A, Kautiainen H, Jarvenpaa S, Arkela-Kautiainen M, Ylinen J. Changes in the total Oswestry Index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007;16(3):347–352. doi: 10.1007/s00586-006-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 2008;33(1):90–94. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 38.Cleland JA, Fritz JM, Childs JD. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with neck pain. Am J Phys Med Rehabil. 2008;87(2):109–117. doi: 10.1097/PHM.0b013e31815b61f1. [DOI] [PubMed] [Google Scholar]
- 39.Grotle M, Vollestad NK, Brox JI. Clinical course and impact of fear-avoidance beliefs in low back pain: prospective cohort study of acute and chronic low back pain: II. Spine. 2006;31(9):1038–1046. doi: 10.1097/01.brs.0000214878.01709.0e. [DOI] [PubMed] [Google Scholar]
- 40.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82(10):973–983. [PubMed] [Google Scholar]
- 41.Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine. 1999;24(23):2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 42.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychological Assessment. 1995;7(4):524–532. [Google Scholar]
- 43.George SZ, Valencia C, Beneciuk JM. A psychometric investigation of fear-avoidance model measures in patients with chronic low back pain. The Journal of orthopaedic and sports physical therapy. 2010;40(4):197–205. doi: 10.2519/jospt.2010.3298. [DOI] [PubMed] [Google Scholar]
- 44.Wall PD, Melzack R. Textbook of Pain. 5th edn. London: Elsevier; 2005. [Google Scholar]
- 45.Louw A. Your Nerves Are Having Back Surgery. MInneapolis: OPTP; 2012. [Google Scholar]
- 46.Van Oosterwijck J, Nijs J, Meeus M, et al. Pain neurophysiology education improves cognitions, pain thresholds, and movement performance in people with chronic whiplash: a pilot study. J Rehabil Res Dev. 2011;48(1):43–58. doi: 10.1682/jrrd.2009.12.0206. [DOI] [PubMed] [Google Scholar]
- 47.McGregor AH, Burton AK, Sell P, Waddell G. The development of an evidence-based patient booklet for patients undergoing lumbar discectomy and un-instrumented decompression. Eur Spine J. 2007;16(3):339–346. doi: 10.1007/s00586-006-0141-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ekedahl H, Jonsson B, Frobell RB. Fingertip-to-floor test and straight leg raising test: validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Arch Phys Med Rehabil. 2012;93(12):2210–2215. doi: 10.1016/j.apmr.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 49.Wilson D, Williams M, Butler D. Language and the pain experience. Physiotherapy research international: the journal for researchers and clinicians in physical therapy. 2009;14(1):56–65. doi: 10.1002/pri.424. [DOI] [PubMed] [Google Scholar]
- 50.Sloan TJ, Gupta R, Zhang W, Walsh DA. Beliefs about the causes and consequences of pain in patients with chronic inflammatory or noninflammatory low back pain and in pain-free individuals. Spine. 2008;33(9):966–972. doi: 10.1097/BRS.0b013e31816c8ab4. [DOI] [PubMed] [Google Scholar]
- 51.Sloan TJ, Walsh DA. Explanatory and diagnostic labels and perceived prognosis in chronic low back pain. Spine (Phila Pa 1976) 35(21):E1120–1125. doi: 10.1097/BRS.0b013e3181e089a9. [DOI] [PubMed] [Google Scholar]
- 52.Butler DS, Moseley GL. Explain Pain. Adelaide: Noigroup; 2003. [Google Scholar]
- 53.Vlaeyen JW, Crombez G. Fear of movement/(re)injury, avoidance and pain disability in chronic low back pain patients. Man Ther. 1999;4(4):187–195. doi: 10.1054/math.1999.0199. [DOI] [PubMed] [Google Scholar]
- 54.Moseley GL. Reconceptualising pain according to modern pain science. Physical Therapy Reviews. 2007;12(3):169–178. [Google Scholar]
- 55.Toyone T, Tanaka T, Kato D, Kaneyama R, Ot-suka M. Patients’ expectations and satisfaction in lumbar spine surgery. Spine. 2005;30(23):2689–2694. doi: 10.1097/01.brs.0000187876.14304.15. [DOI] [PubMed] [Google Scholar]
- 56.Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res. 2008;466(5):1154–1161. doi: 10.1007/s11999-008-0194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ronnberg K, Lind B, Zoega B, Halldin K, Gellerstedt M, Brisby H. Patients’ satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine. 2007;32(2):256–261. doi: 10.1097/01.brs.0000251876.98496.52. [DOI] [PubMed] [Google Scholar]
- 58.McGregor AH, Hughes SP. The evaluation of the surgical management of nerve root compression in patients with low back pain: Part 2: patient expectations and satisfaction. Spine. 2002;27(13):1471–1476. doi: 10.1097/00007632-200207010-00019. discussion 1476-1477. [DOI] [PubMed] [Google Scholar]
- 59.Douglas TS, Mann NH, Hodge AL. Evaluation of preoperative patient education and computer-assisted patient instruction. J Spinal Disord. 1998;11(1):29–35. [PubMed] [Google Scholar]
- 60.LaMontagne L, Hepworth JT, Salisbury MH, Cohen F. Effects of coping instruction in reducing young adolescents’ pain after major spinal surgery. Orthop Nurs. 2003;22(6):398–403. doi: 10.1097/00006416-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 61.Walters M, Coad J. Preparation of children for spinal surgery: an exploratory study. Paediatr Nurs. 2006;18(10):27–29. doi: 10.7748/paed.18.10.27.s20. [DOI] [PubMed] [Google Scholar]
- 62.Johansson K, Nuutila L, Virtanen H, Katajisto J, Salantera S. Preoperative education for orthopaedic patients: systematic review. J Adv Nurs. 2005;50(2):212–223. doi: 10.1111/j.1365-2648.2005.03381.x. [DOI] [PubMed] [Google Scholar]
- 63.McDonald S, Hetrick S, Green S. Pre-operative education for hip or knee replacement. Cochrane Database Syst Rev. 2004;(1):CD003526. doi: 10.1002/14651858.CD003526.pub2. [DOI] [PubMed] [Google Scholar]
- 64.Ostelo RW, de Vet HC, Vlaeyen JW, et al. Behavioral graded activity following first-time lumbar disc surgery: 1-year results of a randomized clinical trial. Spine. 2003;28(16):1757–1765. doi: 10.1097/01.brs.0000083317.62258.e6. [DOI] [PubMed] [Google Scholar]
- 65.Ostelo RW, Costa LO, Maher CG, de Vet HC, van Tulder MW. Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev. 2004;(4):CD003007. doi: 10.1002/14651858.CD003007.pub2. [DOI] [PubMed] [Google Scholar]
- 66.Morris S, Morris TP, McGregor AH, Dore CJ, Jamrozik K. Function after spinal treatment, exercise, and rehabilitation: cost-effectiveness analysis based on a randomized controlled trial. Spine. 2011;36(21):1807–1814. doi: 10.1097/BRS.0b013e31821cba1f. [DOI] [PubMed] [Google Scholar]
- 67.McGregor AH, Dore CJ, Morris TP, Morris S, Jamrozik K. ISSLS prize winner: Function After Spinal Treatment, Exercise, and Rehabilitation (FASTER): a factorial randomized trial to determine whether the functional outcome of spinal surgery can be improved. Spine. 2011;36(21):1711–1720. doi: 10.1097/BRS.0b013e318214e3e6. [DOI] [PubMed] [Google Scholar]