Abstract
Background
Many studies have been developed to characterize the mechanical behavior of the intervertebral disc specifically for the lumbar spine and there have been limited studies done on the cervical spine with the goal to evaluate the strength of the cervical spine under compression without any information on the bulging of the intervertebral discs. The goal of the current study is to examine the deformation response of the cervical intervertebral disc classified with grade III or greater degeneration and analyze the relationship between axial deformation and anterior and posterior bulge under compression up to 550 N.
Methods
Each specimen was compressed for 3 cycles to a maximum load of 550N in steps of 50 N. The bulge was measured using Linear Variable Differential Transformers (LVDTs on an intact spinal segment, spinal segment with post laminectomy, and spinal segment post facetectomy.
Results
The anterior budge for an intact spinal segment shows a change of slope at loads of 262N±66N. For a physiological load of 250N the vertical displacement or spine segment height was reduced by 10.1% for an intact segment and 8.78% for the laminectomy and facetectomy configurations with F = 0.159 (Fcrit = 3.89) with no statistical difference observed. For the post laminectomy there was a decrease of 35% in anterior bulge compared to the intact specimen.
Conclusions
Our results show that for grade III disc degeneration the cervical segments bulging for both the laminectomy and facetectomy procedures are not significantly different. In post laminectomy the average anterior and posterior bulges are similar to the average anterior and posterior bulge post facetectomy.
Keywords: disc degeneration, Cervical Spine, Bulging, Laminectomy, Facetectomy
Introduction
The cervical spine is subject to many ailments. Radiculopathies, myelopathies, and many other disorders are often related to intervertebral disc (IVD) diseases. Neck and upper back pain affects mainly women, has a mean point prevalence of 14.4%, an estimated lifetime prevalence up to 5.6% in US1 and is mainly due to IVD degeneration. Intervertebral disc degeneration is a natural occurrence related to age.2 By the age of 70-80, there is a 100% prevalence of individuals with degenerative disc disease.3 Protrusions and prolapses can place pressure on the spinal cord or nerve roots and cause symptoms. Procedures such as laminectomies and facetectomies are done in an attempt to relieve the associated symptoms. These procedures are often performed on patients with various levels of disc degeneration. Gerard et al.4 reported, for patients with myelopathy from cervical stenosis, clinical improvement in 62.5% to 83% of cases adopting posterior decompression with either laminectomy or laminoplasty. Though outcomes are usually beneficial, these procedures alter the forces on the intervertebral discs, many of which are still not completely understood. IVD degeneration can be measured by the grading system of Pfirrmann et al.5 that provides a semi-quantitative evaluation of disc degeneration. Procedures such as facetectomies also give rise to questions such as stability of the spine. There is a general agreement that total removal of the facet produces an unstable situation. Due to the high prevalence of degenerative disc disease and the decrease in spinal stability after these operations it is important to study the effects of these procedures on the IVD.3, 6
Many studies have been developed to characterize the mechanical behavior of the intervertebral disc specifically for the lumbar spine, since in 1974, Keith Markolf completed a study in which 24 Functional Spinal Units (FSUs) without posterior elements were compressed to 1000 N which resulted in a vertical deformation of 0.7 mm.7 In 1978, a study done by J.S. Shah in which six specimens with two discs and three vertebral body segments were compressed used transducers to measure the bulge of the IVD when compressed to 490 N and 981 N and the amount of bulge was 0.4 mm and 0.6 mm respectively.8 A third lumbar study by Karl Wenger in 1997 took 16 FSU and compressed them from 100 N to 2500 N. The specimens were then measured for amount of bulge by imaging the specimen before loading and at maximum loading: the mean anterior bulge was found to be 0.37 mm±0.27 mm and range 0.07-0.91mm. It was found to have a mean lateral bulge of 0.65 mm±0.42 and range 0.09-1.29 mm.9 More recently advanced techniques to estimate disc bulging have been proposed.10–12 Heuer et al.12 used an effective laser scanning technique which provided some interesting results. The bulging of the cadaveric specimens tested ranged from 0.70mm to 0.87mm with a resolution of 25 µm under a compression of 500N. In contrast there have been limited studies done on the cervical spine with the goal to evaluate the strength of the cervical spine under compression and bending without any information on the bulging of the intervertebral discs. Moroney13 completed a study in which 35 cervical segments were tested and has found a compressional stiffness of 1317 N/mm, reduced by the dissection of the posterior elements in 492 N/mm. M. Shea14 on cervical spinal units specimens composed by two discs and three vertebral body segments with the posterior elements retained, has found at 300N in compression a vertical displacement of 4.7 mm at the failure load of 2158N±1055N. In another study by Przybyla15 in 2007, 22 cervical FSU were secured in aluminum cup with plaster and were compressed until failure found at 2400N±960N and characterized by an elastic limit of 1230N ±460N. Compared to previous studies, our current study takes both variables, vertical deformation and IVD bulge, into account and examined how an axial load on a cervical spinal segment, characterized with grade III or greater disc degeneration on the Pfirrmann grading system is associated with intervertebral disc bulge with posterior elements intact, after laminectomy, and after facetectomy. This study presents additional understanding of the properties and characteristics of the human cervical IVD. Results from this study can be used, for the level of degeneration considered, to evaluate the contribution of the residual IVD bulge in narrowing the intervertebral foramina provide insight for surgical procedures or the development of artificial discs, and help improve therapies for neck related injuries.
Materials and Methods
Specimen preparation
Five intact cervical spines obtained from subjects with age of 54±9 were sectioned into two FSUs: C3-C4 and C5-C6. The FSUs were cleaned of muscles and tendons but the IVDs and associated ligaments were left intact. The specimens were dissected such that a smooth level surface was prepared on the superior and inferior sides of the FSU to allow for symmetric and uniform load distribution. The specimens were stored frozen at -20° C and were thawed slowly in a refrigerator for 24 hours before testing. Each segment was prepared in three configurations according to the three consecutive phases of testing: in the first configuration, the FSUs were left intact (Figure 1a), the second configuration was obtained for dissection of the spinous process, simulating the laminectomy, (Figure 1b) than for sequential dissection was obtained the third configuration characterizing the facetectomy (Figure 1c).
Fig. 1.
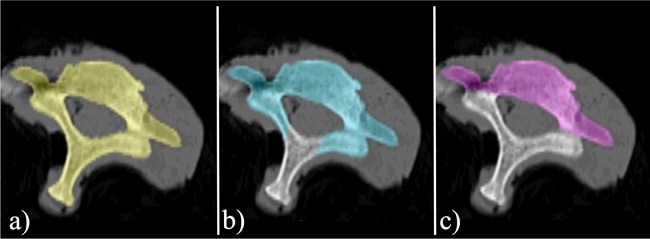
Three configurations adopted for each specimen: a) intact segment, b) laminectomy and c) facetectomy.
Biomechanical testing
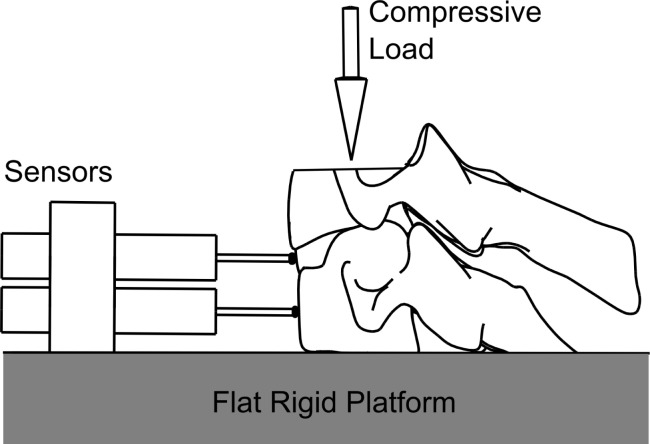
The specimens were placed, unconstrained, into an Instron electromechanical tensile-testing Machine 5569 (Instron, Norwood, MA). A preload of 50 N was applied before testing to ensure full contact and to minimize slippage of the specimen. Each specimen was compressed in the machine for 3 cycles for each maximum load. The maximum axial compressive load increased in the vertical direction from 100 N to 550 N, safe value imposed equivalent to the 45% of the elastic limit load found at 1230N±460N by Przybyla.15 All tests were conducted in steps of 50 N at a rate of 1 mm/min. The change in vertical deformation was measured using the values provided by the Instron machine at a frequency of 50 Hz and the repeatability across cycles between ±10% was assumed has indication of non-damaged specimen. The bulge was then measured using Linear Variable Differential Transformers (LVDTs) series 330 miniature AC (Trans-Tek, Inc. Ellington, CT) with accuracy of +/- 0.25% and nonlinearity less than 0.2% of full scale (Figure 2).
Fig. 2.
Diagram of Deformation and Load Directions. There was an axial load applied to the specimen the deformation was measured in the vertical and anterior directions.
For the first configuration, both LVDTs were placed in the anterior-posterior direction, on the segment C3-C4 one sensor was pointed on the posterior process measuring the rigid displacement of the segment (Figure 3) while the second sensor was measuring the anterior disc bulging, on the bigger segments C5-C6 the two sensors were both placed anteriorly were the rigid motion was evaluated trough the sensor on the vertebral body.
Fig. 3.
Experimental Set-up for Intact Cervical Spine. The anterior sensor measures anterior bulge, the posterior sensor tracks the displacement of the bone movement.
In the other two configurations, associated to the laminectomy and the facetectomy, where the posterior wall of the vertebral body was accessible an additional sensor, also with posterior-anterior direction was added to measure the posterior bulge (Figure 4).
Fig. 4.
Experimental Set-up for Cervical Spine Post Laminectomy, the additional sensor is added to measure the posterior bulge.
After the testing of all the specimens The FSUs were then sectioned along the sagittal plane (Figure 5) for gross analysis of the IVD in order to characterize the type or extent of failure if any. Gross histological analysis of the cadaver spinal units was done to observe tissue properties specific to specimens used. The Pfirrmann grading scale was used to determine the grade of disc degeneration in the spinal units. Specimens with grade III or greater degeneration were used.
Fig. 5.
Cervical Specimen in Axial Plane showing histological proporties of vertebra and intervertebral discs.
Each tested sample was characterized by an estimated axial elasticity EIVD defined as:
The load-deformation ratio was based on the slope of the initial linear portion of the load deformation curve in the axial direction. The reference disc height H0 was measured in the middle of the obtained sagittal section using a digital caliper Mitutoyo 500 series (Mitutoyo America Corp. Aurora, Il) with an accuracy of 0.02 mm. The flattened surface of the superior vertebral body was digitized and scaled to the sagittal and transversal width dimensions taken with the digital caliper. The Cross section area (CSA) was calculated as the area of the NURBS surface created on the digitized profile using Rhinoceros 3D (Robert McNeel & Associates, Seattle, WA).
Results
The vertebral bodies of the C5-C6 specimens had average sagittal dimension of 16.5mm±2.1mm and coronal of 26.25mm±1.8mm and they were bigger than the specimens C3-C4 characterized by sagittal thickness of 14.1mm±1.9mm and a coronal width of 21.7mm±3.2mm. The average cross sectional area (CSA) of all the specimens was found to be 296.25 mm2±49.8 mm2 with a range of 240 mm2 to 373 mm2. Dimensional measurements match with literature.16 Histological examination showed cervical spinal segment's intervertebral disc with a gray, inhomogeneous structure with unclear distinction between the nucleus and annulus. These were classified to have grade III degeneration.
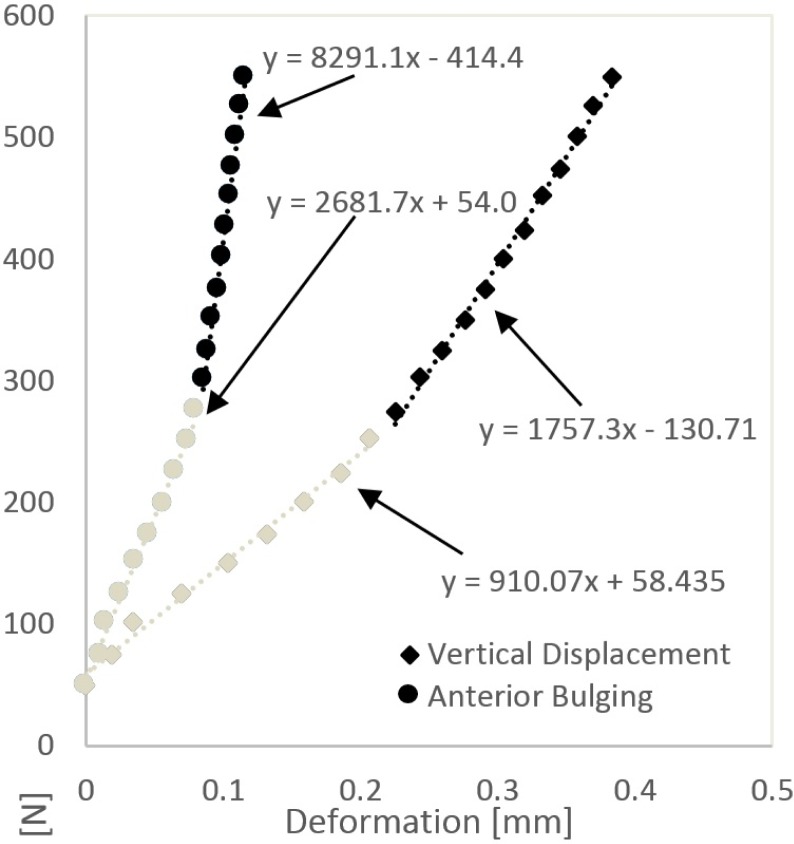
Results of one specimen were discarded because the specimen was compromised by the fracture of the superior endplate during the test on the laminectomy configuration. On the intact configurations the relationships of the applied load to the vertical deformation and to the anterior bulge showed a change in slope at loads of 262N±66N. On the average values the portions distinguished by the change in slope are almost linear R2=0.99 (Figure 6).
Fig. 6.
Experimental results of the intact configuration: Average values of Anterior Bulge (mm) and Vertical Deformation (mm).
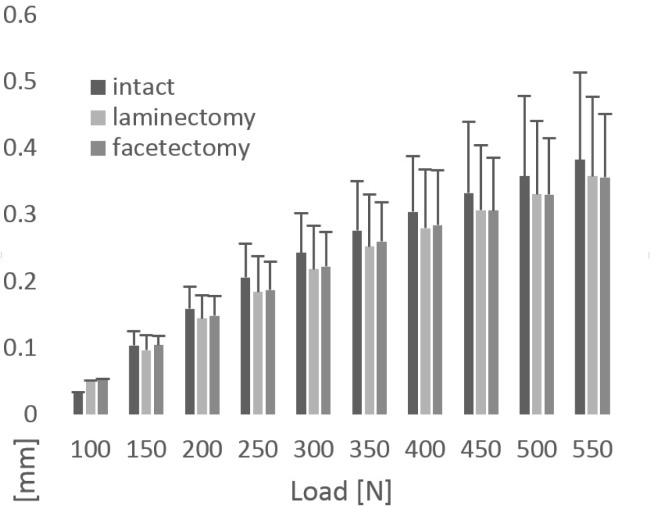
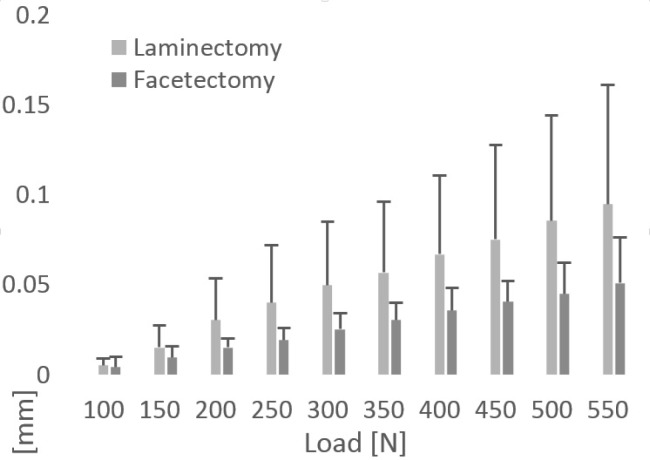
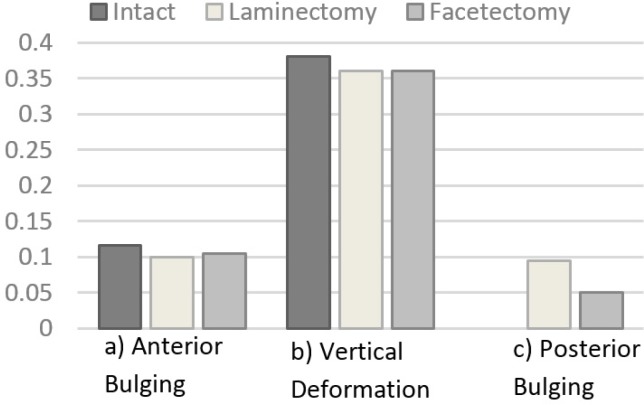
In the in Intact Configuration the average elasticity EIVD was found to be 19.5 MPa ±6.4 MPa for the C3-C4 segments and 14.4 MPa ±4.3MPa for C5-C6. The results from the study show that when an intact spinal segment containing a disc with grade III or greater degeneration is compressed with 550 N an average of 0.116mm±0.002mm anterior bulge occurs along with 0.382mm±0.128mm of vertical deformation or height change (Figure 7).
Fig. 7.
Average values of vertical Deformation (mm) for the three configurations, Standard deviation is shown with error bars for the intact case.
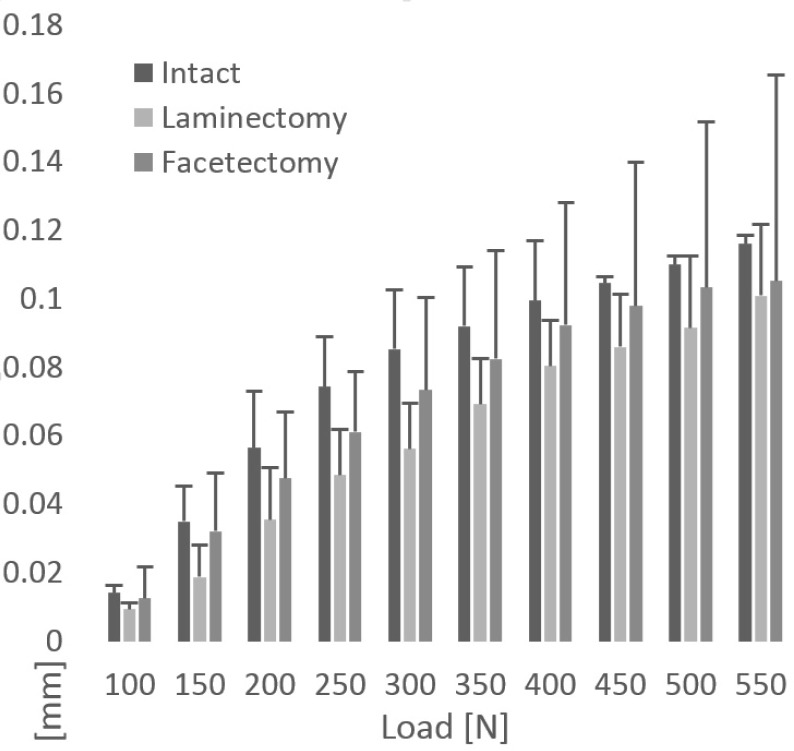
After the laminectomy was performed the same spinal segments showed an average anterior bulge of 0.102mm±0.020mm (Figure 8), posterior bulge of 0.095mm±0.070mm, and a vertical deformation of 0.357mm±0.131mm when compressed with 550 N. After a facetectomy was performed on the spinal segments an average anterior bulge of 0.105mm±0.06mm, posterior bulge of 0.051mm±0.025mm, and vertical deformation of 0.356mm±0.105mm were found (Figure 9).
Fig. 8.
Experimental results of the Anterior Bulge (mm) for the three: intact, laminectomy, and facetectomy.
Fig. 9.
Experimental results of the Posterior Bulge (mm) for both the laminectomy and facetectomy with posterior access.
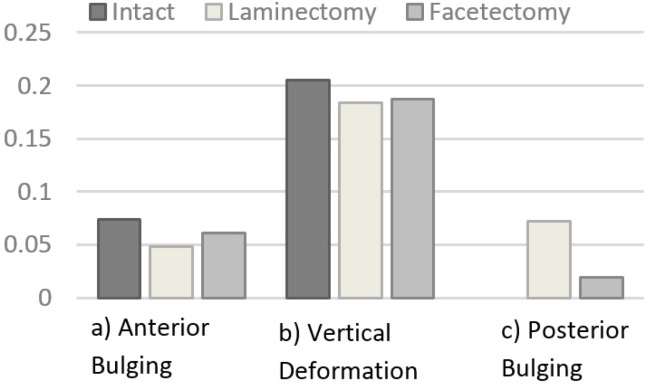
As reported by Patwardhan17, 18 a 250N is a physiologic compressive load during activities involving minimal to moderate isometric muscle effort the disc has an average vertical deformation of 0.205mm±0.060mm with an anterior bulge of 0.074mm±0.014mm that is reduced by 0.048mm±0.013mm and 0.061mm± 0.017mm in the laminectomy and facetectomy respective configurations.
Discussion
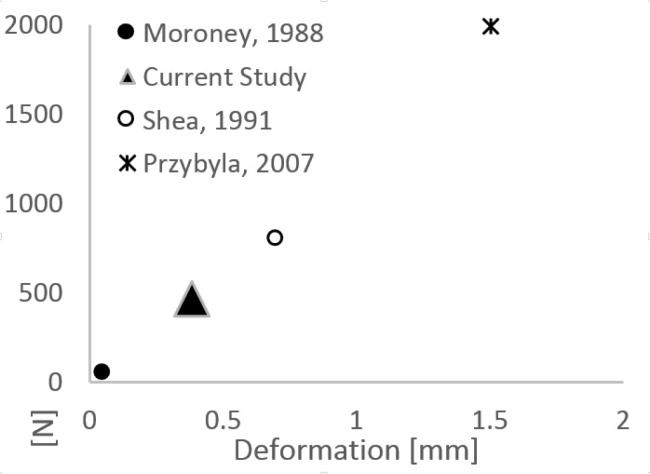
The values of vertical displacements found in this study, despite the disc degeneration are comparable with values previously reported in literature (Figure 10).
Fig. 10.
Comparison of current data with previous reported studies of the Vertical Deformation (mm).
Previous studies have investigated how laminectomy and facetectomy play a role in spinal stability and strength, many in the lumbar spine.19–22 This current study examined the effects of these procedures on the IVD in the cervical spine. The results show that performing a laminectomy reduced the anterior bulge of the spinal segments. However, after performing the facetectomy the anterior bulge increased by 35.1% compared to the laminectomy (Figure 11a) but this difference was not significant (F = 3.10). The posterior bulge decreased after facetectomy when compared to the laminectomy alone (Figure 11c). For a physiological load of 250N the vertical displacement or spine segment height was reduced by 10.1% for an intact segment and 8.78% for the laminectomy and facetectomy configurations with F = 0.159 (Fcrit = 3.89) showing no statistical difference (Figure 11b).
Fig. 11.
Analysis of Average values for the different Spinal segment configuration at a common physiological Load of 250 N (mm).
In a previous study with lumbar spinal segments it was shown that laminectomy procedures increase stress on the annulus fibers.23 Previous studies also examined the role of a facetectomy procedure on the lumbar spine.23–25 It has been shown that facetectomy alters the loading pathway and increases stress on the IVD which leads to an increase in its degeneration.26 The removal of the weight bearing facet joint was shown in the lumbar spine to alter the stress on the annulus of the IVD.26 Our results show a significant (F = 10.47, Fcrit = 5.12) decrease in vertical height for facetectomy followed by a decrease in posterior bulge compared to the posterior results post laminectomy (Figure 11c). These results suggest that there was a change in loading pattern between the laminectomy and facetectomy procedures that decrease posterior bulge and increased anterior bulge. The vertical deformation results show a 16.7% and 16.4% decrease after the laminectomy and facetectomy procedures, respectively (Figure 12b). At the maximal load of 550N no statistical differences were found in all the variables considered (Figure 12).In this study it was observed that the anterior bulge is limited to about 0.1 mm in the intact specimen for a certain loading range creating a plateau region while the axial (vertical) deformation increases; the bulge then continues to increase (Figure 6). A stiffening of the disc may be occurring. In the specimens post laminectomy there was a slight slope change around 450 N in the anterior bulge. No slope change was seen in the posterior bulge post laminectomy (Figure 9). After removal of the facet the IVD bulges in the anterior direction more than the posterior direction. The increase in anterior bulge after the facetectomy may be explained due to the thinner annulus in the posterior region. It was found in our study that facetectomy produced less posterior bulge then laminectomy under axial loads (Figure 11 and Figure 12). These results are found on spinal segments with at least grade III degeneration. Of the three variables considered we found statistical difference on the posterior bulge at 250N but considering that the standard deviation of 0.007mm was of the same order of the accuracy adopted, this difference should not be considered as significant.
Fig. 12.
Comparison of Bulging and vertical height deformation at maximal load of 550N.
In this study we found that the IVD in cervical spine segments with grade III or greater disc degeneration do not significantly alter their bulging pattern after laminectomy and facetectomy procedures. This may be due to the altered load distribution that occurs after these procedures. It was found that between laminectomy and facetectomy the anterior bulge increased and posterior bulge decrease. This study provides further insight into the load pattern and bulging of the degenerated disc and provides information for the spine surgical procedures and postoperative therapies to improve outcomes.
Disclosures
The authors declare no relevant disclosures.
References
- 1.Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010 Dec;24(6):783–92. doi: 10.1016/j.berh.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 2.Buckwalter JA. Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 1995;20:1307–14. doi: 10.1097/00007632-199506000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Krämer J. 3rd ed. Thieme Verlag; 2009. Intervertebral Disk Diseases: Causes, Diagnosis, Treatment, and Prophylaxis. [Google Scholar]
- 4.Gerard CS, O'Toole JE. Current techniques in the management of cervical myelopathy and radiculopathy. Neurosurg Clin N Am. 2014 Apr;25(2):261–70. doi: 10.1016/j.nec.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic Resonance Classification of Lumbar Intervertebral Disc Degeneration. Spine (Phila Pa 1976) 2001 Sep;26(17):1873–8. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 6.Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg. 1985 Aug;63(2):278–82. doi: 10.3171/jns.1985.63.2.0278. [DOI] [PubMed] [Google Scholar]
- 7.Markolf KL, Morris JM. The structural components of the intervertebral disc. A study of their contributions to the ability of the disc to withstand compressive forces. J Bone Joint Surg Am. 1974 Jun 1;56(4):675–87. [PubMed] [Google Scholar]
- 8.Shah JS, Hampson WG, Jayson MI. The distribution of surface strain in the cadaveric lumbar spine. J Bone Jt Surgery, Br. 1978 May 1;60-B(2):246–51. doi: 10.1302/0301-620X.60B2.659474. [DOI] [PubMed] [Google Scholar]
- 9.Wenger KH, Schlegel JD. Annular bulge contours from an axial photogrammetric method. Clin Biomech. 1997 Oct;12(7-8):438–44. doi: 10.1016/s0268-0033(97)00045-4. [DOI] [PubMed] [Google Scholar]
- 10.Spera D, Genovese K, Voloshin A. Application of Stereo-Digital Image Correlation to Full-Field 3-D Deformation Measurement of Intervertebral Disc. Strain. 2011 Jun 8;47:e572–87. [Google Scholar]
- 11.Cuchanski M, Cook D, Jegapragasan M, Whiting DM, Cheng BC. Measurement of disc bulge of the intervertebral disc: an in vitro study using human cadaver lumbar spine segments. ArgoSpine News J. 2010 Sep 1;22(2):73–80. [Google Scholar]
- 12.Heuer F, Schmidt H, Wilke H-J. The relation between intervertebral disc bulging and annular fiber associated strains for simple and complex loading. J Biomech. 2008 Jan;41(5):1086–94. doi: 10.1016/j.jbiomech.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Moroney S, Schultz A. Load-displacement properties of lower cervical spine motion segments. J Biomech. 1988;21(9):769–79. doi: 10.1016/0021-9290(88)90285-0. [DOI] [PubMed] [Google Scholar]
- 14.Shea M, Edwards W, White A, Hayes W. Variations of stiffness and strength along the human cervical spine. J Biomech. 1991;24(2) doi: 10.1016/0021-9290(91)90354-p. [DOI] [PubMed] [Google Scholar]
- 15.Przybyla AS, Skrzypiec D, Pollintine P, Dolan P, Adams MA. Strength of the cervical spine in compression and bending. Spine (Phila Pa 1976) 2007 Jul 1;32(15):1612–20. doi: 10.1097/BRS.0b013e318074c40b. [DOI] [PubMed] [Google Scholar]
- 16.Stemper BD, Yoganandan N, Pintar FA, Maiman DJ, Meyer MA, DeRosia J, et al. Anatomical gender differences in cervical vertebrae of sizematched volunteers. Spine (Phila Pa 1976) 2008 Jan 15;33(2):E44–9. doi: 10.1097/BRS.0b013e318160462a. [DOI] [PubMed] [Google Scholar]
- 17.Patwardhan AG, Havey RM, Carandang G, Simonds J, Voronov LI, Ghanayem AJ, et al. Effect of compressive follower preload on the flexion-extension response of the human lumbar spine. J Orthop Res. 2003 May;21(3):540–6. doi: 10.1016/S0736-0266(02)00202-4. [DOI] [PubMed] [Google Scholar]
- 18.Patwardhan AG, Havey RM, Ghanayem AJ, Diener H, Meade KP, Dunlap B, et al. Load-Carrying Capacity of the Human Cervical Spine in Compression Is Increased Under a Follower Load. Spine (Phila Pa 1976) 2000 Jun;25(12):1548–54. doi: 10.1097/00007632-200006150-00015. [DOI] [PubMed] [Google Scholar]
- 19.Zander T, Rohlmann A, Klöckner C, Bergmann G. Influence of graded facetectomy and laminectomy on spinal biomechanics. Eur Spine J. 2003 Aug;12(4):427–34. doi: 10.1007/s00586-003-0540-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bisschop A, Mullender MG, Kingma I, Jiya TU, van der Veen AJ, Roos JC, et al. The impact of bone mineral density and disc degeneration on shear strength and stiffness of the lumbar spine following laminectomy. Eur Spine J. 2012 Mar;21(3):530–6. doi: 10.1007/s00586-011-1968-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bisschop A, van Royen BJ, Mullender MG, Paul CPL, Kingma I, Jiya TU, et al. Which factors prognosticate spinal instability following lumbar laminectomy? Eur Spine J. 2012 Dec;21(12):2640–8. doi: 10.1007/s00586-012-2250-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tai C-L, Hsieh P-H, Chen W-P, Chen L-H, Chen W-J, Lai P-L. Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome - an experimental study in porcine model. BMC Musculoskelet Disord. 2008 Jan;9:84. doi: 10.1186/1471-2474-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee KK, Teo EC. Effects of laminectomy and facetectomy on the stability of the lumbar motion segment. Med Eng Phys. 2004 Apr;26(3):183–92. doi: 10.1016/j.medengphy.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 24.Abumi K, Panjabi MM, Kramer KM, Duranceau J, Oxland T, Crisco JJ. Biomechanical Evaluation of Lumbar Spinal Stability After Graded Facetectomies. Spine (Phila Pa 1976) 1990;15(11) doi: 10.1097/00007632-199011010-00011. [DOI] [PubMed] [Google Scholar]
- 25.Pintar FA, Cusick JF, Yoganandan N, Reinartz J, Mahesh M. The Biomechanics of Lumbar Facetectomy Under Compression-Flexion. Spine. 1992:804. doi: 10.1097/00007632-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Haher TR, O'Brien M, Dryer JW, Nucci R, Zipnick R, Leone DJ. The Role of the Lumbar Facet Joints in Spinal Stability: Identification of Alternative Paths of Loading. Spine (Phila Pa 1976) 1994;19(23) [PubMed] [Google Scholar]