Abstract
A 2012 update of the Beers criteria categorizes selective serotonin reuptake inhibitors (SSRIs) as potentially inappropriate medications in all older adults based on fall risk. The application of these recommendations, not only to frail nursing home residents, but also to all older adults, may lead to changes in health policy or clinical practice with harmful consequences. A systematic review of studies on the association between SSRIs and falls in older adults was conducted to examine the evidence for causation. Twenty-six studies met the inclusion criteria. The majority of studies were observational and suggest an association between SSRIs and falls. The direction of the relationship – causation or effect- cannot be discerned from this type of study. Standardized techniques for determining likely causation were then used to see if there was support for the hypothesis that SSRI’s lead to falls. This analysis did not suggest causation was likely. There is no Level 1 evidence that SSRIs cause falls. Therefore, changes in the current treatment guidelines or policies on the use of SSRIs in older adults based on fall risk may not be justified at this time given the lack of an established evidence base. Given its significance to public health, well-designed experimental studies are required to address this question definitively.
Keywords: Falls, SSRI, older adults
INTRODUCTION
The Beers criteria aim to promote safe and effective prescribing for all older adults through the identification of inappropriate medications. In 2012, the American Geriatrics Society (AGS) updated Beers criteria(1) categorized, with high quality of evidence and strong recommendations, selective serotonin reuptake inhibitors (SSRIs) as Potentially Inappropriate Medications (PIMs) for older adults with a history of falls or fractures. The Beers criteria were created in 1991 with a focus on potential adverse effects and excessive use of medications in frail residents of long-term care. The list has been updated twice and is now widely applied to older adults in all settings regardless of frailty status.(2) Older versions of this list included amitriptyline(2, 3) and doxepin(3) as antidepressant medications to avoid independent of diagnosis, and only recommended the avoidance of SSRIs in patients with SIADH/hyponatremia.(4) In 2012, the AGS released the latest Beers criteria. This updated list now includes most classes of psychotropic drugs.(1)
This shift in the Beers criteria towards covering entire classes of antidepressant drugs is a major shift with implications for practice, policy, and public health. The Beers Criteria are influential and have an impact on clinical guidelines, healthcare policy and quality monitoring. Moreover, falls and antidepressant use are highly prevalent in older adults. Around thirty percent of community dwelling older adults fall at least once a year(5–8) and the yearly cost of falls is estimated at $30 billion.(9) Several systematic reviews and meta-analyses have concluded that the use of psychotropic medications in general and antidepressants in particular are associated with an increased risk of falls.(10–13) Furthermore, there has been an increased focus on SSRIs and the possible association with falls and fractures.(14–18) At least one in seven community-dwelling older adults(19) and one in two nursing home residents are prescribed antidepressants.(20) Before eliminating or decreasing use of SSRIs it is vital to understand the relationship to falls. It is possible there is a common risk factor leading those at higher risk of falls to be treated with SSRIs.
If the AGS Beers recommendations are to be followed, then SSRIs (and serotonin-norepinephrine reuptake inhibitors (SNRIs)) should be avoided in most older adults because the risks and burden clearly exceed benefits.(21) Such a recommendation may lead to policies to decrease the use of antidepressants, as has been the case for antipsychotics in older adults with dementia.(22) Up to 15% of older adults have clinically significant depressive symptoms resulting in impairments in quality of life, increased morbidity and mortality and increased risk of suicide.(23–28) Therefore, a decrease in SSRI use, in the absence of a safer alternative, will either increase the prevalence of untreated depression in older adults or shift prescribing towards other, potentially more harmful medications. This may create a scenario analogous to that observed in children and adolescents, in which the observation of elevated rates of suicidality with antidepressants led to a decrease in prescribed SSRIs following the issuance of public health warnings and the possible unintended consequence of increased rates of suicidal behavior (although this point remains controversial).(29) (30)
Multiple expert panels have examined inappropriate medication prescription in older adults, but have not found reason or evidence to include SSRIs. Stefanacci et al. used the same technique as the AGS did to develop the Beers criteria to actually recommend the use of certain preferred medications in older adults and they included two SSRIs in their list, citalopram hydrochloride and escitalopram oxalate.(31) Not all instruments for improving prescribing in older adults use the Beers criteria, i.e. the Screening Tool of Older Person’s Prescriptions (STOPP) and Screening Tool to Alert doctors to Right Treatment (START) criteria.(32) A systematic review identified several prescribing criteria in older adults(33) which included French,(34) Canadian,(35) Norwegian(36) and Italian(37) expert consensus panels that have not identified SSRIs as medications to avoid in older adults, and in fact, recommend SSRIs over tricyclic antidepressants (TCAs).
Given the significant clinical, public health and policy concerns related to SSRIs and falls, we conducted a systematic review to examine the current literature on this topic. While a lack of evidence supporting causation does not indicate that SSRIs do not cause falls, a threshold of evidence is in fact needed to demonstrate causation. Thus, we applied the Bradford-Hill criteria(38) for the critical examination of the results. In doing so, we examine not only whether studies are “positive” or “negative,” but other elements of the association- such as strength and specificity of the association, experimental design, and alternative explanations- elements that are key in establishing causality.
METHODS
Search strategy
We followed the guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement.(39) A research librarian conducted a detailed systematic biomedical literature search in PubMed/MEDLINE, EMBASE, the Cochrane Library, PsycInfo and ClinicalTrials.gov from the inception of the database to February 2014. We also checked reference lists to identify relevant publications and used the authors’ knowledge of the literature to obtain additional references. The search was performed using standardized subject terms for Accidental Falls, Serotonin Uptake Inhibitors, Psychotropic Drugs, Antidepressive Agents, Second-Generation, Central Nervous System Agents and plain language for the terms according to the databases including synonyms. Finally, limits included human studies, English for language, and age limits were set from middle aged adults to 80 plus years.
Selection criteria
Exclusion criteria included mean age of the study sample below 60 years. Studies that examined antidepressant use in general but did not specify SSRI use were excluded. Although fracture was not the primary outcome, studies that examined injurious falls and/or fractures were included. Studies that examined particular disease populations where falls are more likely to occur (e.g. Parkinson’s disease or Alzheimer’s dementia) were excluded to reduce confounding.(40–44)
Data collection and extraction
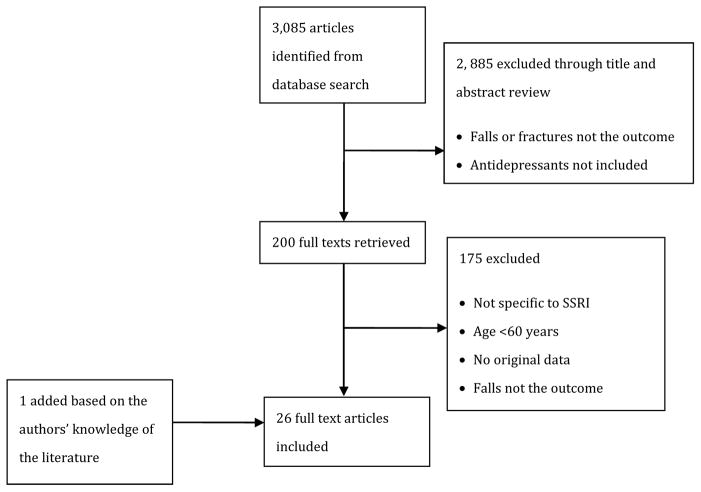
Two reviewers (MG and EL) conducted independent title, abstract, and full text reviews to determine eligibility. Disagreements between reviewers were resolved by discussion. MG and EL extracted data from eligible studies. Data extracted from the tables and text included: First author and publication year, study design, study setting, sample size, method of falls assessment, association and odds ratio (OR) (when applicable) between SSRI use and falls. A flow chart summarizing the article selection process is shown in Figure 1.
Figure 1.
Flow Chart Describing Review Process for Identification of Eligible Studies
RESULTS
The search strategy identified 3,085 articles, of which 2,880 were excluded after an initial title and abstract review. An additional 180 were excluded after full text review and one article was added based on the authors’ knowledge of the literature. A total of 26 articles were included, two of which were from the same study.(45, 46) The results are summarized in Table 1.
Table 1.
Characteristics of studies assessing Selective Serotonin Reuptake Inhibitors and falls and/or fractures
| Authors | Study design | Study setting | Sample size (N) | Fall assessment | SSRI increases risk of fall and/or fracture | Outcome measure | Type of fall |
|---|---|---|---|---|---|---|---|
| Arafken et al. 2001(16) | Observational/Retrospective | Nursing Home | 368 | Incident reports and fall logs | Yes | Adjusted OR; at least 1 fall = 2.01 (CI: 1.23–3.28) and injurious fall OR=1.77 (CI: 1.0–3.13) | Falls and injurious falls |
| Bakken et al. 2013 (47) | Observational/Prospective | Community | 906,422 | Hip fracture | Yes | SIR= 1.8 (CI: 1.7–1.8) | Injurious falls, fracture |
| Berry et al. 2011(59) | Case-crossover | Nursing Home | 1,181 | Nursing incident reports | No | OR= 0.7 (CI: 0.3–1.6) | Falls |
| Coupland et al. 2011(48) | Retrospective cohort | Community | 55,767 | ICD 9 code/self report in medical record | Yes | Adjusted HR for falls= 1.66 (CI: 1.58–1.73), adjusted HR for fracture = 1.58 (CI: 1.46–1.68) | Falls and fracture |
| Ensrud et al. 2002(45) | Observational/Prospective | Community | 8,127 | Post card for past 4 months | Yes | One fall MOR = 2.61, (CI: 1.51–4.5), frequent falls MOR =3.45 (CI: 1.89–6.30) | Falls |
| Ensrud et al. 2003(46) | Observational/Prospective | Community | 8,127 | Fractures | No | Any non-spine fracture HR= 1.44 (CI: 0.93–2.24); hip fracture HR =1.54 (CI: 0.62–3.82) | Injurious, non-spine and hip fracture |
| De Carle et al. 2001(60) | Observational/Retrospective | Inpatient | 1,834 | Fall reporting on inpatient | No | Data not available | Falls |
| Fisher et al. 2005(49) | Observational/Cross-section/Retrospective | Residential care | 179 | Daily diary nursing records and medical records | Yes | OR =2.3 (CI: 1.00–5.40) | Falls |
| Flint et al. 2014(61) | Randomized control trial | Community | 142 | History of fall assessed during study visit | No | OR= 1.56 (underpowered) (CI: 0.63–3.83) | Falls |
| Formiga et al. 2008(62) | Observational/Cross-section/Retrospective | Community | 1,225 | Direct history and chart review of recurrent falls prior to index fall | No | Data not available | Injurious falls |
| Gribbin et al. 2011(50) | Case-control/Prospective | Community | 61,782 | Read Code/Medical record | Yes | Adjusted OR= 1.55 (CI: 1.46–1.65) | Falls |
| Hubbard et al. 2003(58) | Case control and case series | Community | 46,230 | Hip fracture | Yes | OR= 1.35 (CI: 1.20–1.51); IR(1st 15 days) =1.96 (CI: 1.35–2.83) | Hip fracture |
| Kallin et al. 2002(51) | Observational/Prospective | Residential care | 83 | Nurse reporting | Yes | OR = 4.66 (CI: 1.23 – 17.59) | Falls and injurious falls |
| Kallin et al. 2004(52) | Observational/Cross-section/Retrospective | Residential care | 3,604 | Questionnaire for staff | Yes | OR= 1.67 (CI: 1.31–2.13) | Falls |
| Kerse et al. 2008(53) | Observational/Cross-section/Retrospective | Community | 21,900 | Mailed questionnaire asking falls over past 12 months | Yes | 1 fall OR =1.55 (CI: 1.26–1.90); 2 or more falls OR= 1.66 (CI: 1.36, 2.02), injurious falls OR= 1.52 (CI: 1.25, 1.84) | Falls and injurious falls |
| Landi et al. 2005(63) | Observational/Cross-section/Retrospective | Community | 2,854 | Fall history from MDS-HC in past 90 days | No | Adjusted OR= 0.99 (CI: 0.69– 1.41) | Falls |
| Lewis et al. 2007(64) | Observational/Prospective | Community | 5,995 | Fractures | No | Adjusted HR= 1.65 (CI: 0.92–2.94) | Injurious falls, fracture |
| Liu et al. 1998(15) | Case-control | Community (hospital admission for fracture) | 49,434 | Hip fracture | Yes | Adjusted OR= 2.4 (CI: 2.0–2.7) | Injurious falls, fracture |
| Mahoney et al. 2000(65) | Observational/Prospective | Community | 311 | Patient report in calendar and postcards | No | Data not available | Falls |
| Payne et al. 2013(54) | Case-cohort | Inpatients for fall or fracture | 39,813 | Hospitalization for fall or fracture | Yes | OR =1.99 (CI: 1.29–3.08) | Injurious falls, fracture |
| Richards et al. 2007(17) | Observational/Prospective | Community | 5,008 | Self report for past month | Yes | OR (fall)=2.2 (CI: 1.4–3.5), HR (fragility fracture)= 2.1 (CI: 1.3–3.4) | Falls and fragility fracture |
| Quach et al. 2013(66) | Observational/Prospective | Community | 763 | Daily self reporting falls calendar post cards | Yes (outdoor), No (indoor) | SSRI outdoor IRR = 1.53, (CI: 1.05–2.25), AD indoor IRR= 0.94 (CI: 0.64–1.37) | Falls |
| Souchet et al. 2005(55) | Case-control | Community | 67,464 | ADR reporting system (French) | Yes | Adjusted OR= 2.2 (CI: 1.5–3.1) | Falls |
| Thapa et al. 1998(56) | Observational/Retrospective | Nursing home | 2,428 | Nursing home incident reports and medical records | Yes | OR= 1.8 (CI: 1.6 to 2.0) | Falls and injurious falls |
| von Heideken et al. 2009(57) | Observational/Prospective | Nursing home and community | 220 | Fall report/daily fall calendar | Yes | HR = 2.103 (CI: 1.242–3.560) | Falls |
| Ziere et al. 2009(14) | Observational/Prospective | Community | 7,983 | Non-vertebral fracture | Yes | Adjusted HR= 2.35 (CI: 1.32–4.18) | Injurious falls and fracture |
OR= Odds ration, CI = Confidence Interval (95% in all studies), SIR= Standardized Incidence Ration, MOR= Multivariate Odds Ration, IR= Incidence Ratio, HR= Hazard ratio, IRR= Incidence Rate Ration, SSRI= Selective Serotonin Reuptake Inhibitor, AD= Antidepressant
Positive studies
Seventeen studies found an increased association of falls or injurious falls with SSRI users.(14–17, 45, 47–58) Several of these studies showed that SSRI users had other risk factors that may be associated with frailty such as multiple comorbidities, higher number of medications(15, 16), baseline higher rate of falls(48), or higher age (i.e. the oldest old).(49, 54–57) This raises concerns about biased risk estimates of falls due to confounds, as described in the discussion.
Negative studies
Nine studies did not find a significant association between SSRI use and falls or injurious falls.(46, 59–65) Only one study was a randomized controlled trial which assessed the treatment of psychotic depression.(61) Although there was no statistically significant increase in the rate of falls with sertraline (compared to placebo), the wide confidence interval of the odds ratio suggest that the study was underpowered, as the authors themselves reported; OR= 1.56 (95% CI: 0.63–3.83). A study with weekly follow up did not find SSRIs to increase the risk of falls. (65) One study found that SSRIs only increases the risk of outdoor falls and not indoor falls.(66)
Study design
All the studies were observational except for one randomized controlled trial (RCT).(61) Nine studies were retrospective and used healthcare databases (16, 48, 49, 52, 53, 56, 60, 62, 63) while ten were prospective(14, 17, 45–47, 51, 57, 64–66) and one was a case-crossover design.(59) There were five case-control studies,(15, 50, 54, 55, 58) with one(58) that also included a self-controlled case series.
Study setting
Seventeen of the studies were conducted among community dwelling older adults,(14, 15, 17, 45–48, 50, 55, 58, 61–66) two study populations were selected from inpatients, admitted either to a psychiatric unit(60) or to a medical/surgical unit,(54) and one(57) used both nursing home and community dwelling subjects.(57) Six studies were conducted in nursing homes or residential care.(16, 49, 51, 52, 56, 59) In comparison to community dwelling older adults, nursing home residents have a higher rate of falling(51, 67) and mood disorders.(68, 69)
Fall assessment
Fall assessment in nursing homes and residential care generally relied on nursing incident reports or fall logs.(16, 49, 51, 52, 56, 59) Fall assessment was more varied for community dwelling subjects. This includes quarterly postcards on which patients documented number of falls,(45, 46) self-report or clinician-determined, which ranged from past week,(52) month,(17) to past year,(53) and was obtained directly from the patient, from medical records(48, 50, 61–63), or fall calendars.(57, 65, 66) One study also used reporting based on Adverse Drug Reactions (ADR)(55) which could lead to underreporting since it relies on spontaneous reporting by clinicians.
History of falls
Multiple studies reported and factored in a history of falls, often considered as a risk factor for future falls(14, 17, 45, 49, 51, 52, 54, 56–59, 62, 64, 65) but only one study specifically compared the rates of falls before and after SSRI use. Hubbard et al conducted a case-series analysis on the incidence ratio of falls before and after antidepressant exposure.(58) This study included both SSRIs and TCAs and showed an increased rate after TCA (OR= 2.30 [95% CI 1.82–2.90]) and SSRI (OR= 1.96 [95% CI 1.35–2.83]) exposure.
Injurious falls
Eight studies specifically looked at injurious falls and fractures. Hip fractures can be considered a proxy for falls since around 95% of fractures result from falls. Of those, six(14, 15, 17, 47, 54, 58) showed a positive association between SSRI use and fractures or injurious falls requiring medical care. Two studies(14, 15) specifically excluded cases of fractures that were pathological or those that were not likely secondary to falls. One study(14) had a low number of SSRI users (N=18). A third study(47) found that only 5% of hip fractures were attributable to antidepressant exposure. In a fourth study(17) examining the association of falls and fragility fractures, despite adjustment for falls and bone mineral density, the rate of fractures remained elevated suggesting other potential mechanisms (e.g. reduced bone strength) that may play a role in fractures. Furthermore, SSRI users constituted 2.7% of the total participants and were also more likely to have depressive symptoms and have a history of falls. A retrospective case-control study(54) showed that SSRIs did have an increased OR for falls or fractures, (1.99 [95% CI 1.29–3.08]) but it was less than that of non-SSRIs, such as TCA antidepressants (4.39 [95% CI 2.21–8.71]). One case control study(58) also conducted a case-series analysis and found smaller effects in their analysis. Of the two that did not show significant results, one has been mentioned above(46) and the other(64) found that combinations of risk factors such as TCA use or previous falls to have an increased risk but did not find a significant association with SSRI use with fractures.
Assessing evidence for causation: The Bradford-Hill criteria (Table 2)
Table 2.
Applying the Bradford Hill Criteria(38): (+) Criterion is met; (−) Criterion is not met
| Bradford Hill Criterion | Association between SSRI and falls | Supporting evidence |
|---|---|---|
| Strength | − | Underpowered results, small effect sizes |
| Consistency | + | 16/25 positive studies |
| Specificity | − | Confounding by indication |
| Temporality | − | Unknown fall rates prior to SSRI use |
| Biological gradient | + | Dose dependent response |
| Plausibility | − | No clear mechanism of action |
| Coherence | − | No available evidence |
| Experiment | − | Only 1 RCT found, underpowered and no statistically significant results |
| Analogy | − | No available evidence |
The Bradford-Hill criteria(38) call for examination of different aspects of an association to establish causation. A quick review of the results of our search shows that at least one of the criteria, consistency, is met, with the majority of studies showing an association between SSRI and falls. Also, some studies(17, 48, 56) have shown biological gradient or dose-dependent response with higher doses of SSRIs resulting in more falls. However, there are several other criteria to consider before making the conclusion of causation. For example, there is no strength of the association with odds ratios or hazard ratios rarely exceeding 2.0. These small effect sizes may reflect a low likelihood of true results.(70) Despite using large samples, the numbers for fallers who used SSRIs were usually small(14, 45, 46, 49, 52, 53, 57, 64, 66) which increase potential for underpowered results. The third criteria, specificity is difficult to prove in terms of the association between SSRI use and falls as there is confounding by indication (discussed below). Also, some studies(47, 51) attributed falls to factors such as infections or medical illness despite SSRI use. Bakken et al.(47) calculated the risk of hip fracture attributed to antidepressant use and found the highest (3.6%) risk with SSRI exposure as compared to other antidepressants classes. Next, the criteria of temporality cannot be clearly established. There are no clear answers to the question of what came first, falls or SSRI prescription. Older adults with unsteadiness, falls, or a decline in physical function may be more likely to develop depression(71) and to receive medical attention resulting in increased frequency of SSRI therapy. This is best exemplified in the study by Echt et al.(72) which found the highest fall risk 4 days before a new psychotropic drug prescription or dose change. As for plausibility, several potential pathways have been suggested in the association between SSRIs and falls, but no clear mechanism has yet been elucidated. It has been suggested that SSRIs may increase the risk of falls because of cardiovascular effects.(73) Other possible mechanisms by which SSRIs may lead to falls are reviewed elsewhere(74) and include but are not limited to arrhythmias, insomnia, and sedation. Other potential implicated pathways have involved postural control as a risk factor for falls, but the results have not been consistent: while some studies did not find any change in postural sway with use of paroxetine in older depressed adults,(75, 76) others have found that sertraline and paroxetine cause an increase in postural sway.(77, 78) Depression itself is associated with impaired gait(79) with improvement in gait after successful treatment of depression with SSRI.(80) There have been inconsistent results regarding the effects of paroxetine on obstructed gait.(78, 81) A recent cross-sectional study found that antidepressants were an independent risk factor for impaired gait that potentially increases fall risk, although SSRIs only constituted around half of all antidepressants used.(82) While other medications have been associated with increased risk of falls in older adults, coherence and analogy are not very clear in this case. And lastly, the evidence from experimental studies is scarce as we identified only one experimental study that examined the association between SSRI use and falls which was underpowered without finding a statistically increased risk of falls.
Study Quality Assessment (Table 3)
Table 3.
Study Quality Assessment
| Authors | Newcastle-Ottawa Scale | Bradford-Hill Criteria | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Strength | Consistency | Specificity | Temporality | Biological gradient | Plausibility | Coherence | Experiment | Analogy | ||
| Arafken et al. 2001(16) | ★★★★★ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Bakken et al. 2013 (47) | ★★★ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Berry et al. 2011(59) | ★★★★★★★★ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Coupland et al. 2011(48) | ★★★★★★ | ✗ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ |
| Ensrud et al. 2002(45) | ★★★★★★★★ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Ensrud et al. 2003(46) | ★★★★★★★★ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| De Carle et al. 2001(60) | ★★★★ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Fisher et al. 2005(49) | ★★★★ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Flint et al. 2014(61) | 28/37 CONSORT checklist | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ |
| Formiga et al. 2008(62) | ★★★★ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Gribbin et al. 2011(50) | ★★★★★★ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Hubbard et al. 2003(58) | ★★★★★★★ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Kallin et al. 2002(51) | ★★★★★★ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Kallin et al. 2004(52) | ★★★ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Kerse et al. 2008(53) | ★★★ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Landi et al. 2005(63) | ★★★★★★ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Lewis et al. 2007(64) | ★★★★★ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Liu et al. 1998(15) | ★★★★★★★ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Mahoney et al. 2000(65) | ★★★ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Payne et al. 2013(54) | ★★★★★ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Richards et al. 2007(17) | ★★★★★★★ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ |
| Quach et al. 2013(66) | ★★★★★ | ✗ | ✓ (outdoor) ✗ (indoor) |
✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Souchet et al. 2005(55) | ★★★ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Thapa et al. 1998(56) | ★★★★★★ | ✗ | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ |
| von Heideken et al. 2009(57) | ★★★★ | ✗ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Ziere et al. 2009(14) | ★★★★★★★★ | ✗ | ✗ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
The Bradford-Hill criteria were applied for every study to identify the criteria that were met. Furthermore, the Newcastle-Ottawa scale, which utilizes a star scale system to measure the quality of observational studies was used.(83) For the randomized control trial, the CONSORT assessment scale was used. (84)
DISCUSSION
The results of our systematic review indicate that there are many observational studies pointing to an association between SSRI use and falls, but no experimental studies, such as RCTs, that support this finding. Up to 15% of older adults have clinically significant depressive symptoms, and roughly 10% have an anxiety disorder.(23, 25, 85) (86). Hence, there needs to be a robust evidence base upon which to make recommendations and subsequent policy decisions about the use of SSRIs in older adults. In particular, consideration should be given to the limited ability to determine causality when evaluating observational studies. The Bradford-Hill criteria set out the conditions needed to establish a causal relationship with relative certainty. In the sections below, we describe the inherent limitations of observational studies and demonstrate that the Bradford Hill criteria are not sufficiently met at this time.
Limitations of observational studies
Observational studies have numerous inherent limitations. There are several examples showing opposing and discrepant results between observational studies and RCTs;(87) one of the more well-publicized recent examples is hormone therapy in postmenopausal women in which RCTs showed that combined estrogen plus progestin are not to be used for prevention of coronary heart disease(88) contradicting large observational studies.(89, 90) The reasons for these discrepant results have been described previously,(70, 87, 91–94) but here we highlight some that are particularly relevant to the relationship between SSRI use and falls.
First, adjusting for confounders in analysis does not eliminate the bias or effect of unmeasured confounders. (91) Several of the studies used a retrospective design for large population – based databases; however diagnoses such as “depression” are poorly captured by administrative data. This is particularly apparent when variables cannot be measured well and conceptual or measurement errors can be made, such as severity of depression or frailty compared to other variables that can be more easily adjusted for such as age or sex.(93) As a prominent example, while observational studies found antioxidant levels to be protective against cardiovascular disease and cancer, these results were not replicated in RCTs because social and behavioral factors such as socioeconomic position (which is associated with antioxidant levels) could not be adjusted for, and residual confounding remained.(92) The study by Hubbard et al.(58) demonstrates another example that supports the effect of unmeasured confounders. The smaller results obtained from the case-series analysis when compared to the case-control analysis indicates residual bias that was not controlled for. In fact, when previously unaccounted for confounders are included in analysis, there is a decrease in the effect size of the risk between SSRIs and fractures.(18)
Second, these observational studies may suffer from confounding by indication or indication bias.(91) Large scale observational follow up studies help to identify adverse drug effects, but the caveat to that is for the adverse effects of the drug to be different from the disease itself.(93) A major limitation to the observational studies linking SSRIs to falls is the evidence from a recent systematic review and meta-analysis showing that depression is associated with an increased risk of falls.(95) Many of the strongest risk factors for falls in older adults are also common risk factors for depression.(96, 97) Additionally, antidepressants are often used off-label in older adults for the treatment of behavioral disturbances in dementia,(98) and both dementia and behavioral disturbance are independent risk factors for falls.(6, 99) In other words, observational studies cannot answer the question: Is the behavioral condition -or the antidepressants used to treat it - causing falls? Several studies controlled for potential confounders such as age, gender, measures of frailty, memory problems, number of medications and psychotropic medication classes, history of falls (16, 18, 47, 52, 54, 55, 59, 62) and other studies also specifically accounted for depression or depressive symptoms in their analysis. (14, 15, 17, 45, 46, 51, 53, 56, 57, 63–66) Two studies used case-series analysis to control for depression and eliminate confounding by indication, both showing a positive association between SSRI use and increased risk of falls and fractures(50, 58).
The third limitation to observational studies is allocation bias. There must be no link between prescription and prognosis for an observational study to satisfy the condition of unbiased allocation that is provided through randomization. This channeling effect or selective prescribing(15) i.e. prescription of SSRIs to avoid exposure to TCA in patients who are already at higher risk for falls is a potential confounder. One of the advantages of randomized controlled trials lies in the fact that randomization strives to decrease the bias of having certain patients receive a particular treatment while others do not.(93) In contrast, data obtained from observational studies are reflective of medical decisions made based on characteristics of patients and their providers that influenced these decisions and outcomes. It is impossible to delineate whether it is these characteristics or the intervention that led to the outcome being studied.(100)
The validity of falls reporting represents another significant limitation to observational studies on falls. Several of the studies relied on medical record reviews or on self- report. This poses a problem relating to the accuracy of falls reported as higher reporting rates are obtained when adverse events are solicited as compared to spontaneous reporting.(101) A review on falls reporting showed that data collection on falls should be gathered at frequent intervals i.e. weekly or monthly compared to quarterly or yearly.(102) Furthermore, the number of reported falls increases with direct assessment.(103)
Other observational study biases that may apply in the case of antidepressants and falls also include bias due to differential recall of treatment exposure(94) when patients provide reports that may not be reliable, and publication bias(104) with trends towards only reporting positive results.
When they are feasible, RCTs provide a much better estimate of causal effect(92) in comparison to results obtained from observational studies that have been described as “low grade evidence.”(105) Some argue that observational studies may increase the cost of health care and even harm patients due to discrepancies between the results of observational studies and RCTs.(91) Depending on the results obtained from observational studies to make sweeping changes to treatment/non-treatment recommendations is not justified by an absence of RCTs. The quality of results obtained from RCTs surpasses those obtained from observational studies when trying to determine causality. And while observational studies are important in detecting rare outcomes that are typically unrelated to the indication for treatment,(94) they cannot replace randomized trials or exclude the need to have them. Some of the main concerns arising from randomized controlled trials include cost and generalizability; however, it has been argued that researchers could design relatively inexpensive trials with generalizable results.(91) Recent calls for large pragmatic trials by various funding agencies, such as the National Institute for Mental Health(106) (NIMH), National Institute on Aging (NIA), and the Patient-Centered Outcome Research Institute (PCORI), reflect a move towards such studies.
CONCLUSION
We conclude from our systematic review that there is insufficient evidence to support clinical guidelines or policy changes recommending the avoidance of SSRI use in older adults based on fall risk. Given the available evidence, we do not think that clinicians should be deterred from using SSRIs in late-life depression.
Recommendations.
1. In cases of mild depression or subclinical depressive symptoms, cognitive-behavioral therapy and problem- solving therapy are some of the evidence-based psychosocial approaches for treatment in older adults that may be considered as first line treatment.(107) However, in cases of at least moderately severe depression, antidepressants have adequate evidence for efficacy.(103) 2. Clinicians and policy makers should be mindful of the hazard of shifting prescribing towards agents with less evidence for efficacy in older adults and less information regarding potential risk as is the case with SNRIs and the conflicting data with respect to falls.(50, 52, 103) 3. The current literature does not address the question of falls and SSRIs given the limitations of observational studies; thus, there is a need for large, long-term and appropriately powered RCTs similar to those seen other fields of medicine; the high public health importance of this question justifies their cost.(108)
Acknowledgments
Source of Funding:
Dr. Iaboni’s research is supported through the Faculty of Medicine, University of Toronto and Department of Psychiatry University Health Network. Dr. Lenze currently receives research support from Lundbeck and Roche. Dr. Karp has received medication supplies for investigator-initiated trials from Pfizer and Reckitt Benckiser and research support from an R01 grant AG033575.
Footnotes
Conflicts of Interest
Drs. Gebara and Nash and Ms. Lipsey have no financial disclosures.
All authors have no disclosures to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60:616–631. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine Archives of internal medicine. 1991;151:1825–1832. [PubMed] [Google Scholar]
- 3.Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update Archives of internal medicine. 1997;157:1531–1536. [PubMed] [Google Scholar]
- 4.Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Archives of internal medicine. 2003;163:2716–2724. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 5.Tromp AM, Pluijm SM, Smit JH, et al. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. Journal of clinical epidemiology. 2001;54:837–844. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- 6.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 7.Blake AJ, Morgan K, Bendall MJ, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988;17:365–372. doi: 10.1093/ageing/17.6.365. [DOI] [PubMed] [Google Scholar]
- 8.O’Loughlin JL, Robitaille Y, Boivin JF, et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–354. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 9.Stevens JA, Corso PS, Finkelstein EA, et al. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. The journals of gerontology Series A, Biological sciences and medical sciences. 2007;62:1172–1181. doi: 10.1093/gerona/62.10.1172. [DOI] [PubMed] [Google Scholar]
- 11.Bloch F, Thibaud M, Dugue B, et al. Psychotropic drugs and falls in the elderly people: updated literature review and meta-analysis. Journal of Aging and Health. 2011;23:329–346. doi: 10.1177/0898264310381277. [DOI] [PubMed] [Google Scholar]
- 12.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs Journal of the American Geriatrics Society. 1999;47:40–50. doi: 10.1111/j.1532-5415.1999.tb01899.x. [DOI] [PubMed] [Google Scholar]
- 13.Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Archives of internal medicine. 2009;169:1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 14.Ziere G, Dieleman JP, van der Cammen TJ, et al. Selective serotonin reuptake inhibiting antidepressants are associated with an increased risk of nonvertebral fractures. Journal of Clinical Psychopharmacology. 2008;28:411–417. doi: 10.1097/JCP.0b013e31817e0ecb. [DOI] [PubMed] [Google Scholar]
- 15.Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351:1303–1307. doi: 10.1016/s0140-6736(97)09528-7. [DOI] [PubMed] [Google Scholar]
- 16.Arfken CL, Wilson JG, Aronson SM. Retrospective review of selective serotonin reuptake inhibitors and falling in older nursing home residents. International psychogeriatrics/IPA. 2001;13:85–91. doi: 10.1017/s1041610201007487. [DOI] [PubMed] [Google Scholar]
- 17.Richards JB, Papaioannou A, Adachi JD, et al. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med. 2007;167:188–194. doi: 10.1001/archinte.167.2.188. [DOI] [PubMed] [Google Scholar]
- 18.Schneeweiss S, Wang PS. Association between SSRI use and hip fractures and the effect of residual confounding bias in claims database studies. Journal of Clinical Psychopharmacology. 2004;24:632–638. doi: 10.1097/01.jcp.0000145344.76288.39. [DOI] [PubMed] [Google Scholar]
- 19.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66:848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 20.Karkare SU, Bhattacharjee S, Kamble P, et al. Prevalence and predictors of antidepressant prescribing in nursing home residents in the United States. Am J Geriatr Pharmacother. 2011;9:109–119. doi: 10.1016/j.amjopharm.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Qaseem A, Snow V, Owens DK, et al. The development of clinical practice guidelines and guidance statements of the American College of Physicians: summary of methods. Ann Intern Med. 2010;153:194–199. doi: 10.7326/0003-4819-153-3-201008030-00010. [DOI] [PubMed] [Google Scholar]
- 22.FDA. Public Health Advisory: Deaths with Antipsychotics in Elderly Patients with Behavioral Disturbances. 2005 [Google Scholar]
- 23.Blazer D, Burchett B, Service C, et al. The association of age and depression among the elderly: an epidemiologic exploration. J Gerontol. 1991;46:M210–215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- 24.Berkman LF, Berkman CS, Kasl S, et al. Depressive symptoms in relation to physical health and functioning in the elderly. Am J Epidemiol. 1986;124:372–388. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- 25.Doraiswamy PM, Khan ZM, Donahue RM, et al. The spectrum of quality-of-life impairments in recurrent geriatric depression. J Gerontol A Biol Sci Med Sci. 2002;57:M134–137. doi: 10.1093/gerona/57.2.m134. [DOI] [PubMed] [Google Scholar]
- 26.Blazer D, Williams CD. Epidemiology of dysphoria and depression in an elderly population. Am J Psychiatry. 1980;137:439–444. doi: 10.1176/ajp.137.4.439. [DOI] [PubMed] [Google Scholar]
- 27.Beekman AT, Deeg DJ, van Tilburg T, et al. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord. 1995;36:65–75. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- 28.Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 29.Gibbons RD, Brown CH, Hur K, et al. Early evidence on the effects of regulators’ suicidality warnings on SSRI prescriptions and suicide in children and adolescents. The American journal of psychiatry. 2007;164:1356–1363. doi: 10.1176/appi.ajp.2007.07030454. [DOI] [PubMed] [Google Scholar]
- 30.Rhodes AE, Skinner R, McFaull S, et al. Canada-wide effect of regulatory warnings on antidepressant prescribing and suicide rates in boys and girls. Can J Psychiatry. 2013;58:640–645. doi: 10.1177/070674371305801110. [DOI] [PubMed] [Google Scholar]
- 31.Stefanacci RG, Cavallaro E, Beers MH, et al. Developing explicit positive beers criteria for preferred central nervous system medications in older adults. Consult Pharm. 2009;24:601–610. doi: 10.4140/tcp.n.2009.601. [DOI] [PubMed] [Google Scholar]
- 32.O’Mahony D, Gallagher P, Ryan C, et al. STOPP & START criteria: A new approach to detecting potentially inappropriate prescribing in old age. Eur Geriatr Med. 2010;1:45–51. [Google Scholar]
- 33.Dimitrow MS, Airaksinen MS, Kivela SL, et al. Comparison of prescribing criteria to evaluate the appropriateness of drug treatment in individuals aged 65 and older: a systematic review. Journal of the American Geriatrics Society. 2011;59:1521–1530. doi: 10.1111/j.1532-5415.2011.03497.x. [DOI] [PubMed] [Google Scholar]
- 34.Laroche ML, Charmes JP, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. European journal of clinical pharmacology. 2007;63:725–731. doi: 10.1007/s00228-007-0324-2. [DOI] [PubMed] [Google Scholar]
- 35.McLeod PJ, Huang AR, Tamblyn RM, et al. Defining inappropriate practices in prescribing for elderly people: a national consensus panel. Cmaj. 1997;156:385–391. [PMC free article] [PubMed] [Google Scholar]
- 36.Rognstad S, Brekke M, Fetveit A, et al. The Norwegian General Practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients. A modified Delphi study. Scand J Prim Health Care. 2009;27:153–159. doi: 10.1080/02813430902992215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maio V, Del Canale S, Abouzaid S. Using explicit criteria to evaluate the quality of prescribing in elderly Italian outpatients: a cohort study. J Clin Pharm Ther. 2010;35:219–229. doi: 10.1111/j.1365-2710.2009.01094.x. [DOI] [PubMed] [Google Scholar]
- 38.Hill AB. The Environment and Disease: Association or Causation? Proc R Soc Med. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Joo JH, Lenze EJ, Mulsant BH, et al. Risk factors for falls during treatment of late-life depression. J Clin Psychiatry. 2002;63:936–941. doi: 10.4088/jcp.v63n1012. [DOI] [PubMed] [Google Scholar]
- 41.Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age and ageing. 2012;41:299–308. doi: 10.1093/ageing/afs012. [DOI] [PubMed] [Google Scholar]
- 42.Harlein J, Halfens RJ, Dassen T, et al. Falls in older hospital inpatients and the effect of cognitive impairment: a secondary analysis of prevalence studies. J Clin Nurs. 2011;20:175–183. doi: 10.1111/j.1365-2702.2010.03460.x. [DOI] [PubMed] [Google Scholar]
- 43.Allen NE, Schwarzel AK, Canning CG. Recurrent falls in Parkinson’s disease: a systematic review. Parkinsons Dis. 2013;2013:906274. doi: 10.1155/2013/906274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stolze H, Klebe S, Baecker C, et al. Prevalence of gait disorders in hospitalized neurological patients. Movement disorders : official journal of the Movement Disorder Society. 2005;20:89–94. doi: 10.1002/mds.20266. [DOI] [PubMed] [Google Scholar]
- 45.Ensrud KE, Blackwell TL, Mangione CM, et al. Central nervous system-active medications and risk for falls in older women. Journal of the American Geriatrics Society. 2002;50:1629–1637. doi: 10.1046/j.1532-5415.2002.50453.x. [DOI] [PubMed] [Google Scholar]
- 46.Ensrud KE, Blackwell T, Mangione CM, et al. Central nervous system active medications and risk for fractures in older women. Arch Intern Med. 2003;163:949–957. doi: 10.1001/archinte.163.8.949. [DOI] [PubMed] [Google Scholar]
- 47.Bakken MS, Engeland A, Engesaeter LB, et al. Increased risk of hip fracture among older people using antidepressant drugs: data from the Norwegian Prescription Database and the Norwegian Hip Fracture Registry. Age and ageing. 2013;42:514–520. doi: 10.1093/ageing/aft009. [DOI] [PubMed] [Google Scholar]
- 48.Coupland CA, Dhiman P, Barton G, et al. A study of the safety and harms of antidepressant drugs for older people: a cohort study using a large primary care database. Health technology assessment. 2011;15:1–202. iii–iv. doi: 10.3310/hta15280. [DOI] [PubMed] [Google Scholar]
- 49.Fisher AA, Davis MW, McLean AJ, et al. Epidemiology of falls in elderly semi-independent residents in residential care. Australas J Ageing. 2005;24:98–102. [Google Scholar]
- 50.Gribbin J, Hubbard R, Gladman J, et al. Serotonin-norepinephrine reuptake inhibitor antidepressants and the risk of falls in older people: case-control and case-series analysis of a large UK primary care database. Drugs & Aging. 2011;28:895–902. doi: 10.2165/11592860-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 51.Kallin K, Lundin-Olsson L, Jensen J, et al. Predisposing and precipitating factors for falls among older people in residential care. Public Health. 2002;116:263–271. doi: 10.1038/sj.ph.1900849. [DOI] [PubMed] [Google Scholar]
- 52.Kallin K, Gustafson Y, Sandman PO, et al. Drugs and falls in older people in geriatric care settings. Aging clinical and experimental research. 2004;16:270–276. doi: 10.1007/BF03324551. [DOI] [PubMed] [Google Scholar]
- 53.Kerse N, Flicker L, Pfaff JJ, et al. Falls, depression and antidepressants in later life: a large primary care appraisal. PLoS One. 2008;3:e2423. doi: 10.1371/journal.pone.0002423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Payne RA, Abel GA, Simpson CR, et al. Association between prescribing of cardiovascular and psychotropic medications and hospital admission for falls or fractures. Drugs & Aging. 2013;30:247–254. doi: 10.1007/s40266-013-0058-z. [DOI] [PubMed] [Google Scholar]
- 55.Souchet E, Lapeyre-Mestre M, Montastruc JL. Drug related falls: a study in the French Pharmacovigilance database. Pharmacoepidemiol Drug Saf. 2005;14:11–16. doi: 10.1002/pds.1038. [DOI] [PubMed] [Google Scholar]
- 56.Thapa PB, Gideon P, Cost TW, et al. Antidepressants and the risk of falls among nursing home residents. The New England journal of medicine. 1998;339:875–882. doi: 10.1056/NEJM199809243391303. [DOI] [PubMed] [Google Scholar]
- 57.von Heideken Wagert P, Gustafson Y, Kallin K, et al. Falls in very old people: the population-based Umea 85+ study in Sweden. Archives of gerontology and geriatrics. 2009;49:390–396. doi: 10.1016/j.archger.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 58.Hubbard R, Farrington P, Smith C, et al. Exposure to tricyclic and selective serotonin reuptake inhibitor antidepressants and the risk of hip fracture. American journal of epidemiology. 2003;158:77–84. doi: 10.1093/aje/kwg114. [DOI] [PubMed] [Google Scholar]
- 59.Berry SD, Zhang Y, Lipsitz LA, et al. Antidepressant prescriptions: an acute window for falls in the nursing home. The journals of gerontology Series A, Biological sciences and medical sciences. 2011;66:1124–1130. doi: 10.1093/gerona/glr113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Carle AJ, Kohn R. Risk factors for falling in a psychogeriatric unit. International Journal of Geriatric Psychiatry. 2001;16:762–767. doi: 10.1002/gps.407. [DOI] [PubMed] [Google Scholar]
- 61.Flint AJ, Iaboni A, Mulsant BH, et al. Effect of sertraline on risk of falling in older adults with psychotic depression on olanzapine: results of a randomized placebo-controlled trial. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2014;22:332–336. doi: 10.1016/j.jagp.2013.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Formiga F, Navarro M, Duaso E, et al. Factors associated with hip fracture-related falls among patients with a history of recurrent falling. Bone. 2008;43:941–944. doi: 10.1016/j.bone.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 63.Landi F, Onder G, Cesari M, et al. Psychotropic medications and risk for falls among community-dwelling frail older people: an observational study. J Gerontol A Biol Sci Med Sci. 2005;60:622–626. doi: 10.1093/gerona/60.5.622. [DOI] [PubMed] [Google Scholar]
- 64.Lewis CE, Ewing SK, Taylor BC, et al. Predictors of non-spine fracture in elderly men: the MrOS study. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2007;22:211–219. doi: 10.1359/jbmr.061017. [DOI] [PubMed] [Google Scholar]
- 65.Mahoney JE, Palta M, Johnson J, et al. Temporal association between hospitalization and rate of falls after discharge. Archives of internal medicine. 2000;160:2788–2795. doi: 10.1001/archinte.160.18.2788. [DOI] [PubMed] [Google Scholar]
- 66.Quach L, Yang FM, Berry SD, et al. Depression, antidepressants, and falls among community-dwelling elderly people: the MOBILIZE Boston study. The journals of gerontology Series A, Biological sciences and medical sciences. 2013;68:1575–1581. doi: 10.1093/gerona/glt084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Luukinen H, Koski K, Honkanen R, et al. Incidence of injury-causing falls among older adults by place of residence: a population-based study. Journal of the American Geriatrics Society. 1995;43:871–876. doi: 10.1111/j.1532-5415.1995.tb05529.x. [DOI] [PubMed] [Google Scholar]
- 68.Parmelee PA, Katz IR, Lawton MP. Depression among institutionalized aged: assessment and prevalence estimation. Journal of Gerontology. 1989;44:M22–29. doi: 10.1093/geronj/44.1.m22. [DOI] [PubMed] [Google Scholar]
- 69.Rovner BW, German PS, Brant LJ, et al. Depression and mortality in nursing homes. JAMA. 1991;265:993–996. doi: 10.1001/jama.265.8.993. [DOI] [PubMed] [Google Scholar]
- 70.Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2:e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lenze EJ, Rogers JC, Martire LM, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- 72.Echt MA, Samelson EJ, Hannan MT, et al. Psychotropic drug initiation or increased dosage and the acute risk of falls: a prospective cohort study of nursing home residents. BMC geriatrics. 2013;13:19. doi: 10.1186/1471-2318-13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pacher P, Ungvari Z. Selective serotonin-reuptake inhibitor antidepressants increase the risk of falls and hip fractures in elderly people by inhibiting cardiovascular ion channels. Med Hypotheses. 2001;57:469–471. doi: 10.1054/mehy.2001.1366. [DOI] [PubMed] [Google Scholar]
- 74.Darowski A, Chambers S, Chambers D. Antidepressants and falls in the elderly. Drugs & aging. 2009;26:381–394. doi: 10.2165/00002512-200926050-00002. [DOI] [PubMed] [Google Scholar]
- 75.Mamo DC, Pollock BG, Mulsant B, et al. Effects of nortriptyline and paroxetine on postural sway in depressed elderly patients. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2002;10:199–205. [PubMed] [Google Scholar]
- 76.Laghrissi-Thode F, Pollock BG, Miller MC, et al. Double-blind comparison of paroxetine and nortriptyline on the postural stability of late-life depressed patients. Psychopharmacol Bull. 1995;31:659–663. [PubMed] [Google Scholar]
- 77.Laghrissithode F, Pollock BG, Miller M, et al. Comparative Effects of Sertraline and Nortriptyline on Body Sway in Older Depressed-Patients. American Journal of Geriatric Psychiatry. 1995;3:217–228. doi: 10.1097/00019442-199522330-00005. [DOI] [PubMed] [Google Scholar]
- 78.Hegeman J, van den Bemt B, Weerdesteyn V, et al. Unraveling the Association Between SSRI Use and Falls: An Experimental Study of Risk Factors for Accidental Falls in Long-Term Paroxetine Users. Clinical Neuropharmacology. 2011;34:210–215. doi: 10.1097/WNF.0b013e31823337d1. [DOI] [PubMed] [Google Scholar]
- 79.Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2013;21:484–492. doi: 10.1016/j.jagp.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Paleacu D, Shutzman A, Giladi N, et al. Effects of pharmacological therapy on gait and cognitive function in depressed patients. Clinical neuropharmacology. 2007;30:63–71. doi: 10.1097/01.wnf.0000240949.41691.95. [DOI] [PubMed] [Google Scholar]
- 81.Draganich LF, Zacny J, Klafta J, et al. The effects of antidepressants on obstructed and unobstructed gait in healthy elderly people. The journals of gerontology Series A, Biological sciences and medical sciences. 2001;56:M36–41. doi: 10.1093/gerona/56.1.m36. [DOI] [PubMed] [Google Scholar]
- 82.Donoghue OA, O’Hare C, King-Kallimanis B, et al. Antidepressants are Independently Associated with Gait Deficits in Single and Dual Task Conditions. Am J Geriatr Psychiatry. 2014 doi: 10.1016/j.jagp.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 83.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, Ontario, Canada: 2014. [Google Scholar]
- 84.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Annals of internal medicine. 2010;152:726–732. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 85.Doraiswamy PM, Khan ZM, Donahue RM, et al. Quality of life in geriatric depression: a comparison of remitters, partial responders, and nonresponders. Am J Geriatr Psychiatry. 2001;9:423–428. [PubMed] [Google Scholar]
- 86.Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: methodological issues and a review of the literature. J Affect Disord. 2008;109:233–250. doi: 10.1016/j.jad.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 87.Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical research. JAMA : the journal of the American Medical Association. 2005;294:218–228. doi: 10.1001/jama.294.2.218. [DOI] [PubMed] [Google Scholar]
- 88.Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA : the journal of the American Medical Association. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 89.Stampfer MJ, Colditz GA, Willett WC, et al. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses’ health study The New England journal of medicine. 1991;325:756–762. doi: 10.1056/NEJM199109123251102. [DOI] [PubMed] [Google Scholar]
- 90.Grady D, Rubin SM, Petitti DB, et al. Hormone therapy to prevent disease and prolong life in postmenopausal women. Annals of internal medicine. 1992;117:1016–1037. doi: 10.7326/0003-4819-117-12-1016. [DOI] [PubMed] [Google Scholar]
- 91.Albert RK. Lies, damned lies” and observational studies in comparative effectiveness research. Am J Respir Crit Care Med. 2013;187:1173–1177. doi: 10.1164/rccm.201212-2187OE. [DOI] [PubMed] [Google Scholar]
- 92.Lawlor DA, Davey Smith G, Kundu D, et al. Those confounded vitamins: what can we learn from the differences between observational versus randomised trial evidence? Lancet. 2004;363:1724–1727. doi: 10.1016/S0140-6736(04)16260-0. [DOI] [PubMed] [Google Scholar]
- 93.Vandenbroucke JP. When are observational studies as credible as randomised trials? Lancet. 2004;363:1728–1731. doi: 10.1016/S0140-6736(04)16261-2. [DOI] [PubMed] [Google Scholar]
- 94.MacMahon S, Collins R. Reliable assessment of the effects of treatment on mortality and major morbidity, II: observational studies. Lancet. 2001;357:455–462. doi: 10.1016/S0140-6736(00)04017-4. [DOI] [PubMed] [Google Scholar]
- 95.Kvelde T, McVeigh C, Toson B, et al. Depressive symptomatology as a risk factor for falls in older people: systematic review and meta-analysis. Journal of the American Geriatrics Society. 2013;61:694–706. doi: 10.1111/jgs.12209. [DOI] [PubMed] [Google Scholar]
- 96.Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 97.Biderman A, Cwikel J, Fried AV, et al. Depression and falls among community dwelling elderly people: a search for common risk factors. J Epidemiol Community Health. 2002;56:631–636. doi: 10.1136/jech.56.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Porsteinsson AP, Drye LT, Pollock BG, et al. Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA. 2014;311:682–691. doi: 10.1001/jama.2014.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sylliaas H, Selbaek G, Bergland A. Do behavioral disturbances predict falls among nursing home residents? Aging Clin Exp Res. 2012;24:251–256. doi: 10.1007/BF03325253. [DOI] [PubMed] [Google Scholar]
- 100.Sox HC, Greenfield S. Comparative effectiveness research: a report from the Institute of Medicine. Annals of internal medicine. 2009;151:203–205. doi: 10.7326/0003-4819-151-3-200908040-00125. [DOI] [PubMed] [Google Scholar]
- 101.Wernicke JF, Faries D, Milton D, et al. Detecting treatment emergent adverse events in clinical trials : a comparison of spontaneously reported and solicited collection methods. Drug safety : an international journal of medical toxicology and drug experience. 2005;28:1057–1063. doi: 10.2165/00002018-200528110-00006. [DOI] [PubMed] [Google Scholar]
- 102.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. Journal of the American Geriatrics Society. 2005;53:2190–2194. doi: 10.1111/j.1532-5415.2005.00509.x. [DOI] [PubMed] [Google Scholar]
- 103.Nelson JC, Delucchi KL, Schneider LS. Moderators of outcome in late-life depression: a patient-level meta-analysis. The American journal of psychiatry. 2013;170:651–659. doi: 10.1176/appi.ajp.2012.12070927. [DOI] [PubMed] [Google Scholar]
- 104.Dwan K, Gamble C, Williamson PR, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias - an updated review. PLoS One. 2013;8:e66844. doi: 10.1371/journal.pone.0066844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Insel TR. Mental disorders in childhood: shifting the focus from behavioral symptoms to neurodevelopmental trajectories. JAMA : the journal of the American Medical Association. 2014;311:1727–1728. doi: 10.1001/jama.2014.1193. [DOI] [PubMed] [Google Scholar]
- 107.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mulsant BH. Challenges of the treatment of neuropsychiatric symptoms associated with dementia. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2014;22:317–320. doi: 10.1016/j.jagp.2014.01.008. [DOI] [PubMed] [Google Scholar]