Abstract
Background:
Chronic recurrent multifocal osteomyelitis (CREMO) is one of the autoinflammatory bone disorders due to disturbance in innate immune system. Up to now, there is no reported case of caseous granulomas in the CREMO. We report a boy with sterile granolumatous osteomyelitis.
Case Presentation:
A four-year-old boy presented with swelling and pain in the left wrist, malaise and bilateral erythematous pustulosis on the palmar region which had resolved spontaneously after about 7 days. The histopathology of the lesions showed severe acute and chronic inflammatory process and chronic granulomatous reaction with caseating necrosis (granulomatous osteomyelitis). The direct smear, culture and PCR for the mycobacterium tuberculosis and atypical mycobacteria were negative. About five months after initiation of the anti-mycobacterial treatment, he was referred to the rheumatology clinic with left elbow pain, effusion and decreased range of motion, and bilateral erythematous palmar pustulosis. He was diagnosed as CREMO based on two exacerbations, repeatedly negative cultures, and concomitant acute and chronic lesions in the histopathology and X-ray. Naproxen and pamidronate every 3 months were started and all other medications were stopped. Two months after the first dose of pamidronate, he became symptom-free and forearm X-ray showed disappearance of the osteolytic lesions and periosteal reactions.
Conclusion:
The diagnosis of CREMO should be considered in the patients with lytic bone lesions. In addition, the clinicians should be aware of the possibility of caseating granuloma in the cases with possible diagnosis of CREMO.
Keywords: Chronic Recurrent Multifocal Osteomyelitis, Caseous Granuloma, Tuberculosis
Introduction
Chronic recurrent multifocal osteomyelitis (CREMO) is one of the autoinflammatory bone disorders due to disturbance in innate immune system. So, there are no auto-antibodies or autoreactive T-cells [1] . Despite its name, it is not always recurrent or multifocal. It has different clinical courses: unifocal nonrecurrent, recurrent multifocal and persistent multifocal [2] .
Depending on the age of the bone lesions, histopathology can be different. Bone lesions in the CREMO may or may not contain granuloma [3] . The granuloma means a collection of macrophages due to inflammation. Caseating granuloma means necrosis involving dead cells with no nuclei and debris. Without microscope, the cheese like pattern was seen in the these granulomas [4] . In all reports of the CREMO patients, the granulomas were noncaseating [5] . The main diagnosis of the caseous granulomas in the histology of bone lesions is TB osteomyelitis. Moreover, caseous granulomas were reported in the Salmonella osteomyelitis in immunocompromised patients [6] . To our knowledge, there was no reported case of caseous granulomas in the CREMO. In this article, a case of CREMO with caseating granuloma lesions is reported.
Case Presentation
A four-year-old boy, the third child of non-consanguineous parents presented with swelling and pain in the left wrist. It was preceded malaise and bilateral erythematous pustulosis on the palmar region which had resolved spontaneously after about 7 days. The body temperature was normal.
The biopsy of the bone was performed, and the cefazolin was initiated for possible osteomyelitis. The histopathology of the lesions showed severe acute and chronic inflammatory process and chronic granulomatous reaction with caseating necrosis (granulomatous osteomyelitis) (Fig. 1). The direct smear and culture were negative for bacteria, fungi and acid fast bacilli. PCR for mycobacterium tuberculosis and atypical mycobacteria was negative. Collected stomach liquid for three days did not detect any mycobacterium. No mycobacterium grew on the Lowenstein-Jensen medium after 2 months. Chest X-ray and abdominal ultrasound were normal. The result of tuberculin skin test was about 4 mm (with history of vaccination).
Fig. 1:
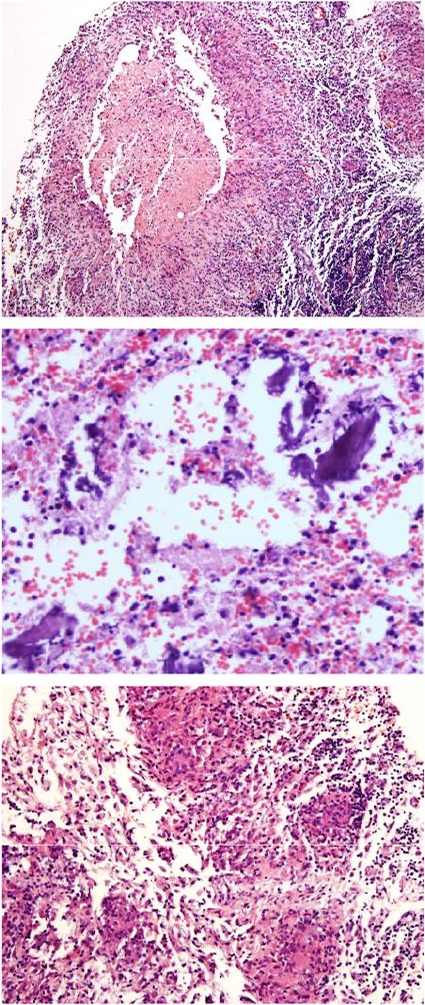
Chronic inflammatory process and chronic granulomatous reaction with caseating necrosis
In spite of negative investigations for the cause of granulomatous osteomyelitis, four drugs anti-mycobacterial regimen was prescribed: Isoniazid, Rifampin, Pyrazinamide, and Ethambutol, plus B6. About five months after initiation of the anti-mycobacterial treatment, he was referred to the rheumatology clinic of the Children’s Medical Center with left elbow pain, effusion and decreased range of motion, and bilateral erythematous palmar pustulosis. The X-ray of the left forearm revealed multiple lytic lesions in ulnar, two chronic osteomyelitis lesions on the distal ulnar, and periosteal reaction over the radius bone (Fig. 2). The bone biopsy showed granulomatous osteomyelitis with some area of necrosis. The direct smear and acid-fast stained smear were negative. The cultures for bacteria, acid-fast bacilli and fungi were negative similar to the previous evaluations.
Fig. 2:

Multiple lytic lesions in ulnar, two chronic osteomyelitis lesions on the distal ulnar, and periosteal reaction over the radius bone.
The results of laboratory tests were as follows: white blood cell 8450/ml with 36.9% neutrophils, 51.3% lymphocytes, and 11.3% monocytes, hemoglobin 10.7g/dl, platelets 295000/ml, erythrocyte sedimentation rate (ESR) 44 mm, and the C-reactive protein 56.9 mg/dl. In the evaluation of immunodeficiencies, immunoglobulins, CD3, CD4, CD8, CD19, CD16, and CD 56 were within normal limit. Nitroblue tetrazolium (NBT) test was 100 percent. The tests of auto-inflammatory diseases and sarcoidosis [Adenosine deaminase level, fluorescent antinuclear antibody (FANA), complement levels (C3, C4, CH50), antineutrophilic cytoplasmic antibodies, rheumatoid factor] were negative. Serological investigation for Brucella and Salmonella, abdominal ultrasonography, and eye examinations were also normal. Chest and skull X-rays were normal. Increased activity was seen in the head of the right humerus in Tc99m MDP bone scintigraphy.
He was diagnosed as CREMO based on two exacerbations, repeatedly negative cultures, and concomitant acute and chronic lesions in the histopathology and X-ray. Naproxen (15mg/kg/day) and pamidronate (1mg/kg) every 3 months were started and all other medications were stopped. Two months after the first dose of pamidronate, he became symptom-free and forearm X-ray showed disappearance of the osteolytic lesions and periosteal reactions (Fig. 3).
Fig. 3:

Disappearance of the osteolytic lesions and periosteal reactions 2 months after treatment with pamidronate.
Discussion
Chronic nonbacterial osteomyelitis (CNO) has a spectrum of manifestations with self-limited mono focal or oligo-focal bone lesion in one end and multifocal chronic recurrent bone lesions in the other end, called CREMO [7] . The most cases were children [8] and a similar syndrome with synovitis, acne, pustulosis, hyperostosis, and osteitis has been described in adults as SAPHO syndrome [9] .
Symptoms at onset are mild pain, low grade fever, malaise, with or without swelling or warmth of the affected area. Skin inflammation can occur as palmoplantar pustulosis (like in our patient), psoriasis, and occasionally pyoderma gangrenosum [10,11] . In immunocompetent children CNO may be much more frequent than bacterial osteomyelitis, even if they do not have any well-known symptoms such as palmoplantar pustulosis or hyperostosis [12] .
Autoinflammatory bone disorders include deficiency of IL1 receptor antagonist (DIRA), pyogenic artheritis, pyoderma gangrenosum and acne (PAPA) syndrome, Majeed syndrome, synovitis, acne, SAPHO syndrome, and sporadic chronic recurrent multifocal osteomyelitis (CREMO) [10,13,14] . Monogenic etiologies are reported in the autoinflammatory bone diseases other than CREMO. Mutation in the PSTPIP1 gene for a protein in the regulation of pyrine was known in PAPA syndrome. In addition, a mutation in the LPIN2 gene was identified in Majeed syndrome, an autosomal recessive disease that manifests as a severe CREMO attack with recurrent fever, osteomyelitis and dyserythropoietic anemia [15] . To date, no single gene was discovered for the CREMO. So, since no specific diagnostic biomarkers are available, the diagnosis of the sporadic CREMO is based on the exclusion of the other etiologies [16] .
In addition to the CREMO, two autosomal dominant diseases, DIRA and cherubism have multifocal inflammatory bone lesions. Cherubism has greater degree of osteolysis than CREMO and characteristic facial features. DIRA is characterized by severe osteolytic lesions, periostitis and pustulosis and manifests in younger age compared with CREMO. Expansive lesions of the ribs are a characteristic feature of the DIRA (not found in CREMO) [17] .
Jansson et al described scores for diagnosis of CREMO [12] . Based on these scores, in a patient with multiple bone lesions and the score of ≤28 points, clinical monitoring should be done. In a patient with the score of 29–38, clinical monitoring should be done as above, although association with palmoplantar pustulosis increases the likelihood of NBO [12] . In a patient with the score of ≥38 points, the diagnosis of NBO is confirmed [12] . Our patient had >2 radiologically-proven bone lesions (score=7), normal blood cell count (score=13), normal body temperature (score=9) and CRP ≥1 mg/dl (score=6). So, our patient score was 35. Because of the presence of palmar pustulosis in this case, the diagnosis of NBO is very likely.
Although CREMO was a sterile osteomyelitis with negative cultures [18] , some investigators reported that the osteitis was triggered by exposure to a microbial agent. A few studies reported positive cultures of the organisms, including propionibacterium acnes, mycoplasma, and different staphylococcus species [19] . In another study, 7 of 13 patients with CREMO had rapid clinical and radiological improvement with azithromycin [20] . However, in some studies, prolonged use of antimicrobial drugs had no effect on improvement [21] .
On the other hand, in the histology of CREMO in the early phase, neutrophils are prominent. In the late lesions, plasma cells, lymphocytes, histiocytes, and in some cases noncaseous granuloma was seen [3] . The granuloma is formed when the immune system attempts to wall-off the foreign substances but could not eliminate it. The caseating granuloma is formed when this foreign substance was infectious [4] . The first diagnosis in caseous granuloma is TB osteomyelitis [4] . Although acid-fast stains were often negative, the cultures were positive in approximately 72% of patients. Multiplex real-time PCR could distinguish typical from atypical mycobacteria [22] . These tests were repeatedly negative in our patient. There might be microbial triggers that form the caseous granuloma in CREMO which remained unknown until now.
Since the placebo-controlled randomized trials have not been done, the treatment of CREMO was empirical [16] . Due to participation of prostaglandins in osteoclast activation and bone remodeling, NSAIDs are used as the first-line treatment [9,23] . The second line treatment includes corticosteroids, sulfasalazine, methotrexate, anti-TNF agents, and bisphosphonates [10,11] . Furthermore, bisphosphonates have anti-inflammatory effects because of suppressing proinflammatory cytokines such as interleukin (IL) 1, IL6, and TNF-α [24] . Bisphosphonates are used in severe cases of treatment resistance or in structural damage such as in our patient.
Conclusion
In conclusion, the diagnosis of CREMO should be considered in the patients with lytic bone lesions. In addition, the clinicians should be aware of the possibility of caseating granuloma in the cases with possible diagnosis of CREMO.
References
- 1. De Almeida J, Goldbach-Mansky R. Monogenic autoinflammatory diseases: concept and clinical manifestations. Clin Immunol 2013; 147 (3): 155– 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kahn MF. Why the “SAPHO” syndrome?. J Rheumatol 1995; 22 (11): 2017– 19. [PubMed] [Google Scholar]
- 3. Bjorksten B, Boquis L. Histopathological aspects of chronic recurrent multifocal osteomyelitis. J Bone Joint Surg 1980; 62 (3): 376– 80. [DOI] [PubMed] [Google Scholar]
- 4. Mukhopadhyay S, Farver CF, Vaszar LT, et al. Causes of pulmonary granulomas: a retrospective study of 500 cases from seven countries. J Clin Pathol 2012; 65 (1): 51– 7. [DOI] [PubMed] [Google Scholar]
- 5. Bjorksten B, Gustavson KH, Eriksson B, et al. Chronic recurrent multifocal osteomyelitis and pustulosis palmoplantaris. J Pediatr 1978; 93 (2): 227– 31. [DOI] [PubMed] [Google Scholar]
- 6. Szilagyi A, Mendelson J, Portnoy J, et al. Caseating granulomas in chronic osteomyolitis: Salmonellosis, tuberculosis or both? Can Med Assoc J 1979; 120 (8): 963–5. [PMC free article] [PubMed] [Google Scholar]
- 7. Girschick HJ, Raab P, Surbaum S, et al. Chronic non-bacterial osteomyelitis in children. Ann Rheum Dis 2005; 64 (2): 279– 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wipff J, Adamsbaum C, Kahan A, et al. Chronic recurrent multifocal osteomyelitis Joint Bone Spine 2011; 78 (6): 555–60. [DOI] [PubMed] [Google Scholar]
- 9. Sayılı A, Tosun O, Cobanoglu N, et al. Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis (SAPHO) Syndrome in Childhood; A Rare Clinical Entity. Iran J Pediatr 2014; 24 (5): 658– 9. [PMC free article] [PubMed] [Google Scholar]
- 10. Morbach H, Hedrich CM, Beer M, et al. Autoinflammatory bone disorders. Clin Immunol 2013; 147 (3): 185– 96. [DOI] [PubMed] [Google Scholar]
- 11. Sharma M, Ferguson PJ. Autoinflammatory bone disorders: update on immunologic abnormalities and clues about possible triggers. Curr Opin Rheumatol 2013; 25 (5): 658– 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jansson AF, Müller TH, Gliera L, et al. Clinical score for nonbacterial osteitis in children and adults. Arthritis Rheum 2009; 60 (4): 1152– 9. [DOI] [PubMed] [Google Scholar]
- 13. Hofmann SR, Roesen-Wolff A, Hahn G, et al. Update: cytokine dysregulation in chronic nonbacterial osteomyelitis (CNO). Int J Rheumatol 2012; 2012: 310206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ahmadinejad Z, Mansori S, Ziaee V, et al. Periodic Fever: A Review on Clinical, Management and Guideline for Iranian Patients - Part II. Iran J Pediatr 2014; 24 (3): 209– 240. [PMC free article] [PubMed] [Google Scholar]
- 15. Ferguson PJ, Chen S, Tayeh MK, et al. Homozygous mutations in LPIN2 are responsible for the syndrome of chronic recurrent multifocal osteomyelitis and congenital dyserythropoietic anaemia (Majeed syndrome). J Med Genet 2005; 4 2: 551– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hedrich CM, Hofmann SR, Pablik J, et al. Autoinflammatory bone disorders with special focus on chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol Online J 2013; 11 (1): 47– 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aksentijevich I, Masters SL, Ferguson PJ, et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med 2009; 360 (23): 2426– 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Girschick HJ, Raab P, Surbaum S, et al. Chronic non-bacterial osteomyelitis in children. Ann Rheum Dis 2005; 64 (2): 279– 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Edlund E, Johnsson U, Lidgren L, et al. Palmoplantar pustulosisand sternocostoclavicular arthro-osteitis. Ann Rheum Dis. 1988; 47 (10): 809– 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schilling F, Wagner AD. Azithromycin: an anti-inflammatory effect in chronic recurrent multifocal osteomyelitis? A preliminary report. Z Rheumatol 2000; 59 (5): 352– 3. [DOI] [PubMed] [Google Scholar]
- 21. Huber AM, Lam PY, Duffy CM, et al. Chronic recurrent multifocal osteomyelitis: clinical outcomes after more than five years of follow-up. J Pediatr 2002; 141 (2): 198– 203 [DOI] [PubMed] [Google Scholar]
- 22. Cruz AT, Starke JR. Clinical manifestations of tuberculosis in children. Paediatr Respir Rev 2007; 8 (2): 107– 17. [DOI] [PubMed] [Google Scholar]
- 23. Beck C, Morbach H, Beer M, et al. Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther 2010, 12 (2): R74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miettunen PM, Wei X, Kaura D, et al. Dramatic pain relief and resolution of bone inflammation following pamidronate in 9 pediatric patients with persistent chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol 2009; 7: 2– 15. [DOI] [PMC free article] [PubMed] [Google Scholar]


