Dear Editor
Extramedullary hematopiesis (EMH) is a response to insufficient blood cell production by producing of blood elements outside of the marrow cavity. It occurs most often due to hemolytic anemias such as thalasemia, hereditary spherocytosis and sickle cell anemia. It also could be seen in prolonged iron deficiency anemia, myelofibrosis, polycythemia, leukemia and lymphoma [1,2,3] .
EMH occurs most commonly in the reticuloendothelial system such as spleen and liver, but it may also be seen in organs, such as bowel, breast, brain, pleura and adrenals [2,4] .
In our review of literature we found reports of adrenal gland EMH in patients with beta-thalasemia, agnogenic myeloid metaplasia and hereditary spherocytosis. EMH in sickle cell anemia has been reported in paranasal sinuses, mediastinum and retroperitoneum.
Here we report a case of adrenal gland EMH as adrenal incidentaloma in a patient with sickle cell anemia; in literature review no similar result is found [1–8] .
The patient was a 15 year-old female with homozygous sickle cell disease. She was diagnosed as a case of sickle cell at the age of two years when she presented with bone pain. After that she was under routine clinical follow-up. She had history of multiple painful bone crises and one episode of acute splenic sequestration in childhood. During hospital course she complained of vague abdominal and left flank pain. In physical examination, findings were normal vital signs, pale conjunctivae and skin with mild soft hepatomegaly. No abdominal tenderness was noticed. No supra renal mass was detected on physical examination. Routine work/up for evaluation of abdominal pain was done.
Laboratory investigation showed hemoglobin 11 g/dL, WBC count 1.0×10 9 / L, platelet count 390×10 9 / L, MCV 70.1 fl, MCH 21.6 pg. Biochemical investigations were: serum bilirubin 1.8 mg/dL; conjugated bilirubin 0.8 mg/ dL, blood urea 27 mg/ dL, serum creatinine 0.7 mg/dL, serum calcium 8.2 mg/ dL, serum phosphorous 6.6 mg/dL, fasting blood sugar 100 mg/dL; alanine aminotransferase 41 IU/ dL, aspartate aminotransferase 50 IU/dL. Tests for hepatitis C virus (anti HCV antibody) and HIV antibodies (Anti HIV-1,2) serum HBsAg and HBc antibody were negative. Fasting serum cortisol level was 13 mcg/dL. Urinalysis was normal. Abdominal sonography showed mild hepatomegaly and a well-defined left suprarenal solid mass in size of 7.7×5.3 cm. Abdominal CT scan confirmed a 7cm well defined suprarenal mass (Fig 1).
Fig. 1:
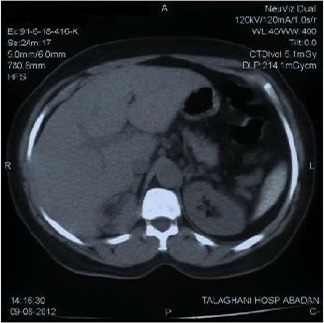
Right supra renal mass.
Surgical plan was considered and left adrenal-ectomy done. On gross examination, a brown mass measuring 7×5×3 cm was detected, surrounded with a rim of normal adrenal gland parenchyma.
The definite diagnosis was confirmed with histopathology that revealed active hematopoiesis in adrenal gland (extramedullary hemopoiesis) (Fig. 2). Her postoperative course was uneventful and she was discharged from hospital in good condition.
Fig. 2:
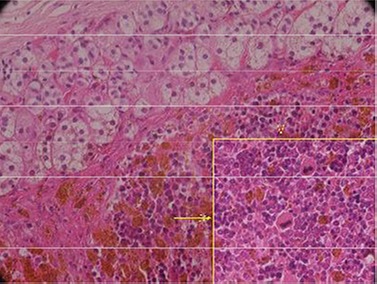
Remnant of adrenal cortical tissue with foci of hematopoietic cells including erythro-myeoloid, megakaryocytic cells with hemosiderin deposit (H&E ×400) (Yellow Arrow)
Adrenal incidentaloma has a prevalence of 5% in the general population. EMH is a rare cause of incidentaloma and is seen in patients with hematologic disorders such as beta-thalasemia, agnogenic myeloid metaplasia and hereditary spherocytosis.
EMH is a physiologic or pathologic compensatory mechanism that occurs because of imbalance between bone marrow erythropoiesis and circulatory blood demands. In histopathology, this intends to mimic a normal bone marrow with all marrow elements [1,2,3] .
EMH occurs most commonly in the reticuloendothelial system, but it may also be developed in organs such as lungs, gastrointestinal tract, breast, brain and kidney and rarely in adrenal [4,5] .
The exact mechanism of EMH in the adrenal gland is unknown, but several hypotheses are suggested. The adrenal gland has hematopoietic capacity during the fetal period and EMH may develop from primitive rests in diseased condition. Other scientists believe that embolization of hematopoietic stem cells and homing in adrenal gland may occur. Chronic hypoxia is another presumptive cause of EMH [3,6,7] .
EMH is seen in hemoglobinopathies such as thalassemia, hereditary spherocytosis and in hematologic diseases including myelofibrosis and myeloproliferative disorders. In the literature, most cases were associated with intermediate thalassemia. The frequency of extramedullary hematopiesis in thalassemia major was very low, especially, when ineffective erythropoiesis was suppressed by regular transfusion. In infrequent transfusion, chronic hypoxia and subsequently EMH develops [4,5,8,9] . EMH is rare in patients with sickle cell disease. Although few cases of intrathoracic, pelvic and paranasal have been documented in literature [8,9] , our case was the first one reported as adrenal incidentaloma.
EMH is usually asymptomatic and discovered incidentally. Symptomatic cases occur due to mass effect with compression to adjacent organ [8,9] . The surgical indication for excision of the adrenal incidentalomas is the tumor size. Adrenal tumor larger than 6 cm in diameter must be excised. In these cases, the risk of adrenal cancer is 35% to 98% [8,9] .
Treatment options for patients with EMH are described for thalassemia patients and depend on the location and symptoms. Different approaches included surgery, local radiation, blood transfusion and hydroxyurea. Hydroxyurea stimulates the synthesis of hemoglobin F and therefore participates in inactivation and shrinking of EMH. This effect was documented in thalassemia diseases. For paraspinal/epidural lesions, directed low-dose radiotherapy is recommended [9] . In conclusion, extramedullary hematopiesis should be considered in the differential diagnosis of patients with sickle cell disease that present with a solitary mass. The CT-guided biopsy can exclude a true neoplasm and alter the management and prognosis.
References
- 1. Sproat IA, Dobranowski J, Chen V, et al. Presacral extramedullary hematopoiesis in thalassemia intermedia. Can Assoc Radiol J 1991; 42 (4): 278– 82. [PubMed] [Google Scholar]
- 2. Chuang CK, Chu SH, Fang JT, et al. Adrenal extramedullary hematopoietic tumor in a patient with beta-thalassemia. J Formos Med Assoc 1998; 97 (6): 431– 3. [PubMed] [Google Scholar]
- 3. Porcaro AB, Novella G, Antoniolli SZ, et al. Adrenal extramedullary hematopoiesis: report on a pediatric case and update of the literature. Int Urol Nephrol 2001; 33 (4): 601– 3. [DOI] [PubMed] [Google Scholar]
- 4. King BF, Kopecky KK, Baker MK, et al. Extramedullary hematopoiesis in the adrenal glands: CT characteristics. J Comput Assist Tomogr 1987; 11 (2): 342– 3. [DOI] [PubMed] [Google Scholar]
- 5. Keikhaei B, Shirazi AS, Pour MM. Adrenal extramedullary hematopoiesis associated with β-thalassemia major. Hematol Rep 2012; 4 (2): e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bastounis EA, Karayiannakis AJ, Anapliotou ML, et al. Incidentalomas of the adrenal gland: diagnostic and therapeutic implications. Am Surg 1997; 63 (4): 356– 60. [PubMed] [Google Scholar]
- 7. Asnani M, Char G, Reid M, et al. Intrathoracic and pelvic extramedullary hematopoiesis in sickle cell disease: a case report. West Indian Med J 2007; 56 (6): 540– 3. [PubMed] [Google Scholar]
- 8. Verani R, Olson J, Moake JL. Intrathoracic extramedullary hematopoiesis: report of a case in a patient with sickle-cell disease-beta-thalassemia. Am J Clin Pathol 1980; 73 (1): 133– 7. [DOI] [PubMed] [Google Scholar]
- 9. Arkadopoulos N, Kyriazi M, Yiallourou AI, et al. A rare coexistence of adrenal cavernous hemangioma with extramedullar hemopoietic tissue: a case report and brief review of the literature. World J Surg Oncol 2009; 7: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]


