Abstract
Hepatic encephalopathy is a brain alteration associated to liver failure that produces cognitive impairments at long term. Neuroimaging are non-invasive methods for the study of the brain by means of spectroscopy and imaging techniques. These technologies give huge information about cerebral metabolism and water distribution to explore brain pathways involved in the pathogenesis of hepatic encephalopathy. Furthermore, new magnetic resonance implementations such as voxel-based morphometry or resting-state functional magnetic resonance imaging allow studying brain atrophy and neuronal connectivity of the cerebral network involved in the neurocognitive impairments observed in the patients. The development of magnetic resonance technology will generate handy tools for the brain study of liver failure to elucidate the time-course of the pathology and thus to obtain an early diagnosis of cerebral complications.
Keywords: magnetic resonance, spectroscopy, imaging, hepatic encephalopathy
Abbreviations: ADC, apparent diffusion coefficient; CFF, critical flicker frequency; fMRI, functional magnetic resonance imaging; HE, hepatic encephalopathy; MR, magnetic resonance; MRI, magnetic resonance imaging; MRS, magnetic resonance spectroscopy; MT, magnetization transfer; MTR, magnetization transfer ratio; NAA, N-acetyl aspartate; PHES, psychometric hepatic encephalopathy score; VBM, voxel-based morphometry
Hepatic encephalopathy (HE), a liver failure complication, is a metabolic encephalopathy that covers a wide range of neurological manifestations, from subtle cognitive deficits (MHE: minimal HE) to deep coma (overt HE). The ammonia accumulation and/or inflammation seem to be involved in the pathogenesis of HE; however, the time-course of these events is not well established. Classically, HE is classified in three types according to the origin of liver injury, type A HE is related to acute liver failure; type B HE to porto-systemic shunts; and type C to cirrhosis that additionally could be minimal (MHE) or overt (in that case could be episodic or persistent).1
Patients with MHE have not an apparent cognitive impairment and it is only detectable by some psychometric tests such as critical flicker frequency (CFF) or psychometric hepatic encephalopathy score (PHES). However, it is difficult to distinguish those cirrhotic patients with MHE from those without HE because of the lack of a “gold” standard in the diagnostic criteria of MHE. In addition, it was estimated that in the future some of these patients with MHE develops an overt HE. For this reason, an early diagnostic of MHE is crucial to avoid future cognitive complications.
Patients with overt HE have brain alterations, from mild upsets (e.g. confusion, depression, somnolence) to deep coma. The grades of HE are well established by neurological assessment (West Haven). Recently, operational definition of the severity of HE according to West Haven have been proposed (HESA: HE Scoring Algorithm).2 The HE grade, the number of episodes and the persistence of HE is important to minimize the long-term cognitive detriment of the patients, especially with chronic liver disease and these factors should be considered in the clinical management (e.g. treatment or transplant).3
Magnetic resonance
The magnetic resonance (MR) is a non-invasive technique used for the assessment of HE degree by spectroscopic and imaging clinical studies. Almost all studies in patients are based on proton signals from metabolites or water content among tissues and organs, respectively. These evaluations allow studying metabolic composition, anatomical structures or functional brain connectivity, according to the processing and the complexity of the sample.
MR spectroscopy (MRS) provides information about the metabolic status of the tissues. MRS consists in evaluating the proton relaxation of a small volume of tissue to obtain a spectrum of signals depending on frequency in which each metabolite has a specific position along the spectrum. This allows the identification of a compound in a mixture of metabolites and the metabolite concentration through the area below the peak. Proton MRS in brain mainly detects lactate (an end-product of anaerobic glycolysis); N-acetyl aspartate (NAA) (considered as neuronal marker); glutamate and glutamine (substrate and precursor of the amino acid involved in the excitatory neurotransmission); creatine and phosphocreatine (metabolites of energetic reservoir); choline derivates (cell membrane components); and myo-inositol (putative glia marker with unknown function).4
MR imaging (MRI) is based on proton signals from water content among tissues and organs. The conventional images in MRI are proton density in which the contrast is proportional to the amount of hydrogen, T1-weighted images that provide information of the T1 relaxation time of the tissues (fat tissue is bright while water is dark) and T2-weighted images give transverse relaxation of tissue trough T2 relaxation time (fluids are more brilliant than fat tissue).5
Techniques that are more sophisticated allow quantifying brain alterations of different pathologies such as water content, atrophy or connectivity. Magnetic transfer ratio (MTR) images offers contrast from the interactions between the protons in free fluid and those protons bound in macromolecules and both type of protons are in constant exchange. Low MTRs indicate reductions in brain structures in which exchange magnetization with the surrounding water molecules and could reflect myelin damage, cell destruction, or changes in water content.5 Diffusion imaging shows local water diffusion by the apparent diffusion coefficient (ADC) and a variant of this imaging, diffusion tensor imaging, gets different anisotropic parameters to study the structural integrity, additionally.6 Furthermore, the amount of brain water has also absolutely quantified using a complex method of MR.7
The volumetric measurements provide tools to determine brain atrophy by different strategies. Classically, these studies consisted in drawing regions of interest of whole brain or subparts (e.g. ventricles) on the brain images and calculating the volume enclosed.3 In recent years, voxel-based morphometry (VBM) has developed to analyze differences in brain anatomy using diverse statistical approaches.8
Currently, a huge MR area has been developed to explore brain activity by functional MRI (fMRI).9 These techniques are based in the assessment of local blood flow and hemoglobin oxygenation changes due to the metabolic changes because of brain activity. A subdivision is the resting-state fMRI that consists in studying the brain when the subject is not performing an explicit task due to cerebral activity.10 These studies are useful to explore the brain's functional connectivity as well as to examine alterations in neurological or psychiatric diseases.
Magnetic resonance studies in hepatic encephalopathy
Magnetic resonance (MR) is a non-invasive technique used for the assessment of HE degree by spectroscopic and imaging clinical studies. However, almost all clinical MR studies have performed in patients whose at the moment of the study did not have clear evidences of HE (cirrhotic patients without HE or with MHE) although those of them have suffered a previous episode of HE. On the contrary, only few articles were analyzed MR parameters during an episode of HE due to the complexity of management of these patients. These evaluations allow studying metabolic composition, brain edema, anatomical structures or functional brain connectivity alterations during one episode of HE (Figure 1).
Figure 1.
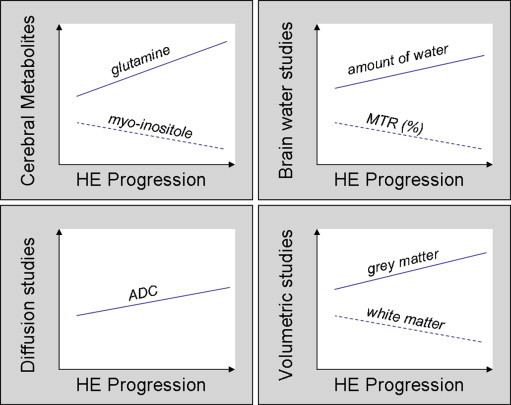
Schema of the general results found in MR studies according to the progression of HE.
Cerebral Metabolism
MRS followed the alterations of brain metabolites in the patients with cirrhosis. Proton spectroscopy studies showed a progressive increase in glutamine and glutamate peak according to the severity of HE (Table 1). In addition, a decrease in glutamine and glutamate peak was found after clinical resolution of HE episode.11,12 Myo-inositol had gradually decreased with the HE degree even though it did not find changes in overt HE probably due to technical limitations. Both metabolites changes are associated to compensatory mechanisms in the brain due to a cerebral osmolytes regulation produced by the increase in ammonia. On the contrary, the studies did not demonstrate any changes neither in choline derivates nor NAA except in advances stages of HE.12–14 These results are compatible with a loss of neurons that could be responsible to neurocognitive impairments observed in the patients.3
Table 1.
Proton magnetic resonance (MR) spectroscopy of cirrhotic patients with different grades of hepatic encephalopathy (HE).
| MR study | Subjects | n | Changes of ratios versus creatine compared to controls group | |||
|---|---|---|---|---|---|---|
| Glutamine | Myo-Inositol | Choline | NAA | |||
| (Poveda et al, 2010) | Control | 9 | ||||
| No HE | 9 | ↑ | ↓ | ≈ | ≈ | |
| Overt HE | 24 | ↑a,b | ↓ | ≈ | ≈ | |
| (Laubenberger et al, 1997) | Control | 20 | ||||
| No HE | 24 | ↑ | ↓ | ≈ | ≈ | |
| MHE | 4 | ↑ | ↓ | ≈ | ≈ | |
| Overt HE (I/II/III/IV) | 11 (4/6/0/1) | ↑b,c | ↓b | ≈ | ↓b | |
| (Tarasow et al, 2003) | Control | 20 | ||||
| No HE | 20 | ↑ | ↓ | ↓ | ≈ | |
| Overt HE (I/II/III/IV) | 14 (11/3/0/0) | ↑ | ↓b | ↓ | ≈ | |
| (Cordoba et al, 2001) | Control | 10 | ||||
| No HE | 24 | ↑ | ↓ | |||
| MHE | ↑b | ↓b | ||||
| (Chavarria et al, 2013) | Control | 8 | ≈ | ≈ | ||
| No HE | 7 | ↑ | ↓ | ≈ | ≈ | |
| Overt HE (I/II/III/IV) | 10 (5/3/0/2) | ↑a,c | ↓ | ↓c | ≈ | |
Decrease of values after recovery.
Significant changes between cirrhotic patients without HE (no HE), with minimal HE (MHE) or with overt HE.
Significant changes between the different HE grades (I/II/III/IV) in overt HE determined by West-Haven criteria where patients with grade I, exhibited lack of awareness; grade II, lethargy or apathy; grade III, somnolence to semi stupor; and grade IV, were in coma.
Brian Water Assessment
Cirrhotic patients with HE showed an increase in cerebral water that was analyzed directly or indirectly by MR (Table 2). MTR studies exhibited a continuous decrease of MTR according to the degree of HE. This indirect parameter denoted an increase in brain water. In addition, the loss of MTR increased in spatial extent and severity in patients with overt HE.15 The augment of water was related with the increase of cerebral ammonia but the time-course of the events was completely not clear. Quantitative MR experiments proved this rise of brain water in cirrhotic patients according to the HE progression.7
Table 2.
Brain water MR assessments of cirrhotic patients with different grades of hepatic encephalopathy (HE).
| MR study | Subjects | n | MR parameters compared to control group |
|
|---|---|---|---|---|
| MTR (%) | Amount of water | |||
| (Poveda et al, 2010) | Control | 9 | ||
| No HE | 9 | ↓a | ||
| Overt HE | 54 | ↓a | ||
| (Miese et al, 2009) | Control | 18 | ||
| No HE | 5 | ↓a | ||
| MHE | 3 | ↓a | ||
| Overt HE (I/II/III/IV) | 11 (6/5/0/0) | ↓a,b | ||
| (Cordoba et al, 2001) | Control | 10 | ||
| No HE | 24 | ↓a | ||
| MHE | ↓a | |||
| (Shah et al, 2008) | Control | 7 | ||
| No HE | 13 | ↑a | ||
| MHE | 12 | ↑a | ||
| Overt HE | 13 | ↑a | ||
Significant changes between cirrhotic patients without HE (no HE), with minimal HE (MHE) or with overt HE.
Significant changes between the different HE grades (I/II/III/IV) in overt HE determined by West-Haven criteria where patients with grade I, exhibited lack of awareness; grade II, lethargy or apathy; grade III, somnolence to semi stupor; and grade IV, were in coma.
The distribution of cerebral water in cirrhotic patients can be studied by means of diffusion studies. The interpretation of the results is still a matter of debate but the majority of authors interpret that an increase in diffusion corresponds to a rise of extracellular brain water. There are only two studies in humans that have applied diffusion weighted imaging during an overt episode of HE (Table 3). While Poveda and colleagues showed no changes in ADC during HE11; in our study we found an increase in ADC values in cirrhotic patients specially in those with high-grade HE12. Indeed, both studies also showed a decrease in ADC after the resolution of HE, supporting an increase of extracellular water during episodic HE in chronic liver failure. The behavior of diffusion parameters was different from those observed in different liver failure (acute or acute-on-chronic liver failure) (Table 4). Acute liver failure patients exhibited a decrease in ADC attributed to an increase of intracellular water.16–18 Controversially, acute-on-chronic patients showed the same alterations in diffusion tensor parameters of liver failure without changes in ADC that could suggest to the presence of mixed cerebral edema (intracellular and extracellular).19 These results show the complexity of brain edema in physiopathology of liver failure.
Table 3.
Diffusion studies of cirrhotic patients with different grades of hepatic encephalopathy (HE).
| MR study | Subjects | n | ADC values |
|
|---|---|---|---|---|
| HE episode | HE recovery | |||
| (Poveda et al, 2010) | Control | 9 | ||
| No HE | 9 | ≈ | ||
| Overt HE | 24 | ≈ | ↓ | |
| (Chavarria et al, 2013) | Control | 8 | ||
| No HE | 7 | ↑a | ||
| Overt HE (I/II/III/IV) | 10 (5/3/0/2) | ↑b | ↓ | |
Significant changes between cirrhotic patients without HE (no HE), with minimal HE (MHE) or with overt HE.
Significant changes between the different HE grades (I/II/III/IV) in overt HE determined by West-Haven criteria where patients with grade I, exhibited lack of awareness; grade II, lethargy or apathy; grade III, somnolence to semi stupor; and grade IV, were in coma.
Table 4.
Diffusion studies according to the origin of liver failure.
| MR studies | Liver failure | MR parameters compared to control group |
|||
|---|---|---|---|---|---|
| ADC/MD |
Diffusion tensor parameters |
||||
| FA | CL | CS | |||
| (Nath et al 2008) | Chronic | ↑ | ↓ | ↓ | ↑ |
| (Nath et al 2008) | Acute-on-chronic | ≈ | ↓ | ↓ | ↑ |
| (Ranjan et al 2005; Rai et al 2008; Saksena et al 2008) | Acute | ↓ | ↓ | ↓ | ↑ |
MR parameters: ADC, apparent diffusion coefficient; MD, mean diffusivity; FA, fractional anisotropy; CL, lineal anisotropy; CS, spherical anisotropy.
Atrophy
VBM are a new MR strategy to perform volumetric studies of brain and subsequently to address atrophy (Table 5). MR experiments with this approach showed that cirrhotic patients had many areas with a decrease in gray matter volume and an increase in white matter volume, compared to healthy controls, which were further aggravated with the HE progression.20,21 These results are compatible with brain atrophy because of the severity of HE. However, Tarasow and co-workers obtained no differences in the atrophy between cirrhotic patients and overt HE.14
Table 5.
Volumetric studies by magnetic resonance (MR) of cirrhotic patients with different grades of hepatic encephalopathy (HE).
| MR study | Subjects | n | Brain density or brain volume compared to control |
|
|---|---|---|---|---|
| Gray matter | White matter | |||
| (Guevara et al, 2011)a | Control | 51 | ||
| No HE | 48 | ↓ | ↓ | |
| (Zhang et al, 2012)b | Control | 40 | ||
| No HE | 31 | ↓c | ↑c | |
| MHE | 18 | ↓c | ↑c | |
| Overt HE | 11 | ↓c | ↑c | |
Voxel-based morphometry study of brain density.
Voxel-based morphometry study of brain volume.
Significant changes between cirrhotic patients without HE (no HE), with minimal HE (MHE) or with overt HE.
Cognitive Function Evaluation
Recently, a cognitive detriment in cirrhotic patients was made obvious especially in those patients that suffered previous episodes of HE. For this reason, resting-state fMRI was developed to evaluate functional connectivity within the default-mode network. Neurocognitive impairments were observed in cirrhotic patients after an apparent recovery of the overt HE (with MHE or without HE and a previous episode of HE), despite normal mental status.22,23 In addition, Zhang and colleagues discovered a reduced tendency of the functional connectivity within the default-mode network in patients with an overt episode of HE.24
Conclusion
HE seems to be an important factor for the follow-up of cirrhotic patients in particular for the cognitive function. In addition, severe brain atrophy is likely involved in the mechanisms underlying incomplete resolution of overt HE. Both functional and structural cerebral impairments after resolution of an overt episode of HE reveals irreversible effects induced by HE on brain function and provide a basis for further evolution of the disease. A refinement of HE diagnostic above MHE could be decisive to avoid future cognitive dysfunction. Maybe other parameters could be taking into account for a better diagnosis of MHE and thus to prevent early decline of cognitive function.
Financial support
CIBEREHD is supported by Instituto de Salud Carlos III, Madrid, Spain.
Conflicts of interest
All authors have none to declare.
References
- 1.Prakash R., Mullen K.D. Mechanisms, diagnosis and management of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010 September;7(9):515–525. doi: 10.1038/nrgastro.2010.116. [DOI] [PubMed] [Google Scholar]
- 2.Hassanein T., Blei A.T., Perry W. Performance of the hepatic encephalopathy scoring algorithm in a clinical trial of patients with cirrhosis and severe hepatic encephalopathy. Am J Gastroenterol. 2009 June;104(6):1392–1400. doi: 10.1038/ajg.2009.160. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Martinez R., Rovira A., Alonso J. Hepatic encephalopathy is associated with posttransplant cognitive function and brain volume. Liver Transpl. 2011 January;17(1):38–46. doi: 10.1002/lt.22197. [DOI] [PubMed] [Google Scholar]
- 4.Govindaraju V., Young K., Maudsley A.A. Proton NMR chemical shifts and coupling constants for brain metabolites. NMR Biomed. 2000 May;13(3):129–153. doi: 10.1002/1099-1492(200005)13:3<129::aid-nbm619>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 5.Filippi M., Rocca M.A., De S.N. Magnetic resonance techniques in multiple sclerosis: the present and the future. Arch Neurol. 2011 December;68(12):1514–1520. doi: 10.1001/archneurol.2011.914. [DOI] [PubMed] [Google Scholar]
- 6.LeBihan D., Mangin J.F., Poupon C. Diffusion tensor imaging: concepts and applications. J Magn Reson Imaging. 2001 April;13(4):534–546. doi: 10.1002/jmri.1076. [DOI] [PubMed] [Google Scholar]
- 7.Shah N.J., Neeb H., Kircheis G., Engels P., Haussinger D., Zilles K. Quantitative cerebral water content mapping in hepatic encephalopathy. Neuroimage. 2008 July 1;41(3):706–717. doi: 10.1016/j.neuroimage.2008.02.057. [DOI] [PubMed] [Google Scholar]
- 8.Ashburner J., Friston K.J. Voxel-based morphometry–the methods. Neuroimage. 2000 June;11(6 Pt 1):805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- 9.Matthews P.M., Jezzard P. Functional magnetic resonance imaging. J Neurol Neurosurg Psychiatr. 2004 January;75(1):6–12. [PMC free article] [PubMed] [Google Scholar]
- 10.Gusnard D.A., Raichle M.E., Raichle M.E. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001 October;2(10):685–694. doi: 10.1038/35094500. [DOI] [PubMed] [Google Scholar]
- 11.Poveda M.J., Bernabeu A., Concepcion L. Brain edema dynamics in patients with overt hepatic encephalopathy A magnetic resonance imaging study. Neuroimage. 2010 August 15;52(2):481–487. doi: 10.1016/j.neuroimage.2010.04.260. [DOI] [PubMed] [Google Scholar]
- 12.Chavarria L., Alonso J., Garcia-Martinez R. Brain magnetic resonance spectroscopy in episodic hepatic encephalopathy. J Cereb Blood Flow Metab. 2013 February;33(2):272–277. doi: 10.1038/jcbfm.2012.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laubenberger J., Haussinger D., Bayer S., Gufler H., Hennig J., Langer M. Proton magnetic resonance spectroscopy of the brain in symptomatic and asymptomatic patients with liver cirrhosis. Gastroenterology. 1997 May;112(5):1610–1616. doi: 10.1016/s0016-5085(97)70043-x. [DOI] [PubMed] [Google Scholar]
- 14.Tarasow E., Panasiuk A., Siergiejczyk L. MR and 1H MR spectroscopy of the brain in patients with liver cirrhosis and early stages of hepatic encephalopathy. Hepatogastroenterology. 2003 November;50(54):2149–2153. [PubMed] [Google Scholar]
- 15.Miese F.R., Wittsack H.J., Kircheis G. Voxel-based analyses of magnetization transfer imaging of the brain in hepatic encephalopathy. World J Gastroenterol. 2009 November 7;15(41):5157–5164. doi: 10.3748/wjg.15.5157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rai V., Nath K., Saraswat V.A., Purwar A., Rathore R.K., Gupta R.K. Measurement of cytotoxic and interstitial components of cerebral edema in acute hepatic failure by diffusion tensor imaging. J Magn Reson Imaging. 2008 August;28(2):334–341. doi: 10.1002/jmri.21438. [DOI] [PubMed] [Google Scholar]
- 17.Ranjan P., Mishra A.M., Kale R., Saraswat V.A., Gupta R.K. Cytotoxic edema is responsible for raised intracranial pressure in fulminant hepatic failure: in vivo demonstration using diffusion-weighted MRI in human subjects. Metab Brain Dis. 2005 September;20(3):181–192. doi: 10.1007/s11011-005-7206-z. [DOI] [PubMed] [Google Scholar]
- 18.Saksena S., Rai V., Saraswat V.A. Cerebral diffusion tensor imaging and in vivo proton magnetic resonance spectroscopy in patients with fulminant hepatic failure. J Gastroenterol Hepatol. 2008 July;23(7 Pt 2):e111–e119. doi: 10.1111/j.1440-1746.2007.05158.x. [DOI] [PubMed] [Google Scholar]
- 19.Nath K., Saraswat V.A., Krishna Y.R. Quantification of cerebral edema on diffusion tensor imaging in acute-on-chronic liver failure. NMR Biomed. 2008 August;21(7):713–722. doi: 10.1002/nbm.1249. [DOI] [PubMed] [Google Scholar]
- 20.Zhang L.J., Qi R., Zhong J., Xu Q., Zheng G., Lu G.M. The effect of hepatic encephalopathy, hepatic failure, and portosystemic shunt on brain volume of cirrhotic patients: a voxel-based morphometry study. PLoS One. 2012;7(8):e42824. doi: 10.1371/journal.pone.0042824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guevara M., Baccaro M.E., Gomez-Anson B. Cerebral magnetic resonance imaging reveals marked abnormalities of brain tissue density in patients with cirrhosis without overt hepatic encephalopathy. J Hepatol. 2011 September;55(3):564–573. doi: 10.1016/j.jhep.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 22.Chen H.J., Zhu X.Q., Shu H. Structural and functional cerebral impairments in cirrhotic patients with a history of overt hepatic encephalopathy. Eur J Radiol. 2012 October;81(10):2463–2469. doi: 10.1016/j.ejrad.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Chen H.J., Jiao Y., Zhu X.Q. Brain dysfunction primarily related to previous overt hepatic encephalopathy compared with minimal hepatic encephalopathy: resting-state functional MR imaging demonstration. Radiology. 2013 January;266(1):261–270. doi: 10.1148/radiol.12120026. [DOI] [PubMed] [Google Scholar]
- 24.Zhang L., Qi R., Wu S. Brain default-mode network abnormalities in hepatic encephalopathy: a resting-state functional MRI study. Hum Brain Mapp. 2012 June;33(6):1384–1392. doi: 10.1002/hbm.21295. [DOI] [PMC free article] [PubMed] [Google Scholar]


