Abstract
Objectives
To evaluate the detection of clinically unsuspected pathologies using 64-slice multidetector computed tomography (CT) of the abdomen in patients with flank pain. The presence of significant incidental findings (those warranting immediate management) was also correlated with that of urolithiasis, to assess potential changes of management.
Patients and methods
The study included 899 patients undergoing CT in a 6-month period between June and December 2008. Patients who were referred from outside, with no medical record in the hospital where the study was conducted, and those who were lost to follow-up, were excluded. All of the CT examinations were reported after a radiology resident and a consultant radiologist with >4 years of experience evaluated the CT. Genitourinary and extra-genitourinary findings were assessed and divided into clinically significant or not.
Results
The overall incidence of additional and incidental findings was 14%. Besides urolithiasis and obstruction there were 34 (28%) genitourinary findings and 87 (72%) extra-genitourinary findings; most of the former were insignificant. Of the extra-genitourinary findings, significant diagnoses were documented in 34 cases.
Conclusions
Abdominal multidetector CT detects more incidental findings which are clinically significant.
Abbreviations: GU, genitourinary; KUB, kidneys, ureters and bladder; MD, multidetector
Keywords: CT, Incidental findings, Clinical significance, Genitourinary, Incidental cancer
Introduction
Unenhanced CT of the kidneys, ureters and bladder (CT KUB) is rapidly replacing IVU as the method of choice for imaging patients with ureteric colic and suspected urolithiasis [1,2]. Trends in the use of CT KUB and IVU show a major change in the number of referrals for CT KUB in comparison to IVU [3]. There are abundant data available showing the higher sensitivity of CT KUB for detecting urolithiasis [4–6]. Sagittal and coronal reformatted images also add important information to the diagnostic findings [7]. Complications and secondary signs of obstruction, such as perirenal and peri-ureteric fat stranding, can also be identified with CT KUB [5]. The overall costs are much lower for CT KUB as it saves significant amount of time [4]. It is safer, as no contrast material is given, but the radiation dose is higher [4,5]. Radiation exposure is still a major challenge in the use of CT for the diagnosis and follow-up of ureterolithiasis and obstruction [8]. Although there are obvious difficulties in comparing the exact effective dose between various imaging methods, measurements made to compare IVU and spiral CT by De Denaro et al. [9] showed that the effective dose for CT is 3.3 times that for IVU.
CT KUB is most advantageous in those patients where the clinical presentation can be vague, might overlap more than one body system, or symptoms are present from two different disease processes. It is also beneficial in those patients where the physician feels that the disease process has progressed to a complication. Even physicians have recognised the diagnostic capability of CT KUB and refer patients with a variety of clinical histories other than urolithiasis [10]. CT KUB has the advantage over other imaging methods used for urolithiasis by its diagnostic potential in diagnosing disease processes that present with symptoms of urolithiasis or disease processes that need to be closely followed or need further evaluation, such as a mass [11–14].
One of the major advantages of CT KUB over IVU is its ability to diagnose alternative causes of abdominal pain and significant incidental diagnoses that can affect health [10–12]. In the present study we aimed to evaluate the detection of incidental pathologies using 64-slice multidetector (MD) CT. In addition, the presence of significant incidental findings (those warranting immediate management) was correlated with that of urolithiasis to assess potential changes of management.
Patients and methods
In all, 899 patients underwent CT KUB examinations from June 2008 to December 2008 at a 600-bed tertiary-care centre. All patients who were referred from the emergency department, from hospital clinics and those who were inpatients were included in the study. The patients referred from outside the hospital were excluded as no clinical history or other medical records besides the radiology report were available to evaluate these patients. Seven more were excluded as their images were substandard or their reports were not available for review, most probably as they had the images taken before the report. Overall 67 patients were excluded from the study.
The CT KUB reports of the 832 patients finally included in the study were reviewed retrospectively after the final official report was available on our radiology information system. All of the CT KUB examinations are reported after a radiology Resident and a consultant radiologist with >4 years of experience had evaluated the CT. The final report was generated after a consultation between the radiology team members. All those examinations that had incidental and additional findings from the entire data were reviewed by a Resident with 3 years of experience and consultant radiologist with 4 years of experience.
Patients with incidental or additional findings were further evaluated by dividing them into different groups and subgroups. In one group the incidental/additional findings were put into two groups, i.e. significant and insignificant. The group of significant findings included those disease processes that required the immediate attention of the referring physician for further management or evaluation. These patients with significant findings were further divided into subgroups to see if they also had no urolithiasis, unobstructive or obstructive urolithiasis. The incidental findings were also divided into genitourinary (GU) findings and non-GU findings. All CT examinations were conducted on a 64-slice MD machine (Aquilion, Toshiba Medical Systems, Shimoishigami, Otawara-Shi, Japan). The images were viewed on picture-archiving computer system (View Pro-X version 4.0.6.2; Rogan-Delft, Veenendaal, Holland) with 5-mm axial sections. Reformatted 3-mm coronal and sagittal sections of all examinations were also constructed at the time of reporting. Volume data with 0.5 mm sections were also available if needed. The CT procedure used exposure factors set at 120 kV and 250–300 mA. The abdomen was scanned from the level of the xiphisternum to the lower border of the symphysis pubis, using 5-mm collimation with patient supine once they had the urge to void. Additional views were obtained with the patient prone, if needed for confirmation of suspected distal ureteric calculi. The time for the scan was ≈16 s.
Apart from the GU and non-GU categories, and significant or insignificant diagnosis, the patients were also divided into those who needed immediate treatment (e.g. for acute inflammatory conditions such as appendicitis and cholecystitis), or later treatment that could be delayed, i.e. an insignificant diagnosis of conditions that did not need immediate attention or need to be reconfirmed.
Tumours, aneurysms (abdominal aortic aneurysm of >5 cm or iliac artery aneurysm of >2 cm), enlarged lymph nodes (>1 cm) or chronic inflammatory disease were defined as findings requiring deferred treatment. Benign lesions that would require treatment later were defined as findings of little clinical importance. Examples are a complicated cyst, adrenal adenoma (Fig. 1), angiomyolipoma, haemangioma, hernia without incarcerated bowel, cholecystolithiasis, marked organ enlargement or atrophy (uterus, prostate, liver, spleen or kidney) or vascular ectasia. Findings of no clinical importance were those considered to be benign and unlikely to require any future treatment or additional assessment. These findings were anatomical variants, uncomplicated cysts, benign calcifications and congenital anomalies.
Figure 1.
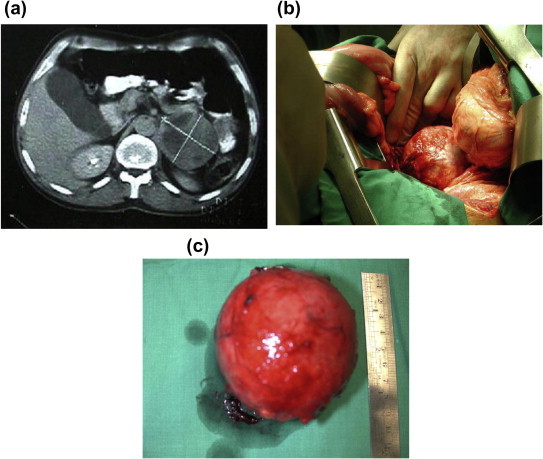
A 45-year-old man presented with acute-onset left-flank pain. He complained of mild flank discomfort, but there was acute exacerbation that brought him to the emergency department. The CT for suspected ureteric colic showed a moderate-sized left adrenal mass (a). After a detailed endocrinological evaluation, which showed no abnormality, he underwent an open left adrenalectomy via a thoraco-abdominal approach (b), and a well-encapsulated 9 × 5 cm mass was removed (c).
Patients were also stratified for the presence or otherwise of urolithiasis and obstruction. They included patients with additional diagnosis, besides obstructive urolithiasis, and other significant diagnoses. Patients with alternative diagnoses were those with no obstructive but with other significant diagnosis. Missed diagnoses were a group with no urolithiasis and obstruction but with other significant conditions. All relevant radiological examinations and laboratory analyses were analysed for the confirmation of patient’s incidental/additional findings. Patient’s medical record files and radiology referral forms were evaluated for the clinical history and pre-clinical and follow-up examinations.
A one-sample t-test was used to assess whether a sample mean (of a normally distributed interval variable) differed significantly from a hypothesised value. The chi-square test was used to assess the relationship between two categorical variables.
The study was approved by the institutional review board; all efforts were made to accurately report data, and to follow all institutional and international guidelines for the publication of original work.
Results
In 832 evaluable patients who had CT KUB for suspected urolithiasis, 121 (14.5%) had 177 (21.4%) additional or alternative diagnoses, besides urolithiasis and obstruction. Of the 121 patients with additional findings, 22 had obstructive urolithiasis, 32 had unobstructive stones, whereas 67 had no evidence of stone disease. In 121 patients with additional/incidental diagnoses, there were 72 males and 49 females. In the studied cohort the incidence of incidental and alternative diagnoses in men was 60%. The median (SD) age of the cohort was 28.6 (16.4) years, and the median (SD) age of patients who had incidental/additional diagnoses was 38.5 (11.4) years.
There were 37 (28%) GU findings and 87 (72%) non-GU findings; in the former (Table 1) the most frequent finding was a renal cyst (eight) followed by an ovarian cyst (seven) and uterine masses, suspected to be leiomyomas (seven). Six (17%) male patients had thick-walled bladders, indicating distal obstruction. All of these had an urodynamic evaluation confirming the diagnosis. There were also three patients with dermoid, two with hydrosalpinx and one case of cervical mass. Two patients had a malpositioned kidney, including a horseshoe kidney and ectopic pelvic kidney. Significant non-GU findings were documented in 37 cases (Table 2).
Table 1.
Clinical significance and confirmation using other imaging, pathology, etc. of alternative or additional diagnoses of the GU tract.
| Other diagnoses | No. | Confirmation | Clinical significance |
|---|---|---|---|
| Dermoid | 3 | Yes | DT |
| Leiomyoma | 7 | Yes | DT |
| Cervix mass | 1 | Yes | II |
| Hydrosalpinx | 2 | Yes | DT |
| Renal cyst | 8 | Yes | NCI |
| Ovary cyst | 7 | Yes | LCI |
| BOO | 6 | Yes | II |
| Malpositioned kidney | 2 | Yes | LCI |
| Vesico-enteric fistula | 1 | Yes | II |
II, requires immediate intervention; DT, deferred treatment; LCI, little clinical importance; NCI, no clinical importance.
Table 2.
Details of significant non-GU findings.
| Significant incidental findings | No. | No. confirmed⁎ | N patients with urolithiasis | Clinical significance |
|---|---|---|---|---|
| Abscess | 7 | 5 | 3 | II |
| Haematoma (retroperitoneal) | 1 | 1 | 1 | DT |
| Appendicitis | 15 | 11 | 1 | II |
| Pancreatitis | 3 | 2 | 2 | II |
| Masses | 6 | 0 | 5 | |
| Adrenal incidentaloma | 3 | DT | ||
| Cervical | 1 | II | ||
| Gall bladder | 1 | II | ||
| Liver | 1 | II | ||
| Aortic aneurysm | 2 | 2 | 0 | LCI |
On clinical, pathology or by other imaging. II, requires immediate intervention; DT, deferred treatment; LCI, little clinical importance; NCI, no clinical importance.
There was more than one condition in 15 patients; two patients had four conditions, three had three conditions and 10 had two diagnoses. Of these, 21 (62%) had no urolithiasis, eight (24%) had an unobstructive small stone and five (15%) had an obstructive calculus (Figs. 1 and 2).
Figure 2.

A coronal section of an unenhanced CT taken for right ureteric colic. No urolithiasis was identified. However, a dilated tubular blind-ended bowel loop (arrow) arising from the caecum (arrowhead) with surrounding fat stranding was apparent, consistent with acute appendicitis.
Discussion
The incidence of findings in the present study was 14%, and thus somewhat higher than those reported in some contemporary series [10–12], including from the present centre on a 16-slice CT system [11,12]. This could be due to both the higher resolution of MD CT and greater awareness among radiologists to actively seek other causes. There has been no direct comparison of MD CT and 16-slice scanners; therefore it is difficult to ascertain whether the higher detection rate is related directly to the quality of the scanner or the disease pattern at different times. A recent report from the American College of Radiology [15] on managing incidental findings noted that most of the incidental findings are probably benign and often have little or no clinical significance; the inclination to evaluate them is often driven by the physician and patient being unwilling to accept uncertainty, even given the rare possibility of an important diagnosis. As some of the incidental findings can have serious consequences (Figs. 3 and 4), there should be clearer guidelines on when and how to evaluate them. However, there are other conditions which are important to recognise, although they might not be life-threatening (Fig. 5). The evaluation of incidentaloma has varied widely both by physician and region, and some standardisation is desirable in the light of the current need to limit costs and reduce the risk to patients. Subjecting a patient with an incidentaloma to unnecessary testing and treatment can result in a potentially injurious and expensive cascade of tests and procedures [16].
Figure 3.

A coronal section of unenhanced CT of a 59-year-old women who complained of right loin pain. CT showed no urolithiasis. Incidentally, a large gallstone (arrow) and hiatus hernia (between arrowheads) was apparent.
Figure 4.

An axial section of unenhanced CT in a 32-year-old man complaining of left renal pain. CT showed two small unobstructing calculi in the left kidney (not shown). However, the tail of the pancreas was swollen (star) with surrounding fat stranding (arrows) consistent with acute pancreatitis.
Figure 5.
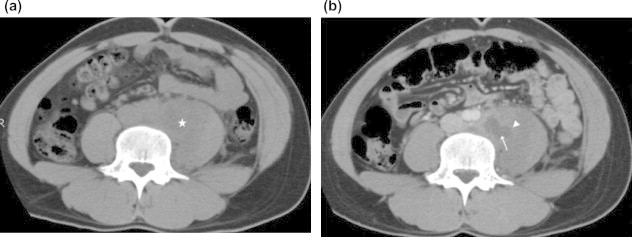
An axial section of unenhanced CT in a 25-year-old man with right renal colic. Initial ultrasonography showed left renal hydronephrosis. The CT (a) shows enlarged left psoas muscles (star) compared to the right psoas muscle. Subsequently contrast-enhanced CT (b) was used, which confirmed a psoas abscess (arrow) with enhancing margins (arrowhead) and inflammatory changes causing enlargement of the left psoas muscle. This was the cause of obstruction of the left ureter, resulting in left renal hydronephrosis, detected on ultrasonography (c).
Alternative diagnoses and incidental findings on unenhanced CT for suspected urolithiasis and obstruction are a recognised advantage over other methods [10–12]. This is not only noted for CT KUB but also for CT used for other reasons. Naidu et al. [16] noted that, unlike conventional angiography, CT angiography can detect abnormalities outside the vascular system. The clinical significance of these findings can range from trivial and of no clinical importance to highly important findings requiring further evaluation or treatment. Awareness of the incidence and clinical significance of these findings at CT is important for many reasons. Most importantly, it calls attention to the many findings that lie outside the GU system and underscores the importance of careful interpretation of the entire CT findings. Also, these studies are often referred to radiologists from the urologists. When important incidental GU and extra-GU findings are reported, appropriate follow-up or referrals can be made.
The main limitations of the present study include that it was retrospective, and the percentage of patients who were lost to clinical and imaging follow-up. If these patients had been followed it is possible that the percentage of undiagnosed malignancies would be higher. Because this study was based on a review of radiology reports, there was variability among radiologists in how the findings were interpreted. However, this variability reflects most clinical practices in which numerous radiologists interpret these examinations. Finally, another limitation lies in the lack of standardisation in the reporting of findings of high clinical significance, making comparison between such studies difficult.
In conclusion, MD CT KUB detect many incidental findings, more than those reported in contemporary studies, including two series from our centre [12,13]. However, there has been no direct comparison reported to date of the two generations of CT scanners. In addition, patients with obstructive calculus were noted to have additional findings that can change their management. Hence, MD CT KUB detect significant conditions, with effects on the course of clinical management.
Conflict of interest
The authors have no conflict of interest to declare.
References
- 1.Smith R.C., Verga M., McCarthy S., Rosenfield A.T. Diagnosis of acute flank pain: value of unenhanced helical CT. AJR Am J Roentgenol. 1996;166:97–101. doi: 10.2214/ajr.166.1.8571915. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad N.A., Ather M.H., Rees J. Unenhanced helical computed tomography in the evaluation of acute flank pain. Int J Urol. 2003;10:287–292. doi: 10.1046/j.1442-2042.2003.00628.x. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed F., Zafar A.M., Khan N., Haider Z., Ather M. Hammad. A paradigm shift in imaging for renal colic – Is it time to say good bye to an old trusted friend? Int J Surg. 2010;8:252–256. doi: 10.1016/j.ijsu.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 4.Pfister S.A., Deckart A., Laschke S., Dellas S., Otto U., Buitrago C. Unenhanced helical computed tomography vs intravenous urography in patients with acute flank pain. accuracy and economic impact in a randomized prospective trial. Eur Radiol. 2003;13:2513–2520. doi: 10.1007/s00330-003-1937-1. [DOI] [PubMed] [Google Scholar]
- 5.Ryu J.A., Kim B., Jeon Y.H., Lee J., Lee J.W., Jeon S.S. Unenhanced spiral CT in acute ureteral colic: a replacement for excretory urography? Korean J Radiol. 2001;2:14–20. doi: 10.3348/kjr.2001.2.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sourtzis S., Thibeau J.F., Damry N., Raslan A., Vandendris M., Bellemans M. Radiologic investigation of renal colic: unenhanced helical CT compared with excretory urography. AJR Am J Roentgenol. 1999;172:1491–1494. doi: 10.2214/ajr.172.6.10350278. [DOI] [PubMed] [Google Scholar]
- 7.Lin W.C., Wang J.H., Wei C.J., Chang C.Y. Assessment of CT urography in the diagnosis of urinary tract abnormalities. J Chin Med Assoc. 2004;67:73–78. [PubMed] [Google Scholar]
- 8.Ather M.H., Memon W.A. Stones. Impact of dose reduction on CT detection of urolithiasis. Nat Rev Urol. 2009;6:526–527. doi: 10.1038/nrurol.2009.196. [DOI] [PubMed] [Google Scholar]
- 9.De Denaro M., Bregant P., Cupardo F., De Guarrini F., Rimondini A., Pozzi Mucelli R. Effective dose in X-ray examinations. comparison between spiral CT and urography in the study of renal colic. Radiol Med. 2001;102:256–261. [PubMed] [Google Scholar]
- 10.Chen M.Y., Zagoria R.J., Saunders H.S., Dyer R.B. Trends in the use of unenhanced helical CT for acute urinary colic. AJR Am J Roentgenol. 1999;173:1447–1450. doi: 10.2214/ajr.173.6.10584780. [DOI] [PubMed] [Google Scholar]
- 11.Katz D.S., Scheer M., Lumerman J.H., Mellinger B.C., Stillman C.A., Lane M.J. Alternative or additional diagnoses on unenhanced helical computed tomography for suspected renal colic: experience with 1000 consecutive examinations. Urology. 2000;56:53–57. doi: 10.1016/s0090-4295(00)00584-7. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad N.A., Ather M.H., Rees J. Incidental diagnosis of diseases on un-enhanced helical computed tomography performed for ureteric colic. BMC Urol. 2003;3:2. doi: 10.1186/1471-2490-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ather M.H., Faizullah K., Achakzai I., Siwani R., Irani F. Alternate and incidental diagnoses on noncontrast-enhanced spiral computed tomography for acute flank pain. Urol J. 2009;6:14–18. [PubMed] [Google Scholar]
- 14.Hoppe H., Studer R., Kessler T.M., Vock P., Studer U.E., Thoeny H.C. Alternate or additional findings to stone disease on unenhanced computerized tomography for acute flank pain can impact management. J Urol. 2006;175:1725–1730. doi: 10.1016/S0022-5347(05)00987-0. [DOI] [PubMed] [Google Scholar]
- 15.Berland L.L., Silverman S.G., Gore R.M., Mayo-Smith W.W., Megibow A.J., Yee J. Managing incidental findings on abdominal CT. White paper of the ACR incidental findings committee. J Am Coll Radiol. 2010;7:754–773. doi: 10.1016/j.jacr.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Naidu S.G., Hara A.K., Brandis A.R., Stone W.M. Incidence of highly important extravascular findings detected on CT angiography of the abdominal aorta and the lower extremities. AJR Am J Roentgenol. 2010;194:1630–1634. doi: 10.2214/AJR.09.3538. [DOI] [PubMed] [Google Scholar]


