Abstract
Objective
To highlight the role of open stone surgery in the management of urolithiasis in the current era of minimally invasive therapies. The introduction and continuous development of extracorporeal shockwave lithotripsy (ESWL), ureterorenoscopy and percutaneous nephrolithotomy (PCNL) over the past 30 years have led to a significant change in the current management of urolithiasis, where the indications for open stone surgery have been narrowed significantly, making it a second- or third-line treatment option.
Methods
We reviewed the most recent guidelines published by the European Association of Urology and the American Urological Association, and reviewed reports through a MEDLINE search to identify the indications and current role of open stone surgery.
Results
From the MEDLINE search, it was obvious that the number of papers published on open renal stone surgery has decreased during the last three decades, soon after the introduction of ESWL and PCNL.
Conclusion
Although currently most patients with stones can be managed by minimally invasive therapy, we believe that open surgery still has a role, and therefore it is of great importance to recognise that a small group of patients with complex stone disease, and those with anatomical and physiological anomalies, will benefit from this treatment option.
Abbreviations: PCNL, percutaneous nephrolithotomy; EAU, European Association of Urology
Keywords: Urolithiasis, Open stone surgery, PCNL, ESWL, Guidelines
Introduction
The surgical treatment of urolithiasis has changed significantly over the past 30 years. Previously, most patients requiring stone removal underwent open surgery [1]. Whereas senior urologists are able to recall the era before the 1980s, when they routinely had to ‘cut for the stone’, open surgery for stone disease of the urinary tract is almost unknown among the latest generation of urologists who were trained during the past 10–15 years.
Advances in the endoscopic management of stone disease, in the form of ureteroscopy, percutaneous nephrolithotomy (PCNL) and laparoscopy, initially promoted a rapid decrease in the use of this approach [2]. The introduction of ESWL into routine clinical practice by Chaussy et al. [3] in 1982 has further reduced the indications for open stone surgery, as currently ESWL is the most widely used method of managing renal and ureteric calculi. Therefore, and as a result, open stone surgery has become a second- or third-line treatment option. Centres worldwide with the equipment, expertise and experience in the surgical treatment of renal tract stones report that open surgery is needed in 1–5.4% of cases [4–7].
Methods
We reviewed the most recent guidelines published by the European Association of Urology (EAU) and the AUA, and reviewed reports through a MEDLINE search between 1980 and March 2012, to identify the indications and current role of open stone surgery in the era of minimally invasive therapies. The following medical subject heading terms and keywords were used to identify relevant publications, and to evaluate the general trend in the percentage of publications comparing ESWL, PCNL and open surgery; ‘open stone surgery for urolithiasis’ or ‘urinary tract stones’, ‘ESWL’, ‘extracorporeal shockwave lithotripsy’, ‘PCNL’, ‘PNL’, ‘percutaneous nephrolithotomy’ or ‘nephrolithotripsy’. Articles in all languages were sought.
Results
From the MEDLINE search it was obvious that the number of papers published on open renal stone surgery has decreased during the last three decades, soon after the introduction of ESWL and PCNL (Fig. 1).
Figure 1.
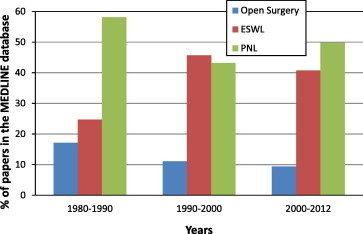
The percentage of papers on open surgery, PCNL and ESWL for treating urinary tract stones, recorded in the MEDLINE database from 1980 to 2012.
Discussion
The range of annual incidence of urolithiasis is 7–21 cases per 10,000 persons, with a reported peak age of onset at 20–30 years [8]. Until the early 1980s most cases of symptomatic urolithiasis were treated by open surgery.
The dramatic advances in endourological technology are considered to be the main reason for changing the indications for open surgery. That a surgeon can reach almost every part of the collecting system using small-calibre, semi-rigid and flexible ureteroscopes ensures that patients usually have a successful diagnostic or therapeutic procedure. As it is a minimally invasive procedure, many patients can usually be discharged on the same day as the procedure, and hence the techniques have gained popularity with surgeons and patients [9].
Advances in technology have also allowed for the development of more effective intracorporeal lithotripsy devices, such as the holmium laser and pneumatic lithotripters. Improvements in flexible grasping devices and the introduction of Nitinol baskets have further improved efficacy. Another factor has been the development of retrograde and antegrade techniques to correct anatomical obstructions associated with stone disease, including PUJ obstruction, calyceal diverticulum, infundibular stenosis, and ureteric stricture [10,11]. All of these factors, in addition to the improvement in the technical expertise of endourological surgeons, have contributed to a significant decline in the current indications for open stone surgery.
However, there are still patients who are candidates for this approach; the appropriate selection of these patients is critical in obtaining optimal surgical results. The most common current indications for open stone surgery include: patients in whom a reasonable number of less-invasive procedures would not be useful; those with a complex stone burden; failure of ESWL or endourological treatment; anatomical abnormalities (e.g. PUJ obstruction and infundibular stenosis with or without renal calyceal diverticulum), morbid obesity, concurrent open surgery, renal transplantation, severe limb contractures and patient preference. Therefore, it remains the critical responsibility of the treating urologist to recognise those rare cases in which open stone surgery might represent at least a reasonable alternative to less-invasive methods, if not even the primary treatment option.
Current guidelines on the role of open surgery
Over the last few years guidelines on ureteric and renal stone management have been published by the EAU and the AUA. Within the EAU guidelines, there is a consensus that most complex stones, including partial and complete staghorn stones, should be approached primarily with PCNL or a combination of PCNL and ESWL. However, if a reasonable number of percutaneous approaches are not likely to be successful, or if several endourological approaches have been attempted unsuccessfully, open surgery might be a valid primary treatment option [12].
The indications according to the most recent EAU guidelines (2011) are [12]:
-
•
Complex stone burden.
-
•
Treatment failure of ESWL and/or PCNL, or failed ureteroscopic procedure.
-
•
Intrarenal anatomical abnormalities: infundibular stenosis, stone in the calyceal diverticulum (particularly in an anterior calyx), PUJ obstruction, stricture.
-
•
Morbid obesity.
-
•
Skeletal deformity, contractures and fixed deformities of hips and legs.
-
•
Comorbid medical disease.
-
•
Concomitant open surgery.
-
•
Non-functioning lower pole (partial nephrectomy), non-functioning kidney (nephrectomy).
-
•
Patient’s choice following failed minimally invasive procedures; the patient might prefer a single procedure and avoid the risk of needing more than one PCNL procedure.
-
•
Stone in an ectopic kidney where percutaneous access and ESWL might be difficult or impossible.
For children, the same considerations apply as for adults.
The EAU guidelines also suggest that because many hospitals now have only limited experience with open stone surgery it might be advisable to send patients to a centre experienced in the use of special open surgical techniques, which are rarely used, such as extended pyelolithotomy, pyelonephrolithotomy, anatrophic nephrolithotomy, multiple radial nephrotomy, partial nephrectomy and renal surgery under hypothermia [13].
Recently, intraoperative B-mode scanning and Doppler ultrasonography [14,15] have been used to identify avascular areas in the renal parenchyma that are close to the stone or dilated calyces. This allows for the removal of large staghorn stones by several small radial nephrotomies, with no loss of kidney function.
The guidelines also conclude that the efficacy of open surgery over less invasive therapy, in terms of stone-free rates, is based on historical data, but no comparative studies are available [16–19].
The AUA recommendations suggest that open ureteric surgery should not be offered as a first-line treatment option in most patients (Table 1) [20]. Ureterolithotomy was recommended only in cases of large-volume ureteric calculi or complex patient anatomy. Postoperative morbidity and hospitalisation were significantly less with ESWL and endourological procedures than with other open surgical techniques [21,22].
Table 1.
AUA recommendations on open surgery for ureteric calculi (based on 1997 AUA recommendations on ureteric calculi) [20].
| Characteristics | Recommendation | Level of flexibilitya |
|---|---|---|
| Ureteric stones | ||
| Stone ⩽ 1 cm in proximal ureter | Open surgery should not be the first-line active treatment | Standard |
| Stone > 1 cm in proximal ureter | Open surgery should not be the first-line treatment for most patients | Guideline |
| Stone ⩽ 1 cm in distal ureter | Open surgery should not be the first-line active treatment | Standard |
| Stone > 1 cm in distal ureter | Open surgery should not be the first-line treatment for most patients | Guideline |
| Staghorn stones | The patient must be informed about the relative benefits and risks | Standard |
| Associated with the active-treatments | ||
| Open surgery (nephrolithotomy by any method) | Recommendation | |
| Should not be used for most patients | ||
| Open surgery can be considered for patients in whom the stone is | Option | |
| Not expected to be removed by a reasonable number of | ||
| Less invasive procedures | ||
Grades of flexibility are defined as: Standard, if (1) the health outcomes of the alternative interventions are sufficiently well known to permit meaningful decisions, and (2) there is virtual unanimity about which intervention is preferred: Recommendation, if (1) the health outcomes of the alternative interventions are sufficiently well known to permit meaningful decisions, and (2) an appreciable but not unanimous majority agrees on which intervention is preferred; Option, if (1) the health outcomes of the alternative interventions are not sufficiently well known to permit meaningful decisions, or (2) preferences are unknown or equivocal.
More recently, the AUA panel of experts on the management of staghorn calculi recommended that nephrolithotomy, by any method, should not be used for most patients with these kinds of stones [13,23] (Table 1). The panel also suggested that open surgery can be considered for patients in whom the stone was not expected to be removed by a reasonable number of less-invasive procedures. Such cases include patients with extremely large staghorn calculi, especially in those with unfavourable collecting system anatomy. Certain abnormalities of body habitus, such as extreme morbid obesity or skeletal abnormalities, can interfere with fluoroscopy and endoscopic therapies, requiring consideration of an open surgical approach. Anatrophic nephrolithotomy should be the preferred operation in such cases [13].
The role of open stone surgery in developing countries
Countries in the Afro-Asian stone belt (stretching from Egypt and Sudan, through the Middle East, India, Pakistan, Burma, Thailand, Indonesia and the Philippines) have consistently reported a high incidence of urolithiasis. Generally in this region there is a high population density, 30–50% of whom live below the poverty line, and the gross national product is low. Poor nutritional status and inadequate health facilities are other common problems in that region. More than half of the people live in rural areas and the climate is moderate to hot [24]. Against this background, urolithiasis constitutes 40–50% of the urological workload in hospitals [25]. A specific problem of this region is neglected asymptomatic large and/or staghorn calculi, and these patients present with renal failure [26,27].
The incidence of open stone surgery has been reported to be ≈1.5% of all stone removal interventions in developed countries, but in developing countries this has decreased from as high as 26% to 3.5% in recent years. In the USA in 2000, only 2% of the Medicare patients who underwent a surgical stone procedure were treated with open surgery [7]. A decade ago the rate of open stone surgery was reported as 26% in a tertiary referral centre in Pakistan, and 3–5% in the USA [28–30]. More recently, this rate decreased to 8% in Pakistan and 0.7–2% in centres of the so-called industrialised world [16,17,31]. Notably, these are data from tertiary referral centres in their respective countries, and there will be a difference between these centres and rural hospitals, in particular in the developing world, where in many places open surgery is still the primary procedure.
Recently, Rizvi et al. [32] retrospectively analysed the data of 3969 surgical procedures that were performed in 3053 children with stone disease in a tertiary referral centre in Pakistan. The rate of open surgery in their series was surprisingly as high as 30%; they attributed this to the fact that in developing countries, a large stone burden, neglected stones with renal failure, the paucity of urological facilities and residence of poor patients away from tertiary centres necessitate open surgical procedures as the therapy of choice in about a third of the patients. Therefore, they concluded that minimally invasive surgery is the way forward; however, the pattern of stone disease, patient volume and overall economy still mean that open surgery is the ‘therapy of choice’ in many situations. Thus the scope of open surgery will remain much wider for a large population of patients for a considerable time in developing countries.
Also, from a financial perspective, with special regard to developing countries, open surgery for staghorn stones remains an economically viable option for difficult stone cases, with comparable efficacy, favourable morbidity and hospital stay when compared to combined treatments (PCNL and ESWL) [33].
The role of laparoscopic surgery in the treatment of urolithiasis
Laparoscopic surgery has recently emerged as a reliable alternative to open stone surgery, because calculi can be removed from almost all locations in the kidney and ureter using a transperitoneal or retroperitoneal access. Functional outcomes and complication rates are comparable. The benefits of laparoscopy are less postoperative pain, shorter hospital stay, faster convalescence, and better cosmetic results [34].
It can be considered a reasonable treatment option [35] as a salvage procedure for failed ESWL and ureteroscopy, in selected patients with large chronically impacted ureteric stones, and particularly those with solitary kidneys. Successful laparoscopic anatrophic nephrolithotomy has been performed in a porcine model, and in humans [36,37]. Moreover, laparoscopic surgery is effective for complex renal stones and allows adjunctive procedures, such as dismembered or non-dismembered pyeloplasty, ablation of calyceal diverticula, partial nephrectomy, heminephrectomy and nephrectomy. It can also be an alternative to PCNL in the absence of availability (developing countries) or PCNL failure, and as an adjunct to PCNL, especially when access proves difficult (ectopic kidneys) [12].
Skolarikos et al. [38] recently tried to identify the level of the evidence and grade of recommendation, according to the evidence-based medicine criteria, in studies supporting the laparoscopic approach to stone extraction. The highest level of evidence (2a) was found for laparoscopic ureterolithotomy.
Conclusion
Although open surgery for treating urinary tract stones is rarely required at present, where most stone cases can be managed by minimally invasive therapy, we believe that it still has a role, and therefore it is of great importance to recognise that a small group of patients with complex stone disease and those with anatomical and physiological anomalies, will benefit from this treatment option.
Conflict of interest
None to declare.
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Assimos D.G. Should one perform open surgery in 1994? Semin Urol. 1994;12:26–31. [PubMed] [Google Scholar]
- 2.Singal R.K., Denstedt J.D. Contemporary management of ureteral stones. Urol Clin North Am. 1997;24:59–70. doi: 10.1016/s0094-0143(05)70354-2. [DOI] [PubMed] [Google Scholar]
- 3.Chaussy C., Schmiedt E., Jochan D., Brendel W., Forssmann B., Walther V. First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. J Urol. 1982;127:417–420. doi: 10.1016/s0022-5347(17)53841-0. [DOI] [PubMed] [Google Scholar]
- 4.Assimos D.G., Boyce W.H., Harrison L.H., McCullough D.L., Kroovand R.L., Sweat K.R. The role of open stone surgery since extracorporeal shock wave lithotripsy. J Urol. 1989;142:263–267. doi: 10.1016/s0022-5347(17)38725-6. [DOI] [PubMed] [Google Scholar]
- 5.Honeck P., Wendt-Nordahl G., Krombach P., Bach T., Häcker A., Alken P. Does open stone surgery still play a role in the treatment of urolithiasis? Data of a primary urolithiasis centre. J Endourol. 2009;23:1209–1212. doi: 10.1089/end.2009.0027. [DOI] [PubMed] [Google Scholar]
- 6.Bichler K.H., Lahme S., Strohmaier W.L. Indications for open stone removal of urinary calculi. Urol Int. 1997;59:102–108. doi: 10.1159/000283037. [DOI] [PubMed] [Google Scholar]
- 7.Paik M.L., Resnick M.I. Is there a role for open stone surgery? Urol Clin North Am. 2000;27:323–331. doi: 10.1016/s0094-0143(05)70261-5. [DOI] [PubMed] [Google Scholar]
- 8.Conference Consensus. Prevention and treatment of kidney stones. JAMA. 1988;260:977–981. [PubMed] [Google Scholar]
- 9.El-Husseiny T., Masood J., Karamanolakis D., Birch M., Buchholz N. The new Invisio® DUR-D ‘chip-on-the-tip’ digital flexible ureterorenoscopes – evaluation of changes in physical properties over time. Therapy. 2010;7:423–427. [Google Scholar]
- 10.Inglis J.A., Tolley D.A. Ureteroscopic pyelolysis for pelvi-ureteric obstruction. Br J Urol. 1986;58:250–252. doi: 10.1111/j.1464-410x.1986.tb09048.x. [DOI] [PubMed] [Google Scholar]
- 11.Nakada S.Y., Pearle M.S., Clayman R.V. Acucise endopyelotomy. Evolution of a less-invasive technology. J Endourol. 1996;10:133–139. doi: 10.1089/end.1996.10.133. [DOI] [PubMed] [Google Scholar]
- 12.Türk CT, Knoll A, Petrik K, Sarica M, Straub C, Seitz A. European Association of Urology Guidelines on Urolithiasis. Available at http://www.uroweb.org/fileadmin/user_upload/guidelines/urolithiasis.pdf.
- 13.Preminger G.M., Assimos D.G., Lingeman J.E., Nakada S.Y., Pearle M.S., Wolf J.S., Jr. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 14.Thüroff J.W., Frohneberg D., Riedmiller R., Alken P., Hutschenreiter G., Thüroff S. Localization of segmental arteries in renal surgery by Doppler sonography. J Urol. 1982;127:863–866. doi: 10.1016/s0022-5347(17)54110-5. [DOI] [PubMed] [Google Scholar]
- 15.Alken P., Thüroff J.W., Riedmiller H., Hohenfellner R. Doppler sonography and B-mode ultrasound scanning in renal stone surgery. Urology. 1984;23:455–460. doi: 10.1016/s0090-4295(84)80008-4. [DOI] [PubMed] [Google Scholar]
- 16.Kane C.J., Bolton D.M., Stoller M.L. Current indications for open stone surgery in an endourology centre. Urology. 1995;45:218–221. doi: 10.1016/0090-4295(95)80008-5. [DOI] [PubMed] [Google Scholar]
- 17.Sy F.Y., Wong M.Y., Foo K.T. Current indications for open stone surgery in Singapore. Ann Acad Med Singapore. 1999;28:241–244. [PubMed] [Google Scholar]
- 18.Goel A., Hemal A.K. Upper and mid-ureteric stone: a prospective unrandomized comparison of retroperitoneoscopic and open ureterolithotomy. BJU Int. 2001;88:679–682. doi: 10.1046/j.1464-4096.2001.00150.x. [DOI] [PubMed] [Google Scholar]
- 19.Skrepetis K., Doumas K., Siafakas I., Lykourinas M. Laparoscopic versus open ureterolithotomy. A comparative study. Eur Urol. 2001;40:32–36. doi: 10.1159/000049746. [DOI] [PubMed] [Google Scholar]
- 20.Alivizatos G., Skolarikos A. Is there still a role for open surgery in the management of renal stones? Cur Opin Urol. 2006;16:106–111. doi: 10.1097/01.mou.0000193379.08857.e7. [DOI] [PubMed] [Google Scholar]
- 21.Segura J.W., Preminger G.M., Assimos D.G., Dretler S.P., Kahn R.I., Lingeman J.E. Ureteral Stones Clinical Guidelines Panel summary report on the management of ureteral calculi. The American Urological Association. J Urol. 1997;158:1915–1921. doi: 10.1016/s0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 22.The American Urological Association Ureteral Stones Clinical Guidelines Panel. Report on the management of ureteral stones. Available at http://www.auanet.org/timssnet/products/guidelines/main_reports/UreStnMain8_16pdf. [DOI] [PubMed]
- 23.Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS, et al. The American Urological Association Staghorn Stones Clinical Guidelines Panel. Report on the management of staghorn calculi. Available at http://www.auanet.org/content/clinical-practice-guidelines/clinical-guidelines.cfm?sub=sc.
- 24.UNDP. Profile of Human Poverty in Human Development. Report 1997. Oxford University Press, 1997: 137–228.
- 25.Hussain M., Lal M., Ali B., Naqvi S.A., Rizvi S.A. Urolithiasis in Sindh. A single centre experience with review of 10,000 cases. J Nephrol Urol Transplant. 1998;1:10–13. [Google Scholar]
- 26.Gupta N.P., Kochar G.S., Wadhwa S.N., Singh S.M. Management of patients with renal and ureteric calculi presenting with chronic renal insufficiency. Br J Urol. 1985;57:130–132. doi: 10.1111/j.1464-410x.1985.tb06404.x. [DOI] [PubMed] [Google Scholar]
- 27.Hussain M., Lal M., Ali B., Ahmed S., Zafar N., Rizvi S.A. Management of urinary calculi associated with renal failure. J Pak Med Assoc. 1995;45:205–208. [PubMed] [Google Scholar]
- 28.Kerbl K., Rehman J., Landman J., Lee D., Sundaram C., Clayman R.V. Current management of urolithiasis: progress or regress? J Endourol. 2002;16:281–288. doi: 10.1089/089277902760102758. [DOI] [PubMed] [Google Scholar]
- 29.Matlaga B.R., Assimos D.G. Changing indications of open stone surgery. Urology. 2002;59:490–493. doi: 10.1016/s0090-4295(01)01670-3. [DOI] [PubMed] [Google Scholar]
- 30.Paik M.L., Resnick M.I. The role of open stone surgery in the management of urolithiasis. Tech Urol. 1997;3:96–99. [PubMed] [Google Scholar]
- 31.Paik M.L., Wainstein M.A., Spirnak J.P., Hampel N., Resnick M.I. Current indications for open stone surgery in the treatment of renal and ureteral calculi. J Urol. 1998;159:374–378. doi: 10.1016/s0022-5347(01)63922-3. [DOI] [PubMed] [Google Scholar]
- 32.Rizvi S.A., Sultan S., Ijaz H., Mirza Z.N., Ahmed B., Saulat S. Open surgical management of paediatric urolithiasis: a developing country perspective. Indian J Urol. 2010;26:573–576. doi: 10.4103/0970-1591.74464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goel M.C., Ahlawat R., Bhandari M. Management of staghorn calculus: analysis of combination therapy and open surgery. Urol Int. 1999;63:228–233. doi: 10.1159/000030456. [DOI] [PubMed] [Google Scholar]
- 34.Hruza M., Türk C., Frede T., Rassweiler J. Importance of open and laparoscopic stone surgery. Urologe A. 2008;47:578–586. doi: 10.1007/s00120-008-1734-1. [DOI] [PubMed] [Google Scholar]
- 35.Gaur D.D., Trivedi S., Prabhudesai M.R., Madhusudhana H.R., Gopichand M. Laparoscopic ureterolithotomy. Technical considerations and long-term follow-up. BJU Int. 2002;89:339–343. doi: 10.1046/j.1464-4096.2001.01562.x. [DOI] [PubMed] [Google Scholar]
- 36.Kaouk J.H., Gill I.S., Desai M.M., Banks K.L., Raja S.S., Skacel M. Laparoscopic anatrophic nephrolithotomy feasibility study in a chronic porcine model. J Urol. 2003;169:691–696. doi: 10.1097/01.ju.0000036471.82870.23. [DOI] [PubMed] [Google Scholar]
- 37.Deger S., Tuellmann M., Schoenberger B., Winkelmann B., Peters R., Loening S.A. Laparoscopic anatrophic nephrolithotomy. Scand J Urol Nephrol. 2004;38:263–265. doi: 10.1080/00365590410028719. [DOI] [PubMed] [Google Scholar]
- 38.Skolarikos A., Papatsoris A.G., Albanis S., Assimos D. Laparoscopic urinary stone surgery: an updated evidence-based review. Urol Res. 2010;38:337–344. doi: 10.1007/s00240-010-0275-4. [DOI] [PubMed] [Google Scholar]



