Abstract
Background
Bladder leiomyomas are benign mesenchymal neoplasms and very rare urinary tumours that represent <0.5% of all bladder tumours, with only 250 cases reported worldwide to date. The importance of recognising their characteristic features, leading to their correct treatment, is fundamental. Therefore, we reviewed reports of leiomyomas of the urinary bladder, their causes, clinical presentations, imaging methods and surgical management, updated to 2012.
Methods
We retrospectively reviewed articles published in the USA, Europe and Asia, from 1953 to date, using PubMed, Medscape, Medline and the several major journals. We report areas of controversies and well-established guidelines.
Results
We reviewed 36 articles that confirmed, with a high level of evidence-based medicine, that the male to female ratio is equal, the cause of bladder leiomyomas remains unknown, and their most common presentation is obstructive uropathy; endovesical tumours are the most common. Their radiological diagnosis can be made by ultrasonography, computed tomography or magnetic resonance imaging. Complete surgical resection is a very effective treatment, associated with almost no recurrence.
Conclusion
In symptomatic patients a complete surgical resection can give a very good outcome, with almost no recurrence.
Abbreviations: US, ultrasonography; TURBT, transurethral resection of the bladder tumour
Keywords: Bladder, Leiomyoma, Benign tumour, Diagnosis
Introduction
Mesenchymal tumours represent 1–5% of all urinary bladder tumours [1,2]. Among these leiomyomas account for 35% and are the most common benign mesenchymal tumours in the bladder [3], and therefore account for 0.43% of all bladder tumours [4]. Leiomyomas of the urinary bladder are very rare neoplasms, with only ≈250 cases previously reported [5].
In 1929, De Berne-Lagarde [6] exhaustively reviewed the literature and described 36 cases. After that, in 1953, Campbell and Gislason [1] found 68 cases, and in 1986, Knoll et al. [3] reviewed five cases of bladder leiomyomas reported at the Mayo Clinic.
Even with the increased availability of high-resolution ultrasonography (US), CT and MRI, bladder leiomyomas remain rare tumours. Previous data were found on gender distribution, age, presenting symptoms, optimal diagnostic tests, and treatment based on size and location, but dating from many years ago. The previous reports seem to have limitations and shortcomings for the selection criteria related to the surgical management of these tumours, with areas of controversy leading to different management when several factors were involved, e.g. the size, exact location, and the natural evolution of these benign tumours.
At the American University of Beirut-Rafik Hariri University Hospital we recently treated a patient with a bladder leiomyoma, and subsequently reviewed in detail previous reports, to describe the contemporary approach to this tumour [1,3,5,7–31].
Therefore, the objective of the present review was to detail leiomyomas of the urinary bladder, their incidence, epidemiology, aetiology, clinical presentation, optimal diagnostic methods, and pathology, and to finally clarify the best therapies, as updated to 2012.
Methods
Between 1937 and 2012, the information assessed included a thorough review of previous reports, including 36 articles published in the USA, Europe and Asia, on leiomyomas of the urinary bladder. We provide the most up-to-date information, in addition to well-established guidelines. The information covered was retrieved from the Annals of Internal Medicine, PubMed, Medscape, Clinical Imaging, Histopathology, Urologia Internationalis, Archives of Surgery, JACS, AUA and Journal of Urology Website, the BMJ, Scandinavian Journal of Urology and Nephrology, Medline, and Springer Link. We also included, for illustrative purposes, the US and CT findings of the patient recently treated in our medical centre for bladder leiomyoma.
Results
Incidence, epidemiology and aetiology
Bladder leiomyomas have been shown to have a similar incidence in men and women [3], although some authors have reported a female preponderance [13] related to a more frequent use of pelvic US in females [4].
In the series of 37 patients reviewed by Goluboff et al. [32], 26 were women (70%) and 11 were men; the mean (range) age was 44 (11–75) years.
The aetiology of these benign tumours is still unknown. It has been speculated that bladder leiomyomas might arise from either chromosomal alterations [4], hormonal disturbances, repeated bladder wall and detrusor infection, perivascular inflammation or dysontogenesis [32].
Clinical presentation
Patients with bladder leiomyomas can be asymptomatic, but the majority present with obstructive symptoms (49%), irritative symptoms (38%) and haematuria (11%) [32]. In the 37 patients reviewed by Goluboff et al. [32] 14 (38%) who had irritative voiding symptoms presented with burning sensation, dysuria and urgency; 18 (49%) who had obstructive voiding symptoms presented initially with acute urinary retention, a weak stream, a sensation of incomplete emptying, and urinary frequency. Four patients (11%) presented with gross haematuria, five had flank pain that was found (later) to be due to ureteric obstruction, and some patients had several symptoms together. Seven patients (19%) were asymptomatic, and that included two who were pregnant; the lesions in asymptomatic patients were incidentally diagnosed, during an evaluation for other complaints (Table 1).
Table 1.
The clinical presentations and chief complaints for bladder leiomyoma.
| Presentation and complaint | % of patients |
|---|---|
| Women | 70 |
| Men | 30 |
| Obstructive symptoms | 49 |
| Irritative symptoms | 38 |
| Gross haematuria | 11 |
| Flank pain | 13 |
| Asymptomatic | 19 |
| Pregnant | 5 |
Leiomyomas are classified into three different locations, i.e. endovesical, intramural and extravesical. Endovesical is the most common location and it corresponds to 63–86% of cases, while intramural leiomyomas are present in 3–7% and extravesical in 11–30% [3,32].
In the office setting cystoscopy can be used and might distinguish an intramural from an endovesical tumour. Endovesical tumours are a result of the submucosal growth of the leiomyoma, and was first described by Campbell and Gislason [1]; they are usually polypoid or pedunculated, while intramural bladder leiomyomas are well encapsulated lesions and surrounded by the bladder wall muscle.
The endovesical form will cause irritative or obstructive symptoms, and gross haematuria [33], resulting in a relatively early diagnosis [4]. Small intramural tumours are far less symptomatic.
Diagnostic options
After cystoscopy, which is considered to be the best initial diagnostic tool, as reported by Goluboff et al. [32], the radiological option is US, for which the findings are very characteristic, mainly for endovesical leiomyomas. They are homogenous smooth lesions with peripheral hyperechogenicity [5,8] (Fig. 1).
Figure 1.
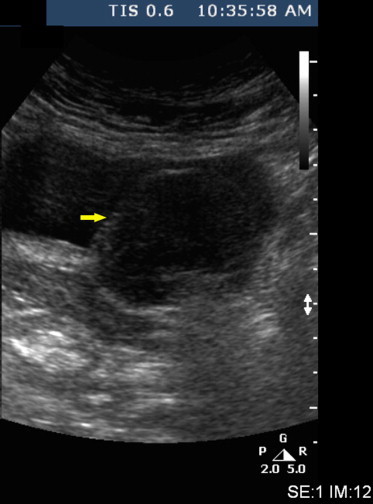
Bladder leiomyoma on pelvic US, showing a smooth endovesical bladder lesion with peripheral hyperechogenicity (yellow arrow).
However, CT can be used to assess the location of these tumours, and to differentiate between a fluid-filled and a solid lesion, in addition to identifying its relation to the surrounding structures (Figs. 2–4).
Figure 2.
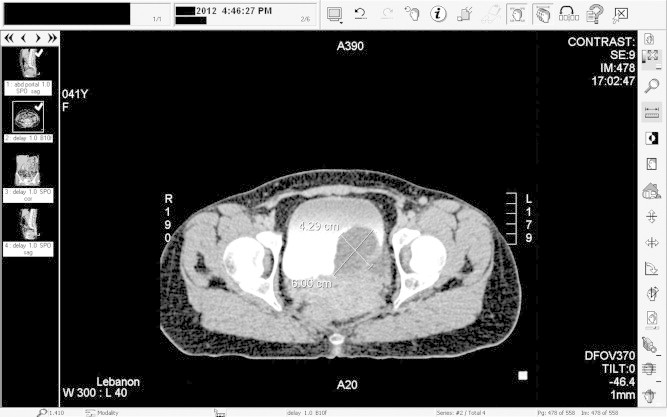
A bladder leiomyoma on CT of the abdomen and pelvis with intravenous contrast medium, showing a well-delineated endovesical bladder tumour, 6 cm × 4.2 cm, arising from the left posterolateral bladder wall.
Figure 3.

A bladder leiomyoma on CT of the abdomen and pelvis with intravenous contrast medium (coronal view), showing an endovesical bladder tumour, arising from the left lateral bladder wall.
Fig. 4.
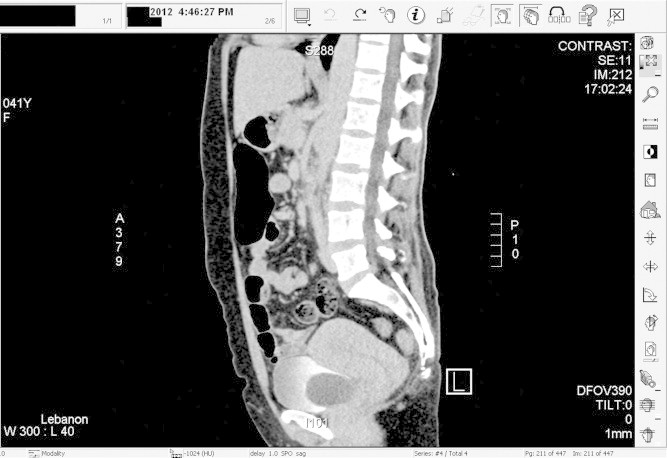
A bladder leiomyoma on CT of the abdomen and pelvis with intravenous contrast medium (sagittal view), showing an endovesical bladder tumour.
MRI can have a higher specificity for the mesenchymal component of these tumours, and will delineate their relation with the bladder wall and detrusor [9]. Leiomyomas on MRI have a low intensity both on T1- and T2-weighted sequences, with a smooth periphery, mimicking a uterine leiomyoma.
After injecting gadolinium contrast medium, many patterns of enhancement might occur; some leiomyomas will enhance homogeneously, while others will not [2,10,11]. If there is a coexisting area of cystic degeneration it will appear as a hyperintense signal on T2-weighted images, and will not enhance with contrast medium. In both cases, all imaging techniques can never exclude a malignancy, and therefore a tissue sample is always needed, for histological studies and for the appropriate therapeutic intervention.
In the series of 37 patients reported by Goluboff et al. [32] IVU was used in 30 (81%) and in all patients showed a smooth filling defect. Currently, IVU does not seem to be included in the options in that particular scenario, and is being progressively abandoned.
Histopathology
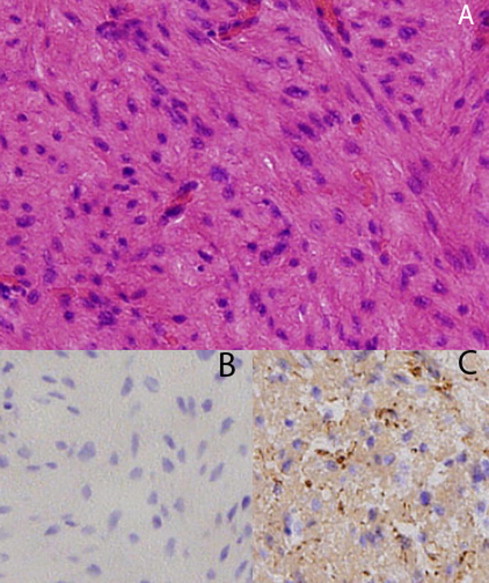
Histopathologically, leiomyoma of the urinary bladder is composed of fascicles of smooth muscle fibres that are separated by connective tissues. They are non-infiltrative smooth muscle benign tumours with no mitotic activity, cellular atypia or necrosis. On immunohistochemistry they will have positive staining for smooth-muscle actin and negative staining for Ki-67 (Fig. 5).
Figure 5.

Histopathological studies show that there is a proliferation of spindle-shaped cells, in addition to an eosinophilic cytoplasm and fibres (haematoxylin and eosin, x), with no evidence of mitotic changes or atypia (A). Leiomyomas of the urinary bladder also stain negatively for Ki-67 (B), but they are positive for smooth muscle staining (actin) (C).
Therapies
Intramural tumours can be managed according to their size and location. Small and easily accessible tumours can be treated with transurethral resection of the bladder tumour (TURBT), while unfavourable positioning and difficulty in recognition might require segmental resection or laparoscopic partial cystectomy [34] (Table 2).
Table 2.
Therapeutic options for bladder leiomyoma.
| Option | Treatment |
|---|---|
| TURBT | |
| Open surgery | Simple enucleation |
| Partial cystectomy | |
| (open, laparoscopic, robotic) | |
| Cystoprostatectomy | |
| (open, laparoscopic, robotic) | |
| Conservative | |
Treatment is determined primarily according to the size and anatomical location of the tumours [35,36]. In the review of Goluboff et al. [32], 62% of the patients were treated with open resection, while 38% were treated with TURBT, similar to the present patient. In all, 18% of patients in the TURBT group required a reoperation due to incomplete resection, while none required a second procedure in the open group. There were no recurrences, other than those that were most probably residual tumour after TURBT, nor any malignant degeneration, necrosis or haemorrhage of these lesions [32].
Case profile
We recently treated a 41-year-old woman who presented at our institution with a 7-week history of gross haematuria, dysuria, and repeated episodes of left flank pain. Her physical examination was normal. The laboratory tests showed mild anaemia and a normal serum creatinine level. US of the kidneys and pelvis (Fig. 1) showed a large bladder tumour, with left hydronephrosis, and a smooth endovesical bladder lesion with peripheral hyperechogenicity. The patient then had enhanced CT of the abdomen and pelvis that showed a well-delineated endovesical bladder tumour of 6 cm × 4.2 cm, arising from the left posterolateral bladder wall (Fig. 2), also visible on the coronal view (Fig. 3) and the sagittal view (Fig. 4).
The enhanced CT showed left hydronephrosis and a left ‘extra-renal’ pelvis in the context of an obstructed and dilated left pelvicalyceal system, due to the bladder tumour located on the left lateral wall, and most probably obscuring the left ureteric orifice (Fig. 6). She underwent an uneventful TURBT and the pathology was assessed as ‘bladder leiomyoma’ (Fig. 5).
Figure 6.
Enhanced CT of the abdomen and pelvis showing left hydronephrosis and a left ‘extra-renal’ pelvis, due to the bladder leiomyoma obstructing the left ureteric orifice.
Discussion
Leiomyomas of the urinary bladder, although rare, are the most common benign mesenchymal tumours of the bladder [3,5]. It was initially thought that bladder leiomyomas occur equally in men and women and are evenly distributed across age groups [1,7–9]. However, recent series reported a female preponderance (70%) [32], and this pathology affects those in their third to sixth decades. The most common symptoms at presentation are obstructive (49%), followed by irritative (38%) and haematuria (11%) [5,9,32].
Cystoscopy can show a characteristic bladder mass with a smooth and regular mucosa. In some reports the tumour was very large, sometimes up to 25 cm [10], and the cystoscope could not be passed into the bladder. In another case report the tumour could be seen and was excised transvaginally [11].
Although, IVU was often used in the past it is currently being replaced by CT and MRI. IVU might show a hydronephrotic kidney if the bladder leiomyoma is obscuring the ureteric orifice, in addition to a smooth filling defect in the bladder. US should be used initially and will typically detect a smooth-walled solid lesion with numerous internal echoes and homogenous texture of medium echogenicity. Therefore, US has been reported as the most sensitive and affordable of the diagnostic tests.
Fernandez et al. [11] compared several diagnostic methods, including IVU, a voiding cysto-urethrogram, transabdominal US, CT and transvaginal US for the diagnosis of a leiomyoma of the bladder floor; transvaginal US provided the most accurate information about the location of the mass and its relationship to adjacent organs. Illescas et al. [14] found US to be better than CT, based on the fact that US was better for assessing this solid tumour, its submucosal location, and its relationship to adjacent organs, because US can analyse multiple planes.
However, US currently seems to have been replaced by three-dimensional CT and MRI for a better assessment of the delineation planes and the sites of origin. CT generally shows a smooth-walled bladder filling defect with an attenuation coefficient of 25–50 Hounsfield units. MRI shows an intermediate signal intensity on T1-weighted images, giving good contrast compared with the low-intensity signal of urine. On T2-weighted images it gives areas of high and low intensity at the same time, giving excellent contrast, as opposed to the intermediate-low intensity of the bladder muscle, facilitating the diagnosis of an extravesical extension [15,16].
In the case report of Bramwell et al. [17], giant bladder tumours were detected, with a high suspicion of malignancy, and therefore an angiogram was taken, and the authors used preoperative embolisation of the internal iliac arteries during the angiography. Some authors previously described angiography as the only test that enabled them to make a specific diagnosis [10]. The vessels, in those cases, came from the internal iliac arteries, had no signs of malignancy, such as parasitic blood supply, arterial invasion, necrosis or haemorrhage, and showed a smoothly outlined, highly vascular lesion with dense capillaries and some corkscrew vessels, which led them to the diagnosis of leiomyoma. Currently, angiography is no longer the standard of care for the diagnosis of bladder leiomyomas.
In the series of Kabalin et al. [13] and Chavez and Neto [19], among the 35 patients who had the bladder leiomyoma excised, only two had residual tumour and needed a re-excision. This low re-intervention rate means that regardless of the excisional method, bladder leiomyoma is adequately and easily treated, with almost no recurrence when fully resected. The exact location, size, extent and potential involvement of the ureters or sphincter will determine which of these therapies is the most appropriate. As a general rule, small endovesical bladder leiomyomas can be treated by TURBT, but larger intramural or extravesical ones are treated by open resection. It is mandatory to make sure that the ureteric orifice will not be obstructed by any residual tumour that initially caused potential hydronephrosis. Some surgeons would advocate taking a retrograde pyelogram and inserting a ureteric stent to avoid the postoperative local oedema causing a persistent pelvicalyceal dilatation.
Leiomyomas of the urinary bladder share common histopathological features with leiomyomas of the uterus, i.e. round nodules, grey-white, with a spiral appearance of smooth muscle fibres gathered in small fascicles and separated by varying amounts of fibrous connective tissue, and fewer than two mitotic figures per high-power field [3].
The endovesical subtype is more common because it bulges into the bladder, resulting in more symptoms and causing the patient to seek medical attention. As the endovesical site is the most common location, corresponding to 63–86% of the cases, TURBT represents the main treatment in almost 90% of cases, unless a large intramural leiomyoma is encountered (3–7%) or an extravesical one (11–30%) [3,32], requiring a wider excision, like a partial cystectomy.
The pathophysiology of these lesions remains unknown but four theories have been proposed: (1) Hormonal disturbances cause these tumours to develop; (2) Dysontogenesis, e.g. embryonic rests of tissue residing in the bladder that transform into leiomyomas; (3) Perivascular inflammation leading to metaplastic transformation of the bladder vascular supply; and (4) Bladder musculature infection leading to inflammation and the development of these benign tumours [20]. More studies and research are needed to elucidate the mechanism of their growth.
Conclusion
Leiomyoma of the bladder is an uncommon neoplasm and despite that, a thorough history and careful physical examination should be made when patients present with a prolonged history of urinary tract symptoms. Women seem to be more affected, and obstructive symptoms predominate. There should be more innovations in research to clarify the reason behind the female preponderance, and to identify any possible genetic or chromosomal defect that might be treated earlier before a future clinical presentation.
Urologists should include a complete assessment, including US, CT or MRI, that will determine the location and local extension, whether endovesical, intramural or extravesical. As the endovesical is the most common location, TURBT is the mainstay of therapy for small endovesical bladder leiomyoma. If the tumour is large and intramural or extravesical, a segmental resection and partial cystectomy should be considered. A better understanding of this disease in the future might perhaps offer the patient a new intravesical agent that will target these cells specifically.
Although urinary cytology studies are being used as options for assessing transitional cell carcinoma of the urinary tract, they might be developed as new methods that could be applied to bladder leiomyoma (although benign), for screening, follow-up and perhaps to avoid the sometimes unnecessary aggressive measures.
Surgical treatment, when the excision is wide enough, is almost always very effective, leaving a very low recurrence rate, and with no symptoms, confirming the benign nature of bladder leiomyomas and their excellent prognosis.
Conflict of interest
None.
Source of funding
None.
Footnotes
Peer review under responsibility of Arab Association of Urology
References
- 1.Campbell E.W., Gislason G.J. Benign mesothelial tumors of the urinary bladder: review of literature and a report of a ease of leiomyoma. J. Urol. 1953;70:733–742. doi: 10.1016/S0022-5347(17)67977-1. [DOI] [PubMed] [Google Scholar]
- 2.Melicow M.M. Tumors of the urinary bladder. J. Urol. 1937;37:117. doi: 10.1016/S0022-5347(17)67309-9. [DOI] [PubMed] [Google Scholar]
- 3.Knoll L.D., Segura J.W., Scheilhauer B.W. Leiomyoma of the bladder. J. Urol. 1986;136:906–913. doi: 10.1016/s0022-5347(17)45124-x. [DOI] [PubMed] [Google Scholar]
- 4.Cornella J.L., Larson T.R., Lee R.A., Magrina J.F., Kammerer-Doak D. Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am. J. Obstet. Gynecol. 1997;176:1278–1285. doi: 10.1016/s0002-9378(97)70346-6. [DOI] [PubMed] [Google Scholar]
- 5.Saunders S.E., Conjeski J.M., Zaslau S., Williams J. Leiomyoma of the urinary bladder presenting as urinary retention in the female. Can. J. Urol. 2009;16:4762–4764. [PubMed] [Google Scholar]
- 6.De Berne-Lagarde A. Les leiomyomes vesicaux. Arch. D Mal des Reins Des Organes Genitourin. 1929;4:412–441. [Google Scholar]
- 7.Mutchler R.W., Gorder J.L. Leiomyoma of the bladder in a child. Br. J. Radiol. 1972;45:538–540. doi: 10.1259/0007-1285-45-535-538. [DOI] [PubMed] [Google Scholar]
- 8.Katz R.B., Waldbaum R.S. Benign mesothelial tumors of the bladder. Urology. 1975;5:236–238. doi: 10.1016/0090-4295(75)90018-7. [DOI] [PubMed] [Google Scholar]
- 9.Kutzmann A.A. Leiomyoma of urinary bladder. J. Urol. 1937;37:117–132. [Google Scholar]
- 10.Wenz W., Sommerkamp H., Dinkel E. Leiomyoma of the bladder. Urol. Radiol. 1986;8:114–117. doi: 10.1007/BF02924092. [DOI] [PubMed] [Google Scholar]
- 11.Fernandez A., Dehesa T.M. Leiomyoma of the urinary bladder floor: diagnosis by transvaginal ultrasound. Urol. Int. 1992;48:99. doi: 10.1159/000282305. [DOI] [PubMed] [Google Scholar]
- 12.Albert N.E. Leiomyoma of bladder. Preoperative diagnosis by ultrasound. Urology. 1981;17:486–487. doi: 10.1016/0090-4295(81)90201-6. [DOI] [PubMed] [Google Scholar]
- 13.Kabalin J.N., Freiha F.S., Niebel J.D. Leiomyoma of bladder: report of 2 cases and demonstration of ultrasonic appearance. Urology. 1990;35:210–212. doi: 10.1016/0090-4295(90)80032-i. [DOI] [PubMed] [Google Scholar]
- 14.Illescas F.F., Baker M.E., Weinerth J.L. Bladder leiomyoma. Advantages of sonography over computed tomography. Urol. Radiol. 1986;8:216–218. doi: 10.1007/BF02924110. [DOI] [PubMed] [Google Scholar]
- 15.Maya M.M., Slywotzky C. Urinary bladder leiomyoma magnetic resonance imaging findings. Urol. Radiol. 1992;14:197–199. doi: 10.1007/BF02926929. [DOI] [PubMed] [Google Scholar]
- 16.Tomoe H., Okumura T., Nakamura M., Toma H., Ishikawa H., Kohno A. Evaluation MR imaging of leiomyoma of the bladder. Urol. Int. 1991;46:349–351. doi: 10.1159/000282165. [DOI] [PubMed] [Google Scholar]
- 17.Bramwell S.P., Pitts J., Gondie S.E., Abel B.J. Giant leiomyoma of the bladder. Br. J. Urol. 1987;60:178. doi: 10.1111/j.1464-410x.1987.tb04959.x. [DOI] [PubMed] [Google Scholar]
- 18.Belis J.A., Post G.J., Rochman S.C., Milam D.F. Genitourinary leiomyomas. Urology. 1979;13:424–429. doi: 10.1016/0090-4295(79)90350-9. [DOI] [PubMed] [Google Scholar]
- 19.Chavez C.A., Neto M. Multiple leiomyomata of the urinary bladder. J. Kans. Med. Soc. 1984;85:298–299. [PubMed] [Google Scholar]
- 20.Teran A.Z., Gambrell R.D. Leiomyoma of the bladder. Int. J. Fertil. 1989;34:289–292. [PubMed] [Google Scholar]
- 21.Hernandez D.J., Chan D.Y. Bladder leiomyomata and pelvic pain. Urology. 2007;70:807–808. doi: 10.1016/j.urology.2007.07.047. [DOI] [PubMed] [Google Scholar]
- 22.O’Connell K., Edson M. Leiomyoma of bladder. Urology. 1975;6:114–115. doi: 10.1016/0090-4295(75)90608-1. [DOI] [PubMed] [Google Scholar]
- 23.Vargas A.D., Mendez R. Leiomyoma of bladder. Urology. 1983;21:308–309. doi: 10.1016/0090-4295(83)90095-x. [DOI] [PubMed] [Google Scholar]
- 24.Delahunt B., Nacey J.N., Ferguson A.F. Giant sclerosing leiomyoma of the bladder presenting as chronic renal failure. Urology. 1991;37:270–272. doi: 10.1016/0090-4295(91)80304-p. [DOI] [PubMed] [Google Scholar]
- 25.Bazeed M.A., Aboulenien H. Leiomyoma of the bladder causing urethral and unilateral Urethral obstruction: a ease report. J. Urol. 1988;140:143–144. doi: 10.1016/s0022-5347(17)41510-2. [DOI] [PubMed] [Google Scholar]
- 26.Van Regemorter G., Germeau F. Leiomyoma of the bladder. Eur. Urol. 1984;10:210–211. doi: 10.1159/000463790. [DOI] [PubMed] [Google Scholar]
- 27.Jacobs M.A., Bavendam T., Leach G.E. Bladder leiomyoma. Urology. 1989;24:56–57. doi: 10.1016/0090-4295(89)90160-x. [DOI] [PubMed] [Google Scholar]
- 28.Lake M.H., Kossow A.S., Bokinsky G. Leiomyoma of the bladder and urethra. J. Urol. 1981;125:742–743. doi: 10.1016/s0022-5347(17)55189-7. [DOI] [PubMed] [Google Scholar]
- 29.Koskivuo I.O., Ala-Opas M.Y. Leiomyoma of the bladder. Scand. J. Urol. Nephrol. 1992;26:193. doi: 10.1080/00365599.1992.11690454. [DOI] [PubMed] [Google Scholar]
- 30.Thompson I.M., Balfour J. Leiomyomatous vesical outlet obstruction. Urology. 1974;3:92–93. doi: 10.1016/s0090-4295(74)80073-7. [DOI] [PubMed] [Google Scholar]
- 31.McLucas B., Stein J.J. Bladder leiomyoma. a rare cause of pelvic pain. Am. J. Obstet. Gynecol. 1985;153:896. doi: 10.1016/0002-9378(85)90701-x. [DOI] [PubMed] [Google Scholar]
- 32.Goluboff E.T., O’Toole K., Sawczuk I.S. Leiomyoma of bladder: report of case and review of literature. Urology. 1994;43:238–241. doi: 10.1016/0090-4295(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 33.Chen M., Lipson S.A., Hricak H. MR imaging evaluation of benign mesenchymal tumors of the urinary bladder. AJR Am. J. Roentgenol. 1997;168:399–403. doi: 10.2214/ajr.168.2.9016215. [DOI] [PubMed] [Google Scholar]
- 34.Lyons T.L., Lee T., Winer W.K. Laparoscopic removal of a bladder leiomyoma. J. Am. Assoc. Gynecol. Laparosc. 1998;5:423–426. doi: 10.1016/s1074-3804(98)80059-5. [DOI] [PubMed] [Google Scholar]
- 35.Soloway D., Simon M.A., Milikowski C., Soloway M.S. Epithelioid leiomyoma of the bladder: an unusual cause of voiding symptoms. Urology. 1998;51:1037–1039. doi: 10.1016/s0090-4295(98)00016-8. [DOI] [PubMed] [Google Scholar]
- 36.Silva-Ramos M., Masso P., Versos R., Soares J. Leiomyoma of the bladder. Analysis of a collection of 90 cases. Actas Urol. Esp. 2003;26:581–586. doi: 10.1016/s0210-4806(03)72979-9. [DOI] [PubMed] [Google Scholar]



