Abstract
Objective
To evaluate whether tamsulosin hydrochloride is effective as an adjunctive medical therapy to increase the effectiveness of extracorporeal shock-wave lithotripsy (ESWL) for treating ureteric stones, and minimises the use of analgesic drugs after the procedure.
Patients and methods
To treat single ureteric stones of 5–15 mm in diameter, 130 patients were treated with ESWL. After treatment, equal numbers of patients were randomly assigned to receive either the standard medical therapy alone (controls) or combined with 0.4 mg tamsulosin daily for ⩽12 weeks. All patients were followed up for 3 months or until an alternative treatment was offered.
Results
At 3 months the treatment was considered to be clinically successful in 55/65 (85%) of those receiving tamsulosin and in 58/65 (89%) of the controls (P = 0.34). When patients were classified according to stone size the success rate was similar in both groups (P = 0.22) for those with a stone of >10 mm. However, ureteric colic was reported in 12% of patients treated with standard therapy but in only 5% of those treated with tamsulosin (P = 0.006). The mean cumulative diclofenac dose was 380 mg/patient in the tamsulosin group and 750 mg/patient in the control group (P = 0.004).
Conclusions
This study showed the effectiveness of tamsulosin as an adjunctive medical therapy after ESWL for ureteric stones, but it did not improve stone clearance when treating ureteric stones. However, it decreased the use of analgesics and reduced the complication rate, especially for steinstrasse.
Abbreviation: US, ultrasonography
Keywords: Stone, Ureter, ESWL, Tamsulosin
Introduction
ESWL is currently considered one of the best treatments for ureteric stones, with a reported success rate of 80–90% [1,2]. The complications of ESWL include colic, delayed passage of stone fragments, or an obstructed ureter due to steinstrasse (a column of stone fragments). The benefit of pharmacotherapy in promoting the spontaneous passage of ureteric calculi has been reported in several randomised clinical trials [3–7].
The exact mechanism of action of tamsulosin in expulsive therapy is unknown. In the ureter, tamsulosin is presumed to inhibit the uncontrolled contraction of ureteric smooth muscle, thereby facilitating the spontaneous passage of stones [5]. Several studies investigated the efficacy of tamsulosin with ESWL in clearing renal and lower ureteric stones [3–10]. However, few studies have reported its efficacy for upper ureteric stones [10,11].
The objective of the present study was to compare the effect of tamsulosin hydrochloride and standard medical therapy on the rate of stone passage and clearance of stone fragments, the severity of ureteric colic after ESWL, and the frequency of the use of analgesics.
Patients and methods
Between July 2010 and May 2012 this prospective randomised, controlled study included 130 consecutive patients with a solitary ureteric stone of 5–15 mm diameter, and who were attending the outpatient urology clinic of the author’s institution. The study protocol was approved by the hospital ethics committee, and informed consent was obtained from all patients. All patients were evaluated by a detailed history, clinical examination and routine laboratory investigations, including urine analysis, urine culture, serum creatinine measurement, liver function tests, a complete blood analysis, coagulation profile and random blood sugar estimates. The radiological assessment comprised a plain abdominal film. Pelvi-abdominal ultrasonography (US) and/or excretory urography were used to evaluate the stone site, size and radio-density, and to detect the degree of dilatation of the pelvicalyceal system in 117 patients (90%). Non-contrast enhanced spiral CT of the abdomen and pelvis was used in 13 patients (10%) with radiolucent stones. The exclusion criteria in the study included: patients aged <15 years, pregnancy, uncontrolled UTI, multiple ureteric stones, the presence of ureteric stricture distal to the stone, previous unsuccessful ESWL, concomitant use of calcium-channel blockers or α-adrenergic antagonists, patients with an uncorrected coagulation profile, severe vertebral malformation, morbid obesity, severe cardiopulmonary disorders, elevated serum creatinine (>2 mg/dL), high-grade hydronephrosis, diabetes mellitus, BOO, neuropathic bladder, and gastric ulcer disease (to avoid exacerbation of ulcer disease by analgesics). A prophylactic antibiotic was given to all patients 24 h before ESWL.
ESWL was administered using an electromagnetic lithotripter (Dornier SII, Germany) under fluoroscopic guidance for radio-opaque stones and US guidance for 13 radiolucent stones (the Dornier SII has an integral location system using a real-time 3.5 mHz monitoring transducer, which is satisfactory for imaging radiolucent ureteric stones). Among the patients with radiolucent stones, eight stones were in the upper ureter and five were in the juxtavesical ureter. Stones in the proximal part of the upper ureter were identified by US, as the kidney provided a good acoustic window. The flexibility of the US probe arm helped to provide the optimal stone image. Initially a complete and clear longitudinal scan of the kidney was obtained. The target cross was positioned at the dilated pelvi-ureteric junction and the dilated ureter was followed until the stone appeared as a hyperechoic mass with a black posterior acoustic shadow. Also, stones in the lower part of the ureter were visualised using US. A full bladder was required to act as an acoustic window for visualisation of the lower ureter. The target cross was positioned on the posterior bladder wall and then moved laterally to visualise the stone.
ESWL sessions were applied at a mean (range) of 13.5 (12–15) kV and a shock rate of 80–100/min. The ESWL session was considered complete if there was satisfactory fragmentation or a maximum of 3000–4000 shocks. The energy dose for upper ureteric stones was 130–160 J, with a maximum of three sessions as the protocol followed at the ESWL unit.
The 130 patients were randomised into two equal groups using a computer program (www.randomization.com). Group 1 (control) included patients treated by standard medical therapy after ESWL which included oral fluids, furosemide 20 mg every morning and diclofenac sodium tablets (50 mg three times/day or a 75 mg ampoule) on demand after ESWL. In group 2 65 patients received tamsulosin 0.4 mg once daily for 3 weeks after the first session of ESWL, in addition to oral fluids, furosemide 20 mg every morning and diclofenac sodium as necessary for the relief of pain.
Patients in both groups were instructed to record the number of analgesic tablets and ampoules taken during the course of treatment, and advised to attend the hospital if they had severe ureteric colic, fever, oliguria or any side-effects from the drugs.
Stone clearance was assessed at 30 and 908 days after ESWL by a plain abdominal film and US. Being stone-free was defined as complete stone clearance, and failed ESWL was defined as failed fragmentation after three sessions, the presence of clinically significant residual stone fragments, and the requirement for an auxiliary procedure after any session (ureteroscopy, and percutaneous nephrostomy, for residual calculi or steinstrasse). The course of the patients through the various stages (enrolment, follow-up and analysis) is shown in the Fig. 1.
Figure 1.
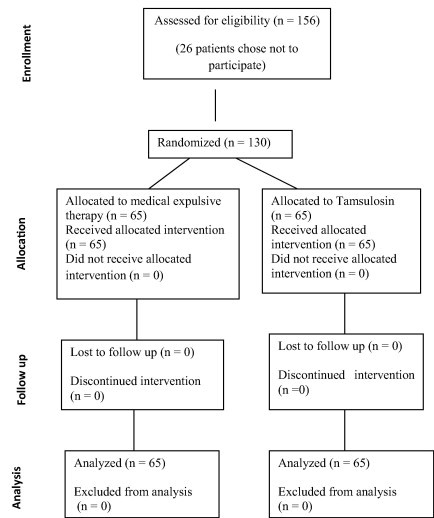
A diagram of the distribution of patients throughout the study.
The results of both groups were compared, assessing the expulsion rate, stone clearance, analgesic requirement, and the occurrence of steinstrasse after ESWL. Among those in group 2 the treatment efficacy was analysed using the intention-to-treat population, defined as all enrolled patients who received at least one dose of any study medication. Significance was assessed by Student’s t-test, a z-test and chi-squared test, as appropriate, with P < 0.05 taken to indicate significance. Differences in the success rate between treatments were compared using the chi-squared test or Fisher’s exact test.
Results
There were no significant differences between the groups in demographic characteristics, stone size, location, radiodensity or positioning, and mode of location, number of ESWL sessions and shocks or energy used (Table 1).
Table 1.
The demographic and other variables in the study groups, and the analysis of results.
| Mean (SD) or n (%) variable | Group 1 (control) | Group 2 (tamsulosin) | P |
|---|---|---|---|
| Age (years) | 43.8 (10.4) | 40.1 (11.8) | 0.066 |
| Sex (M/F) | 39 (60)/26 (40) | 41 (63)/24 (37) | 0.718 |
| Presentation | |||
| Ureteric colic | 52 (80) | 52(80) | 0.927 |
| LUTS | 11(17) | 9 (14) | |
| Haematuria | 2 (3) | 4 (6) | |
| History of recurrent | |||
| Ureterolithotomy | 4 (6) | 2 (3) | 0.558 |
| Ureteroscopy | 3 (5) | 5 (8) | |
| None | 58 (89) | 58 (89) | |
| Stone site | |||
| Upper | 31 (48) | 25 (39) | 0.469 |
| Middle | 13 (20) | 14(22) | |
| Lower | 21 (32) | 26(40) | |
| Stone size (mm) | |||
| 5–10 | 48 (74) | 50 (77) | 1.000 |
| 11–15 | 17 (26) | 15 (23) | |
| Stone density | |||
| Radio-opaque | 58 (89) | 59 (91) | 0.028 |
| Radiolucent | 7 (11) | 6 (9) | |
| Localisation by | |||
| Fluoroscopy | 58 (89) | 59 (91) | 0.028 |
| US | 7 (11) | 6 (9) | |
| Energy/session | |||
| 6 | 29 (45) | 285(43) | 1.000 |
| 7 | 36 (55) | 37 (57) | |
| Shock waves/session | |||
| 3000 | 3 (5) | 3 (5) | 0.556 |
| 3500 | 31 (48) | 25 (39) | 0.556 |
| 4000 | 31 (48) | 37 (57) | 0.370 |
| Outcome | |||
| Stone clearance | |||
| Failure | 4 (6) | 3 (5) | 0.070 |
| CSRF | 3 (5) | 7 (11) | 0.010 |
| Stone-free | 58 (89) | 55 (85) | 0. 340 |
| Complications (Clavien grade) | |||
| Grade 1 | 4 (6) | 0 | 0.002 |
| Grade 3 | 4 (6) | 4 (6) | 0.130 |
| None | 57 (88) | 61 (94) | 0.003 |
| Auxiliary procedures | |||
| JJ stent | 1 (2) | 1 (2) | 0.400 |
| Perc. nephrostomy | 1 (2) | 0 | 0.007 |
| Ureteroscopy | 2 (3) | 3 (5) | 0.130 |
| None | 61 (94) | 61 (94) | 0.500 |
| Stone clearance vs. stone size and location | |||
| Stone free, n/N (%) | |||
| 5–10 mm | 45/48 (94) | 44/50 (88) | 0.016 |
| 11–15 mm | 13/17 (77) | 11/15 (73) | 0.220 |
| Upper ureter | 28/31 (90) | 23/25 (92) | 0.130 |
| Middle ureter | 10/13 (77) | 10/14 (71) | 0.520 |
| Lower ureter | 18/21 (86) | 22/26 (85) | 0.170 |
| Secondary outcome analysis | |||
| Expulsion time (days) | 45.4 (22.94) | 33.6 (15.18) | 0.001 |
| Median n ESWL sessions | 2.5 | 2.2 | 0.360 |
| Steinstrasse, n | 4 | 2 | 0.011 |
| Cumulative diclofenac dose (mg) | 750 | 380 | 0.004 |
CSRF, clinically significant residual fragments.
After 30 days of ESWL most patients became stone-free in both groups, with an overall stone-free rate of 89% (58/65) and 85% (55/65) in groups 1 and 2, respectively, with no statistically significant difference (P = 0.34; Table 1).
Table 1 also shows the treatment failures after three sessions of ESWL, in seven patients (11%) of group 1 (four with no fragmentation and three with significant residual stones) and 10 (15%) in group 2 (three had no fragmentation and seven had significant residual stones). Ureteroscopy was used in five patients (two in group 1 and three in group 2). Open ureterolithotomy was used to treat three patients in each group after failed trials of ureteroscopy. Three patients in each group passed their stones spontaneously during the follow-up. The mean (range) time to stone expulsion in both groups is also shown in Table 1; the difference was statistically significant (P = 0.001).
Table 1 also shows the overall complication rate (12 patients, 9%) and in both groups. The classification according to the modified Clavien system showed that four complications (3%) were grade I and eight (6%) were grade III. In group 1 there were complications in eight (12%) patients, four with severe ureteric colic that required hospital admission and auxiliary procedures, and another four had fever with progressive hydronephrosis. Two patients in group 1 required ureteroscopy, one a JJ stent and one a percutaneous US-guided nephrostomy. In group 2 there were complications in four (6%) patients, with two developing fever with progressive hydronephrosis, one with severe ureteric colic that required hospital admission and another one had massive haematuria; auxiliary procedures were required in three (ureteroscopy) and one (JJ stent).
The ureter was obstructed by steinstrasse in four patients in group 1 and two in group 2. There were no statistically significant differences between the groups in stone size, site, radio-density, positioning, mode of localisation, number of sessions, shocks or energy used.
When patients were stratified according to stone size, in those with a stone of >10 mm the success rate was similar in both groups (77% in group 1 vs. 73% in group 2), and the difference was statistically insignificant (P = 0.22; Table 1) When patients were stratified by stone location the clearance rates for upper, middle and lower ureteric stones in group 2 vs. group 1 were 92%, 71% and 85%, vs. 90%, 77% and 86% (P = 0.13, 0.52 and 0.17, respectively), and the difference was statistically insignificant (P = 0.15; Table 1).
There were no adverse effects of tamsulosin and none of the patients in group 2 stopped the drug.
Table 1 also shows the mean cumulative diclofenac dose, at 380 mg/patient in group 2 and 750 mg/patient in group 1; the difference was statistically significant (P = 0.004)
Discussion
Tamsulosin hydrochloride is the most commonly used α1-blocker for the medical treatment of ureteric stones, because it has excellent tolerability, lack of dose titration on starting treatment and its selectivity for the α1a and α1d receptors. This action results in relaxation of the smooth muscle of the ureter, releasing the spasm of the smooth muscle, thus facilitating stone passage and relieving pain [12].
The mean age of the present study groups was 43.8 years for group 1 and 40.1 years for group 2, with a preponderance of men in both groups (Table 1). These results agree with those reported previously by several authors [13,14]. The results of the present study agree with most previous studies for the absence of associations between the age and sex of the patient, side and nature of the stone, and the treatment outcome [15–17].
Several studies reported that adjunctive therapy with tamsulosin after ESWL was more effective than and equally as safe as lithotripsy alone in the treatment of patients with lower ureteric stones [3–9]. The stone free rates in the present study were 89% and 85% in groups 1 and 2, respectively, using the Dornier machine for ESWL, and the difference was statistically insignificant (P = 0.34). These rates lie in the range reported by others [12,17] (63.3–96.6%). These results give the impression that tamsulosin did not improve stone clearance, a finding reported previously by some [13,18]. Losek and Mauro [19] concluded that evidence for ureteric stone clearance was inconclusive and the overall ureteric stone clearance rates were 33.3–79.3% in the control groups, compared with 66.6–96.6% in the tamsulosin groups. A meta-analysis by Zhu et al. [20] showed a 16% difference in the risk of stone clearance after ESWL, favouring the tamsulosin group over the control group, i.e., an average of six patients had to be treated with tamsulosin after ESWL to achieve clearance in one. A subgroup analysis for the six studies that used a dose of 0.4 mg tamsulosin showed a pooled risk difference of 19 (10–29)%, i.e., five patients had to be treated with 0.4 mg tamsulosin after ESWL to achieve clearance in one. However, there is no conclusive evidence of the effectiveness of tamsulosin for stone clearance.
Several variables are fundamental for the migration process of stone fragments, i.e., stone size, intrinsic areas of narrowing within the ureter, ureteric peristalsis and oedema, infection, and spasm of the ureter at the site at which the stone is lodged. Oedema, infection, spasm and ureteric peristalsis could be modified by an appropriate medical therapy. Some investigators reported the effectiveness of different pharmacological therapies for increasing ureteric stone expulsion by acting primarily on spasm and peristalsis [3–5,21].
One of the main advantages of tamsulosin therapy is to shorten the period of stone passage. The mean time to stone passage in the present study was 33.6 days for patients in group 2 and 45.4 days in the control group (P = 0.001). These results agree with those reported previously [13,22]. Singh et al. [11] reported that the mean (SD) time for expulsion of the fragments was 26.78 (11.960 days in a tamsulosin group and 31.28 (18.31) days in a control group. In the study by Wang et al. [23], the mean time to stone expulsion was 8.1 days and 11.6 days in a tamsulosin group and control group, respectively. The expulsion time was analysed in three studies by Zhu et al. [20]. The expulsion time was shortened by 8 days in the tamsulosin groups.
Another advantage of adjunctive tamsulosin treatment in the present and other studies [6,13,24] is the significant reduction in the need for analgesics. The mean cumulative diclofenac dose in the present study was 380 mg/patient in group 2 and 750 mg/patient in group 1 (P = 0.004). Dellabella et al. [24] used tamsulosin as a spasmolytic drug during episodes of ureteric colic associated with juxtavesical calculi. They reported an increased stone expulsion rate, with a decrease in stone expulsion time and the need for hospitalisation and endoscopic procedures. In particular, there was good control of colic. Conversely, Gravas et al. [13], in a study of 64 patients with lower ureteric calculi, found a statistically similar success rate in patients receiving or not receiving tamsulosin (66.6% vs. 58.1%; P > 0.05). However, the mean diclofenac dose was 57 mg in the tamsulosin group and 119 mg in the control group, a difference that was statistically significant (P = 0.02). Losek and Mauro [19] reviewed five prospective studies to evaluate the efficacy of tamsulosin combined with ESWL. Reports of pain and supplemental analgesic dosing were consistently lower with tamsulosin. Tamsulosin has been reported to reduce painful episodes. In the present study there was no great effect of stone size, location or radiodensity on the rate of failure of ESWL.
A few studies have reported the efficacy of tamsulosin in upper ureteric stones [8,11]. In the present series, the stone-free rate for ESWL in upper ureteric stones was slightly higher in group 2 than in group 1 (92% vs. 90%; P = 0.13). Singh et al. [11] treated 117 patients who had a single upper ureteric calculus with ESWL. The clearance rates after 1–3 months were higher in the tamsulosin group than the control group (85%, 90% and 92% vs. 71%, 80% and 86%; P = 0.01, 0.11 and 0.34, respectively). The stone-free rates were not statistically different between larger stones (length > 10 mm) and smaller stones (length < 10 mm).
The better results in upper ureteric stones were largely due to the advantages of the lithotripter used, with the facility to rotate the treatment head. For middle and lower stones, it was mainly used in the overhead position, which enables easy and precise focusing, but for patients with upper ureteric stones, it would be more comfortable to maintain a supine rather than a prone position.
Although from previous reports there is still no consensus on the number of ESWL treatments that should be administered for ureteric calculi before alternative treatments are used [15], in the present series we considered absent or poor fragmentation after three ESWL sessions as a failure.
In the present study the overall complication rate was 9.2% (12/130) and auxiliary procedures were required in only 6% of patients. In previous studies, the need for auxiliary procedures was 2–28% [25,26].
Although this study was carefully devised and conducted, it has some limitations and shortcomings. First, there were relatively few patients, and it is known from previous studies that in those with fewer than 200 patients, the stone-free rate was relatively low and mostly <85%. There is a possibility that experience with the third generation ESWL machines is required to achieve a high stone-free rate [26]. Logarakis et al. [27] compared the operator-specific success rate using the same lithotripter, and showed that the best outcome was achieved by the surgeon who had treated the most patients. Second, the low power (12–15 kV) used in the present study might be related to the increase in the number of sessions and could have a role in the relatively low stone-free rates. Many researchers recommended higher voltages for treating ureteric stones (17–19 kV) [17]. The best surgeon also used more shocks and had the longest fluoroscopy time [27]. The third limitation is the inclusion of radiolucent stones in the present study, with the known difficulty in locating such stones even using US. Finally, there was a heterogeneous population of stones in different locations with different stone-free rates. It is probably better to include all cases with stones at one location.
In conclusion, despite these limitations, the present results indicate that the use of tamsulosin after ESWL in this specific subgroup of patients did not result in improved success and stone-free rates, but decreased the expulsion time and significantly reduced the need for analgesics, and was associated with significantly fewer complications, especially steinstrasse.
Conflict of interest
None.
Source of Funding
None.
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Mitre A.I., Chambo J.L., Nahas W.C. Ureteral calculi. extracorporeal shock-wave lithotripsy performed in situ on an outpatient basis. World J Urol. 1992;10:213–215. [Google Scholar]
- 2.Gnanapragasam V.J., Ramsden P.D., Murthy L.S., Thomas D.J. Primary in situ extracorporeal shock wave lithotripsy in the management of ureteric calculi: results with a third-generation lithotripter. BJU Int. 1999;84:770–774. doi: 10.1046/j.1464-410x.1999.00284.x. [DOI] [PubMed] [Google Scholar]
- 3.Hollingsworth J.M., Rogers M.A., Kaufman S.R. Medical therapy to facilitate urinary stone passage: a meta-analysis. Lancet. 2006;368:1171–1179. doi: 10.1016/S0140-6736(06)69474-9. [DOI] [PubMed] [Google Scholar]
- 4.Gravina G.L., Costa A.M., Ronchi P., Galatioto G.P., Angelucci A., Castellani D. Tamsulosin treatment increases clinical success rate of single extracorporeal shock wave lithotripsy of renal stones. Urology. 2005;66:24–28. doi: 10.1016/j.urology.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Kupeli B., Irkilata L., Gurocak S., Tunc L., Kirac M., Karaoglan U. Does tamsulosin enhance lower ureteral stone clearance with or without shock wave lithotripsy? Urology. 2004;64:1111–1115. doi: 10.1016/j.urology.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Bhagat S.K., Chacko N.K., Kekre N.S., Gopalakrishnan G., Antonisamy B., Devasia A. Is there a role for tamsulosin in shock wave lithotripsy for renal and ureteral calculi? J Urol. 2007;177:2185–2188. doi: 10.1016/j.juro.2007.01.160. [DOI] [PubMed] [Google Scholar]
- 7.Naja V., Agarwal M.M., Mandal A.K. Tamsulosin facilitates earlier clearance of stone fragments and reduces pain after shockwave lithotripsy for renal calculi: results from an open-label randomized study. Urology. 2008;72:1006–1011. doi: 10.1016/j.urology.2008.05.035. [DOI] [PubMed] [Google Scholar]
- 8.Preminger G.M., Tiselius H.G., Assimos D.G. Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610–1631. doi: 10.1016/j.eururo.2007.09.039. [DOI] [PubMed] [Google Scholar]
- 9.Argyropoulos A.N., Tolley D.A. Optimizing shock wave lithotripsy in the 21st century. Eur Urol. 2007;52:344–352. doi: 10.1016/j.eururo.2007.04.066. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal M.M., Naja V., Singh S.K. Is there an adjunctive role of tamsulosin to extracorporeal shockwave lithotripsy for upper ureteric stones: results of an open label randomized nonplacebo controlled study. Urology. 2009;74:989–992. doi: 10.1016/j.urology.2009.06.075. [DOI] [PubMed] [Google Scholar]
- 11.Singh S.K., Pawar D.S., Griwan M.S., Indora J.M., Sharma S. Role of tamsulosin in clearance of upper ureteral calculi after extracorporeal shock wave lithotripsy: a randomized controlled trial. Urol J. 2011;8:14–20. [PubMed] [Google Scholar]
- 12.Ahmed A.A., Al-Sayed A.S. Tamsulosin versus alfuzosin in the treatment of patients with distal ureteral stones: prospective, randomized, comparative study. Korean J Urol. 2010;51:193–197. doi: 10.4111/kju.2010.51.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gravas S., Tzortzis V., Karatzas A., Oeconomou A., Melekos M.D. The use of tamsulosin as adjunctive treatment after ESWL in patients with distal ureteral stone: do we really need it? Results from a randomised study. Urol Res. 2007;35:231–235. doi: 10.1007/s00240-007-0106-4. [DOI] [PubMed] [Google Scholar]
- 14.Gerber R., Studer U.E., Danuser H. Is newer always better? A comparative study of 3 lithotriptor generations. J Urol. 2005;173:2013–2016. doi: 10.1097/01.ju.0000158042.41319.c4. [DOI] [PubMed] [Google Scholar]
- 15.Abdel-Khalek M., Sheir K., Elsobky E. Prognostic factors for extracorporeal shock-wave lithotripsy of ureteric stones – a multivariate analysis study. Scand J Urol Nephrol. 2003;37:413–418. doi: 10.1080/00365590310006255. [DOI] [PubMed] [Google Scholar]
- 16.Kanao K., Nakashima J., Nakagawa K. Preoperative nomograms for predicting stone-free rate after extracorporeal shock wave lithotripsy. J Urol. 2006;176:1453–1457. doi: 10.1016/j.juro.2006.06.089. [DOI] [PubMed] [Google Scholar]
- 17.Abdelghany M., Zaher T., El Halaby R., Osman T. Extracorporeal shock wave lithotripsy of lower ureteric stones: Outcome and criteria for success. Arab J Urol. 2011:35–39. doi: 10.1016/j.aju.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skolarikos A., Alivizatos G., de la Rosette J.J. Extracorporeal shock wave lithotripsy 25 years later. Complications and their prevention. Eur Urol. 2006;50:981–990. doi: 10.1016/j.eururo.2006.01.045. [DOI] [PubMed] [Google Scholar]
- 19.Losek R.L., Mauro L.S. Efficacy of tamsulosin with extracorporeal shock wave lithotripsy for passage of renal and ureteral calculi. Ann Pharmacother. 2008;42:692–697. doi: 10.1345/aph.1K546. [DOI] [PubMed] [Google Scholar]
- 20.Zhu Y., Duijvesz D., Rovers M.M., Lock T.M. α-Blockers to assist stone clearance after extracorporeal shock wave lithotripsy: a meta-analysis. BJU Int. 2010;106:256–261. doi: 10.1111/j.1464-410X.2009.09014.x. [DOI] [PubMed] [Google Scholar]
- 21.Cervenàkov I., Fillo J., Mardiak J., Kopecný M., Smirala J., Lepies P. Speedy elimination of ureterolithiasis in lower part of ureters with the alpha-1 blocker- Tamsulosin. Int Urol Nephrol. 2002;34:25–29. doi: 10.1023/a:1021368325512. [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi M., Naya Y., Kino M. Low dose tamsulosin for stone expulsion after extracorporeal shock wave lithotripsy: efficacy in Japanese male patients with ureteral stone. Int J Urol. 2008;15:495–498. doi: 10.1111/j.1442-2042.2008.02033.x. [DOI] [PubMed] [Google Scholar]
- 23.Wang H., Liu K., Ji Z., Li H. Effect of alpha1-adrenergic antagonists on lower ureteral stones with extracorporeal shock wave lithotripsy. Asian J Surg. 2010;33:37–41. doi: 10.1016/S1015-9584(10)60007-3. [DOI] [PubMed] [Google Scholar]
- 24.Dellabella M., Milanese G., Muzzonigro G. Efficacy of Tamsulosin in the medical management of juxtavesical ureteral stones. J Urol. 2003;170:2202–2205. doi: 10.1097/01.ju.0000096050.22281.a7. [DOI] [PubMed] [Google Scholar]
- 25.Hochreiter W.W., Danuser H., Perrig M., Studer U.E. Extracorporeal shock wave lithotripsy for distal ureteral calculi: what a powerful machine can achieve. J Urol. 2003;169:878–880. doi: 10.1097/01.ju.0000051896.15091.0c. [DOI] [PubMed] [Google Scholar]
- 26.Murota-Kawano A., Ohya K., Sekine H. Outpatient basis extracorporeal shock wave lithotripsy for ureter stones. Efficacy of the third generation lithotripter as the first line treatment. Int J Urology. 2008;15:210–215. doi: 10.1111/j.1442-2042.2007.01970.x. [DOI] [PubMed] [Google Scholar]
- 27.Logarakis N.F., Jewett M.A., Luymes J., Honey R.J. Variation in clinical outcome following shock wave lithotripsy. J Urol. 2000;163:721–725. [PubMed] [Google Scholar]



