Abstract
Aim: To evaluate platelet function in patients with a history of surgical treatment for hepatic hydatid disease (HD). Methods: This retrospective case-controlled study was performed in a state hospital in Turkey from January 2009 to November 2013. The patients were divided into two groups: those evaluated in the preoperative period (Group 1) and those evaluated in the postoperative period (Group 2). The patient groups were compared with a control group (Group 3). All three groups were evaluated using laboratory records from day 1 of the preoperative period and day 30 of the postoperative period. The haematocrit level (HTC), platelet count (PLT), mean platelet volume (MPV), platelet distribution width (PDW), and percentage of eosinophils (EOS) were compared among the groups. Results: Fifty-three patients who had undergone surgical treatment of hepatic HD and 55 healthy controls were included in the study. The mean follow-up time for all patients was 45 (14-70) months. The patients comprised 33 (62%) females and 20 (38%) males. The control group comprised 37 (67%) females and 18 (33%) males. The median age of the patients was 48 (19-78) years, while that of the control group was 42 (16-64) years. No significant differences in the HTC, PLT, or EOS were present among the groups. The MPV and PDW indicated that platelet function was significantly different between Group 1 and Groups 2 and 3. Additionally, nine patients had undergone previous surgical treatment for HD. In a separate long-term follow-up, these patients exhibited no statistically significant differences in MPV or PDW between the preoperative and postoperative periods. Conclusions: MPV and PDW can be used in the initial follow-up of patients with hepatic HD, but have limited use in long-term follow-up.
Keywords: Hepatic hydatid cysts, platelet function test, disease management
Introduction
The dog tapeworm Echinococcus granulosus is one of a group of medically important parasitic helminths of the family Taeniidae (phylum, Platyhelminthes; class, Cestoda; order, Cyclophyllidea) that infect at least 50 million people globally. Its life cycle involves two mammals: an intermediate host (usually a domestic or wild ungulate) and a canine definitive host (such as the domestic dog) [1]. A zoonosis caused by the larval stages of the cestode E. granulosus is widespread in developing and underdeveloped regions of the world. The disease is endemic in the Middle East, Central Asia, and Northern and Eastern Africa [2-4]. Humans are accidental intermediate hosts of this helminth parasite and are unable to transmit this disease to other humans. The larval (metacestode) stage causes hydatidosis (cystic hydatid disease (HD) or cystic echinococcosis), a chronic cyst-forming disease in the accidental intermediate (human) host [1,5]. The eggs of this cestode are orally ingested, and the larvae are subsequently released into the intestine. They later invade the bloodstream and may be dispersed throughout the whole body. The larvae usually reach the liver through the portal tract, but may cross this barrier and spread to the lungs and other visceral organs to form cysts [6]. The location and size of these cysts and the clinical symptoms and complications determine the treatment modality. Although the main treatment is surgical, medical treatments may be considered in selected patients because of concerns regarding morbidity and mortality [7].
Platelets actively participate in haemostasis, tissue repair, induction of inflammation, and antimicrobial host defence [8]. Because they possess strong protective properties against helminths, they have the ability to kill the parasites independently from the leukocytes. The mean platelet volume (MPV) and platelet distribution width (PDW) are platelet function parameters and may be more sensitive biological markers of various diseases than the platelet count [9].
In the present study, we evaluated both the preoperative and postoperative MPV and PDW of patients who had undergone surgical treatment of hepatic HD.
Materials and methods
Patients
In this retrospective case-controlled study, the preoperative and postoperative laboratory records of 53 patients who had undergone surgical treatment of hepatic HD in the general surgery department of a state hospital from January 2009 to November 2013 were compared with those of a control group. The patients were divided into two groups: those evaluated in the preoperative period (Group 1) and those evaluated in the postoperative period (Group 2). The laboratory records from day 1 of the preoperative period and day 30 of the postoperative period were evaluated for both patient groups and the control group (Group 3) (Figure 1). The control group comprised healthy individuals who presented to the hospital for check-ups and had no acute or chronic disease. All controls were of similar age and sex as those in the patient groups. No patients had a history of drug use or blood transfusion.
Figure 1.
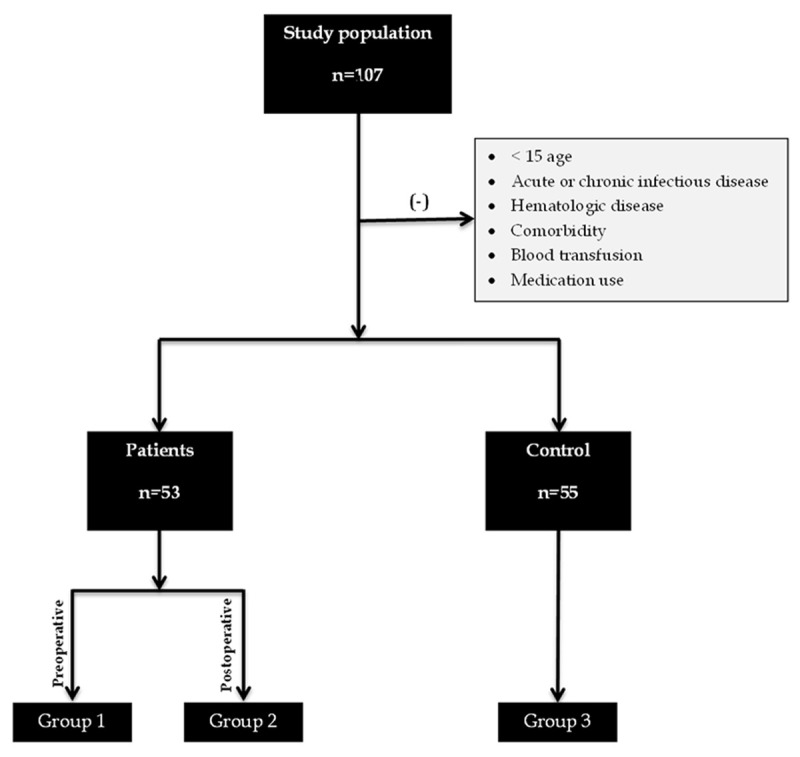
Study population and group distributions.
The diagnosis of hepatic HD was based on clinical evaluation, serological tests, and imaging findings. The patients’ preoperative and postoperative blood test results were compared. Additionally, the patients’ preoperative imaging findings were accessed from their electronic medical records, and the number and size of hepatic cysts were recorded. None of the patients had received preoperative antiparasitic treatment. All patients were given postoperative albendazole to prevent recurrence.
The exclusion criteria were age < 15 years, presence of acute or chronic infectious disease, presence of comorbidities (cardiac, respiratory, renal, endocrine, or vascular disease; cancer; and other conditions), presence of haematologic disease or a history of a blood transfusion within the last year for any reason, and on-going use of medication (analgaesics, oral contraceptives, antimetabolites, and other drugs).
Test methods
The patients’ venous blood samples were obtained on preoperative day 1 and postoperative day 30. All blood samples were stored in tubes containing ethylenediaminetetraacetic acid (EDTA) and assayed automatically using internationally certified devices. The reference values were as follows: haematocrit (HTC), 37% to 52%; platelet count (PLT), 130 to 400 × 103 cells/μL; MPV, 7.2 to 11.0 fL; PDW, 10% to 18%; and eosinophil percentage (EOS), 0% to 7%. All results were examined by an independent biochemistry expert who was unaware of the patients’ histories. Extreme results were reanalysed. All blood samples were evaluated in ≤ 10 min.
Statistical methods
The data were statistically compared among the three groups using statistical software (SPSS for Windows 21.0). The demographic and clinical characteristics of the patients are expressed using means ± standard deviation, medians, ranges, and percentages. Parametric parameters were investigated with Student’s t-test and one-way ANOVA, and nonparametric parameters were investigated using the Mann-Whitney U test and chi-squared test. The Wilcoxon test was used to compare the preoperative and postoperative complete blood count parameters. Associations between numeric data were compared using correlation analysis. The parameters in the patient and control groups were described using receiver operating characteristic curve analysis. The sensitivity, specificity, positive predictive value, negative predictive value, diagnostic accuracy, and likelihood ratio were calculated using the area under the receiver operating characteristic curve. All results were evaluated within the 95% confidence interval and at a P value of < 0.05.
Results
Fifty-three patients who had undergone surgical treatment of hepatic HD and 55 healthy individuals were included in the study. The patients comprised 33 (62%) females and 20 (38%) males. The control group comprised 37 (67%) females and 18 (33%) males. The patients’ median age was 48 (19-78) years, while the controls’ median age was 42 (16-64) years. Nine patients had undergone previous surgical treatment of HD. The mean time for recurrence among these nine patients was 26.4 months. In a separate long-term follow-up of these nine patients (Table 1), the mean size of the hepatic cysts was 86 ± 37 mm (calculated as the maximum hepatic cyst size in patients with multiple hepatic cysts). Among these patients, 66%, 12%, and 22% had single, double, and multiple cysts, respectively. Most were located in the right lobe (58%) and were not complicated (69%) (Table 1).
Table 1.
Demographic data and cyst characteristics
| Patients (n = 53) | Controls (n = 55) | |
|
| ||
| Median age (years) | 48 (19–78) | 42 (16-64) |
| Sex (M/F) | 20 (38%)/33 (62%) | 18 (33%)/37 (67%) |
| Recurrence | 9 (16%) | |
| Mean time for recurrence | 26.4 months | |
|
| ||
| Cyst Characteristics | ||
|
| ||
| Size (mm)* | 85.5 ± 37 (10-160) | |
| Number (n) | ||
| 1 | 32 (66%) | |
| 2 | 6 (12%) | |
| ≥ 2 | 11 (22%) | |
| Location | ||
| Right lobe | 30 (58%) | |
| Left lobe | 15 (29%) | |
| Bilateral | 7 (13%) | |
| Complicated cysts | ||
| Yes | 16 (31%) | |
| No | 36 (69%) | |
Calculated size of the maximal hepatic cyst in patients with multiple hepatic cysts.
No significant differences were observed in the HTC, PLT, or EOS among the groups. On the other hand, the MPV and PDW indicated that platelet function was significantly different between Group 1 and Groups 2 and 3. There was no statistically significant difference between Groups 2 and 3 (Table 2). The distribution of the MPV and PDW among the groups is presented in Figures 2 and 3. Among patients with recurrence, no significant difference in these parameters was noted between the preoperative and postoperative periods. A diagnostic comparison of the platelet parameters is presented in Table 3. The diagnostic efficacy of these parameters was limited. A negative correlation was detected between the MPV and PLT during the postoperative period (r = -0.314, P = 0.022) (Figure 4). The MPV was higher in patients with thrombocytopaenia. No correlation was observed between the size/number of cysts and the MPV or PDW.
Table 2.
Comparison of complete blood count parameters among the groups
| Group 1 | Group 3 | P value | |
|
| |||
| HTC (%) | 40 ± 5 | 39.2 ± 7.9 | NS |
| PLT (× 103 cells/μL) | 272 ± 108 | 254 ± 56 | NS |
| MPV (fL) | 8.9 ± 1.6 | 8.4 ± 0.8 | 0.038 |
| PDW (%) | 40.4 ± 17.6 | 32.7 ± 15.8 | 0.022 |
| EOS (%) | 3.7 ± 4.9 | 3.2 ± 1.7 | NS |
|
| |||
| Group 2 | Group 3 | P value | |
|
| |||
| HTC (%) | 38.7 ± 7.9 | 39.2 ± 7.9 | NS |
| PLT (× 103 cells/μL) | 278 ± 111 | 254 ± 56 | NS |
| MPV (fL) | 8.3 ± 1.8 | 8.4 ± 0.8 | NS |
| PDW (%) | 35.7 ± 17.1 | 32.7 ± 15.8 | NS |
| EOS (%) | 3.3 ± 2.7 | 3.2 ± 1.7 | NS |
|
| |||
| Group 1 | Group 2 | P value | |
|
| |||
| HTC (%) | 40 ± 5 | 38.7 ± 7.9 | NS |
| PLT (× 103 cells/μL) | 272 ± 108 | 278 ± 111 | NS |
| MPV (fL) | 8.9 ± 1.6 | 8.3 ± 1.8 | 0.009 |
| PDW (%) | 40.4 ± 17.6 | 35.7 ± 17.1 | 0.032 |
| EOS (%) | 3.7 ± 4.9 | 3.3 ± 2.7 | NS |
HTC: haematocrit, PLT: platelet count, MPV: mean platelet volume, PDW: platelet distribution width, EOS: percentage of eosinophils, NS: not significant. Data are presented as means ± standard deviation.
Figure 2.

Distribution of MPV among the groups.
Figure 3.

Distribution of PDW among the groups.
Table 3.
Diagnostic comparison of platelet parameters
| Cut-off point | AUC | Sensitivity | Specificity | PPV | NPV | LR+ | LR- | DA | |
|---|---|---|---|---|---|---|---|---|---|
| PLT | 272 (× 103 cells/μL) | 0.44 (CI: 0.33-0.55) | 48% | 65% | 57% | 57% | 1.39 | 0.79 | 57% |
| MPV | 7.75 fL | 0.41 (CI: 0.30-0.52) | 71% | 27% | 48% | 50% | 0.9 | 1.06 | 48% |
| PDW | 30.85% | 0.38 (CI: 0.27-0.48) | 69% | 49% | 56% | 62% | 1.36 | 0.63 | 58% |
PLT: platelet count, MPV: mean platelet volume, PDW: platelet distribution width, AUC: area under the receiver operating characteristic curve, PPV: positive predictive value, NPV: negative predictive value, LR+: positive likelihood ratio, LR–: negative likelihood ratio, DA: diagnostic accuracy.
Figure 4.

Correlation between platelet count and MPV. NS: not significant.
Discussion
Cystic echinococcosis or HD, a zoonosis caused by the adult or larval stages of the cestode E. granulosus, is endemic in some Mediterranean countries, the Middle East, South America, South Africa, and Oceania. It is a disease of rural areas where farming is traditionally practiced [5,10]. Humans are the incidental intermediate host. The eggs are orally ingested, and the larvae are subsequently released into the intestine. They later invade the bloodstream and may be dispersed throughout the whole body. The larvae usually reach the liver through the portal tract, but sometimes cross this barrier and spread to the lungs and other visceral organs to form cysts [6]. The location and size of these cysts and the patient’s clinical symptoms and complications determine the treatment modality. Although the main treatment is surgical, medical treatment may be considered in selected patients because of concerns regarding morbidity and mortality [7]. HD may occur in patients of any age and sex, although it is more common in those aged 20 to 40 years [11]. It affects the right liver lobe more commonly [12], and the cysts are usually solitary [13]. In the present study, HD was most frequently seen in the fourth decade of life and in female patients. Similarly, the cysts were usually located in the right lobe and solitary.
Platelets participate in various stages of blood coagulation; in various diseases, neoplasms, and inflammatory processes; and in allergic and immune reactions. Activated platelets play a role in the organism’s defence mechanisms, such as in antiparasitic immunologic reactions [14]. The cytotoxic activity of blood platelets is characterised by the release of various inflammatory mediators; they also exhibit phagocytic activity and cooperate with other cells of the immunologic system [15,16]. In these ways, blood platelets are effective in the prevention of infectious diseases. Furthermore, they are effective defenders in helminthic infections. Joseph et al. [17] reported that platelets can eliminate parasites independent of white blood cells.
Among the various platelet parameters, MPV and PDW are associated with parasitic infections. In a study by Maina et al. [18], the MPV was significantly higher in patients with malaria than in controls. Similarly, Coelho et al. [19] found higher MPVs in patients with thrombocytopaenic malaria. They also reported a negative correlation between the PLT and MPV. Kucukbayrak et al. [20] recently observed significantly higher MPVs were during the preoperative period than in the postoperative period in patients with pulmonary HD; Sit et al. [7] reported similar findings in patients with hepatic HD. Likewise, we observed significantly higher MPVs during the preoperative period than in the early postoperative period in our patients with hepatic HD. Additionally, we detected a statistically significant negative correlation between the PLT and MPV.
Although no previous studies have demonstrated a relationship between PDW and HD, the PDW was significantly higher during the early postoperative period in the present study. However, this relationship was absent during the long-term follow-up.
Only a limited number of reports have described the use of the MPV and PDW in the follow-up of patients with hepatic HD. Studies on the use of the PDW are particularly scarce. MPV and PDW measurement is low-cost and simple to perform, and these parameters are easy to evaluate. These tests can be used during the follow-up after treatment of conditions such as HD, thus having an impact on public health.
In conclusion, the MPV and PDW can be used in the short-term follow-up of patients with HD, but have limited use in the long-term follow-up and diagnosis. The MPV and PDW may be related to the performance of operations or presence of inflammation associated microorganisms other than E. granulosus. Thus, randomised, prospective studies using larger patient populations are needed for further investigation.
Disclosure of conflict of interest
None.
References
- 1.Garcia HH, Del Brutto OH. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol. 2005;4:653–661. doi: 10.1016/S1474-4422(05)70194-0. [DOI] [PubMed] [Google Scholar]
- 2.Eckert J, Deplazes P, Craig PS, Gemmell MA, Gottstein B, Heath D, Jenkins DJ, Kamiya M, Lightowlers M. Geographic Distribution and Prevalence. In: Eckert J, Gemmell MA, Meslin FX, Pawlowski ZS, editors. WHO/OIE Manual on Echinococcosis in Humans and Animals: A Public Health Problem of Global Concern. Paris: World Organisation for Animal Health; pp. 100–142. [Google Scholar]
- 3.Sadjjadi SM. Present situation of echinococcosis in the Middle East and Arabic North Africa. Parasitol Int. 2006;55:S197–202. doi: 10.1016/j.parint.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 4.Azlaf R, Dakkak A. Epidemiological study of the cystic echinococcosis in Morocco. Vet Parasitol. 2006;137:83–93. doi: 10.1016/j.vetpar.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Symeonidis N, Pavlidis T, Baltatzis M. Complicated liver echinococcosis: 30 years of experience from an endemic area. Scand J Surg. 2013;102:171–177. doi: 10.1177/1457496913491877. [DOI] [PubMed] [Google Scholar]
- 6.Geramizadeh B. Unusual locations of the hydatid cyst: a review from Iran. Iran J Med Sci. 2013;38:2–14. [PMC free article] [PubMed] [Google Scholar]
- 7.Sir M, Aktaş G, Yilmaz EE, Hakyemez IN, Alçelik A, Küçükbayrak A. Platelet parameters in hepatic hydatid cysts. Int J Inflam. 2013;2013:593273. doi: 10.1155/2013/593273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klinger MH, Jelkmann W. Role of blood platelets in infection and inflammation. J Interferon Cytokine Res. 2002;22:913–922. doi: 10.1089/10799900260286623. [DOI] [PubMed] [Google Scholar]
- 9.Liu R, Gao F, Huo J, Yi Q. Study on the relationship between mean platelet volume and platelet distribution width with coronary artery lesion in children with Kawasaki disease. Platelets. 2012;23:11–16. doi: 10.3109/09537104.2011.586073. [DOI] [PubMed] [Google Scholar]
- 10.Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459–463. doi: 10.1148/radiology.139.2.7220891. [DOI] [PubMed] [Google Scholar]
- 11.Bekçi TT. Diagnosis and treatment of human hydatid disease. Eur J Gen Med. 2012;9(Suppl 1):15–20. [Google Scholar]
- 12.Magistrelli P, Masetti R, Coppola R. Surgical treatment of hydatid disease of the liver: a 20-year experience. Arch Surg. 1991;126:518–523. doi: 10.1001/archsurg.1991.01410280122020. [DOI] [PubMed] [Google Scholar]
- 13.Silva MA, Mirza DF, Bramhall SR, Mayer AD, McMaster P, Buckels JAC. Treatment of hydatid disease of the liver. Dig Surg. 2004;21:227–234. doi: 10.1159/000079492. [DOI] [PubMed] [Google Scholar]
- 14.Matowicka-Karna J. The blood platelets in parasitic diseases. Pol Merkur Lekarski. 2006;21:295–298. [PubMed] [Google Scholar]
- 15.Panasiuk A, Matowicka-Karna J. Role of blood platelets in parasitic diseases. Wiad Parazytol. 1999;45:309–318. [PubMed] [Google Scholar]
- 16.Polack B, Peyron F, Auriault C. Platelet cytotoxicity against parasites. Nouv Rev Fr Hematol. 1991;33:317–322. [PubMed] [Google Scholar]
- 17.Joseph M, Auriault C, Capron A, Vorng H, Viens P. A new function for platelets: IgE-dependent killing of schistosomes. Nature. 1983;303:810–812. doi: 10.1038/303810a0. [DOI] [PubMed] [Google Scholar]
- 18.Maina RN, Walsh D, Gaddy C, Hongo G, Waitumbi J, Otieno L, Jones D, Ogutu BR. Impact of Plasmodium falciparum infection on haematological parameters in children living in Western Kenya. Malar J. 2010;9(Suppl 3):S4. doi: 10.1186/1475-2875-9-S3-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coelho HC, Lopes SC, Pimentel JP, Nogueira PA, Costa FT, Siqueira AM, Melo GC, Monteiro WM, Malheiro A, Lacerda MV. Thrombocytopenia in Plasmodium vivax malaria is related to platelets phagocytosis. PLoS One. 2013;8:e63410. doi: 10.1371/journal.pone.0063410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Küçükbayrak A, Oz G, Fındık G, Karaoğlanoğlu N, Kaya S, Taştepe I. Evaluation of platelet parameters in patients with pulmonary hydatid cyst. Mediterr J Hematol Infect Dis. 2010;2:e2010006. doi: 10.4084/MJHID.2010.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


