Abstract
There are many risk factors for the cause of postoperative cognitive dysfunction (POCD), however, the anesthesia selection always trigger controversy for the POCD occurrence. This study aims to explore the relationship between the anesthesia and the occurrence of POCD in elder patients, and also investigate the mechanism of the POCD. One hundred elder patients with hip replacement were included in this study, which were divided into general anesthesia (GA) and epidural analgesia (EA) group. Minimum mental state examination (MMSE) method was employed to assess the nervous and mental function (POCD) in both analgesia group patients. Aβ and tau protein levels in blood were detected by using the ELISA assay. The correlation between MMSE in POCD patients and Aβ or tau was analyzed by employing the Spearman rank correlation method. The results indicated that epidural analgesia decreases the MMSE scoring compared to general analgesia (P < 0.05). General analgesia enhanced the Aβ and tau level compared to epidural analgesia (P < 0.05). Aβ and tau level were increased in the patients with POCD. The POCD occurrence rate in GA group was significantly higher compared to EA group (P < 0.05). MMSE scores of POCD patients positively correlated with Aβ or tau level (P < 0.05). In conclusion, the epidural analgesia method was better than general analgesia method for the hip replacement in elder patients. The mechanism of the POCD may be caused by the enhancement of Aβ and Tau protein.
Keywords: General anesthesia, epidural analgesia, postoperative cognitive dysfunction, minimum mental state examination, cognitive dysfunction
Introduction
Postoperative cognitive dysfunction (POCD) is a subtle disorder of thought processes following anesthesia, surgery and injury, particularly in elderly [1]. The POCD may affect the short-term memory, cognitive functions, such as visual memory, verbal memory, attention, language comprehension, visuospatial abstraction and concentration [2]. Patients who experience cognitive decline or dysfunction account for 25% to 50% of hospitalized patients [1]. The incidence of POCD depends on the definition, composition of the test battery, and time of postoperative assessment. The previous studies showed that the incidence of POCD after surgery even achieves to 40.5% a few weeks after surgery for the elder patients [3]. There are many risk factors for the cause of POCD, however, the anesthesia selection always trigger controversy for the POCD happen. Anwer et al. [4] found that general anesthesia poses a significant risk for the occurrence of POCD compared to the epidural analgesia in elder patients. However, Williams-Russo P et al. [5] indicated that the type of anesthesia, general or epidural, does not affect the magnitude or pattern of POCD in older adults.
Aβ is derived from amyloid Precursor protein (APP) by cellular processing pathways that involve the excision of the Aβ region, possibly in distinct subcellular compartments [6]. The increased Aβ generation is central to the disease process comes from studies of very rare inherited forms of Alzheimer’s disease (AD). Tau protein is a highly soluble microtubule-associated protein (MAP), which are found mostly in neurons compared [7,8]. The main function of tau is to modulate the stability of axonal microtubules. Tau has two ways of controlling microtubule stability, including isoforms and phosphorylation [9]. Several studies have shown that the incidence tau phosphorylation was triggered by the β-amyloid (Aβ) peptide [10,11]. Nishimori et al. [12] proved that there is a closely relationship between levels of Aβ (and/or tau) and the occurrence of POCD.
Therefore, this study aims to explore the relationship between the anesthesia and the occurrence of POCD in elder patients, investigate the mechanism of the POCD, and hope to discover the optimized anesthesia for clinical.
Materials and methods
Patients
One hundred elder patients with hip replacement were included in this study, including 43 males and 57 females. The average age is 68.3 ± 8.1 years (range from 60 to 75 years). All of the total 100 patients were divided into two groups, including general anesthesia (GA) and epidural analgesia (EA) group, and with 50 patients each group, respectively.
Inclusive and exclusive criteria
Inclusive criteria: No stabilizing agent and antidepressant used pre-operation with long-time; No history of cardio surgery or nervous system operation; No family history of mental disorder; No serious defective vision; No AD and the other neurodegenerative diseases; with normal conscious.
Exclusive criteria: The patients with Minimum Mental State Examination (MMSE) score less than 23; The patients with no education history; The patients with central nervous system disease or mental disease; Long term administration of sedatives or antidepressant; Patient with the habit of excessive drinking.
Anaesthesia and monitor
The electrocardiogram, blood pressure, heart rate and blood oxygen saturation were monitored. The general anesthesia was induced with Midazolam (0.1 mg/kg), fentanyl (2-4 μg/kg), propofol (1-1.5 mg/kg), vecuronium bromide (0.1-0.15 mg/kg), by maintaining with 1% to 3% vol isoflurane. The tidal volume was 8-10 mg/kg, respiratory frequency was 10-12 time/min, and partial pressure of carbon dioxide maintaining with 30-35 mmHg. For the epidural analgesia patients, The L1-2 or L2-3 intervertebral spaces were selected for spinal puncture. The ropivacaine (0.5%) was used to anaesthetize. For all of the patients, the fentanyl (0.001%) was venoclysized with the speed of 2-2.5 ml/h within 48 hours to keep the analgesic effect.
POCD assessment
MMSE method was employed to assess the nervous and mental function (POCD) in both analgesia group patients. There are 30 items for mental state examination, including time, location, memory, contention, calculation, object naming, language repeat, reading comprehension, making sentences and graphical pinch painting. Totally, 30 scores, one score for one item, right with one score and wrong without score. The MMSE score of < 23 was considered as the POCD patients.
ELISA examination for Aβ and tau
Five milliliters fasting venous blood were drawn at 1 day pre-operation (T1), 1 day post-operation (T2) and 5 days post-operation (T3), respectively, for both group patients. The ELISA detection kit (Boshide, Wuhan, China) was used to examine the level of Aβ and tau in both group patients. The detail of the experimental process was performed according to the instructions of the ELISA kit.
Statistical analysis
The statistical analysis was performed using SPSS 17.0. Student’s t-test was used to find the significance of study parameters on the continuous scale within each group. Chi-square test was used to calculate the incidence of POCD. The correlation between MMSE in POCD patients and Aβ or tau was analyzed by employing the Spearman rank correlation method. Statistical significance was accepted with P < 0.05.
Results
General analgesia decreases the MMSE scoring
We assessed the MMSE scores at the different time of T1, T2 and T3, respectively. The MMSE scores at T2 were significantly lower compared to T1 and T3 in GA group (Figure 1, P < 0.05). There were no significant changes of MMSE scores in all of the time points (T1, T2 and T3) in EA group. Furthermore, the MMSE score at T2 in EA group was significantly higher compared to the GA group (Figure 1, P < 0.05). However, there were no significant differences at T1 and T3 in both groups.
Figure 1.
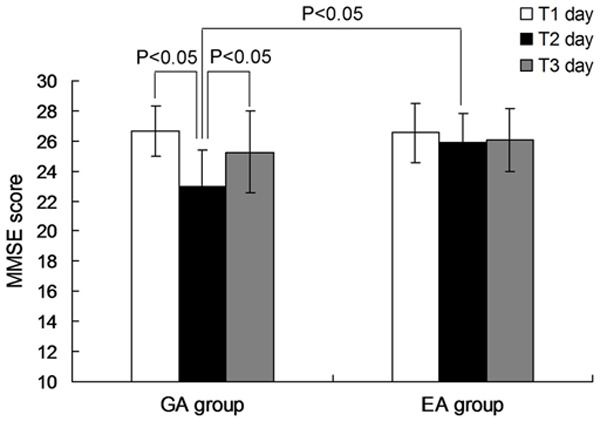
The MMSE scores in GA and EA group at different time. P < 0.05 represents the MMSE scores in GA group compared to EA group, or presents the MMSE scores in T2 day compared to T1, T2 day. GA: general anesthesia; EA: epidural analgesia; MMSE: minimum mental state examination.
Aβ and tau level enhanced in GA group compared to EA group
The level of Aβ and tau in GA group at T2 day was significantly higher compared to T1 or T3 day (Figure 2, P < 0.05). There were not significant differences among the T1, T2 and T3 day for the EA group (Figure 2, P > 0.05). However, At T2 day, the level of Aβ (Figure 2A) and tau (Figure 2B) in GA group was significantly increased compared to EA group (P < 0.05).
Figure 2.
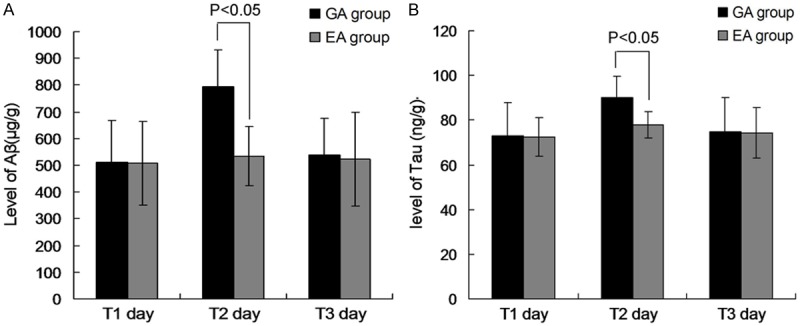
Aβ and Tau protein levels in GA and EA group at different time points. A. Aβ levels in GA and EA group. B. Tau levels in GA and EA group. P < 0.05 represents the Aβ or Tau level in GA group compared to EA group at T2 day. GA: general anesthesia; EA: epidural analgesia.
POCD occurrence rate in GA and EA group
The POCD occurrence rate in GA group at T1 was 36.0% (18 cases), 16.0% in EA group. The POCD occurrence rate in GA group was significantly higher compared to EA group (Table 1, P < 0.05). However, there were no significant differences in GA group compared to EA group at T2 and T3 day post-operation (Table 1, P > 0.05).
Table 1.
POCD occurrence rate in GA and EA group
| Group | POCD occurrence rate (n) | ||
|---|---|---|---|
|
| |||
| T1 day | T2 day | T3 day | |
| GA group | 36.0% (18) | 12.0% (6) | 10.0% (5) |
| EA group | 16.0% (8) | 8.0% (4) | 6.0% (3) |
GA: general anesthesia; EA: epidural analgesia.
Aβ and tau level were increased in the patients with POCD
In order to investigate the relationship between the POCD occurrence and Aβ or tau level, we divided all of the patients into two another groups, including patients with POCD post-operation (with POCD group) and patients without POCD post-operation (without POCD group). The results indicated that the Aβ and tau level in patients with POCD group were significantly higher compared to the patients without POCD group at T2 day (Figure 3, P < 0.05). Meanwhile, within the patients with POCD group, the Aβ and tau level in T2 day were significantly higher compared to the T1 and T3 day (Figure 3, P < 0.05).
Figure 3.
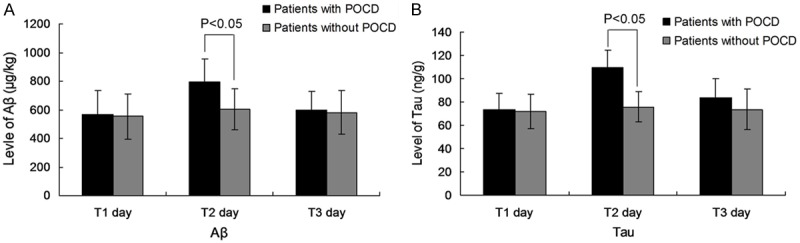
Aβ and Tau protein levels in patients with POCD and without POCD at different time points. A. Aβ levels in patients with and without POCD. B. Tau levels in with and without POCD. P < 0.05 represents the Aβ or Tau level in with POCD compared to patients without POCD at T2 day. POCD: postoperative cognitive dysfunction.
MMSE scores of POCD patients correlate with Aβ or tau level
To more clearly illustrate the function of Aβ or tau level in POCD, we analyzed the correlation between MMSE scores and POCD. The results showed that the MMSE scores in POCD patients were positively correlated with the Aβ level (Figure 4A, P < 0.05). Furthermore, the MMSE scores in POCD patients were also positively correlated with the tau levels (Figure 4B, P < 0.05).
Figure 4.
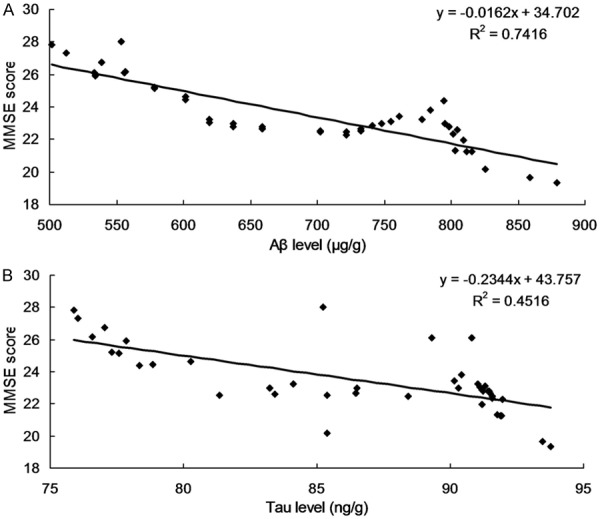
Correlation between MMSE scores and Aβ or Tau protein levels. A. Correlation between MMSE scores and Aβ protein levels. B. Correlation between MMSE scores and Tau protein levels.
Discussion
Following with the developing of the medical techniques, the ends of analgesia in clinical setting has been required to be safe, comfortable and minimal side effects, but not only is convenient for the operation. Especially, the analgesia strategy should not affect the functions of central nerve system or minimize the influence [13]. In clinical practice, the POCD is a very normally complication after the operation or surgery, however, the specific biomarker for the complication is also un-clarified [14]. The present study investigated the different analgesia method affecting the cognitive dysfunctions in patients underwent hip replacement in elderly, and discussed the different analgesia method influencing the occurrence of POCD. Furthermore, the correlation between POCD and the biomarkers (Aβ or tau) was also observed to reveal the mechanism of POCD.
Currently, the assessment of cognitive functions mainly depends on the mental examination. MMSE examination is the most frequently used method for the screening and assessing the cognitive dysfunctions [15]. Wiklund et al. [16] found that, for the brain cognitive function assessment, the sensitivity of MMSE method is 87% and the specificity of MMSE method is 82%. The MMSE method is the simple, feasible, extensive used screening tool for cognitive dysfunction or cognitive decline in clinical [17]. In this study, there was no significant difference between GA and EA group pre-operation (P > 0.05). However, the MMSE scores in GA group were decreased significantly compared to the EA group at T1 day (P < 0.05), though both GA and EA group with the declined MMSE scores. These results suggest that the both general and epidural methods could affect the cognitive functions in different degrees. Our study results indicated that the POCD occurrence rate at T1 day in GA group (36.0%) was significantly higher compared to the EA group (16.0%) (P < 0.05). This result suggests that the general analgesia could trigger the more obvious cognitive dysfunctions. The difference in both groups may be caused by the neuro-toxicity of the general analgesia drugs.
The previous study [18] proved that the toxicity of Aβ protein could induce the early apoptosis of the neurons. In this study, the Aβ level was increased in GA group, which illustrates that the general analgesia drug may activate the change of Aβ protein. The enhanced Aβ, therefore, mediates the neuron-toxicity of the patients. However, the epidural analgesia drug may not involve this pathway. The retrospective study [19] also indicated that the Aβ level in mild cognitive impairment patient was significantly increased compared to the normal individuals. Tau protein is kind of functional protein in brain tissues, and is a kind of highest expressed tubilin-associated protein. The expression of tau protein could induce the cellular morphology change, synapsis decreased, and causes the cell apoptosis finally. Some scientists [20] have defined the Tau protein as the biomarker of the neuron degeneration. In this study, the Aβ and Tau level in GA group was higher compared to EA group, which hints that the POCD occurrence may associate with the Aβ and Tau protein. The correlation analysis also indicated that the POCD was positively correlated with the Aβ or Tau protein expression.
In conclusion, the POCD occurrence rate in EA group was significantly lower compared to the GA group. The Aβ and Tau level in patients with POCD was higher significant compared to the patients without POCD. Therefore, the epidural analgesia was better than the general analgesia method for the hip replacement elder patients. The mechanism of the POCD may be caused by the enhancement of Aβ and Tau protein.
Disclosure of conflict of interest
None.
References
- 1.Terrando N, Brzezinski M, Degos V. Perioperative cognitive decline in the aging population. Mayo Clin Proc. 2011;86:885–893. doi: 10.4065/mcp.2011.0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang C, Zhu B, Ding J, Wang ZG. Isoflurane anesthesia aggravates cognitive impairment in streptozotocin-induced diabetic rats. Int J Clin Exp Med. 2014;7:903–910. [PMC free article] [PubMed] [Google Scholar]
- 3.Hansen MV. Chronobiology, cognitive fuction and depressive symptoms in surgical patients. Dan Med J. 2014;61:B4914. [PubMed] [Google Scholar]
- 4.Steinmetz J, Christensen KB, Lund T. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110:548–555. doi: 10.1097/ALN.0b013e318195b569. [DOI] [PubMed] [Google Scholar]
- 5.Coburn M, Fahlenkamp A, Zoremba N, Schaelte G. Postoperative cognitive dysfunction: Incidence and prophylaxis. Anaesthesist. 2010;59:177–184. doi: 10.1007/s00101-009-1657-2. [DOI] [PubMed] [Google Scholar]
- 6.Anwer HM, Swelem SE, el-Sheshai A, Moustafa AA. Postoperative cognitive dysfunction in adult and elderly patients: general anesthesia vs. subarachnoid or epidural analgesia. Middle East J Anaesthesiol. 2006;18:1123–1138. [PubMed] [Google Scholar]
- 7.Williams-Russo P, Sharrock NE, Mattis S, Szatrowski TP, Charlson ME. Cognitive effects after epidural vs general anesthesia in older adults, a randomized trial. JAMA. 1995;274:44–50. [PubMed] [Google Scholar]
- 8.Iversen LL, Mortishire-Smith RJ, Pollack SJ, Shearman MS. The toxicity in vitro of beta-amyloid protein. Biochem J. 1995;311:1. doi: 10.1042/bj3110001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanfilippo M, Wefki Abdelgawwad Shousha AA, Paparazzo A. Emergence in elderly patient undergoing general anesthesia with xenon. Case Rep Anesthesiol. 2013;2013:736790. doi: 10.1155/2013/736790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galimberti D, Scarpini E. Genetics and biology of Alzheimer’s disease and frontotemporal lobar degeneration. Int J Clin Exp Med. 2010;3:129–143. [PMC free article] [PubMed] [Google Scholar]
- 11.Harada A, Oguchi K, Okabe S, Kuno J, Terada S, Ohshima T, Sato-Yoshitake R, Takei Y, Noda T, Hirokawa N. Altered microtubule organization in small-calibre axons of mice lacking tau protein. Nature. 1994;369:488–491. doi: 10.1038/369488a0. [DOI] [PubMed] [Google Scholar]
- 12.Manukhina EB, Goryacheva AV, Barskov IV, Viktorov IV, Guseva AA, Pshennikova MG, Khomenko IP, Mashina SY, Pokidyshev DA, Malyshev IY. Prevention of neurodegenerative damage to the brain in rats in experimental Alzheimer’s disease by adaptation to hypoxia. Neurosci Behav Physiol. 2010;40:737–743. doi: 10.1007/s11055-010-9320-6. [DOI] [PubMed] [Google Scholar]
- 13.Kitazawa M, Cheng D, Laferla FM. Chronic copper exposure exacerbates both amyloid and tau pathology and selectively dysregulates CDK5 in a mouse model of AD. J Neurochem. 2009;108:1550–1560. doi: 10.1111/j.1471-4159.2009.05901.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nishimori ML, Low JH, Zheng H. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database Syst Rev. 2012;11:CD005059. doi: 10.1002/14651858.CD005059.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Hemerka JN, Wu X, Dixon CE, Garman RH, Exo JL, Shellington DK, Blasiole B, Vagni VA, Janesko-Feldman K. Severe brief pressure-controlled hemorrhagic shock after traumatic brain injury exacerbates functional deficits and long-term neuropathological damage in mice. J Neurotrauma. 2012;29:2192–2208. doi: 10.1089/neu.2011.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rohan D, Buggy DJ, Crowley S. Increased incidence of postoperative cognitive dysfunction 24 h after surgery in the elderly. Can J Anaesth. 2005;52:137–142. doi: 10.1007/BF03027718. [DOI] [PubMed] [Google Scholar]
- 17.Yang C, Zhu B, Ding J, Wang ZG. Isoflurane anesthesia aggravates cognitive impairment in streptozotocin-induced diabetic rats. Int J Clin Exp Med. 2014;7:903–110. [PMC free article] [PubMed] [Google Scholar]
- 18.Wiklund A, Granon S, Faure P. Object memory in young and aged mice after sevoflurane anaesthesia. Neuroreport. 2009;20:1419–1423. doi: 10.1097/WNR.0b013e328330cd2b. [DOI] [PubMed] [Google Scholar]
- 19.Yang C, Zhu B, Hua F. Leptin deficiency is involved in the cognitive impairment of streptozocin-induced diabetic rats undergoing cardiopulmonary bypass. Int J Clin Exp Med. 2014;7:2571–2577. [PMC free article] [PubMed] [Google Scholar]
- 20.Homma S, Watanabe N, Matsuo H. Topographical electrogastrograms after radical esophagectomy with colonic replacement. Surg Today. 2003;33:584–589. doi: 10.1007/s00595-003-2550-2. [DOI] [PubMed] [Google Scholar]
- 21.Xiang J, Pan J, Chen F, Zheng L, Chen Y, Zhang S, Feng W. L-3-n-butylphthalide improves cognitive impairment of APP/PS1 mice by BDNF/TrkB/PI3K/AKT pathway. Int J Clin Exp Med. 2014;7:1706–1713. [PMC free article] [PubMed] [Google Scholar]
- 22.Burburan SM, Xisto DG, Rocco PR. Anaesthetic management in asthma. Minerva Anestesiol. 2007;73:357–365. [PubMed] [Google Scholar]


