Abstract
Objective: To investigate superiorities of a special needle-over-cannula adopting different location methods for continuous femoral nerve block (CFNB) for geriatric lower extremity joint arthroplasty. Methods: 60 elderly patients intending to receive scheduled knee or hip replacement surgery were recruited and divided into 3 groups randomly. Group 1 (n=20) adopted fascial pop for continuous femoral nerve block and postoperative analgesia with indwelling cannula. Group 2 (n=20) adopted location guided by B ultrasound, and Group 3 (n=20) adopted fascial pop combined with B ultrasound. Results: There was significant difference in the performing time of cannula indwelling on average between each two groups (P<0.01). There was no significant difference among three groups about visual analogue scale (VAS) score, Ramsay sedation score (RSS), incidence of nausea and vomit, or patient’s satisfaction at 6, 12, 24 and 48 h. Infection at the puncture site, toxic reaction of local anesthetics and respiratory depression were absent during the cannula indwelling. All the patients did not receive any other analgesic, and the indwelling time of external cannula was 45.3 hours on average. There was only one patient in group 2 who felt mild pains in front of the thigh after removing the indwelling cannula. No stolidity or other abnormal symptom was found among the remaining patients. Conclusions: Shorter indwelling cannula time and higher success rate of single attempt placement suggest that fascial pop combined ultrasound guidance is worth for clinical recommendation.
Keywords: Needle-over-cannula, femoral nerve block, ultrasound guidance, lower extremity joint arthroplasty, postoperative analgesia
Introduction
In order to reduce the complication or adverse reaction caused by intraspinal postoperative analgesia and opioid medicines for relieving pain via vein, presently multimodal analgesia based on nerve block in perioperative period of lower extremity joint arthroplasty is recommended [1]. In recent years, the use of CFNB is becoming increasingly wider benefits from its simple operation and explicit analgesic effect. International experience of continuous nerve block is normally accomplished through the nerve block needle produced by B. Braun Melsungen AG or Pajunk Medical Produkte and indwelling catheter for continuous analgesia. But the operation is quite complex because the location needs a nerve stimulator or B ultrasound for guidance [2,3]. We adopted a specially designed needle-over-cannula which is one of our patent products (Figure 1) (The Patent of P.R.C No: 200820152063.9 and 200920166821.7) and has more simple operation for CFNB. Its simple operation and effective analgesia has been proved by clinical research [4]. This study aimed to compare different locating methods of the indwelling cannula for CFNB in geriatric lower extremity joint arthroplasty.
Figure 1.
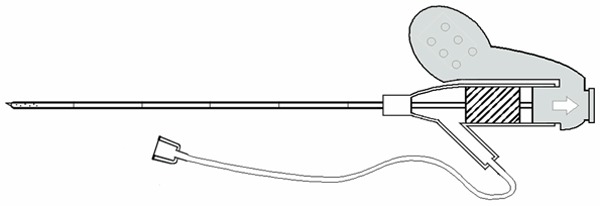
Specially designed needle-over-cannula for continuous femoral nerve block.
Patients and methods
This study has been approved by the Research Ethics Board of Tongji Hospital of Tongji University.
Patient enrollment
Sixty elderly patients aged over 65 years, ASA I-III, who intended to receive scheduled knee or hip replacement surgery were recruited and divided into 3 groups by means of random number table. Group 1 (n=20) adopted fascial pop for CFNB, Group 2 (n=20) adopted location guided by B ultrasound and Group 3 (n=20) adopted fascial pop combined with ultrasound guidance. The serial numbers of each group were sealed into opaque envelopes. Informed consent was obtained prior to enrollment from each patient. Patients, who were allergic to amides local anesthetics had dysfunction of heart, lung, liver or kidney and had irritability or abuse of opioid medicine, were eliminated. The anesthesia were all completed by the same anesthetist and the hip joint replacement all adopted posterior-lateral approach.
Anesthetic procedures
Preoperative fasting was required for 8 hours and then patients received preoperative sedation through atropine (0.5 mg) and Phenobarbital (0.1 g) given by intramuscular injection 30 minutes before anesthesia. In the operation room, the patients received routine noninvasive monitoring of blood pressure, pulse, oxygen saturation and electrocardiograph (ECG). Moreover, oxygen was delivered at 2L/min while access to the median cubital vein was established. Dexmedetomidine was given to achieve sedation through intravenous infusion with syringe pump and the pump speed was regulated from 1 ug/kg/h to 0.3 ug/kg/h after 10-minute infusion. At the same time, lower limb on affected side received nerve block. The locating point of fascial pop was 2 cm below inguinal ligament and 1.5 cm outward femoral pulse. After sterilizing and draping, 1% Lidocaine 1 ml was infused at puncture point for local anesthesia. Then the needle was inserted by the right hand at an angle of 45° in direction of the long axis of body with the needle point toward the side of head (Figure 2). 0.5% Ropivacaine 30 ml was infused through the side cannula of the puncture needle after feeling sense of pop twice (fascia lata and fascia iliaca). Then the needle was put down about 10° gently and the cannula was advanced by 3-4 cm. The plunger of the syringe was drawn to ensure there was no blood blew or no resistance to infuse medicine and fix the external cannula to the skin with no-pressure medical tape (Figure 3). When the surgery was finished, analgesia pump was connected to the cannula for postoperative analgesia. The long axis of ultrasonic probe was placed below the midpoint of inguinal ligament and needle outward femoral nerve was inserted under direct vision (Figure 4). If the position of needle point is uncertain, we could infuse a small amount of liquid test. 0.5% Ropivacaine 30 ml was infused at the exact position and the other operation was same as the former. The steps of fascial pop combined with ultrasound guidance location were as follows: Locate with fascial pop in advance and place ultrasonic probe above the needle. The external indwelling cannula can also be placed in long axis out-of-plane guided by ultrasound. The local anesthetics of three groups were all 0.5% Ropivacaine 30 ml. The lap skin on affected side was pricked to measure sense 10 minutes later and satisfied anesthetic was achieved if there was no sense of pain. Trachea intubation and general anesthesia were combined with Propofol, Sevoflurane and Dexmedetomidine. When surgery was finished, all patients received patient-controlled analgesia (PCA) through the indwelling external cannula.
Figure 2.

Continuous femoral nerve block with location of fascial pop.
Figure 3.

Continuous femoral nerve block with indwelling cannula for postoperative analgesia.
Figure 4.

Continuous femoral nerve block with location of fascial pop and ultrasound guiding.
The analgesic consisted of 60 ml of 1% ropivacaine, Sufentanil 50 ug in 300 ml of normal saline: a loading dose was 20 ml, followed by continuous infusion at a rate of 6 ml/h and a bolus injection of 4 ml within 20 min. Before the surgery was over, the patient was infused with 40 mg of Parecoxib sodium, 0.3 mg of Ramosetron for preventing vomiting, and 5 mg of Dexamethasone intravenously. The outcome measurements included single attempt success and average performing time (placement indwelling cannula), postoperative VAS score (quiet/active), severe intoxication, analgesic effect, incidence of nausea and vomiting, infection at the puncture site, nerve injury related complication, cannula occlusion and slipping , average duration of PCA use and patient’s satisfaction. The analgesic outcomes were assessed with VAS after surgery as follows: 0-2, no or mild pain; 3-6, moderate but tolerable pain; 7-10, severe and intolerable pain. Analgesia with no more than 3 was efficacious analgesia. The Ramsay Sedation Scale (RSS) was used to assess the sedation as follows: 0, sober; 1, occasional somnolence but easy to wake up; 2, frequent somnolence but easy to wake up; 3, lethargic and difficult to wake up. Respiratory depression is identified when the respiratory rate is below 8 per minute. Patients’ satisfaction was determined using a 10-point scale, with 0 being the least satisfied and 10 being the most satisfied. The anesthesia performing was completed by one anesthetist and postoperative visiting was performed by another anesthetist.
Statistical analysis
To analyze most measurements in this study, descriptive statistics were applied. Fisher’s exact test was used to analyze the enumeration data. The quantitative data were expressed as means ± standard deviation. Descriptive P<0.05 was considered statistically significant.
Results
Surgery type contains knee or hip replacement. Age, weight, sex, ASA grading, surgery and surgery time of each patient were all recorded (Table 1). Single placement was achieved successfully in 15 patients (75%) in group 1, 18 patients (90%) in both group 2 and group 3. Postoperative visiting was performed at 6, 12, 24 and 48 h (Table 2). The VAS score of 60 patients were all below 3 when quiet and there were a part of patients who got a score over 3 when active. There was no significant difference among three groups about above points. According to statistics, all the patients got RSS of 0 on average, with no nausea or vomiting, no cannula occlusion and slipping, or toxic reaction of local anesthetics. There was only one patient who pulled out the cannula unintentionally during sleeping. The cannula was indwelled more than 40 hours on average in three groups and the degree of patients’ satisfaction was all over 9.4. There was no significant difference among three groups. No respiratory depression or infection at the puncture site was found. There was only one patient in group 2 who felt mild pains in front of the thigh after removing the indwelling cannula nevertheless no abnormal condition was found by X-ray and nerve electrophysiology examination. It is worth noting that patients’ BP all dropped about 20 percent 1.5 hour after the beginning of operation.
Table 1.
The general condition of patients (X̅±s)
| Group | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Number (n) | 20 | 20 | 20 |
| Sex (M/F) | 10/10 | 9/11 | 12/8 |
| Age (Y) | 78±7.3 | 77±7.4 | 77±7.1 |
| Weight (kg) | 62±7.1 | 59±7.0 | 61±7.1 |
| Operation time (min) | 108±41 | 112±43 | 105±39 |
| Operation type (K/H) | 8/12 | 10/10 | 11/9 |
| ASA | 1.8±0.6 | 1.7±0.6 | 1.9±0.7 |
Table 2.
Postoperative follow-up visit conditions
| Group | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| Performing time (min) | 3.1±0.4 | 4.9±0.7 | 3.5±0.5 |
| Success rate of single attempt (Y/N) | 15/5 | 18/2 | 18/2 |
| Effective rate of postoperative analgesia (R/A) | 100/90 | 100/95 | 100/95 |
| RSS | 0 | 0 | 0 |
| Nausea and Vomiting | 1/0 | 0/0 | 1/0 |
| Cannula occlusion | 0/20 | 0/20 | 0/20 |
| Cannula slipping | 1/19 | 0/20 | 0/20 |
| Infection at puncture site | 0 | 0 | 0 |
| Indwelling time of cannula (hour) | 43.4±3.0 | 42.2±7.9 | 42.5±8.0 |
| Nerve injury related complication | 0 | 0 | 0 |
| Local anesthetics related toxicity | 0/20 | 0/20 | 0/20 |
| Urinary retention | 0 | 0 | 0 |
| Patient satisfaction (0~10 points) | 9.5±0.7 | 9.4±0.7 | 9.4±0.8 |
Discussion
Patients always feel obvious pain after lower extremity joint operation especially total knee replacement. It has been reported that 86% of patients could feel pain over moderate two weeks after knee or hip replacement surgery [5,6]. Intravenous or spinal analgesia are adopted traditionally for postoperative analgesia after lower extremity joint arthroplasty. The use of venous opioid medicines has been reduced because the untoward effect and side effect of venous opioid medicines appear frequently especially for elder patients who have preoperative cardiopulmonary comorbidities [7,8]. In order to prevent postoperative deep venous thrombosis, anticoagulant therapy is used ordinarily. Thus epidural analgesia is not recommended because of potential risk of epidural hematoma or other complications [9,10]. In 2014, Multiple methods based on nerve block and multi-mode analgesia were recommend by American anesthesia and orthopedics experts for analgesia in perioperative period of hip or knee replacement arthroplasty [1]. In recent years many clinical practices have proved that nerve block has definite analgesic effect to hip or knee replacement surgery thus the use of CFNB (3 in 1) is becoming increasingly wider for lower extremity joint arthroplasty [11].
Tuohy needle or Contiplex (r) A/Contiplex (r) D often use the continuous nerve block suite produced by B. Braun Melsungen AG or Pajunk Medical Produkte. Sometimes clinical application cannot get a satisfactory analgesic effect and even cause serious complications because of difficult placement of the soft internal indwelling catheter and shifting of cannula cusp [12]. Our study adopted a patent needle-over-cannula which has proprietary intellectual property right [4]. The external indwelling cannula is a specially designed needle-over-cannula and gets a quite blunt needle point. The advantage of this design is that we can feel the tunica vaginalis around nerve via the needle, meanwhile the direct damage to nerve can be reduced. After the needle got the right place, we should infuse enough liquids to form a potential gap to leave the external cannula (the cannula made from polyurethane has a good histocompatibility and has several side apertures in the leading end to ensure unimpeded liquid infusion) which can be detected by ultrasound. Postoperative analgesia is achieved by infusing local anesthetics through external indwelling cannula. The superiority of needle-over-cannula is brought into full play especially in the operation guided by ultrasound in short axis out-of-plane. The result of experiment showed that there was no significant difference among three location methods in terms of postoperative analgesic effect, untoward effect, complication, duration time of cannula and patient’s satisfaction in geriatric lower extremity joint arthroplasty adopting needle-over-cannula. Even though the nerve block adopting fascial pop is easy to handle, the success is closely related to operator’s proficiency of this method and anatomy knowledges. Femoral nerve is located outside of arteria cruralis, below fascia lata and fascia iliaca and has flat spindle structure. The operator can feel sense of pop twice when adopting fascial pop and the first sense is more obvious than the second one. Because of different fascia thicknesses in different patients, each operator could not have the same sense, thus the success rate of single attempt was only 75%. Placement of cannula is easier to complete if we block nerve guided by ultrasound in short axis out-of-plane as the indwelling cannula is parallel to the long axis of nerve. The disadvantage of this method is that the position of needle point cannot be observed obviously and nerve may be injured. It has been proved in our result that we have to confirm the position of needle point by infusing small amount of liquid constantly when puncturing, and it increases the operation time. It is also proved that the most recommendable method is fascial pop combined with ultrasound guidance in continuous nerve block using this needle-over-cannula. So both advantages of needle-over-cannula and B ultrasound guidance can be used better into application and nerve injury can be decreased. Meanwhile the placement is easier to complete and the performing time can be shortened.
There are still limitations in this study: the sample size is relatively small, and there may be deviation in statistics. In order to show the resistance change of fascial pop objectively, we can measure the resistance change of needle inserting. The nerve block needle with cannula beneficial for ultrasound developing has already been on trial and we hope it can apply to clinical patients in the near future.
Disclosure of conflict of interest
None.
References
- 1.Barrington JW, Halaszynski TM, Sinatra RS Expert Working Group On Anesthesia And Orthopaedics Critical Issues In Hip And Knee Replacement Arthroplasty FT. Perioperative pain management in hip and knee replacement surgery. Am J Orthop (Belle Mead NJ) 2014;43:S1–S16. [PubMed] [Google Scholar]
- 2.Borgeat A, Dullenkopf A, Ekatodramis G, Nagy L. Evaluation of the lateral modified approach for continuous interscalene block after shoulder surgery. Anesthesiology. 2003;99:436–442. doi: 10.1097/00000542-200308000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Mariano ER, Afra R, Loland VJ, Sandhu NS, Bellars RH, Bishop ML, Cheng GS, Choy LP, Maldonado RC, Ilfeld BM. Continuous interscalene brachial plexus block via an ultrasound-guided posterior approach: a randomized, triple-masked, placebo-controlled study. Anesth Analg. 2009;108:1688–1694. doi: 10.1213/ane.0b013e318199dc86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu B, Zhang X, Sun P, Xie S, Pang Q. Non-stimulation needle with external indwelling cannula for brachial plexus block and pain management in 62 patients undergoing upper-limb surgery. Int J Med Sci. 2012;9:766–771. doi: 10.7150/ijms.5007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warfield CA, Kahn CH. Acute pain management. Programs in U.S. hospitals and experiences and attitudes among U.S. adults. Anesthesiology. 1995;83:1090–1094. doi: 10.1097/00000542-199511000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534–540. doi: 10.1213/01.ANE.0000068822.10113.9E. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine Committee on Advancing Pain Research Council and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US) and National Academy of Sciences; 2011. The National Academies Collection: Reports funded by National Institutes of Health. [PubMed] [Google Scholar]
- 8.Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse events associated with postoperative opioid analgesia: a systematic review. J Pain. 2002;3:159–180. doi: 10.1054/jpai.2002.123652. [DOI] [PubMed] [Google Scholar]
- 9.Rawal N. Epidural technique for postoperative pain: gold standard no more? Reg Anesth Pain Med. 2012;37:310–317. doi: 10.1097/AAP.0b013e31825735c6. [DOI] [PubMed] [Google Scholar]
- 10.Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990-1999. Anesthesiology. 2004;101:950–959. doi: 10.1097/00000542-200410000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Richman JM, Liu SS, Courpas G, Wong R, Rowlingson AJ, McGready J, Cohen SR, Wu CL. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg. 2006;102:248–257. doi: 10.1213/01.ANE.0000181289.09675.7D. [DOI] [PubMed] [Google Scholar]
- 12.Yanovski B, Gaitini L, Volodarski D, Ben-David B. Catastrophic complication of an interscalene catheter for continuous peripheral nerve block analgesia. Anaesthesia. 2012;67:1166–1169. doi: 10.1111/j.1365-2044.2012.07222.x. [DOI] [PubMed] [Google Scholar]


