Abstract
Background: Syphilitic chorioretinitis can produce severe vision loss. However, the clinical manifestations of syphilitic chorioretinitis are still unclear, particularly during different stages. Herein, we will present our diagnostic technique for syphilitic chorioretinitis. Methods: This retrospective study recruited 109 cases; we performed a clinical evaluation including case history, serology analysis, fundus photography, fluorescein fundus angiography with or without indocyanine green angiography, auto-fluorescence, and optical coherence tomography. Results: 109 were diagnosed with acute syphilitic posterior placoid chorioretinitis by fundus photograph that revealed filthy, yellowish-white lesions. For autofluorescence, during early-stage syphilitic chorioretinitis, hyperfluorescence could be observed. During the convalescence stage, the fluorescence became hypofluorescence or disappeared. Fluorescein fundus angiography indicated early-stage transmitted fluorescence or hypofluorescence. During the venous stage, the lesion area had fluorescent leakage, mostly accompanied by retinal vasculitis. During the late stage, speckle staining was observed with optic disc fluorescence. Hypofluorescence or undistinguishable fluorescence was seen at an early stage with indocyanine green angiography. At an advanced stage, the lesion had obvious hypofluorescence. Optical coherence tomography indicated various inner segment/outer segment damage, accompanied by retinal pigment epithelium impairment. The inner segment/outer segment alteration could be lessened with treatment. Conclusions: The clinical manifestations of syphilitic chorioretinitis include impaired vision, shadow blocking, or photopsia of one or both eyes. Fundus photography, fluorescein fundus angiography with or without indocyanine green angiography, autofluorescence, and optical coherence tomography could be useful accessory examinations. Autofluorescence and optical coherence tomography could be the main examinations for monitoring disease progression.
Keywords: Syphilitic chorioretinitis, fluorescein fundus angiography, indocyanine green angiography, optical coherence tomography, autofluorescence
Introduction
Syphilis was recognized as one of the common causes of intraocular inflammation [1]. Ocular syphilis is becoming an increasingly common clinical problem, reflecting the growing incidence of syphilis in immunocompetent patients of all ages and in particular, patients with human immunodeficiency virus (HIV) [2,3]. Eye infections can occur at any stage of this disease and include interstitial keratitis; anterior, intermediate, and posterior uveitis; chorioretinitis; retinitis; retinal vasculitis; and cranial nerve and optic neuropathies [4,5]. Syphilitic chorioretinitis could produce severe vision loss [6]. However, few reports have systematically listed the clinical manifestations of syphilitic chorioretinitis at different stages. Herein, we will present our evaluation and analysis of the clinical features and ophthalmologic findings of syphilitic chorioretinitis in 109 patients.
Methods
One hundred nine patients with a diagnosis of syphilitic chorioretinitis were recruited from June 2008 to August 2013 in the Ophthalmology Department of The second hospital of Jilin University. The clinical data were analyzed, including gender, age, case history, serology analysis, fundus photography, fluorescein fundus angiography (FFA) with or without indocyanine green angiography (ICGA), autofluorescence (AF), and optical coherence tomography (OCT).
Case 1
A 56-year-old man complained of right eye blurry vision that had persisted for 8 days. His best-corrected visual acuity (BCVA) was 0.2 for the right eye and 1.0 for the left eye. The anterior segment of both eyes was normal. There were some inflammatory cells in the vitreous of the right eye. In the macula, some filthy yellowish-white lesions were observed (Figure 1A). FFA revealed slight transmitted fluorescence in the macula after the first 23 s, and the optic disc boundary was obscured (Figure 1C). At 1 min and 14 s, fluorescent leakage was observed from the lesion; distended segmental vein leakage fluorescence and optic disc leakage were observed (Figure 1D). At 12 min and 16 s, the optic disc lesion had fluorescence (Figure 1E). The blood investigation indicated positive treponema pallidum antibody (TP) and a rapid plasma reagin test (RPR) of 1:128. After antisyphilitic treatment for 3 months, the BCVA was 0.8 for the right eye, with an RPR of 1:4. The yellowish-white lesions had vanished. Meanwhile, FFA demonstrated slight transmitted fluorescence in the macula (Figure 1F).
Figure 1.
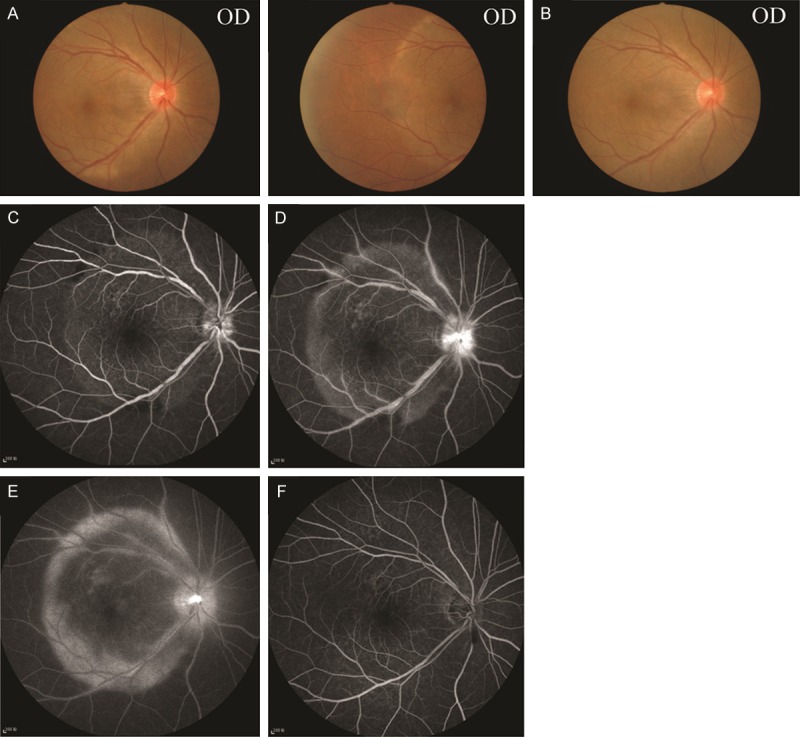
The fundus of case 1 with FFA. A. The fundus had filthy yellowish-white lesions on the macula before treatment. B. After antisyphilitic treatment, the fundus returned to normal. C. Early-stage FFA indicated slight transmitted fluorescence in the macula and an obscure optic disc boundary. D. At 1 min and 14 s, FFA demonstrated fluorescent leakage and distended segmental vein leakage fluorescence and optic disc leakage. E. During the late stage, the optic disc lesion had fluorescence. F. FFA demonstrated slight transmitted fluorescence in the macula.
Case 2
A 54-year-old female presented with a 10-day history of a shadow in her left eye. The BCVA was 1.0 for the right eye and 0.6 for the left eye. Yellowish-white lesions were in the macula of the left eye (Figure 2B), while the posterior of the right eye was normal (Figure 2A). The blood investigation revealed a positive treponema pallidum hemagglutination assay (TPPA) and an RPR of 1:64. An FFA with ICGA was conducted. At 2 min and 27 s, there was slight fluorescent leakage of the optic disc in the right eye, and the superior retinal artery was slightly dilated, while the peripheral vessel near the optic disc had fluorescent leakage. ICGA for choroidal fluorescence was normal (Figure 2C). At 30 min and 49 s, with FFA, the macula and the superior-temporal aspect of the retina had fluorescence. The macula and superior choroid had hypofluorescence (Figure 2D). As for the left eye, after the first 18 s, the FFA was normal. Further, with ICGA, the macula had a slightly lower fluorescence. At 33 min and 42 s, the macula had fluorescence with FFA, while the choroid had hypofluorescence with ICGA (Figure 2E). This case indicated that ICGA could be used to investigate lesions and could supply important information for diagnosis.
Figure 2.

IGCA and FFA for case 2. A. The fundus of the right eye was normal. B. The fundus of the left eye had a yellowish-white lesion on the macula. C. FFA showed slight fluorescent leakage of the optic disc; the retinal vasculature in the superior-temporal sector was slightly dilated, and the peripheral vessel near the optic disc had fluorescent leakage. ICGA of the choroid had normal fluorescence. D. Fluorescence was observed in the macula and superior-temporal aspect of the retina with FFA. The macula and superior choroid had hypofluorescence. E. During the early stage, the choroid had fluorescence, while the macula had a slightly lower degree of fluorescence. During the late stage, the macula had fluorescence with FFA, with obvious choroid hypofluorescence with ICGA.
Case 3-1
A 39-year-old female complained of right eye blurry vision that had lasted for 10 days. The BCVA was 0.5 for the right eye and 1.0 for the left eye. The RPR was 1:32. The fundus results revealed a partially depigmented lesion on the superior macula. OCT suggested that the inner segment and outer segment (IS/OS) were irregular on the macula, while some part was lost (Figure 3A). After antisyphilitic treatment for 2 weeks, the BCVA of both eyes was 1.0. However, the patient still experienced blurry vision in her right eye. The OCT results indicated that her eye had returned to normal (Figure 3B).
Figure 3.

OCT for case 3-1 and ERG for case 3-2. A. The IS/OS was irregular in the macula, while some part was lost in case 3-1. B. After antisyphilitic treatment for 2 weeks, the OCT examination was normal. The fundus of the left eye had a yellowish-white lesion on the macula. C, E. OCT indicated cystoid macular edema in both eyes, while the IS/OS was obscure, especially in the left eye. D, F. After antisyphilitic treatment for 7 months, the IS/OS of the surrounding retina was obscure. Other examinations were normal. G. EGR indicated that the rod response was low, and the wave was almost gone.
Case 3-2
A 24-year-old man presented with decreased vision for 2 months. The BCVA was 0.1 for the right eye and 0.3 for the left eye. The fundus of both eyes had a yellowish lesion, and the left eye had macular edema. The TPPA was positive, while the RPR was 1:32. This case was diagnosed with syphilitic chorioretinitis after FFA and ICGA examinations. OCT demonstrated cystoid macular edema in both eyes, and the IS/OS was obscure, especially in the left eye (Figure 3C, 3E). After antisyphilitic treatment for 7 months, the IS/OS on the macula could be clearly seen with OCT; however, the IS/OS of the surrounding retina was still obscure. The BCVA was 0.6 for the right eye and 1.0 for the left eye (Figure 3D, 3F). The patient’s visual acuity improved, but he still had poor vision in the dark. Thus, we obtained a full-field ERG. The results suggested that the rod response was low, while the wave was almost eliminated (Figure 3G). However, this case was not consistent with the previous case reported by S.R. Menon [7] that indicated the absence of an early rod response, which completely recovered upon restoration.
Case 4
A 33-year-old female complained of flashing in her left eye for 3 days. The BCVA was 1.0 for the right eye, while it was 0.2 for the left eye, with an RPR of 1:8. The posterior fundus had yellowish-white lesions (Figure 4A). FFA and ICGA examinations suggested slight transmitted fluorescence at an early stage, with fluorescent leakage at the venous stage; FFA demonstrated retinal and optic disc late-stage fluorescence. ICGA demonstrated that the posterior choroid had hypofluorescence at an early stage that was more significant at a late stage (Figure 4B, 4C). As for AF, the posterior had strong AF, and the superior macula had spotty AF (Figure 4D). After antisyphilitic treatment for 8 months, the patient had a BCVA of 1.0 for both eyes and a normal fundus (Figure 4E). An additional FFA examination revealed slight transmitted fluorescence on the macula and superior retina (Figure 4F). With AF, the lesion turned into mottled hypo-AF (Figure 4G), suggesting that the RPE was impaired after inflammation.
Figure 4.

FFA with ICGA and AF for case 4. A. The fundus had posterior yellowish-white lesions. B, C. During the early stage, slight transmitted fluorescence and fluorescent leakage were observed, while during the venous stage, the retina and optic disc had fluorescence at a later stage with FFA. ICGA indicated that the posterior choroid had hypofluorescence during the early stage that was more significant during the late stage. D. The posterior aspect had strong AF, with spotty AF on the superior macula. E. The fundus was normal. F. With AF, the lesion turned into mottled hypo-AF after treatment. G. FFA indicated slight transmitted fluorescence on the macula and superior retina after treatment.
Results
Of all 109 cases (167 eyes), 51 cases had affected sigle eye, while 58 cases had both eyes affected. For 62 cases, 47 cases (43.1%) were female, while 62 cases (56.9%) were male. The youngest patient was 24 years old, while the oldest was 79 years old (average age, 51.36 y). All patients had immune examinations including hepatitis B virus surface antigen and antibody (HBsAg and HBsAb), hepatitis C virus antibody (HCVAb), HIV, and treponema pallidum antibody (TP). One hundred and nine cases had a positive TP test, while 3 cases were HIV positive. All patients were diagnosed with syphilitic chorioretinitis, of which 1 case was diagnosed with neurosyphilis by lumbar puncture (Table 1). The rapid plasma reagent for syphilis was 1:2-128. After diagnosis, all the patients were given antisyphilitic treatments (first, penicillin or cefdinir was administered orally, followed by a tardocillin intramuscular injection of 120 million units bilaterally, once a week). The patients complained of vision loss, shade of visual field or photopsia. The time of visiting from 3 days to 3 years and follow-up of 7 days to 8 months, the patients’ vision acuity was the range of hand movement to 1.0.
Table 1.
Demographic and clinical data of patients with syphilitic posterior placoid chorioretinitis
| Age | Total number | Gender F/M | FFA with or without ICGA (n) | RPR (n) |
|---|---|---|---|---|
| 25-44 | 27 | 15/12 | FFA (17) | ≥ 64 (7) |
| FFA + ICGA (10) | 32-64 (8) | |||
| ≤ 32 (9) | ||||
| HIV+(1) | ||||
| 45-55 | 45 | 20/25 | FFA (19) | ≥ 64 (21) |
| FFA + ICGA (26) | 32-64 (6) | |||
| ≤ 32 (13) | ||||
| HIV+(1) | ||||
| > 55 | 37 | 17/25 | FFA (20) | ≥ 64 (18) |
| FFA + ICGA (17) | 32-64 (10) | |||
| ≤ 32 (6) | ||||
| HIV+(1) CSF+(1) |
Of 54 patients who had FFA and 53 patients who had an FFA combined with ICGA, early-transmitted fluorescence was demonstrated in 97 eyes or hypofluorescence was demonstrated in 8 eyes. During venous metaphase, fluorescent leakage was found, combined with retinal vasculitis in 118 eyes, with slight venous circuity and segmental dilated leakage in 64 eyes and venous leakage only without other vessel alterations in 54 eyes. During late-stage fluorescence, fluorescence speckle with optic disc dyeing was observed in 129 eyes (Table 2A). During early-stage ICGA, 30 eyes had slight hypofluorescence, while 39 eyes had obvious hypofluorescence. With venous metaphase, sustained hypofluorescence and late-stage diffuse hypofluoresence was observed in the entire affected area (Table 2B). Thirty-two eyes were able to have OCT. Examinations of the affected macular cases indicated that the IS/OS had vanished in 14 eyes combined with retina pigment epithelium (RPE) atrophy in 7 eyes. The IS/OS layer was nonsequential (partially disappeared) in 31 eyes, accompanied by cystoid macular edema in 7 eyes, a macular epiretinal membrane in 3 eyes, neural epithelium macular detachment in 5 eyes, and retinal pigment epithelium detachment in 1 eye (Table 3). For 79 cases, the AF results for 86 eyes indicated hyperfluorescence, while 11 eyes had high or low fluorescence and 19 eyes had blurry fluorescence because of vitreous opacification (Table 4).
Table 2A.
FFA of syphilitic posterior placoid chorioretinitis
| FFA stage | Clinical manifestations |
|---|---|
| Early stage | Transmitted fluorescence: 97 eyes |
| Hypofluorescence: 8 eyes | |
| Venous metaphase | With reinal vasculitis: 118 eyes |
| Only venous leakage without other vessels alterations: 54 eyes | |
| With slight venous circuity or segmental dilated leakage: 64 eyes | |
| Late stage | Fluorescence speckle with optic disc dyeing: 129 eyes |
Table 2B.
ICGA of syphilitic posterior placoid chorioretinitis
| FFA stage | Clinical manifestations |
|---|---|
| Early stage | Slight hypofluorescence: 30 eyes |
| Obvious hypofluorescence: 39 eyes | |
| Venous metaphase | Sustained hypofluorescence |
| Late stage | Diffuse hypofluorescence in the entire affected area |
Table 3.
OCT of syphilitic posterior placoid chorioretinitis
| OCT | Number of eyes |
|---|---|
| IS/OS defect | 14 |
| With RPE atrophy | 7 |
| IS/OS nonsequential | 31 |
| With cystoid macular edema | 7 |
| With neural epithelium and macular detachment | 5 |
| With RPE detachment | 1 |
Table 4.
Autofluorescence of syphilitic posterior placoid chorioretinitis
| AF | Number of eyes |
|---|---|
| Hyperfluorescence | 86 |
| High or low fluorescence | 11 |
| Blurry fluorescence | 19 |
Discussion
Syphilis is caused by the spirochete bacterium treponema pallidum subspecies pallidum [8,9]. And its prevalence increases. Ocular syphilis can involve any or all of these structures. Inflammatory changes in the choroid, as well as in the retina, are also common in syphilitic posterior uveitis. Manifestations of ocular syphilis are manifold [10,11]. So in our study, we summarized 109 cases to establish a typical diagnosis progress for acute syphilitic posterior placoid chorioretinitis (ASPPC).
The sexuality in our study suggested that male was more than female. The ages of patients were from 40 to 60 which occupied almost 68.8% and this maybe associated with social factors. The visit time was within 30 days for almost 65.6% of all patients, which may be because that ASPPC affected vision obviously, so that patients would come as early as possible.
Fundus: 109 cases (167 eyes) were taken fundus photography. For those cases with short history, the vitreous was without or with little inflammatory cells. The fundus showed filth yellowish white lesion. For the long history cases, the vitreous opacification was obvious, bounds of the lesions were obscure and the retina was filth and lost gloss. The lesions were called as acute syphilitic posterior placoid chorioretinitis (ASPPC) defined by Gass at 1990 [12]. Lesions of 56 eyes were only limited on the posterior pole, and had clear bounds .Lesions of 111 eyes affected both macular and other quadrant. Here in our report, lesions of all patients affected macular and that was probably because of the redundant circulation of macular.
FFA and ICGA: in our study, 59.5% of all cases which received FFA presented transmitted fluorescence which suggested the lesion impaired on RPE. 72.4% cases also had retinal vasculitis and 79.1% had optic disc dyeing at the late stage. For ICGA, all cases showed not typical hypofluorescence at early stage, however, at late stage the hypofluorescence was significant. That’s maybe because that the great vessel angioplerosis at early stage and later fluorescence lower as the dyeing in great vessel decreasing, so that the lesion bound was clear. ICGA suggested that lesion of ASPPC was focused on choroid [13]. RPE impairment and vasculitis were secondary. The hypofluorescence may cause by inflammation infiltration, or choroidcapillary blockage or both effects [14]. Some reports considered the ASPPC as inflammation of choroid stromatic and the sustained hypofluorescence suggested the impairment of all choroid stromatic. 30 eyes hypofluorescence obviously at late stage while not significant at early suggested that these cases affected the superficial choroidcapillary. Other 39 eyes could be observed hypofluorescence at early stage showed those cases may affect both great vessel and capillary of choroid.
OCT: the impairment of IS/OS of all the patients in our study were recovered during treatment. And prognosis of vision improved. OCT of some cases with RPE atrophy did not recover and bad vision prognosis. It could be concluded that ASPPC was induced by immune that could affect the neural retina temporarily. If the lesions were structure impairment, OCT could not recover [15,16]. So OCT could be a Noninvasive examination for follow-up.
AF: AF is a index of RPE function. When inflammation being activited, the RPE metabolism function was abnormal and could result in the accumulation of fluorescence material [17]. So we could find out strong hyperfluorescence and low AF which suggested RPE degeneration and atrophy. AF could investigate inflammation of choroid response which presented a inflammation progress and RPE impairment. So that AF of SPPC consistent with the progress of inflammation and could monitor the change of SPPC. However, the limitation of AF was restricted by refracted medium. In our study, there were 19 eyes were not very clear for AF as vitreous opacification.
Conclusion
The clinical manifestations of syphilitic chorioretinitis include impaired vision, shadow-blocking, and photopsia for one or both eyes. The fundus had a yellowish-white lesion. At an early stage, hyperfluorescence might be apparent with AF; however, after recovery, no fluorescence or hypofluorescence was visible. With FFA, transmitted fluorescence or hypofluorescence was apparent early; during the venous period, fluorescent leakage was apparent with mostly retinal vasculitis; and at late stage, entire lesions were dyed, along with most of the optic disc. Hypofluorescence could be observed with ICGA at an early stage; however, later, the lesion had significant hypofluorescence. OCT suggested varied IS/OS impairment. Serious impairment could affect the RPE. OCT changes could revert if the cases recovered. Moreover, AF and OCT could be the main examinations for monitoring disease progression.
Acknowledgements
This research sponsored by JiLin Province Science and Technology Agency, NO. 3D511Y903429.
Disclosure of conflict of interest
None.
Abbreviations
- FFA
fluorescein fundus angiography
- ICGA
indocyanine green angiography
- AF
autofluorescence
- OCT
optical coherence tomography
- BCVA
best-corrected visual acuity
- RPR
rapid plasma reagin test
- IS/OS
inner segment and outer segment
- HBsAg
hepatitis B virus surface antigen
- HBsAb
hepatitis B virus surface antibod
- HCVAb
hepatitis C virus antibody
- HIV
human immunodeficiency virus
- TP
treponema pallidum antibody
- RPE
retina pigment epithelium
References
- 1.Janeiro S, Fernandes AM, Lopes P, Pedroso E. Secondary syphilis: a rare cause of nephrotic syndrome. BMJ Case Rep. 2014:2014. doi: 10.1136/bcr-2013-201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elshatory YM, Larson TA. Ocular syphilis. JAMA Ophthalmol. 2013;131:1219. doi: 10.1001/jamaophthalmol.2013.1614. [DOI] [PubMed] [Google Scholar]
- 3.Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433–441. doi: 10.1097/00055735-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Lee SB, Kim KS, Lee WK, Kim YJ, Kang MW. Ocular syphilis characterised by severe scleritis in a patient infected with hiv. Lancet Infect Dis. 2013;13:994. doi: 10.1016/S1473-3099(13)70198-1. [DOI] [PubMed] [Google Scholar]
- 5.Bonnin N, Laurichesse H, Beytout J, Mrozek N, Lesens O, Andre M, Aumaitre O, Bacin F, Romazko JP, Chiambaretta F. Ophthalmologists play a key role in the management of syphilis presenting with ocular involvement. Acta Ophthalmol. 2014;92:e328–329. doi: 10.1111/aos.12315. [DOI] [PubMed] [Google Scholar]
- 6.Pan SW, Yusof NS, Hitam WH, Noor RA, Embong Z. Syphilitic uveitis: Report of 3 cases. Int J Ophthalmol. 2010;3:361–364. doi: 10.3980/j.issn.2222-3959.2010.04.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menon SR, Fleischhauer J, Jost K, Helbig H. Clinical and electrophysiological course of acute syphilitic posterior placoid chorioretinitis. Klin Monbl Augenheilkd. 2005;222:261–263. doi: 10.1055/s-2005-857998. [DOI] [PubMed] [Google Scholar]
- 8.Lima BR, Mandelcorn ED, Bakshi N, Nussenblatt RB, Sen HN. Syphilitic outer retinopathy. Ocul Immunol Inflamm. 2014;22:4–8. doi: 10.3109/09273948.2013.841960. [DOI] [PubMed] [Google Scholar]
- 9.Baigalmaa J, Erdenechimeg C, Narantuya J, Bulbul A, Tugsjargal J, Dolgion E, Soyolmaa E, Enkhtuya M, Jugderjav B, Otgonsukh S. Increasing syphilis notifications in mongolia: Results from national surveillance for 2001-2011. Western Pac Surveill Response J. 2012;3:86–93. doi: 10.5365/WPSAR.2012.3.2.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joseph A, Rogers S, Browning A, Hall N, Barber C, Lotery A, Foley E, Amoaku WM. Syphilitic acute posterior placoid chorioretinitis in nonimmuno-compromised patients. Eye (Lond) 2007;21:1114–1119. doi: 10.1038/sj.eye.6702504. [DOI] [PubMed] [Google Scholar]
- 11.Veys MC, Lafaut B. Ocular syphilis, a case of acute posterior placoid chorioretinitis. Bull Soc Belge Ophtalmol. 2013:21–25. [PubMed] [Google Scholar]
- 12.Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97:1288–1297. doi: 10.1016/s0161-6420(90)32418-1. [DOI] [PubMed] [Google Scholar]
- 13.Baglivo E, Kapetanios A, Safran AB. Fluorescein and indocyanine green angiographic features in acute syphilitic macular placoid chorioretinitis. Can J Ophthalmol. 2003;38:401–405. doi: 10.1016/s0008-4182(03)80053-4. [DOI] [PubMed] [Google Scholar]
- 14.Teplinskaia LE, Kaliberdina AF, Zaitseva NS, Bulanova TD, Katsnel’son LA. [clinical-immunological disorders in uveitis in patients with behcet’s syndrome] . Vestn Oftalmol. 1994;110:23–25. [PubMed] [Google Scholar]
- 15.Nabholz N, Navarre S, Villain M. [spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis] . J Fr Ophtalmol. 2014;37:e53–56. doi: 10.1016/j.jfo.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Brito P, Penas S, Carneiro A, Palmares J, Reis FF. Spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis: The role of autoimmune response in pathogenesis. Case Rep Ophthalmol. 2011;2:39–44. doi: 10.1159/000324086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robson AG, Moreland JD, Pauleikhoff D, Morrissey T, Holder GE, Fitzke FW, Bird AC, van Kuijk FJ. Macular pigment density and distribution: Comparison of fundus autofluorescence with minimum motion photometry. Vision Res. 2003;43:1765–1775. doi: 10.1016/s0042-6989(03)00280-3. [DOI] [PubMed] [Google Scholar]


