Abstract
Background:
Iron-loaded cardiac complication is the essential cause of mortality in patients with thalassemia. Early detection and treatment of cardiac over-load can reduce mortality.
Objectives:
The current study aimed to evaluate the relationship between serum ferritin levels and T2* magnetic resonance imaging (MRI) of heart and liver and liver iron concentration (LIC) to diagnose iron over load in countries with limited access.
Patients and Methods:
In the current cross-sectional study, 85 Iranian patients with thalassemia with the mean age of 22.7 ± 7 years were randomly selected. All patients were on regular blood transfusion. Echocardiography of heart and liver T2* MRI, determination of serum ferritin levels, and LIC were performed in all subjects at the same time. The correlation of serum ferritin levels with T2*MRI of heart and liver, and LIC was assessed. P value < 0.05 was considered statistically significant.
Results:
Abnormal myocardial iron load (T2* MRI < 20 ms) was detected in 58% of the patients and among whom, 36% had severe myocardial iron load (T2* MRI < 10 ms). Median and interquartile range of serum ferritin levels were 1434 and 2702 respectively in patients with thalassemia. Serum ferritin levels showed a statistically significant positive correlation with LIC (rs = 0.718, P < 0.001) and significant negative correlation with T2* Heart (rs = -0.329, P = 0.002), and T2* Liver (rs = -0.698, P < 0.001). However, Ejection fraction was not significantly correlated with serum ferritin levels in the patients (P = 0.399).
Conclusions:
Serum ferritin levels can be used to diagnose iron over-load in patients with thalassemiaas an alternative method in areas where T2* MRI is not available.
Keywords: Beta-thalassemia, Ferritin, Magnetic Resonance Imaging, Liver, Heart
1. Background
Thalassemia, which is an inherited disorder, is associated with anemia caused by impaired synthesis of globin chain and has a range of complications such as extra medullary hematopoiesis, cardiac failure, arrhythmia, leg ulcer and gall stones (1-3). Cardiac failure, secondary to iron over-load, remains the essential cause of mortality in these patients (4, 5). Early diagnosis and precise measurement of myocardial iron deposition would allow better treatment and reduction of cardiac mortality. The principal methods of iron loading measurement are assessment of Liver Iron Concentration (LIC) and serum ferritin (6, 7). Also, non-invasing modalities are increasingly used as an alternative to biopsy and ferritin level assessment, although T2* Magnetic Resonance Imaging (MRI) is currently the gold standard approach (8, 9). However, T2* MRI is expensive, not widely available, and its interpretation needs an expert radiologist. The current study aimed to investigate the correlation of serum ferritin levels with LIC, T2* MRI of heart and liver inpatients with thalassemia.
2. Objectives
The current study aimed to detect whether the serum ferritin levels could be considered a reliable alternative test or not, also to evaluate cardiac function by echocardiography and investigate the association of systolic ejection fraction with iron over-load.
3. Patients and Methods
In the current cross sectional study, 90 patients with Thalassemia Major (TM) and Thalassemia Intermedia (TI) participated from January 2013 to January 2014 in Shiraz, Iran. All patients attended the thalassemia clinic located at the referral state hospital, the only referral hospital with 45 beds for such patients, in Southern Iran. Subject selection was based on systematic random sampling method from a sampling frame (about 720 patients with thalassemia) available at this center. List of the patients was reviewed and medical details including the drug and transfusion histories were obtained. Also, patients or their parents signed consent letters. The study was approved in the Medical Ethics Committee of Shiraz University of Medical Sciences (approval code: 3663 date: 92/9/3). The diagnosis of TM and TI in patients was based on complete blood count and hemoglobin electrophoresis tests, and clinical history evaluated by an expert hematologist. Inclusion criteria were patients with TM when the age of the first blood transfusion was less than two years old, and in patients with TI it was above two years old. All patients have been on regular blood transfusion. Patients with any infections, fever, or positive history of viral hepatitis during checking serum ferritin levels as well as overt heart and liver failure were excluded from the study. Finally five patients were excluded. Blood samples were obtained to assess fasting serum ferritin levels (electrofluorescentassay method, mini VIDAS machine, France) at the beginning of the study by calibrated equipments. All of the patients were assessed by T2* MRI of liver and heart (Zimmence, Germany, Avanta, 1.5 Tesla), echocardiography (GE VIVID 3, U.S.A, probe 3 MHz), and serum ferritin at the beginning of the research. Conventional echocardiography including the measurement of Ejection Fraction (EF) was done for each patient by an expert cardiologist. All radiographic findings were evaluated by one expert radiologist. According to the type of chelator therapy, patients were categorized into five groups: Group1, used only deferroxamine (Desferal, Novartis) 50 mg/kg/day; group 2 used combination therapy with deferiprone 75 mg/kg/day and deferoxamine 50 mg/kg/day, two days a week; group 3, used only deferasirox 20 - 40 mg/kg/day; group 4 used combination of deferasirox and deferroxamine, and group 5 did not receive any treatment. The duration of iron chelation therapy was at least six months before the study. Myocardial and hepaticiron loading and LIC were classified as normal, mild, moderate, and severe according to T2* MRI of heart and liver (Table 1).
Table 1. Classification of Hepatic and Cardiac iron Loading and Liver Iron Concentration a.
| Group | Cardiac T2* MRI | Hepatic T2* MRI | LIC |
|---|---|---|---|
| 1, Normal | > 20 | > 6.3 | < 2 |
| 2, Mild | 14 - 20 | 2.8 - 6.3 | 2 - 5 |
| 3, Moderate | 10 ≤ 14 | 1.4 - 2.7 | 5 - 10 |
| 4, Severe | < 10 | < 1.4 | < 10 |
aAbbreviations: LIC, Liver Iron Concentration.
3.1. Statistical Analysis
Data were analyzed by SPSS v. 17. Test of normality was done by Shapiro-Wilk test. Due to small sample size in subgroups exact methods were used (bootstrap and Monte Carlo) to report P values and confidence interval. Serum ferritin levels did not show normal distribution. Descriptive data were presented as mean, standard deviation, median, inter quartile range (IQR), and boxplots. Student t-test or Mann-Whitney test were used to compare quantitative variables between two groups, and Kruskal-Wallis test was used for the comparison among three or more groups of patients. Qualitative variables were compared by Chi-square test. Spearman correlation test was done to find the correlation between serum ferritin levels and values of T2* MRI and LIC. All tests considered two-sided and P values < 0.05 were considered statistically significant. Sample size calculation: Considering α = 0.05, power = 90% and correlation between serum ferritin levels and T2* MRI of liver: r = -0.44 (10), 49 patients with thalassemia were acceptable. Finally, 90 patients were enrolled for more accuracy, and five patients were excluded from the study.
4. Results
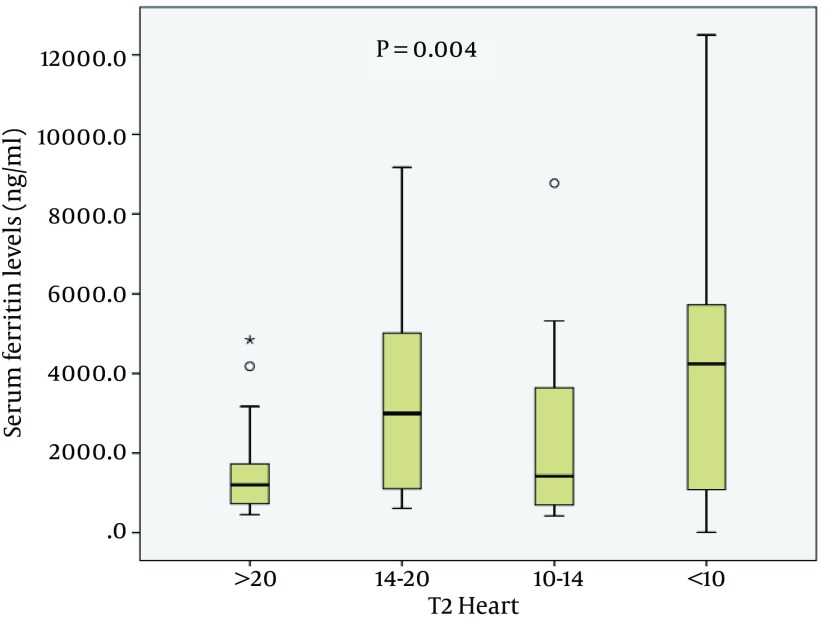
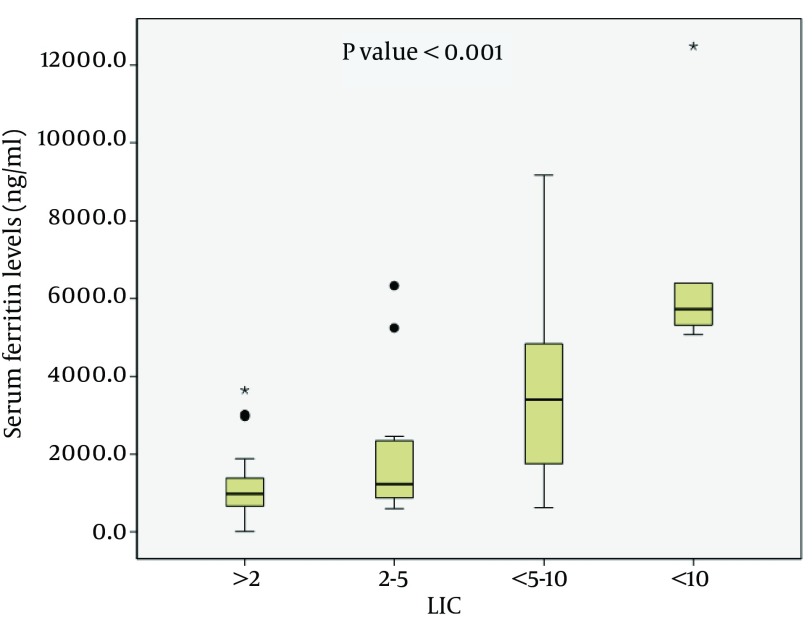
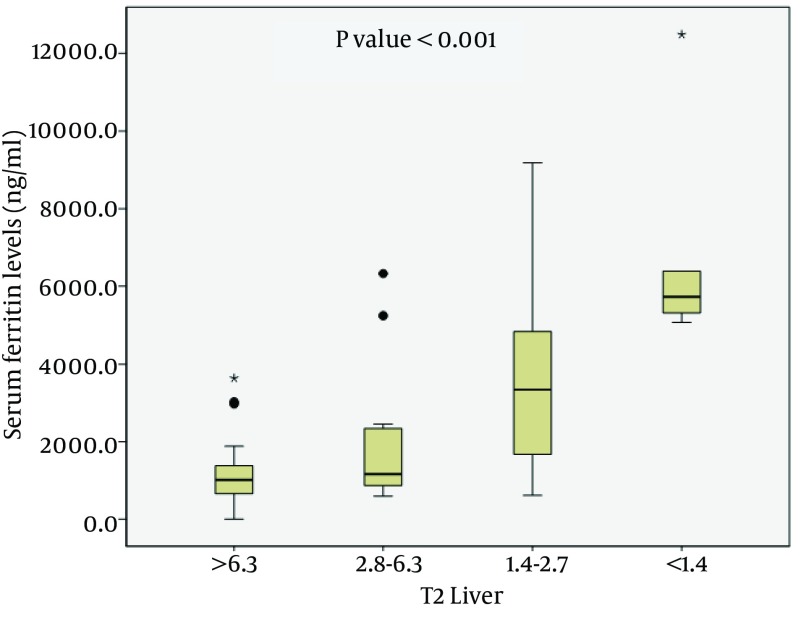
Patients with thalassemia consisted of 63, and 22 patients with TM, and TI respectively. The demographic and clinical features of patients with thalassemia are presented in Table 2. There are no statistically significant differences between the two groups of patients with thalassemia regarding gender, age, Body Mass Index (BMI) or serum ferritin levels (P > 0.05). Serum ferritin levels showed a statistically significant positive correlation with LIC (rs = 0.718, P < 0.001), and statistically significant negative correlation with T2* Heart (rs = -0.329, P = 0.002), and T2 Liver (rs = -0.698, P < 0.001), in patients with thalassemia (Table 3). However, Ejection fraction was not significantly correlated with serum ferritin levels in the patients (P = 0.399). Also, comparison results of serum ferritin levels among the four groups of patients with thalassemia based on T2 MRI heart and liver, and LIC are presented in Table 4 and Figures 1-3. Median serum ferritin levels were significantly associated with the values of T2* heart (P = 0.004) and T2 liver (P < 0.001), and LIC (P < 0.001). Abnormal myocardial iron load (T2* MRI < 20 ms) was detected in 58% of the patients among whom 36% had severe myocardial iron load (T2* MRI < 10 ms).
Table 2. Comparison of Demographic and Paraclinical Data Between the Two Groups of Patients With Thalassemia a.
| Group | Age, Mean ± SD | Bootstrap 95% CI | BMI, Mean ± SD | Bootstrap 95% CI | Ferritin, Median, IQR | Bootstrap 95% CI | Male/Female |
|---|---|---|---|---|---|---|---|
| Thalassemia major (n = 63) | 22.79 ± 7.1 | 21.06-24.65 | 21.15 ± 3.5 | 20.32-21.99 | 1700, 3428 | 1312-2970 | 30/33 |
| Thalassemia intermedia (n = 22) | 22.77 ± 6.2 | 20.24-25.17 | 21.13 ± 3.2 | 19.7-22.4 | 1094, 1119 | 935-1434 | 11/11 |
| Bootstrap P value | 0.994 | 0.974 | 0.085 | > 0.9999 |
aAbbreviations: IQR, Interquartile Range; CI, Confidence Interval.
Table 3. Correlation of Serum Ferritin Level With T2* MRI, liver Iron Concentration and Ejection Fraction in Patients With Thalassemia a.
| Variables | Values | Boot strap P Value |
|---|---|---|
| T2* MRI Heart | 0.002 b | |
| Correlation coefficient | -0.329 | |
| Bootstrap 95% CI | -0.532 - 0.122 | |
| T2* MRI Liver | ||
| Correlation coefficient | -0.698 | < 0.001 b |
| Bootstrap 95% CI | -0.804 - 0.545 | |
| LIC | < 0.001 b | |
| Correlation coefficient | + 0.718 | |
| Bootstrap 95% CI | 0.58 - 0.817 | |
| EF | 0.399 | |
| Correlation coefficient | +0.093 | |
| Bootstrap 95% CI | -0.116 - 0.294 |
aAbbreviations: LIC, liver iron concentration; EF, ejection fraction.
bStatistically significant.
Table 4. Comparison of Median of Serum Ferritin Levels Among Different Groups of Thalassemia Patients Based on T2 Heart, T2 Liver, and LICa.
| Serum Ferritin Median, IQR | Serum Ferritin Bootstrapped 95% CI for Median | Monte Carlo Significant | |
|---|---|---|---|
| T2 heart | 0.004b | ||
| > 20 (n = 35) | 1207, 1049 | 809 - 1434 | |
| 14-20 (n = 14) | 2995,4257 | 1403 - 5013 | |
| 10 ≤ 14 (n = 18) | 1425,3014 | 933 - 3232 | |
| < 10 (n = 18) | 4245,4846 | 1198 - 5520 | |
| T2 liver | |||
| > 6.3 (n = 35) | 1020, 743 | 699 - 1259 | |
| 2.8 - 6.3 (n = 15) | 1168, 1541 | 819 - 2319 | < 0.001b |
| 1.4 - 2.7 (n = 30) | 3345, 3267 | 2086 - 4304 | |
| < 1.4 (n = 5) | 5724, 4251 | 5072 - 12491 | |
| LIC | < 0.001b | ||
| < 2 (n = 35) | 976, 743 | 697 - 1257 | |
| 2 ≤ 5 (n = 16) | 1225, 1501 | 935 - 2319 | |
| 5-10 (n = 29) | 3397, 3212 | 2377 - 4304 | |
| > 10 (n = 5) | 5724, 4251 | 5072 - 12491 |
aAbbreviations: LIC, liver iron concentration; IQR, inter quartile range.
bStatistically significant.
Figure 1. Comparison of Serum Ferritin Levels Among the Four Groups of Patients With Thalassemia Regarding T2* MRI of Heart.
Figure 3. Comparison of Serum Ferritin Levels Among the Four Groups of Patients With Thalassemia Regarding LIC.
Figure 2. Comparison of Serum Ferritin Levels Among the Four Groups of Patients With Thalassemia Regarding T2* MRI of Liver.
5. Discussion
Cardiac problems such as heart failure and arrhythmias are the main cause of mortality in patients with thalassemia. Although, cardiac complications in patients with thalassemia are multifactorial, they are mainly related to iron loading toxicity (11, 12). The current study focused on whether the serum ferritin levels could be considered as a parameter to detect cardiac and liver iron loading in patients with thalassemia or not. On the other hand, there was a direct relationship between serum ferritin levels and T2* MRI of heart and liver. The obtained results showed strong correlation between T2* MRI of heart relaxation times and serum ferritin indicating that serum ferritin can estimate the cardiac iron loading. Other studies found different correlation strengths, ranging from no correlation to moderate correlation (13, 14). Also, a significant correlation between T2* MRI of liver and serum ferritin levels was observed in the current study. This is in line with the findings of the study by Zamani et al. who reported that serum ferritin is a good parameter to detect hepatic iron loading (15). In the literature, several studies showed significant relationship between serum ferritin and LIC. The findings of the current study were in accordance with these studies (16, 17). The current study did not find any statistically significant relationship between the ejection fraction and serum ferritin levels to predict the complications of iron loading. Butsome reports such as those of Montazare et al. and Bosi et al. demonstrated significant correlation between serum ferritin and left ventricular EF (18, 19). The current study was limited due to small sample size in subgroups of patients resolved by performing exact methods of statistical analysis. However, the strong point of the current study was that it found that serum ferritin levels can be used as an alternative method of T2* MRI in the areas where T2* MRI is not available. The serum ferritin levels had a significant relationship with liver and heart iron burden. Therefore, it can be used to evaluate iron over-load in areas where access to T2* MRI is limited.
Acknowledgments
The present article was extracted from the thesis by Zahra Majd M.D; financially supported by Shiraz University of Medical Sciences (grant number 3663).
References
- 1.Taher A, Isma'eel H, Cappellini MD. Thalassemia intermedia: revisited. Blood Cells Mol Dis. 2006;37(1):12–20. doi: 10.1016/j.bcmd.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Cappellini MD, Robbiolo L, Bottasso BM, Coppola R, Fiorelli G, Mannucci AP. Venous thromboembolism and hypercoagulability in splenectomized patients with thalassaemia intermedia. Br J Haematol. 2000;111(2):467–73. doi: 10.1046/j.1365-2141.2000.02376.x. [DOI] [PubMed] [Google Scholar]
- 3.Atichartakarn V, Likittanasombat K, Chuncharunee S, Chandanamattha P, Worapongpaiboon S, Angchaisuksiri P, et al. Pulmonary arterial hypertension in previously splenectomized patients with beta-thalassemic disorders. Int J Hematol. 2003;78(2):139–45. doi: 10.1007/BF02983382. [DOI] [PubMed] [Google Scholar]
- 4.Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, et al. Cardiac morbidity and mortality in deferoxamine- or deferiprone-treated patients with thalassemia major. Blood. 2006;107(9):3733–7. doi: 10.1182/blood-2005-07-2933. [DOI] [PubMed] [Google Scholar]
- 5.Wood JC, Enriquez C, Ghugre N, Otto-Duessel M, Aguilar M, Nelson MD, et al. Physiology and pathophysiology of iron cardiomyopathy in thalassemia. Ann N Y Acad Sci. 2005;1054:386–95. doi: 10.1196/annals.1345.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ludwig J, Batts KP, Moyer TP, Baldus WP, Fairbanks VF. Liver biopsy diagnosis of homozygous hemochromatosis: a diagnostic algorithm. Mayo Clin Proc. 1993;68(3):263–7. doi: 10.1016/s0025-6196(12)60047-0. [DOI] [PubMed] [Google Scholar]
- 7.Fischer R, Harmatz PR. Non-invasive assessment of tissue iron overload. Hematology Am Soc Hematol Educ Program. 2009:215–21. doi: 10.1182/asheducation-2009.1.215. [DOI] [PubMed] [Google Scholar]
- 8.Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, et al. MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood. 2005;106(4):1460–5. doi: 10.1182/blood-2004-10-3982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson LJ, Holden S, Davis B, Prescott E, Charrier CC, Bunce NH, et al. Cardiovascular T2-star (T2*) magnetic resonance for the early diagnosis of myocardial iron overload. Eur Heart J. 2001;22(23):2171–9. doi: 10.1053/euhj.2001.2822. [DOI] [PubMed] [Google Scholar]
- 10.Leung AW, Chu WC, Lam WW, Lee V, Li CK. Magnetic resonance imaging assessment of cardiac and liver iron load in transfusion dependent patients. Pediatr Blood Cancer. 2009;53(6):1054–9. doi: 10.1002/pbc.22170. [DOI] [PubMed] [Google Scholar]
- 11.Marsella M, Borgna-Pignatti C, Meloni A, Caldarelli V, Dell'Amico MC, Spasiano A, et al. Cardiac iron and cardiac disease in males and females with transfusion-dependent thalassemia major: a T2* magnetic resonance imaging study. Haematologica. 2011;96(4):515–20. doi: 10.3324/haematol.2010.025510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koonrungsesomboon N, Chattipakorn SC, Fucharoen S, Chattipakorn N. Early detection of cardiac involvement in thalassemia: From bench to bedside perspective. World J Cardiol. 2013;5(8):270–9. doi: 10.4330/wjc.v5.i8.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kirk P, Roughton M, Porter JB, Walker JM, Tanner MA, Patel J, et al. Cardiac T2* magnetic resonance for prediction of cardiac complications in thalassemia major. Circulation. 2009;120(20):1961–8. doi: 10.1161/CIRCULATIONAHA.109.874487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azarkeivan A, Hashemieh M, Akhlaghpoor S, Shirkavand A, Yaseri M, Sheibani K. Relation between serum ferritin and liver and heart MRI T2* in beta thalassaemia major patients. East Mediterr Health J. 2013;19(8):727–32. [PubMed] [Google Scholar]
- 15.Zamani F, Razmjou S, Akhlaghpoor S, Eslami SM, Azarkeivan A, Amiri A. T2* magnetic resonance imaging of the liver in thalassemic patients in Iran. China Natl J New Gastroenterol. 2011;17(4):522–5. doi: 10.3748/wjg.v17.i4.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taher A, El Rassi F, Isma'eel H, Koussa S, Inati A, Cappellini MD. Correlation of liver iron concentration determined by R2 magnetic resonance imaging with serum ferritin in patients with thalassemia intermedia. Haematologica. 2008;93(10):1584–6. doi: 10.3324/haematol.13098. [DOI] [PubMed] [Google Scholar]
- 17.Pakbaz Z, Fischer R, Fung E, Nielsen P, Harmatz P, Vichinsky E. Serum ferritin underestimates liver iron concentration in transfusion independent thalassemia patients as compared to regularly transfused thalassemia and sickle cell patients. Pediatr Blood Cancer. 2007;49(3):329–32. doi: 10.1002/pbc.21275. [DOI] [PubMed] [Google Scholar]
- 18.Montazare Lotfe Elahi S, Hashemi AS, Behjati SM, Zaolfaghari F, Dehghani A. The relation between left ventricular function and serum ferritin in major β-thalassemia. Iran J Pediatr Hematol Oncol. 2011;1(3):94–7. [Google Scholar]
- 19.Bosi G, Crepaz R, Gamberini MR, Fortini M, Scarcia S, Bonsante E, et al. Left ventricular remodelling, and systolic and diastolic function in young adults with beta thalassaemia major: a Doppler echocardiographic assessment and correlation with haematological data. Heart. 2003;89(7):762–6. doi: 10.1136/heart.89.7.762. [DOI] [PMC free article] [PubMed] [Google Scholar]