Abstract
The aim of this metaanalysis was to evaluate the association between nonsurgical factors and survival rate of digital replantation. A computer search of MEDLINE, OVID, EMBASE and CNKI databases was conducted to identify literatures for digital replantation, with the keywords of “digit,” “finger” and “replantation” from their inception to June 10, 2014. Based on the inclusion and exclusion criteria, data were extracted independently by two authors using piloted forms. Review Manager 5.2 software was used for data analysis. The effect of some nonsurgical factors (gender, age, amputated finger, injury mechanisms, ischemia time and the way of preservation) on the survival rate of digital replantation was assessed. The metaanalysis result suggested that gender and ischemia time had no significant influence on the survival rate of amputation replantation. However, the survival rate of digital replantation of adults was significantly higher than that of children. The guillotine injury of a finger was easier to replant successfully than the crush and avulsion. The little finger was more difficult for replantation than thumb. Survival rate of fingers stored in low temperature was higher than that in common temperature. The present metaanalysis suggested that age, injury mechanism, amputated finger and the way of preservation were significantly associated with the survival rate of digital replantation.
Keywords: Digits, microvascular surgery, replantation, survival rate, finger
MeSH terms: Finger, microsurgery, replantation, survival rate
INTRODUCTION
Digital replantation is a complex and delicate process of microvascular surgery. The surgery contains debridement, bone and joint fixation, tendon suture, vascular anastomosis, nerve suture and skin suture. When considering reattached surgery there are some obvious facts that should be taken into concern, including the adverse outcomes of surgery, failure rates for replantation, the length of recovery and the limits of function and aesthetic appearance.1
Since the first successful digital replantation performed by Komatsu and Tamai in 1967,2 surgeons and researchers have done numerous attempts to improve the survival rate of digital replantation. Obviously, the survival rate is largely improved with the evolution of surgical techniques and scientific technology. Also, the use of microvascular technique in digital replantation, efficient techniques to minimize ischemia times, the rituals for preparation, guidelines for postoperative care and strategies for treating complications has widely increased the survival rate in recent years.3,4,5 However, reconstruction of the fingertip by replantation is still a technically challenging.6 To take vascular anastomosis as an example, a digital vessel with a diameter of 1 mm needs to be repaired with 6–8/0 sutures.1 The replantation does not always happen under favorable circumstances, it depends on some factors such as the conditions of the amputated finger, the timing of the operation and the surgical teams.7 As for the effect of some nonsurgical factors such as patient gender, mechanisms of injury and ischemia time on survival rate, there are different points of view. For instance, Hattori et al. reported the effect of gender on survival rate of replantation and the survival rate was 80.4% in male,8 while as Lin et al. reported, the survival rate was only 37.5%.9 Additionally, fewer systematic reviews of the nonsurgical factors were conducted, especially in the recent years.
Therefore, in the present study, a metaanalysis was conducted to evaluate the influence of some nonsurgical factors on the survival rate of digital replantation. Nonsurgical factors such as gender, age, amputated finger, injury mechanisms, ischemia time and the way of preservation were investigated in our study.
MATERIALS AND METHODS
A detailed protocol including the literature-search strategies, the inclusion and exclusion criteria, outcome measurements and methods of statistical analysis was developed before conducting the study. The protocol was prepared for metaanalysis guidelines according to the preferred reporting items.
Search strategy
Aimed to identify all relevant researches regardless of language, a computer retrieval of MEDLINE, OVID, EMBASE and CNKI database was conducted using the combination of text keywords “digit,” “finger” and “replantation” from their inception to June 10, 2014. All of the included articles were also hand searched to identify any other relevant citations. No restriction was set on the source of participants (race, clinic or hospital).
Inclusion and exclusion criteria
All of the studies identified were carefully reviewed by two investigators independently and any discrepancy was resolved by discussion, when necessary, adjudicated by a third reviewer. The inclusion and exclusion criteria were as follows:
Inclusion criteria
(1) Human studies (2) Primary data In study (3) Single/multiple distal replantations. (4) Extractable survival data for distal replantation. (5) Followup not <6 months.
Exclusion criteria
(1) Review or case report articles. (2) Case series with <10 patients (3) Incomplete information of amputations or revascularization or surgical procedure (4) Report only successful cases (5) Experimental studies.
Data extraction
Data were extracted independently by two authors using pilot forms. The data included the general characteristics of each study and the outcome measures. General characteristics included study design, first author, year of publication, sample size, interventions and various types.
Statistical analysis
Review Manager 5.2 (Cochrane Collaboration, Oxford, UK) was used to analyze the data according to the Cochrane Handbook. The heterogeneity among combined study results was tested by Cochran's Q-test and by the degree of inconsistency (I2 values). I2 < 50% was considered as no significant heterogeneity and a fixed effects model was used. While, I2 > 50% indicated that there was heterogeneity among the included studies and a random effects model was used. Publication bias was assessed by the Egger's test. The comparison results were displayed in the forest plot and odds ratio (OR) with 95% confidence interval (CI) was used for comparison of the effect of each factor.
RESULTS
Description of studies
The selection process of studies was shown in Figure 1. Finally, 23 articles,3,4,5,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26 including 4,871 amputated digits, were chosen for metaanalysis. The characteristics of included studies were listed in Table 1. No publication bias was observed except the metaanalysis of gender and survival rate.
Figure 1.
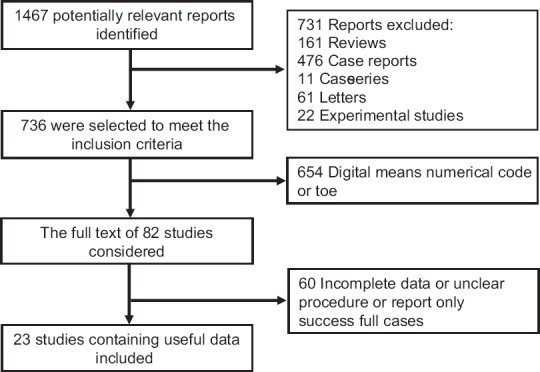
Study selection process for metaanalysis
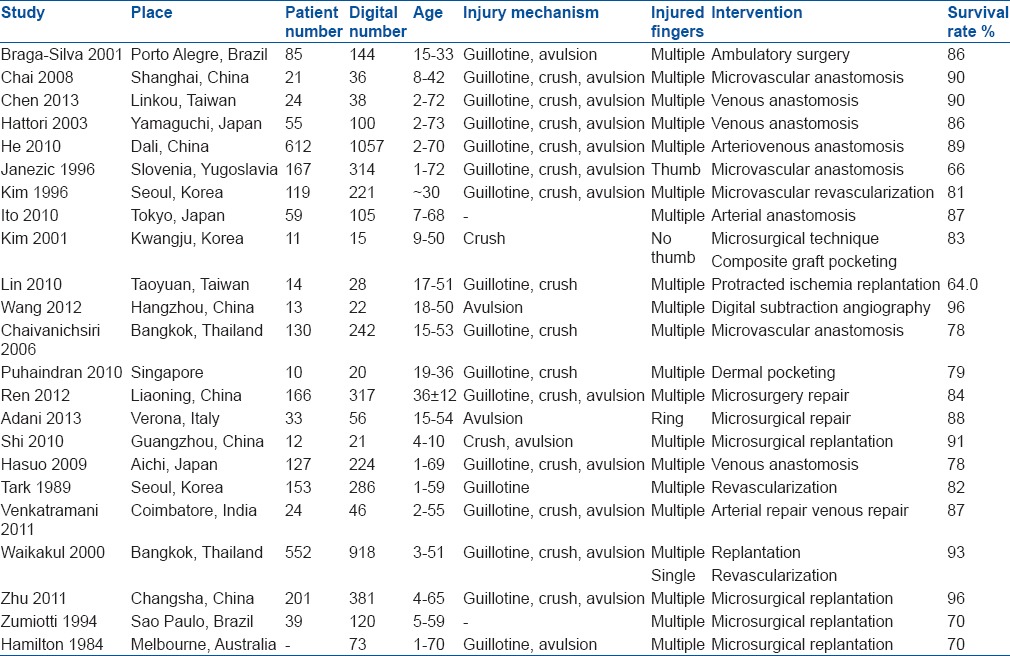
Table 1.
Characteristics of the included studies
Patient characteristics and survival rate
There were 10 studies involved in a metaanalysis of gender and survival rate. The result showed that the difference of survival rate between male and female did not reach a statistically significant criterion (OR: 1.17; 95% CI [0.77, 1.79]; P = 0.46).
We also divided patients into children group and adults group. The children were defined as age <18 years. The survival rate of adults group was significantly higher than that of children group (OR: 0.49; 95% CI [0.30, 0.82]; P = 0.006) [Figure 2].
Figure 2.
Comparison of survival rate between children and adults. The area of the squares reflects the study specific weight. The diamond shows the summary odds ratio estimate from ten studies
Mechanisms of injury and survival rate
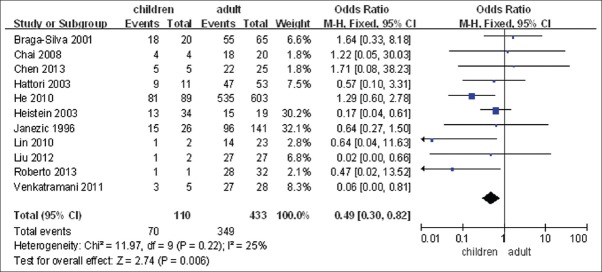
There were 15 studies referred to the mechanisms of injury. The injury mechanisms of amputated digits mainly included guillotine, crush and avulsion. We defined guillotine, crush, and avulsion according to Venkatramani's classifications.21 Guillotine amputation refers to sharp injury (like from a knife). Crush injury is caused by an object that resulted in the compression of the finger. Finally, avulsion is an injury in which the body structure is forcibly detached from its normal point of insertion by either trauma or surgery. It occurs when a digit is rapidly pulled out of the hand and in accidents involving fast moving machines. The results showed that the survival rate of digital replantation of guillotine was significantly higher than that of crush (OR: 2.86; 95% CI [1.03, 7.97], P = 0.04) and avulsion (OR: 7.22; 95% CI [4.83–10.79], P < 0.00001) [Figure 3]. The survival rate of digital replantation between crushed and avulsed digits was not significantly different (OR: 1.26; 95% CI [0.46, 3.41], P = 0.65).
Figure 3.
(a) Metaanalysis of guillotine, avulsion and survival rate. The area of the squares reflects the study specific weight. The diamond shows the summary odds ratio (OR) (b) Metaanalysis of guillotine, crushing and survival rate. The area of the squares reflects the study specific weight. The diamond shows the summary OR
There were 6 studies about complete/incomplete amputation. The result showed that there was no significant difference of the survival rate between complete amputation and an incomplete amputation (OR: 0.73; 95% CI [0.52, 1.02], P = 0.07).
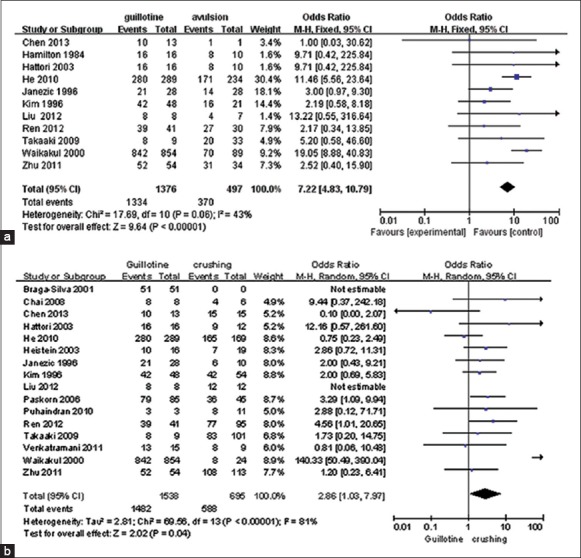
The amputated digits and survival rate
There were 12 studies involved in the metaanalysis of survival rate of the amputated digits. The amputated digits have been classified into five categories: Thumb, index finger, middle finger, ring finger and little finger. For each selected finger, we compared the survival rate of the selected finger with that of all the other fingers. We found that only the little finger was more difficult to replant successfully than the thumb (OR: 2.09; 95% CI [1.02, 4.25], P = 0.04) [Figure 4]. Significant difference was not found in analysis of other fingers (P > 0.05).
Figure 4.
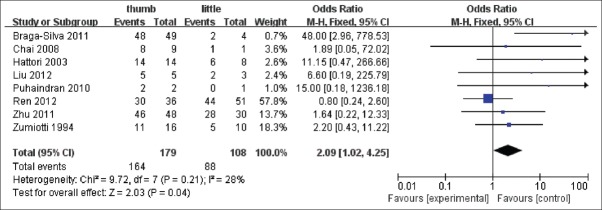
Comparison of survival rate between thumb and little. The area of the squares reflects the study specific weight. The diamond shows the summary odds ratio estimate from eight studies
The zones of injury have been divided into distal phalanx (DP), middle phalanx, proximal phalanx and their interphalangeal (IP) joint. In our study, the association between injury zone of DP and survival rate was studied since few studies involved other zones were reported. There were 11 studies included in the metaanalysis. The DP was divided into two subgroups according to the Tamai's classification: Zone I and zone II. Zone I and zone II were defined as distal to nail base and distal interphalangeal joint to the nail base, respectively. Metaanalysis suggested that there was no significant association between injury zone of DP and survival rate (OR: 0.95; 95% CI [0.64, 1.40], P = 0.79).
The way of preservation and survival rate
There were three studies included in the metaanalysis of the way of preservation and survival rate. We compared the survival rate of amputated fingers preserved in the ice bag and common temperature, respectively. Metaanalysis suggested that the amputated digits stored in low temperature were more likely to survive than that in common temperature (OR: 4.89; 95% CI [2.14, 11.20], P = 0.0002) [Figure 5].
Figure 5.
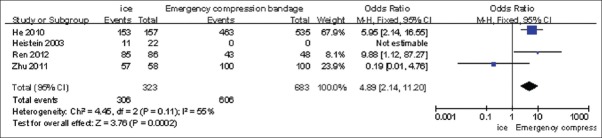
Comparison of survival rate between ice and bandage. The area of the squares reflects the study specific weight. The diamond shows the summary odds ratio estimate from three studies
Ischemia time and survival rate
There were four studies reported the ischemia time and replantation survival rate. The patients were divided into two groups according to whether the ischemia time was more than 12 h. The results indicated there was no significant association between ischemia time and survival rate (OR: 1.45; 95% CI [0.88, 2.37], P = 0.14).
DISCUSSION
When creating a metaanalysis, numerous inherent problems emerged from the studies, such as the publication bias and technical differences of surgeons. In our study, high homogeneity was required in clinical medicine and methodology. We evaluated the effects of several nonsurgical factors on the survival rate of digital replantation by a metaanalysis. The experiment involved 4871 amputated digits. The results indicated that age of patients, mechanisms of injury, amputated digits and the way of preservation were significantly associated with the survival rate of digital replantation (P < 0.05), while gender and ischemia time had no significant influence (P > 0.05).
Our metaanalysis of gender showed that the difference of survival rate between male and female did not reach a statistically significant criterion (P > 0.05), which was different with earlier reports. Previous studies provided inconsistent results when analyzing the influence of sex on the survival rate of digital replantation. Hamilton et al. reported a review about the amputated thumb between 1970 and 1980, and suggested that females showed a greater failure rate than males.25 To the contrary, Dec indicated that the replanted digits of female patients survived at a rate 2.3 times greater than those of male patients.27 These differences might be caused by surgery technological disparity in different era or sample differences.
Classification of adults and children was different in the selected citations, with 9, 12, 16, 18 years old as boundaries. In this study, we defined children as no more than 18 years old, and adults as more than 18 years old. The results indicated that digits of adults were more likely to survive than those of children, which were consistent with the previous report.5 The results also were similar with Hamilton et al. reported, in which higher failure rate was present in children under 10 years.25 A possible explanation is that the blood vessel of children is usually narrow, and the venous wall is thin, which increase the technical difficulties of digital replantation.25,28
For the mechanisms of injury, our results suggested that the failure rate of digits with crush or avulsion injury was higher than that of guillotine, while no statistical difference was found between crush and avulsion injury (P > 0.05). Choi et al. reported that the severe crush of parts was one of the contraindications of digital replantation.29 This was consistent with the observation that there was a significant difference in survival between clean cut amputations and the more crushed amputations types (crush-cut and crush avulsion). There are two possible explanations: One is that veins are destructed in crush and avulsion injured finger is more severed.22 For example, failure of revascularization was associated with severe diffuse crush/avulsion injury and resulted in the damage of restoration of blood flow;25 another is that there is a selection bias in distal replantation in which the severely crushed digits are not replanted, and the so called crush avulsion amputations are likely to have a narrower zone of injury.30
There were few number of studies to evaluate the association between survival rate and another injury zone such as middle phalanx, proximal IP joint, proximal phalanx and the metacarpal phalanx. Therefore, only the relationship between injury zone of DP and survival rate was assessed. Metaanalysis showed that there was no significant difference of survival rate between zone I and II (P > 0.05).
As reported in some researches,27 postoperative functional recovery of the replanted digits largely depended on the duration of ischemia. Conversely, this metaanalysis showed that there was no significant association between ischemia time (≤12 h and >12 h) and replantation survival rate. This can be partly explained as follows: Fingers have very little muscle tissue, so they can tolerate relatively long duration of ischemia. Moreover, favorable outcomes were reported in replantation after prolonged ischemic insults. However, some studies showed that ischemia might be prolonged due to unexpected intraoperative complications as well as health problems, which thus delayed the replantation surgery. The survival rate was low and postoperative functional recovery of replanted fingers was poor after ischemia for >24 h. As reported, finger replantation after protracted ischemia (>24 h) had a survival rate of 66.7%, which was far below that of the short term ischemia.9 Ischemia leads to progressive damage of an amputated segment and finally causes cellular death. Reestablishment of arterial flow to the tissue after ischemia prolonged results in some pathophysiologic changes collectively known as ischemia-reperfusion injury or no-reflow phenomenon.8,15,16
Our result indicated that the cold preservation improved the survival rate. The methods used to preserve organs mainly based on suppression of metabolism by hypothermia.31 Cold storage can be used in the preservation of organs such as kidney, liver, and heart. It could make most organs lose adenosine triphosphate (ATP) rapidly, prolong survival time, and most organs can regenerate ATP when transplanted after preservation.31 Our result suggested that the low temperature was superior to the common temperature for amputated finger preservation.
In a large part, the main factor for survival of replanted digit is the skill of the surgeon performing the replanted operation since digits replantation is very skill dependent surgery. In additions, in order to guarantee the homogeneous security in methodology, we also evaluated the combined, study strictly, including random method, blind method implementation and random concealment. Thus, though here we cannot identify the effect of skill of the surgeon on survival of replantation, the results of other factors are still relievable.
CONCLUSION
The present metaanalysis suggested that crush and avulsion injury, the amputated little finger, children, and cold preservation seem to have a somewhat worse prognosis. Gender, injury zone of DP and ischemia time were not significantly associated with the survival rate of digital replantation. What should be noted here is that adverse factors mentioned above are not absolute contraindications for replantation. Many digits were successfully replanted in the disadvantageous conditions as the surgical techniques are more advanced. Now, the focus is not just limited to the achievement of digit survival, but the achievement of digital function that can improve the quality of life as compared to digital replantation. This metaanalysis of nonsurgical factors of digital replantation could provide a comprehensive guidance to surgeons in surgery decision and help patients made correct initial preprocessing for severed finger and know the possibility of outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Wilhelmi BJ, Lee WP, Pagenstert GI, May JW., Jr Replantation in the mutilated hand. Hand Clin. 2003;19:89–120. doi: 10.1016/s0749-0712(02)00137-3. [DOI] [PubMed] [Google Scholar]
- 2.Komatsu S, Tamai S. Successful replantation of a completely cut-off thumb. Plast Reconstr Surg. 1968;42:374–7. [Google Scholar]
- 3.Chen YC, Chan FC, Hsu CC, Lin YT, Chen CT, Lin CH. Fingertip replantation without venous anastomosis. Ann Plast Surg. 2013;70:284–8. doi: 10.1097/SAP.0b013e3182321b81. [DOI] [PubMed] [Google Scholar]
- 4.Wang LH, Zhang GQ. Use of digital subtraction angiography for assessment of digital replantation. J Zhejiang Univ Sci B. 2012;13:209–12. doi: 10.1631/jzus.B1100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu ZB. Multiple Factors Analysis on Survival Rate of Digital Replantation [Master's Thesis] Central South University. 2011 [Google Scholar]
- 6.Scheker LR, Becker GW. Distal finger replantation. J Hand Surg Am. 2011;36:521–8. doi: 10.1016/j.jhsa.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Chaivanichsiri P, Rattanasrithong P. Type of injury and number of anastomosed vessels: Impact on digital replantation. Microsurgery. 2006;26:151–4. doi: 10.1002/micr.20181. [DOI] [PubMed] [Google Scholar]
- 8.Hattori Y, Doi K, Ikeda K, Abe Y, Dhawan V. Significance of venous anastomosis in fingertip replantation. Plast Reconstr Surg. 2003;111:1151–8. doi: 10.1097/01.PRS.0000046497.88549.E0. [DOI] [PubMed] [Google Scholar]
- 9.Lin CH, Aydyn N, Lin YT, Hsu CT, Lin CH, Yeh JT. Hand and finger replantation after protracted ischemia (more than 24 hours) Ann Plast Surg. 2010;64:286–90. doi: 10.1097/SAP.0b013e3181b0bb37. [DOI] [PubMed] [Google Scholar]
- 10.Adani R, Pataia E, Tarallo L, Mugnai R. Results of replantation of 33 ring avulsion amputations. J Hand Surg Am. 2013;38:947–56. doi: 10.1016/j.jhsa.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 11.Braga-Silva J. Single digit replantations in ambulatory surgery 85 cases. Ann Chir Plast Esthet. 2001;46:74–83. doi: 10.1016/s0294-1260(01)00002-4. [DOI] [PubMed] [Google Scholar]
- 12.Chai Y, Kang Q, Yang Q, Zeng B. Replantation of amputated finger composite tissues with microvascular anastomosis. Microsurgery. 2008;28:314–20. doi: 10.1002/micr.20508. [DOI] [PubMed] [Google Scholar]
- 13.Hasuo T, Nishi G, Tsuchiya D, Otsuka T. Fingertip replantations: Importance of venous anastomosis and the clinical results. Hand Surg. 2009;14:1–6. doi: 10.1142/S0218810409004177. [DOI] [PubMed] [Google Scholar]
- 14.Ito H, Sasaki K, Morioka K, Nozaki M. Fingertip amputation salvage on arterial anastomosis alone: An investigation of its limitations. Ann Plast Surg. 2010;65:302–5. doi: 10.1097/SAP.0b013e3181cc0021. [DOI] [PubMed] [Google Scholar]
- 15.Janezic TF, Arnez ZM, Solinc M, Zaletel-Kragelj L. One hundred sixty-seven thumb replantations and revascularisations: Early microvascular results. Microsurgery. 1996;17:259–63. doi: 10.1002/(SICI)1098-2752(1996)17:5<259::AID-MICR4>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 16.Kim KS, Eo SR, Kim DY, Lee SY, Cho BH. A new strategy of fingertip reattachment: Sequential use of microsurgical technique and pocketing of composite graft. Plast Reconstr Surg. 2001;107:73–9. doi: 10.1097/00006534-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Kim WK, Lim JH, Han SK. Fingertip replantations: Clinical evaluation of 135 digits. Plast Reconstr Surg. 1996;98:470–6. doi: 10.1097/00006534-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Puhaindran ME, Paavilainen P, Tan DM, Peng YP, Lim AY. Dermal pocketing following distal finger replantation. J Plast Reconstr Aesthet Surg. 2010;63:1318–22. doi: 10.1016/j.bjps.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 19.Shi D, Qi J, Li D, Zhu L, Jin W, Cai D. Fingertip replantation at or beyond the nail base in children. Microsurgery. 2010;30:380–5. doi: 10.1002/micr.20743. [DOI] [PubMed] [Google Scholar]
- 20.Tark KC, Kim YW, Lee YH, Lew JD. Replantation and revascularization of hands: Clinical analysis and functional results of 261 cases. J Hand Surg Am. 1989;14:17–27. doi: 10.1016/0363-5023(89)90054-3. [DOI] [PubMed] [Google Scholar]
- 21.Venkatramani H, Sabapathy SR. Fingertip replantation: Technical considerations and outcome analysis of 24 consecutive fingertip replantations. Indian J Plast Surg. 2011;44:237–45. doi: 10.4103/0970-0358.85345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waikakul S, Sakkarnkosol S, Vanadurongwan V, Un-nanuntana A. Results of 1018 digital replantations in 552 patients. Injury. 2000;31:33–40. doi: 10.1016/s0020-1383(99)00196-5. [DOI] [PubMed] [Google Scholar]
- 23.He Y. Analysis on Influencing Factors of Survival Rate of Replantation of Severed Cut-Fingers with Logistic Regression [Master's Thesis] Dali University. 2010 [Google Scholar]
- 24.Ren ZP, Liu YH, Liu D, Liang YH. The related factors affecting the survival rate of fingertip replantation. Hebei Med J (Chin) 2012;34:2790–1. [Google Scholar]
- 25.Hamilton RB, O’Brien BM, Morrison A, MacLeod AM. Survival factors in replantation and revascularization of the amputated thumb-10 years experience. Scand J Plast Reconstr Surg. 1984;18:163–73. doi: 10.3109/02844318409052833. [DOI] [PubMed] [Google Scholar]
- 26.Zumiotti A, Ferreira MC. Replantation of digits: Factors influencing survival and functional results. Microsurgery. 1994;15:18–21. doi: 10.1002/micr.1920150107. [DOI] [PubMed] [Google Scholar]
- 27.Dec W. A meta-analysis of success rates for digit replantation. Tech Hand Up Extrem Surg. 2006;10:124–9. doi: 10.1097/01.bth.0000225005.64605.17. [DOI] [PubMed] [Google Scholar]
- 28.Yang FC, Zhao JM, Yang Z, Sha K. The analysis on the risk factors of distal finger replantation. Guangxi Med J (Chin) 2003;25:3. [Google Scholar]
- 29.Choi MS, Lee JH, Ki SH, Ahn HC. Trends in digital replantation. Curr Orthop Pract. 2012;23:284–8. [Google Scholar]
- 30.Sebastin SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011;128:723–37. doi: 10.1097/PRS.0b013e318221dc83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Southard JH, Belzer FO. Organ preservation. Annu Rev Med. 1995;46:235–47. doi: 10.1146/annurev.med.46.1.235. [DOI] [PubMed] [Google Scholar]


