Abstract
Background:
Many implants and techniques are used for the treatment of open phalangeal fractures with varying grades of stability. The ubiquitous and simple Kirschner (K) wiring does not provide adequate stability to allow early mobilization of fingers. Lister described a combination of coronal interosseous wire and oblique K-wire technique for phalangeal fracture fixation with a stable construct that allowed early mobilization. Due to the fancied resemblance of this construct to the Greek alphabet θ (theta), we have referred to this as the theta fixation.
Materials and Methods:
Ten patients with open proximal phalangeal shaft (transverse) fractures were treated with theta fixation between January and June 2010. Outcome was analysed in terms of stability, early mobilization, fracture healing and function of hand. They were graded according to the Belsky score.
Results:
90% patients were graded excellent and 10% good, with none having fair or poor results. All fractures allowed the mobilization at a mean of 2.9 days and all healed at an average of 6.1 weeks. No loss of stability was seen on followup X-rays. All patients returned to their old profession.
Conclusion:
The theta fixation technique is a safe, simple and effective method for open transverse phalangeal fractures with results comparable to other techniques. This method gives superior fracture stability to allow early mobilization of joints and thus early return of function. It is also a cost effective way of management for the developing world.
Keywords: Hand fracture, interosseous wiring, Lister fixation, phalanx fracture, theta fixation
MeSH terms: Hand, finger, fracture, fracture fixation
INTRODUCTION
The most quoted statement regarding the management of hand fractures probably is the following comment by Swanson: “The treatment of hand fractures is complicated by deformity from no treatment, stiffness from overtreatment and both from poor treatment.”1 This simple but eloquent statement points out the problems associated with phalangeal fracture treatment.
Various methods to treat phalangeal fractures include buddy strapping, percutaneous cross Kirschner (K) wiring, plate fixation and tension band wiring. Open transverse phalangeal fractures require internal fixation. Open fractures, however, must be fixed with a minimum of implants to reduce the possibility of infections, but with a stable construct to commence early mobilization to prevent stiffness. Lister described a technique of coronal interosseous wiring with oblique coronal K-wire supplementation for the treatment of phalangeal fractures.2
Early mobilization of phalangeal shaft fractures within the first 4 weeks after injury resulted in 75–80% return of hand function.3 However, when mobilization was initiated later than 4 weeks; the hand function was only 66% of preinjury levels. From this, the need for early mobilization is well-understood. Rigid fixation allows early mobilization of the injured digit. Various fixation techniques like single oblique K-wire fixation, crossed K-wire fixation, oblique screw fixation, plate and screw fixation etc., have been described for phalangeal shaft fractures. Fyfe and Mason4 produced experimental fractures of the proximal phalangeal shaft and tested different methods of fixation. They reported that the least rigid was the single K-wire fixation. Crossed K-wire fixation was more rigid and interosseous wiring supplemented with an oblique K-wire the most rigid. Since this configuration resembles the Greek letter theta (θ), we refer to it as “theta fixation.” The theta fixation, therefore, can be considered a rigid fixation allowing early mobilization of the fractured digit.
There is no specific literature available for the outcome of fixation of open phalangeal fractures. We report our experience in the management of open transverse phalangeal fractures of the hand using the theta fixation technique.
MATERIALS AND METHODS
Ten patients with open transverse fracture of the proximal phalanx from January to June 2010 who underwent fracture fixation using the theta technique after appropriate debridement and wound care were included in this study. The inclusion criteria were (a) single digit open transverse proximal phalanx fracture (b) no other injured structures in hand (c) no co-morbidities. The exclusion criteria were (a) comminution (b) extensive soft tissue injury (d) patients already with stiffness of any digit.
Operative procedure
Meticulous debridement and irrigation of wound was first done in the operating room. The fracture was classically approached by a dorsal curvilinear incision but required to be modified according to the position of the original wound [Figure 1a–d]. The extensor tendon was split longitudinally to expose the fracture. After trial reduction, two coronal transverse holes were drilled on each fragment parallel to fracture line using a 1.25 mm K-wire. Stainless steel wire (Ormed Surgicals, Chennai, India) (gauge 24–26) was threaded through the holes to complete a loop The wire was tightened with a wire twister making sure that there was good apposition on the far cortex with a nitch-notch fracture reduction. A K-wire was then drilled obliquely avoiding the drill holes for the steel wires. The K-wire was cut flush with the bone while the steel wire cut and twisted such that the extensor tendon was not impaled in any way [Figure 2a–c]. The free end of the wire loop may also be buried in the bone by a separate drill hole.
Figure 1.
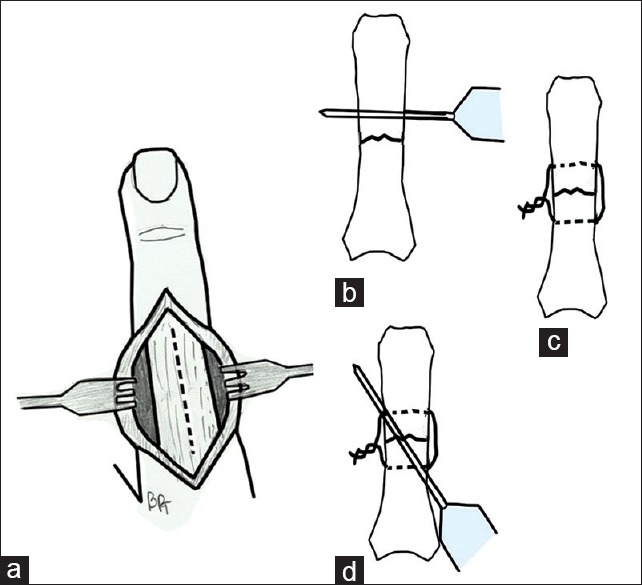
Diagrammatic representation of the theta fixation. (a) Dorsal extensor splitting approach. (b) Transverse drill hole for the cerclage wire. (c) Cerclage wire applied. (d) Oblique Kirschner-wire insertion
Figure 2.
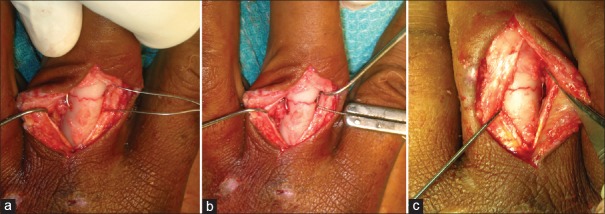
Intraoperative clinical photographs of theta fixation. (a) Fracture exposed through the dorsal extensor splitting approach, reduced and cerclage wire inserted. (b) Cerclage wire tightened. (c) Kirschner-wire inserted
The extensor tendon was then repaired with Ethilon™ (Ethicon, Johnson and Johnson, Aurungabad, India) (4–0) followed by skin closure. The fingers were immobilized in volar plaster of Paris slab in the James position.
Postoperative care
Gentle mobilization of the fingers was done by the surgeon during wound inspection and patients were encouraged to move the fingers actively. After the 3rd day, the hand therapist was instructed to commence active and passive mobilization of the hand daily. In order to protect the fixation from unwanted unprotected activity, the splint was continued for 3 weeks. Patients attended the hand therapy clinic daily where the therapists would remove the splint to encourage active and passive range of motion exercises under supervision and then reapply the splint. The sutures were removed on the 10th day. The slab support to the hand was discontinued at the end of 3rd week. The K-wires were removed under local anesthesia in OPD after fracture union if required.
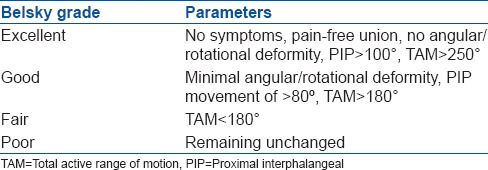
The radiographs were taken on 3rd day, at 6th week and 12th week and 24th week [Figures 3 and 4]. Patients were allowed to do light work at the end of 6 weeks to return to their profession with full unrestricted activity when radiological evidence of fracture union was confirmed. The outcome was measured by Belsky et al.5 score [Table 1] at end of 6th week, 3rd month, and 24th month.
Figure 3.

Preoperative X-ray of hand anteroposterior and oblique views showing a transverse fracture of the proximal phalanx of the middle finger
Figure 4.

Postoperative X-rays of hand anteroposterior and oblique views showing the theta fixation with sound fracture union
Table 1.
The Belsky et al.5 score
RESULTS
Of the 10 patients, nine were male [Table 2]. The most common mechanism of injury was road traffic accident (n = 6). The average age was 33.6 years (range 19-53 years). Index, middle and ring finger were involved in three cases each and the thumb in one. Little finger was not involved in any patient in this series. The average followup was 28.8 months (range 25-33 months). The average hospital stay was 5.9 days (range 5-8 days). The average time for starting mobilization of joints was 2.9 days. The average time to return to unrestricted routine activities and work was 11.3 weeks.
Table 2.
Clinical details of patients and followup
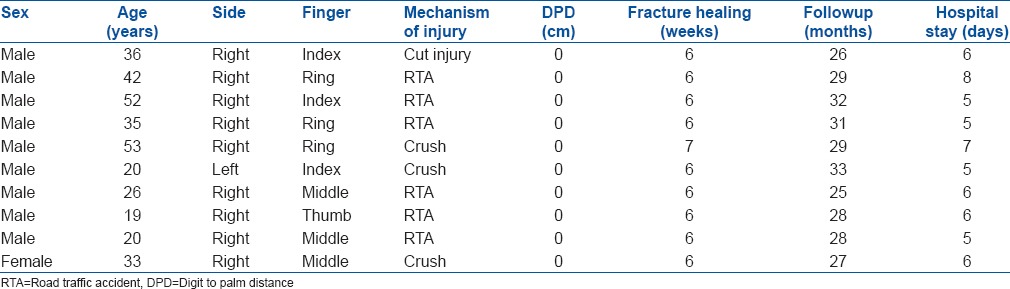
The average duration for radiological healing was 6.1 weeks (range 6-7 weeks). The outcome measured by Belsky et al. scoring method revealed seven excellent and three good results at the end of 6 weeks which changed to nine excellent and one good at the end of 3 months. The digit to palm distance (DPD) of all patients at the end of 6 weeks was zero [Figure 5]. No patients had infection or resurgery. Implants were removed in three patients following irritation of the skin by the wire. In one, it was done on the patient's request.
Figure 5.
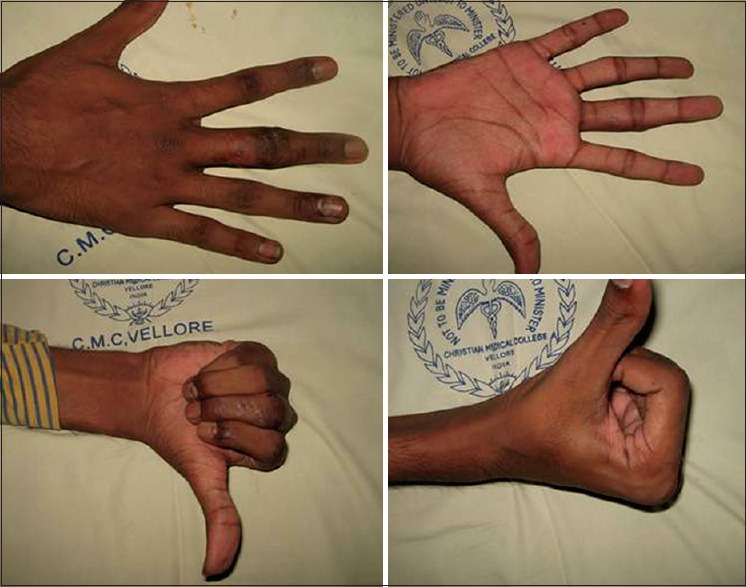
Clinical photographs showing the range of movements following theta fixation at 3 months followup
DISCUSSION
Phalangeal fractures are not uncommon injuries. The extensor tendon over the phalangeal shaft may adhere to the fracture site during union causing stiffness of the proximal interphalangeal joint, as well as an extensor lag.6 Early mobilization helps in preventing the adhesion. A rigid fixation is a prerequisite for early mobilization. Open transverse phalangeal fractures require internal fixation. Open fractures, however, must be fixed with a minimum of implants to reduce the possibility of infections, but with a stable construct to commence early mobilization to prevent stiffness. Closed reduction and percutaneous cross K-wiring is the standard treatment for closed phalangeal fractures. However, cross K-wire fixation fails to provide compression at the fracture site especially for transverse shaft fractures7 and may also result in distraction of the fracture with subsequent delayed unions or gap nonunions.8 As the construct is not very rigid, early mobilization is not routinely done. Reports on phalangeal fracture fixations generally deal with closed fractures. Though extremely stable, plate, and screw fixation is best avoided in open fractures to minimize the chance of subsequent infection. In this context, the Lister fixation provides adequate stability but minimizes the chance of infection as there is a minimum implant used.
Lister2 described fixation of transverse fractures and arthrodesis of digits with a cerclage wire and oblique K-wire which is type of tension band fixation, insisting on obtaining congruous reduction and maintaining fixation till the union. In his series, he had a 100% union rate in the case of transverse fractures. Overall, 83.2% of the maximum attainable total active range of motion (TAM) was achieved in the 100 cases. We have been utilizing this technique for the treatment of transverse phalangeal shaft fractures. The theta fixation technique is not as simple as crossed K-wire fixation, has a definite learning curve, but is our fixation of choice for open phalangeal fractures when the fracture line is transverse and there is no comminution.
Many studies have shown the efficacy of the tension band technique of fracture fixation. The strength of the K-wire and cerclage wire construct nears that of the plate and screw fixation. Rayhack et al.9 in their study concluded that single looped tension band wires were superior in strength to figure-of-eight constructs in experimental transverse osteotomies. Hung et al.10 following biomechanical testing of different fracture fixation techniques in the fifth metatarsal of porcine forelimbs concluded that an intra-medullary K-wire and a cerclage interosseous wire was more stable than crossed K-wires though not as rigid as a dorsal plate and screw fixation.
Pun et al.11 reported 70% fair or poor results in 109 unstable digital fractures treated with K-wire fixation. Lag screw fixation for proximal phalangeal fractures can be done only if the length of the fracture exceeds 2 times the diameter of the bone.12 Hence, screw fixation alone is not applicable to a transverse shaft fracture. Page and Stern13,14 reported total active digital motion was <180° in 62% of fractures after plate fixation of 39 phalangeal fractures. Green15,16,17 and Safoury18 have demonstrated that fracture stability is enhanced when the K-wires are supplemented with stainless steel wire, a technique termed composite (or tension band) wiring.
Massengill et al.19 noted that the only construct that is superior in stiffness and strength to any configuration of the wire loop or the K-wires is volar or lateral plate and screw fixation. Gould et al.20 concluded that tension band stabilization provides superior strength, stiffness, and approximation when compared with K-wire fixation.
Our result is comparable to other studies.21 The percutaneous pinning alone was reported to give 83% excellent result in a study by Hornbach and Cohen.22 They reported the results of 12 unstable extraarticular fractures of the proximal phalanx treated with intra medullary K-wires.
To conclude, theta fixation technique is a safe and effective method for open transverse proximal phalangeal fractures. The technique gives good stability and compression at the fracture site which allows early mobilization of joints to prevent stiffness.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Swanson AB. Fractures involving the digits of the hand. Orthop Clin North Am. 1970;1:261–74. [PubMed] [Google Scholar]
- 2.Lister G. Intraosseous wiring of the digital skeleton. J Hand Surg Am. 1978;3:427–35. doi: 10.1016/s0363-5023(78)80135-x. [DOI] [PubMed] [Google Scholar]
- 3.Strickland JW, Steichen JB, Klienman WB, Hastings H, II, Flynn N. Phalangeal fractures. Factors influencing digital performance. Orthop Rev. 1982;11:39–50. [Google Scholar]
- 4.Fyfe IS, Mason S. The mechanical stability of internal fixation of fractured phalanges. Hand. 1979;11:50–4. doi: 10.1016/s0072-968x(79)80009-1. [DOI] [PubMed] [Google Scholar]
- 5.Belsky MR, Eaton RG, Lane LB. Closed reduction and internal fixation of proximal phalangeal fractures. J Hand Surg Am. 1984;9:725–9. doi: 10.1016/s0363-5023(84)80023-4. [DOI] [PubMed] [Google Scholar]
- 6.Patankar H, Meman FW. Multiple intramedullary nailing of proximal phalangeal fractures of hand. Indian J Orthop. 2008;42:342–6. doi: 10.4103/0019-5413.39573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freeland AE, Geissler WB, Weiss AP. Surgical treatment of common displaced and unstable fractures of the hand. Instr Course Lect. 2002;51:185–201. [PubMed] [Google Scholar]
- 8.Ikuta Y, Tsuge K. Micro-bolts and micro-screws for fixation of small bones in the hand. Hand. 1974;6:261–5. doi: 10.1016/0072-968x(74)90037-0. [DOI] [PubMed] [Google Scholar]
- 9.Rayhack JM, Belsole RJ, Skelton WH., Jr A strain recording model: Analysis of transverse osteotomy fixation in small bones. J Hand Surg Am. 1984;9:383–7. doi: 10.1016/s0363-5023(84)80228-2. [DOI] [PubMed] [Google Scholar]
- 10.Hung LK, So WS, Leung PC. Combined intramedullary Kirschner wire and intra-osseous wire loop for fixation of finger fractures. J Hand Surg Br. 1989;14:171–6. doi: 10.1016/0266-7681_89_90121-6. [DOI] [PubMed] [Google Scholar]
- 11.Pun WK, Chow SP, So YC, Luk KD, Ip FK, Chan KC, et al. A prospective study on 284 digital fractures of the hand. J Hand Surg Am. 1989;14:474–81. doi: 10.1016/s0363-5023(89)80006-1. [DOI] [PubMed] [Google Scholar]
- 12.Steel WM. The A.O. small fragment set in hand fractures. Hand. 1978;10:246–53. doi: 10.1016/s0072-968x(78)80045-x. [DOI] [PubMed] [Google Scholar]
- 13.Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23:827–32. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 14.Stern PJ, Wieser MJ, Reilly DG. Complications of plate fixation in the hand skeleton. Clin Orthop Relat Res. 1987:59–65. [PubMed] [Google Scholar]
- 15.Greene T. Open pin fixation of the diaphysis for phalangeal fractures. In: Blair WF, editor. Techniques in Hand Surgery. Baltimore: Williams and Wilkins; 1996. pp. 187–91. [Google Scholar]
- 16.Greene TL, Noellert RC, Belsole RJ. Treatment of unstable metacarpal and phalangeal fractures with tension band wiring techniques. Clin Orthop Relat Res. 1987:78–84. [PubMed] [Google Scholar]
- 17.Greene TL, Noellert RC, Belsole RJ, Simpson LA. Composite wiring of metacarpal and phalangeal fractures. J Hand Surg Am. 1989;14:665–9. doi: 10.1016/0363-5023(89)90188-3. [DOI] [PubMed] [Google Scholar]
- 18.Safoury Y. Treatment of phalangeal fractures by tension band wiring. J Hand Surg Br. 2001;26:50–2. doi: 10.1054/jhsb.2000.0499. [DOI] [PubMed] [Google Scholar]
- 19.Massengill JB, Alexander H, Parson JR, Schecter MJ. Mechanical analysis of Kirschner wire fixation in a phalangeal model. J Hand Surg Am. 1979;4:351–6. doi: 10.1016/s0363-5023(79)80073-8. [DOI] [PubMed] [Google Scholar]
- 20.Gould WL, Belsole RJ, Skelton WH., Jr Tension-band stabilization of transverse fractures: An experimental analysis. Plast Reconstr Surg. 1984;73:111–6. doi: 10.1097/00006534-198401000-00027. [DOI] [PubMed] [Google Scholar]
- 21.Al-Qattan MM. Closed reduction and percutaneous K-wires versus open reduction and interosseous loop wires for displaced unstable transverse fractures of the shaft of the proximal phalanx of the fingers in industrial workers. J Hand Surg Eur. 2008;33:552–6. doi: 10.1177/1753193408090130. [DOI] [PubMed] [Google Scholar]
- 22.Hornbach EE, Cohen MS. Closed reduction and percutaneous pinning of fractures of the proximal phalanx. J Hand Surg Br. 2001;26:45–9. doi: 10.1054/jhsb.2000.0524. [DOI] [PubMed] [Google Scholar]


