Abstract
Background:
The neglected femoral neck fracture is one where there has been a delay of more than 30 days to seek medical help from the time of the original injury. Salvage procedures, such as osteotomy and other treatment options such as vascularized and nonvascularized bone grafts have high failure rates and arthroplasty procedures are not ideal, given the patient's young age and higher levels of activity. We designed a hollow bone graft dynamic hip screw (Hb-DHS) (modified DHS, Hb-DHS) for use in neglected femoral neck fractures. This study evaluates the efficacy and safety of the modified dynamic hip screw (DHS) with autogenous bone and bone morphogenetic protein 2 (BMP-2) composite materials grafting for the treatment of the neglected femoral neck fractures.
Materials and Methods:
A prospective study was carried out in twenty patients of neglected femoral neck fractures treated with the modified DHS with autogenous bone and BMP-2 composite materials grafting between July 2007 and February 2010. There were 14 men and 6 women with a mean age of 29.6 years (range 19–42 years). The mean time from injury to surgery was 9.7 weeks (range 6–16 weeks). The operation time, intraoperative blood loss, fracture healing time, Harris scoring for hip function and complications were recorded to evaluate treatment effects.
Results:
The mean operation time was 75.8 min (range 55–100 min) with mean intraoperative blood loss volume of 105 mL (range 70–220 mL). The mean time to union was 17 weeks (range 12–24 weeks). One patient did not achieve union, and two patients had avascular necrosis of the femoral head. This patient with nonunion underwent intertrochanteric osteotomy. In patients with avascular necrosis one required total hip arthroplasty, the other did not require intervention at the last followup. A total of 14 patients (70%) had excellent results, 2 (10%) had good, 1 (5%) had moderate and 3 (15%) had poor results.
Conclusion:
The modified DHS with autogenous bone and BMP-2 composite materials grafting for the treatment of neglected femoral neck fractures waseffective and had less complications.
Keywords: Bone graft, dynamic hip screw, femoral neck fractures, fixation, bone morphogenic protein
MeSH terms: Femur, femoral neck fractures, autograft, bone screws
INTRODUCTION
The neglected femoral neck fracture is one where there has been a delay of more than 30 days to seek medical help from the time of the original injury.1 This complication may lead to collapse of the femoral head and osteoarthritis. Salvage procedures, such as osteotomy and other treatment options such as vascularized and nonvascularized bone grafts have high failure rates and arthroplasty procedures are not ideal, given the patient's young age and higher levels of activity.2,3 We designed a hollow bone graft dynamic hip screw (Hb-DHS) (modified DHS, Hb-DHS) for use in neglected femoral neck fractures. It was shown in previous study that the Hb-DHS promotes femoral neck bone union, stimulates trabecular bone formation, increases bone mineral density with reliable internal fixation in an experimental study.4 Thus nonunion and femoral head avascular necrosis could be greatly decreased. The purpose of this study was to evaluate the efficacy and safety of the Hb-DHS with autogenous bone and bone morphogenetic protein 2 (BMP-2) composite materials grafting for the treatment of the neglected femoral neck fractures in young adults.
MATERIALS AND METHODS
Implant details
We have designed a Hb-DHS, for which we have obtained a patent (patent number: 201110146729.6). This device is made of titanium alloy and is divided into a head, middle and end sections. The head section, which is threaded and has some holes in it, is used to fix the femoral head. Autogenous bone and BMP-2 composite materials are inserted into the middle section, which has a flabellum-like-cavity. The diameter of the head and middle sections are 13 mm. The end section is inserted into a 135° angle plate [Figure 1].
Figure 1.
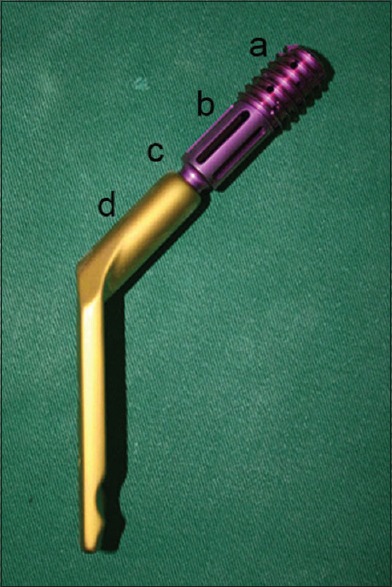
Clinical photograph of hollow-bone-graft dynamic hip screws. (a) The head section, which is threaded and has some holes in it, is used to fix the femoral head. (b) The middle section, which has a flabellum-like-cavity for autogenous bone and bone morphogenetic protein 2 composite materials. (c) The end section, which connects 135° angle plate. (d) The 135° angle plate
20 patients of neglected femoral neck fractures were treated with the modified DHS with autogenous bone and BMP-2 composite materials grafting from July 2007 to February 2010. There were 14 men and 6 women with a mean age of 29.6 years (range 19–42 years). 11 patients had right side involvement and 9 patients had a left side involvement. The mode of trauma included motor vehicle accident (n = 11), fall from height (n = 9). The mean time from injury to surgery was 9.7 weeks (range 6–16 weeks). Sandhu's classification was used in the classification of the fractures.5 There were 11 patients of stage I and 9 in stage II [Table 1]. The study was approved by the ethics committee. Anteroposterior and lateral radiographs of the hip joint were taken in all patients and computerized tomography examinations were obtained if necessary.
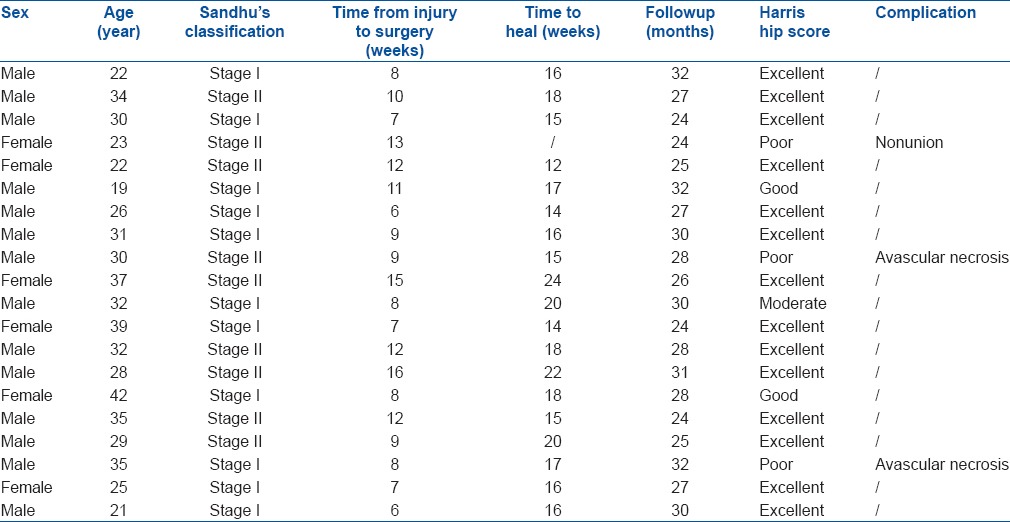
Table 1.
Clinical details of patients
Operative procedure
All the patients were operated using fracture table in supine position under general or spinal anesthesia through anterolateral Watson–Jones approach. After fracture reduction under direct vision, the capsular incision was not closed. Satisfactory reduction (<5 mm of displacement and/or <10° of angulation in any plane) was confirmed by fluoroscopy before internal fixation. A 2.0 mm guide wire using an appropriate angle guide, (usually 125°–135°), was introduced at the level of the lesser trochanter. It is important that the wire should not be positioned too anteriorly or posteriorly from its entry portal and should be central in the femoral head on the anteroposterior and the lateral X-rays into the femoral head. A triple reamer type device reams a path for the screw into the femoral head and also the lateral cortex for the plate barrel junction. The autogenous iliac-crest graft and BMP-2 (Hangzhou Jiuyuan Gene Engineering Co., Ltd., Hangzhou, China) composite materials were filled into the flabellum-like-cavity of a Hb-DHS [Figure 2], and fixation was achieved with Hb-DHS. Addition of a derotational screw placed in the cranial part of the femoral neck superior to the Hb-DHS in all the patients can improve the rotational stability of the construct.
Figure 2.

Clinical photograph of the autogenous bone and bone morphogenetic protein 2 composite materials filled into hollow-bone-graft dynamic hip screws
Postoperative treatment and followup assessment
Patients were mobilized and instructed to use toe-touch weight-bearing with crutches or a walker for 12 weeks. Patients progressed to full weight-bearing when they had the strength and the balance to do so. They were instructed to wean off from crutch support when they were able to walk without a substantial limp.7 They were called for followup at 6 months, 1 year and 2 years.
Clinically they were assessed for pain, limitations of movements and limb length discrepancy. Radiologically the degree of union, loss of fracture alignment, trabecular integrity at the fracture site, late segmental collapse and the presence of avascular necrosis were observed. Avascular necrosis was assessed according to criteria of Ficat.8 Patients were evaluated by the Harris hip scoring system.9
RESULTS
The mean followup period was 27.7 months (range 24–32 months). There were no intraoperative complications related to this technique. The mean operation time was 75.8 minutes (range 55-100 minutes) with mean intraoperative blood loss volume of 105 mL (range 70–220 mL). The direct radiography of all patients showed that the position of the implants was good and the screw did not pull out of the femoral head. In postoperative radiographs the quality of femoral neck reduction was assessed by Haidukewych et al.10 Fracture reduction was classified as excellent (<2 mm of displacement and <5° of angulation in any plane), good (2–5 mm of displacement and/or 5°–10° of angulation), fair (>5–10 mm of displacement and/or >10°–20° of angulation), or poor (>10 mm of displacement and/or >20° of angulation, or any varus). Postoperative success of implant placement was excellent in fifteen cases, good in three and fair in two cases.
The mean time to union was 17 weeks (range 12–24 weeks) [Figures 3A–D and 4]. One patient (stage II) did not achieve union and two patients (one was stage I and other was stage II) had avascular necrosis of the femoral head during their followup. The patient with nonunion was taken up for intertrochanteric osteotomy in the 12th postoperative month. This patient was considered as having a poor outcome. The patient with avascular necrosis stage II required total hip replacement while the other did not require any intervention till the last followup. These were considered as poor outcome [Table 1].
Figure 3A.
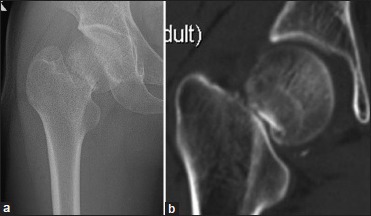
Radiographs of a right femoral neck fracture in a man aged 22 years. The time from injury to surgery was 8 weeks. (a and b) Preoperative X-ray and computerized tomography showing nonunion in femoral neck fracture
Figure 3D.

(a and b) Computerized tomography at 16 weeks after surgery
Figure 4.

(a) Preoperative x-ray showing femoral neck fracture in a man aged 21 years. The time from injury to surgery was 6 weeks (b) X-ray anteroposterior view on the day of surgery (c) X-ray anteroposterior view at 16 weeks post surgery showing union (d-f) CT at 16 weeks post surgery showing union
Figure 3B.
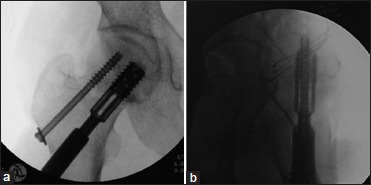
(a and b) Peroperative fluoroscopic view anteroposterior and lateral showing reduction and implant in situ
Figure 3C.
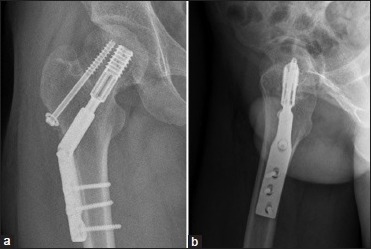
(a and b) The anteroposterior and lateral position X-ray at 16 weeks after surgery showing union
According to the Harris hip score, 14 patients (70%) had excellent results, 2 (10%) had good, 1 (5%) had moderate and 3 (15%) had poor results [Table 1].
DISCUSSION
Salvaging the femoral head for young adults (age <60 years) with neglected femoral neck fracture is challenging. In geriatric patients (age ≥60 years), hemiarthroplasty or total hip arthroplasty often results in a satisfactory outcome. In younger patients, joint replacements are less ideal because of higher functional demands. The beneficial effects of valgus osteotomy, fibular grafting with internal fixation, vascularized bone grafting and muscle pedicle bone grafting in enhancing and promoting union of neglected femoral neck fractures has been documented in the literature.1,3,11 However, valgus osteotomy has two important problems. Shortening, limp and a decreased range of movement are common, probably because of increased pressures on the femoral head leading to degenerative disease or osteonecrosis. Second, there is potential risk of nonunion at the osteotomy site. Fibular grafting with internal fixation, vascularized bone grafting and muscle pedicle bone grafting have donor site complications plus these techniques are highly technical and require microsurgical facilities and experience.12
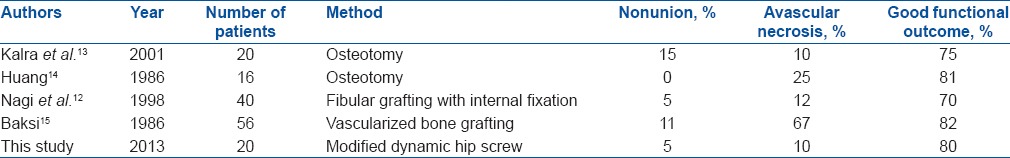
In consideration of the above, our research group designed a new device in collaboration with Double Engine Medical Material Co. Ltd., (Xiamen, China) to produce it. The device is an improved DHS. The head section of the Hb-DHS is threaded, has some holes and is used to fix the femoral head, possibly with less capsular and intramedullary pressure than there is with the traditional DHS. The middle section of the Hb-DHS has a flabellum-like-cavity into which autogenous bone and BMP-2 composite materials are inserted to decrease nonunion and chances of femoral head AVN and also to promote creeping substitution of bone and to some extent, augment bone trabecular volume and bone mineral density. Moreover, the diameter of the head and middle sections are 13 mm, which is significantly greater than for the traditional DHS and therefore provides reliable internal fixation. The end section of the Hb-DHS inserts into a 135° angle plate. In this study, the method involved the use of autogenous iliac-crest graft and BMP-2 composite materials which promote fracture healing. The “two in one” mode of bone grafting with autogenous iliac-crest graft and BMP-2 enhances stimulation of bone induction. The overall rate of nonunion for patients in this series was 5%. Regarding avascular necrosis, the overall rate in our series was 10%. Meanwhile, the reoperation rate in our series was 10%. Compariing with available literature [Table 2], this study showed a low incidence of nonunion and femoral head AVN in the treatment of neglected femoral neck fractures.13,14,15
Table 2.
Neglected femoral neck fractures in young adults - a comparison of the literatures
However, once bone healing has occurred, Hb-DHS may have certain drawbacks in that it would be more difficult to remove than other internal devices. In the future, it may be possible to substitute absorbable materials such as porous tantalum for the titanium alloy. In addition our study sample size is low, the long term curative effect requires further research.
In summary, our study demonstrates that the modified DHS with autogenous bone and BMP-2 composite materials grafting show a low incidence of nonunion and femoral head avascular necrosis complication, and is suitable for the treatment of the neglected femoral neck fractures in young adults.
Footnotes
Source of Support: The study was supported by key projects from Nanjing Military Region (no. 10MA073)
Conflict of Interest: None.
REFERENCES
- 1.Roshan A, Ram S. The neglected femoral neck fracture in young adults: Review of a challenging problem. Clin Med Res. 2008;6:33–9. doi: 10.3121/cmr.2008.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sandhu HS, Sandhu PS, Kapoor A. Neglected fractured neck of the femur: A predictive classification and treatment by osteosynthesis. Clin Orthop Relat Res. 2005:14–20. [PubMed] [Google Scholar]
- 3.Kapoor A, Deety LV, John VZ, Devadoss S, Devadoss A. Management of neglected femoral neck fractures and nonunions using a novel triple surgery combination: An Indian experience. Int J Low Extrem Wounds. 2012;11:49–58. doi: 10.1177/1534734612438056. [DOI] [PubMed] [Google Scholar]
- 4.Shen JZ, Yao JF, Lin DS, Lian KJ, Ding ZQ, Lin B, et al. Hollow-bone-graft dynamic hip screw can fix and promote bone union after femoral neck fracture: An experimental research. Int J Med Sci. 2012;9:916–22. doi: 10.7150/ijms.4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandhu HS. Management of fracture neck of femur. Indian J Orthop. 2005;39:130–6. [Google Scholar]
- 6.Andrew H, Crenshaw JR. Surgical techniques and approaches. In: Canale ST, editor. Campbell's Operative Orthopaedics. 10th ed. Vol. 1. Philadelphia: Mosby Company; 2003. pp. 61–2. [Google Scholar]
- 7.Lin D, Lian K, Ding Z, Zhai W, Hong J. Proximal femoral locking plate with cannulated screws for the treatment of femoral neck fractures. Orthopedics. 2012;35:e1–5. doi: 10.3928/01477447-20111122-08. [DOI] [PubMed] [Google Scholar]
- 8.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 9.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. [PubMed] [Google Scholar]
- 10.Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am. 2004;86:1711–6. doi: 10.2106/00004623-200408000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Kainth GS, Yuvarajan P, Maini L, Kumar V. Neglected femoral neck fractures in adults. J Orthop Surg (Hong Kong) 2011;19:13–7. doi: 10.1177/230949901101900104. [DOI] [PubMed] [Google Scholar]
- 12.Nagi ON, Dhillon MS, Goni VG. Open reduction, internal fixation and fibular autografting for neglected fracture of the femoral neck. J Bone Joint Surg Br. 1998;80:798–804. doi: 10.1302/0301-620x.80b5.8703. [DOI] [PubMed] [Google Scholar]
- 13.Kalra M, Anand S. Valgus intertrochanteric osteotomy for neglected femoral neck fractures in young adults. Int Orthop. 2001;25:363–6. doi: 10.1007/s002640100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang CH. Treatment of neglected femoral neck fractures in young adults. Clin Orthop Relat Res. 1986:117–26. [PubMed] [Google Scholar]
- 15.Baksi DP. Internal fixation of ununited femoral neck fractures combined with muscle-pedicle bone grafting. J Bone Joint Surg Br. 1986;68:239–45. doi: 10.1302/0301-620X.68B2.3958010. [DOI] [PubMed] [Google Scholar]


