Abstract
Objectives
To determine whether there is an Appalachian disparity in caries prevalence or extent in children living in Pennsylvania.
Methods
We conducted a cross-sectional clinical assessment of caries in a sample representing 1st, 3rd, 9th, and 11th grade students across Pennsylvania. We used logistic regression and zero-inflated negative binomial regression controlling for age to examine the association of residence in an Appalachian county with caries prevalence and extent in the primary and permanent dentitions.
Results
Compared with children living outside Appalachia, more children living in Appalachia had a dft > 0 (OR = 1.37, 95% CI = 1.07 – 1.76) and more had a DMFT > 0 (OR = 1.32, 95% CI = 1.06 – 1.64). In addition, compared with children living outside Appalachia, children living in Appalachia had a greater primary but not permanent caries extent (IRR = 1.10, 95% CI = 1.01 – 1.19).
Conclusions
We found Appalachian disparities in caries prevalence in both the primary and permanent dentitions and an Appalachian disparity in caries extent in the primary dentition. None of the disparities was moderated by age. This suggests that the search for the mechanism or mechanisms for the Appalachian disparities should focus on differential exposures to risk factors occurring prior to and at the start of elementary school.
Keywords: dental caries, child, adolescent, Appalachia region
When the health of members of one group is worse than the health of members of a reference group, we say there is a health disparity (1). Health disparities can be measured using many different indicators (1), with disparities in disease prevalence being a commonly-used indicator. A disparity in prevalence occurs when more people in a comparison group have disease than do people in a reference group. Disparities can also be examined using measures of the extent of disease. When there is a disparity in extent of caries, the people in the comparison group have more carious lesions than the people in the reference group have.
The main reason to identify disparities is to facilitate their elimination. Finding a disparity defined by membership in a particular group suggests that exposure or susceptibility to disease-causing risk factors in that group differs in some way from exposure to these risk factors in the reference group. To the extent that these differences in exposure to risk factors can be identified, interventions targeting the specific risk factors can be devised to reduce the disparity. However, sometimes the risk factors are not so easy to identify. In such cases, determining the onset of the disparity may be informative. For example, at the population level the onset of dental caries may begin prior to the start of elementary school, whereas a disparity between groups in caries prevalence might not be seen until children are differentially exposed to a risk factor after starting school. Identifying the onset of a disparity can help narrow the range of possible risk factors to those occurring at the right time and can help identify the time before which a preventive intervention would need to begin.
In addition, if the risk factors affecting disease susceptibility differ from the risk factors affecting extent of disease, a disparity in extent could occur whether or not there is also a disparity in prevalence and vice versa. For example, it is possible for the same percentage of people in both populations to be affected, but the affected people in the comparison population could have more disease, on average, than the affected people in the reference population. Thus, identifying disparities in different outcomes, such as prevalence and extent, may help us pinpoint where to look for differences in risk factors and what kinds of difference to look for across different communities.
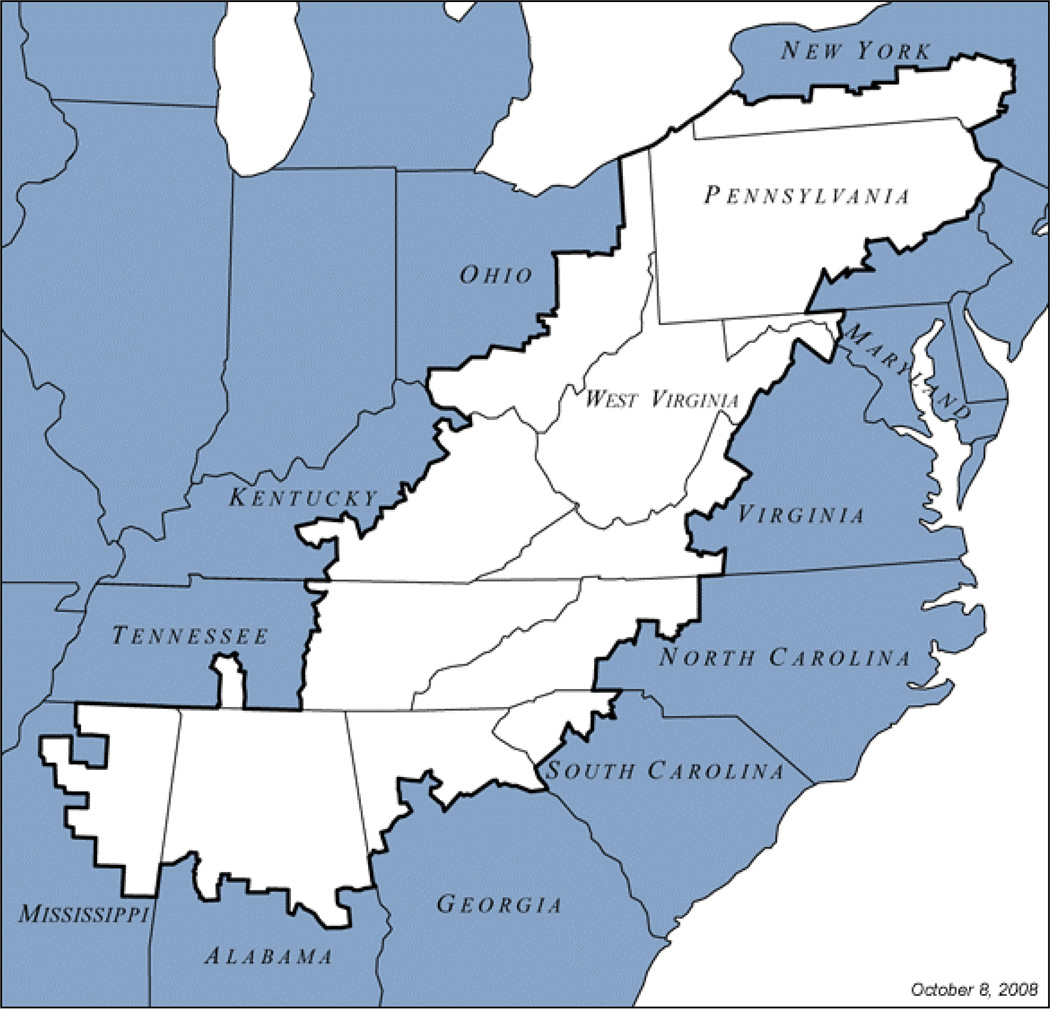
Residence in Appalachia, a region in the eastern United States along the Appalachian mountain range from southern New York to northern Mississippi, is one defined group of particular interest. Appalachia encompasses all or part of 13 states (Figure 1, (2)). Economically, the Appalachian region is diverse. Although some parts are economically thriving, other parts have high levels of poverty, unemployment, under-education, and poor health, including oral health. Both adults and children living in the less-well-off parts of Appalachia have worse oral health than people in much of the rest of the country (3–9). For example, with respect to caries in children, several papers have reported Appalachian disparities in prevalence over the years. In 1998, 65.6% of children age 8 in West Virginia, which is entirely within Appalachia, had dental caries (6) compared with 53.2% in the nation as a whole (10). In 2011, the state dental director of Kentucky reported continued high incidence of dental caries in five- and six-year-olds in the Appalachian part of the state (9). This suggests that in states which are not entirely within Appalachia, Appalachian disparities can occur within a state. In the United States, many policies affecting oral health are created and implemented at the state level. The presence of within-state disparities would raise questions about the source of those disparities and appropriate interventions to address disparities within states.
Figure 1.
Map of Appalachian region.
The purpose of this paper is to determine whether there are Appalachian disparities in dental caries prevalence (i.e., percent of children with dft > 0 or DMFT > 0) and extent (i.e., dft or DMFT) in a representative study population of children drawn from all public schoolchildren in Pennsylvania. We examined these relationships in a cross-sectional sample of children and adolescents selected from grades 1, 3, 9, and 11.
Materials and Methods
Study Design
Data for this study were collected as part of the Pennsylvania Oral Health Needs Assessment (PaOHNA), which began data collection in September 1998 and concluded data collection in May 2000. The PaOHNA was a state-wide, school-based screening survey. As is typical for surveys such as these, basic information about adolescents’ oral health was obtained to guide state-level policy and planning. The PaOHNA collected data on a sample of 6040 public school children and adolescents in grades 1, 3, 9, and 11. The study design was cross-sectional.
The sample for the PaOHNA was obtained using a stratified, three-stage, probability proportional to size selection of classrooms within schools within school districts from the public school system of Pennsylvania with stratification on eight Dental Health Districts (including six state regions, Philadelphia, and Pittsburgh), and school district enrollment as a proxy for urban/rural status. Although stratification did not directly address the Appalachian/non-Appalachian status of school districts, the regional stratification along with the random probability proportional to size sampling of school districts contributed to good representation of Appalachian and non-Appalachian child populations, especially in this situation where the Appalachian population is not a proportionally small sub-population. Due to missing data for calculating analysis weights, 11 children were dropped from the analysis. Institutional Review Board approval was obtained from the University of Pittsburgh prior to initiation of this study. The parent or guardian of each child or adolescent selected for the study provided consent, either active or passive depending on the policy of the individual school, prior to study participation.
Clinical Assessment
Each child and adolescent received a clinical assessment by a licensed dental hygienist using portable dental equipment in the selected schools. Details of the training and calibration of examiners and of the clinical protocols have been reported elsewhere (11). Strict infection control guidelines recommended by CDC (Bloodborne Pathogens Standard), OSHA, and the American Dental Association were followed at all times. Parents were given a report of findings via the school nurse, and referrals for dental care were provided when needed.
Each tooth was assessed for caries, restorations, and dental sealants. Explorers were not used. Using a modified version of the NHANES III criteria (12, 13), examiners recorded the numbers of teeth that were filled, carious, or missing. A tooth was classified as carious if on a smooth surface there was visual evidence of cavitation (i.e., a break in the enamel surface) or if on the occlusal surface there was evidence of cavitation or undermined enamel, which included frosting or shadowing of the enamel. White spots and non-occlusal pre-cavitated lesions were not assessed. Due to the survey’s focus on treatment needs, the number of sound teeth was not recorded. Thus, the total number of teeth cannot be determined. Third molars were not included in this study. For each child and adolescent, the numbers of decayed (d) and filled (f) primary teeth and decayed (D), missing (M), and filled (F) permanent teeth were determined. These were summed to create dft and DMFT measures. These variables were used in the analyses of caries extent. Thus, our definition of caries extent includes both carious and filled teeth.
Appalachian Status
Children were considered to reside in Appalachia if their school was located in a county listed by the Appalachian Regional Commission as being located within Appalachia (http://www.arc.gov/counties, accessed November 5, 2008). Because the sampling was stratified by region and schools were selected probability proportional to size, Appalachian schools statistically would be represented proportionally in the sample, and thus Appalachian children should be represented proportionately to the state population distribution.
Data Entry and Statistical Analysis
Details of data management and the training and calibration of the examiners, including inter- and intra-examiner reliability have been reported elsewhere (11).
To describe caries prevalence, we presented the percentages and corresponding 95% confidence intervals [CI] for all children in Pennsylvania, children living in the Appalachian counties of Pennsylvania, and children living in the non-Appalachian counties in Pennsylvania. To examine the associations of age and Appalachian residence with caries prevalence, we used logistic regression. These results are presented as risk estimates (odds ratio [OR]) and corresponding 95% CI and p-values.
For children with caries, caries extent was described as median (interquartile range [IQR]) for all children in Pennsylvania and for children living within and not within Appalachian counties. To examine the associations of age and Appalachian residence with caries extent (i.e., dft, DMFT), among children with or without caries, we used zero-inflated negative binomial regression. We accounted for non-linearity of age using quadratic or cubic terms as needed. These results are presented as risk estimates (incidence rate ratio [IRR]) and corresponding 95% CI and p-values. Zero-inflated negative binomial regression is used when the distribution of the outcome variable (i.e., dft and DMFT) meets the requirements that there is an “excess” of zeroes and the mean is greater than the variance. In our data, these requirements are met. In this modeling approach, logistic regression is used to model the association between a predictor and the probability that someone is susceptible to caries. Simultaneously and jointly, negative binomial regression is used to determine the strength of association between a predictor and amount of carious lesions (i.e., extent). Separate equations, each with their own predictors, are written for the two different portions of the model. Predictors identified as significant in the logistic regression analyses of caries prevalence were incorporated into the logistic regression (inflated) portions of the zero-inflated negative binomial regression analyses. Simultaneously, age and Appalachian residence were tested as predictors in the negative binomial portion of the model.
Sample weights were included in all analyses to account for unequal selection probabilities and nonresponse. We considered differences to be statistically significant at P < 0.05. All analyses were conducted in STATA 12.1 (StataCorp, College Station, TX).
Results
According to census data from 2000, the total population in the Commonwealth of Pennsylvania was 12,281,054; whereas, the total population in the Appalachian portion of Pennsylvania was 5,819,800 (47.4%). Compared with the Appalachian portion of the state, the non-Appalachian portion had a smaller percentage who were less than a high school graduate and larger percentages with a Bachelor’s, Master’s or professional school degrees (Table 1). Within each level of schooling, age was evenly distributed (Table 2). Children with primary dentition had a weighted mean age of 8. Children with permanent dentition had a weighted mean age of 11.
Table 1.
Percentages of demographic variables by Appalachian and Non-Appalachian residence in Pennsylvania.
| Demographic variable | Appalachian (M, SD) |
Non-Appalachian (M, SD) |
t-test | ||
|---|---|---|---|---|---|
| Population density per square mile | 163.8 | 249.8 | 1,456.3 | 2,796.9 | 1.79 |
| Less than high school graduate | 19.4 | 3.5 | 18.1 | 5.1 | −1.12 |
| High school graduate (including equivalency) | 46.1 | 4.5 | 36.8 | 6.0 | −6.57*** |
| Some college | 19.6 | 3.1 | 21.1 | 2.3 | 1.80 |
| Bachelor’s degree | 9.4 | 2.8 | 15.1 | 5.2 | 4.02** |
| Master’s degree | 3.6 | 1.4 | 5.9 | 2.1 | 3.95** |
| Professional school degree | 1.3 | 0.6 | 2.1 | 0.8 | 4.95*** |
| Doctorate degree | 0.6 | .8 | 1.0 | 0.5 | 1.76 |
Note.
< .001;
< .0001.
Table 2.
Percentage of children by age.
| Age (y) | Percentage (%) |
|---|---|
| Primary Dentition | |
| 5 | 0.08 |
| 6 | 25 |
| 7 | 24 |
| 8 | 25 |
| 9 | 25 |
| 10 | 2 |
| Permanent Dentition | |
| 5 | 0.04 |
| 6 | 14 |
| 7 | 13 |
| 8 | 14 |
| 9 | 14 |
| 10 | 1 |
| 11 | 0 |
| 12 | 0 |
| 13 | .08 |
| 14 | 11 |
| 15 | 12 |
| 16 | 11 |
| 17 | 10 |
| 18 | 1 |
| 19 | .06 |
| 20 | .04 |
| 21 | .03 |
Prevalence in Pennsylvania
In the primary dentition group, 46.4% of the children had a dft > 0 (95% CI = 43.24 – 49.61). In the permanent dentition group, 31.2% of the children had a DMFT > 0 (95% CI = 29.06 – 33.32). In the primary dentition, the odds of having caries (i.e., prevalence) were 8% higher for each additional year of age (OR = 1.08, 95% CI = 1.01–1.16). In the permanent dentition, the odds of having caries were 103% higher for each additional year of age (OR = 2.03, 95% CI = 1.67 – 2.47), and the model included terms for both age and age2.
Appalachian Disparities in Caries Prevalence
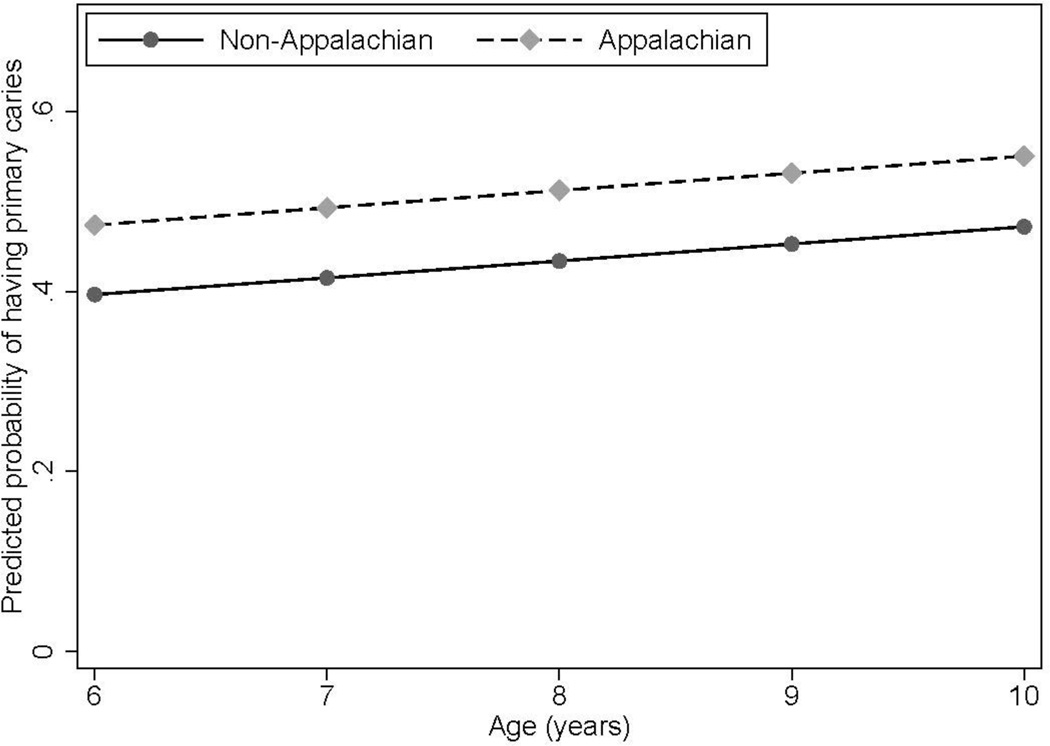
In the primary dentition, 43% of the children living outside Appalachia had a dft > 0 (95% CI = 38.88 – 46.3); and 50.4% of the children living in Appalachia had a dft > 0 (95% CI = 45.39 – 55.36; Table 3). After controlling for age, compared with children living outside Appalachia, more children living in Appalachia had a dft > 0 (OR = 1.37, 95% CI = 1.07 – 1.76; Table 4 and Figure 1). There was no interaction of age by Appalachian residency (P = 0.61).
Table 3.
Prevalence and extent by residence in an Appalachian county in Pennsylvania.
| Variable | Appalachian counties |
Non-Appalachian counties |
|---|---|---|
| Sample, N | 2930 | 3099 |
| Weighted population, N | 228,569.46 | 235,623.12 |
| dft | ||
| Prevalence, % | 50.38 | 42.55 |
| Extent in all children, mean±SD | 1.87±2.54 | 1.47±2.28 |
| Extent in children with caries, mean±SD | 3.72±2.44 | 3.45±2.29 |
| DMFT | ||
| Prevalence, % | 33.58 | 28.8 |
| Extent in all children, mean±SD | 1.14±2.25 | 0.94±2.00 |
| Extent in children with caries, mean±SD | 3.39±2.73 | 3.25±2.53 |
Table 4.
Odds ratio and 95% confidence interval for prevalence of dft and DMFT in Pennsylvania
| Predictor | Odds ratio (95% CI) | p-value |
|---|---|---|
| dft | ||
| Appalachian counties (vs. Non-Appalachian counties) | 1.37 (1.07–1.76) | 0.015 |
| Age, years (per 1 year increase) | 1.08 (1.01–1.15) | 0.025 |
| DMFT | ||
| Appalachian counties (vs. Non-Appalachian counties) | 1.32 (1.06–1.64) | 0.012 |
| Age, years (per 1 year increase)a | 2.03 (1.67–2.47) | <0.001 |
Note.
Risk estimate was calculated using age and age2 risk estimates (OR=2.07 95% CI=1.69–2.54 for age; OR=0.98 95% CI=0.97–0.99 for age2).
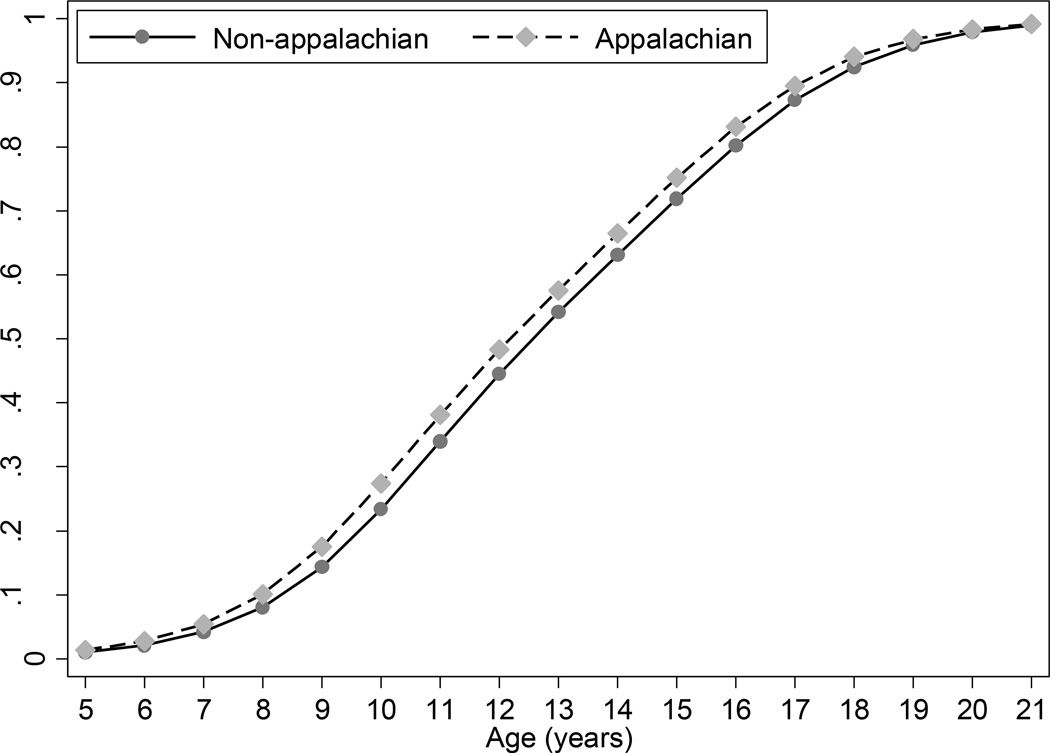
In the permanent dentition, 29% of the children living outside Appalachia had a DMFT > 0 (95% CI = 26.03 – 31.74); and 34% of the children living in Appalachia had a DMFT > 0 (95% CI = 30.46 – 36.85; Table 3). After controlling for age and age2, compared with children living outside Appalachia, more children living in Appalachia had a DMFT > 0 (OR = 1.32, 95% CI = 1.06 – 1.64; Table 4 and Figure 2). There was no interaction of age by Appalachian residency (P = 0.82).
Figure 2.
Predicted probability of primary caries prevalence by age and Appalachian residency.
Caries Extent in Pennsylvania
Of the children with a dft > 0, the median number of primary teeth with caries experience (decayed or filled) was 3 (IQR = 2 – 5). Of the children with a DMFT > 0, the median number of permanent teeth with caries experience (decayed, filled, or missing due to caries) was 2 (IQR = 1 – 4). In the primary dentition after adjusting for age and Appalachian residency in the logistic regression portion of the model, being older was associated with protection against higher caries extent in the negative binomial portion of the model (IRR = 0.96, 95% CI = 0.92 – 0.99). In the permanent dentition after adjusting for age, age2, and Appalachian residency in the logistic regression portion of the model, being older was associated with greater caries extent in the negative binomial portion of the model (IRR = 1.14, 95% CI = 1.12 – 1.16).
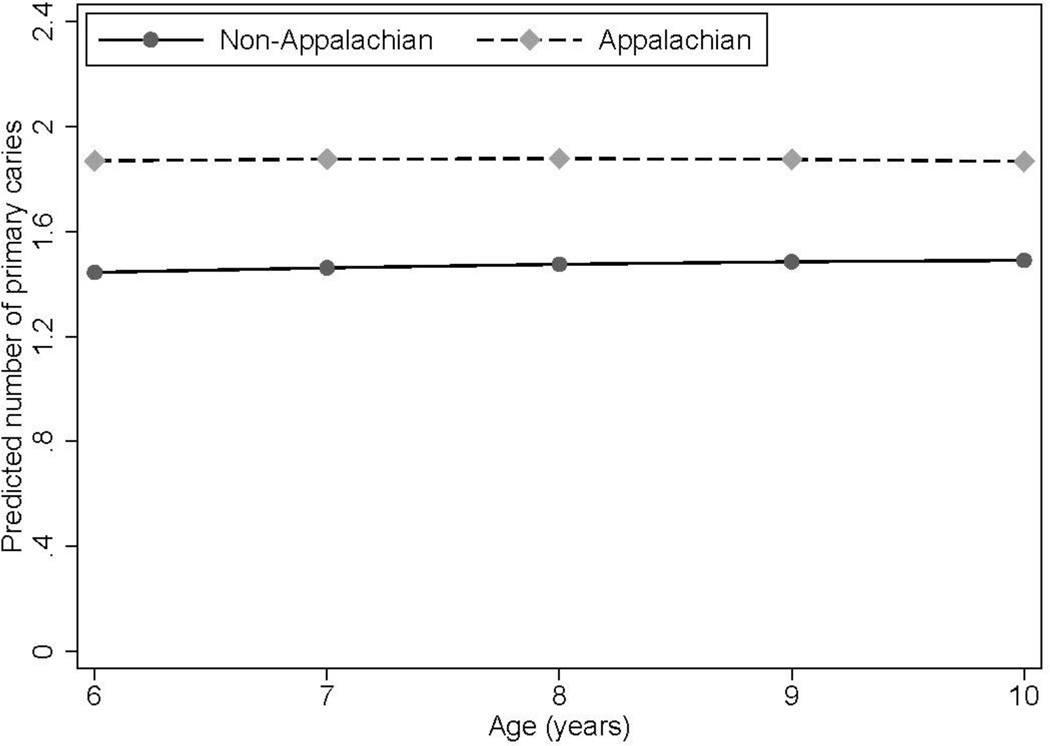
Appalachian Disparities in Caries Extent
Of the children with a dft > 0, the median number of primary teeth with caries experience (decayed or filled) was 3 (IQR = 2 – 5) both in Appalachia and outside Appalachia (Table 3). Of the children with a DMFT > 0, the median number of permanent teeth with caries experience (decayed, filled, or missing due to caries) was 3 (IQR = 1 – 4) in Appalachia and was 2 (IQR = 1 – 4) outside Appalachia (Table 3). In the primary dentition, after adjusting for age and Appalachian residency in the logistic portion of the model and age in the negative binomial portion of the model, compared with children living outside Appalachia, children living in Appalachia had greater caries extent (IRR = 1.10, 95% CI = 1.01 – 1.19; Table 5 and Figure 3). There was no interaction of age by Appalachian residency (p = .26). In the permanent dentition, after adjusting for age, age2, and Appalachian residency in the logistic portion of the model and age in the negative binomial portion of the model, Appalachian residency was not associated with caries extent (IRR = 1.07, 95% CI = 0.95 – 1.22; p = 0.27).
Table 5.
Incidence rate ratio and 95% confidence interval for extent of dft and DMFT in Pennsylvania
| Caries Extent | ||
|---|---|---|
| Predictor | IRR (95% CI) | p-value |
| dfta | ||
| Appalachian counties (vs. Non-Appalachian counties) | 1.10 (1.01–1.19) | 0.024 |
| Age, years (per 1 year increase) | 0.96 (0.92–0.99) | 0.012 |
| DMFTb | ||
| Appalachian counties (vs. Non-Appalachian counties) | 1.07 (0.95–1.22) | 0.27 |
| Age, years (per 1 year increase) | 1.14 (1.12–1.16) | <0.001 |
Note.
Adjusted for age and Appalachian residency in the logistic portion of the model.
Adjusted for age, age2, and Appalachian residency in the logistic portion of the model.
Figure 2.
Predicted probability of permanent caries prevalence by age and Appalachian residency.
Discussion
The purpose of this paper was to determine whether there were Appalachian disparities in dental caries prevalence or extent in children living in Pennsylvania. We found disparities between Appalachian residents and residents of non-Appalachian counties in caries prevalence in both the primary and permanent dentitions and a disparity in caries extent in the primary but not the permanent dentition. None of the disparities was moderated by an interaction with age, which suggests that compared with younger children, the disparities were neither larger nor smaller in older children.
To our knowledge, only one report has included information about exposures that could possibly cause Appalachian disparities in the oral health of children (9). In this report, data were compiled from several national surveys; clinical examinations were not conducted. As reported by states in the Community Water System (14), ten of the 13 states composing Appalachia, but not Pennsylvania, ranked in the top 20 nationwide in terms of percentage of population with fluoridated water. Thus, some people in Pennsylvania are not exposed to fluoridated water. If water fluoridation varies within Pennsylvania, it is possible that differential exposure to water fluoridation could account for the Appalachian disparities in prevalence and extent that we obtained. The other outcome relevant to children examined in the report was the percentage of children using preventive dental services as measured by the CDC’s National Survey of Children’s Health (15) in 2007. The study authors found that the Pennsylvania percentage was close to the national average. Thus, future studies should examine whether within Pennsylvania differential exposure to preventive dental services can account for the Appalachian disparity in caries extent we obtained. Finally, the report found that much of the Appalachian disparity could be accounted for by differences in socioeconomic status. Furthermore, research has demonstrated support for the effect of early childhood socioeconomic status on later health outcomes (16). Thus, future studies should examine whether within Pennsylvania socioeconomic status varies across Appalachian and non-Appalachian counties. In sum, several possible mechanisms for the disparities have been identified and should be explored.
Most research on the etiology of caries focuses on individual-level factors such as oral hygiene (17), salivary flow (18), diet (19), genes (20), or environmental exposures causing developmental defects of enamel (21, 22). According to Rose, however, “to find the determinants of prevalence and incidence rates, we need to study characteristics of populations, not characteristics of individuals” (23). That we obtained disparities based on a community-level variable like Appalachian residency suggests that there may be community-level factors as well. Many of the individual-level risk factors described above may have community-level sources. For example, although genes influence individuals, members of a community could be similar genetically if, for example, people from the same ethnic heritage, who presumably are genetically similar, choose to live together in neighborhoods and form communities. Similarly, all people living downwind from a coal-fired power plant will share exposure to any environmental toxins produced by that plant. Finally, individual level behaviors, such as daily tooth brushing frequency or drinking sugar-sweetened beverages, are determined in part by community-level social norms regarding the appropriateness of the behavior (24) or policies such as those influencing access to sugar-sweetened beverages. Targeting these community-level factors at their source is more efficient and holds greater potential for prevention than targeting each individual affected by them (25).
Strengths and Limitations
There were several strengths to this study. There is large variability in oral health status from state to state. Relative to states in southern Appalachia, Pennsylvania and other northern Appalachian states reported better oral health on the CDC’s Behavioral Risk Factor Surveillance System from 2005 (9). By using a sample drawn from one state, we were able to control for variability in caries experience due to differences in state-related health policies. Second, by using zero-inflated negative binomial regression, we were able to examine the effect of Appalachian residence on caries extent only among those children who were predicted to be susceptible to caries. Third, the measure of extent of disease was obtained through a clinical assessment and not based on self-report. All three of these strengths reduce the likelihood of making Type II errors.
There are several limitations to this study that should be considered when interpreting the findings. Because the study was designed to assess treatment need, the total number of primary and permanent teeth was not measured. Therefore, we were unable to examine this important variable. As a proxy for total number of primary and permanent teeth, we controlled for age. Future studies should record which teeth are in the mouth and in which teeth and on what surfaces the decay is occurring. This would enable us determine whether there are Appalachian disparities on a surface-by-surface basis. We could also examine whether there are Appalachian disparities in growth and maturation of the dentitions. Similarly, although some of the missing teeth could have been lost to causes other than caries, because we observed very little trauma (data not shown), we do not believe this is a threat to the validity of the dft and DMFT measures. Finally, residence in an Appalachian county does not automatically confer a specific set of exposures. There is variability in the demographics of people living within and outside of Appalachian counties. Similarly, there is variability across Appalachian counties. But given variability, that there are Appalachian disparities suggests that residence in an Appalachian county is likely a proxy for factors that have yet to be identified.
Future Directions
Based on our findings, several next steps should be considered. First, the ages at which the Appalachian disparities in prevalence and extent appear in the primary dentition remain unknown. Thus, the onset of the disparities should be explored in children younger than age 6. Second, pathways through which the three disparities occur should be identified. Third, to clarify causal relationships and change in the predictive value of possible pathways as children age, longitudinal studies should be conducted.
In sum, we identified Appalachian disparities in caries prevalence in the primary and permanent dentitions of children, and an Appalachian disparity in caries extent in the primary but not permanent dentition. Future research should work to identify causes of these disparities. As the causes of these disparities are understood better, more effective prevention interventions can be identified and less disease should occur.
Figure 3.
Predicted probability of primary caries extent by age and Appalachian residency.
Acknowledgements
With thanks to Paul Moore and the members of the Peer-Mentored Research Development Meeting for their thoughtful critique and editing and to the reviewers for their helpful comments in shaping the paper. Deborah Polk was supported by a grant from the National Institutes of Health NICDR K23 DE019485. The research was supported by a grant from the Commonwealth of Pennsylvania, Department of Health.
Reference List
- 1.Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Kim I, Mays V, et al. Methodological issues in measuring health disparities. Vital and Health Statistics: National Center for Health Statistics. 2005 [PMC free article] [PubMed] [Google Scholar]
- 2.Appalachian Regional Commission. The Appalachian Region. 2008 [Google Scholar]
- 3.Halverson JA, Ma L, Harner EJ. An analysis of disparities in health status and access to health care in the Appalachian region. Washington, DC: Appalachian Regional Commission; 2004. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Surveillance for use of preventive health-care services by older adults, 1995 – 1997. MMWR. 1999;48:51–88. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Total tooth loss among persons aged greater than or equal to 65 years - selected states, 1995 – 1997. MMWR. 1999;48:206–210. [Google Scholar]
- 6.Lutfiyya MN, Young D, Medley K, Black G. Epidemiological Snapshot. Charleston, WV: Office of Maternal and Child Health, Division of Research, Evaluation, and Planning, West Virginia Bureau of Public Health; 1999. West Virginia oral needs assessment: Dental survey of school-aged children. [Google Scholar]
- 7.West Virginia Bureau for Public Health. Unpublished data from the 1994 Behavioral Risk Factor Surveillance System. Charleston, WV: West Virginia Department of Health and Human Resources; 1999. [Google Scholar]
- 8.Martin CA, McNeil DW, Crout RJ, Ngan PW, Weyant RJ, Heady HR, et al. Oral health disparities in Appalachia: orthodontic treatment need and demand. Journal of the American Dental Association. 2008;139:598–604. doi: 10.14219/jada.archive.2008.0221. [DOI] [PubMed] [Google Scholar]
- 9.Krause DD, May WL, Lane NM, Cossman JS, Konrad TR. An analysis of oral health disparities and access to services in the Appalachian region. Washington, DC: Appalachian Regional Commission; 2011. [Google Scholar]
- 10.Dye BA, Thornton-Evans G. Trends in oral health by poverty status as measured by Healthy People 2010 objectives. Public Health Reports. 2009;125:817–830. doi: 10.1177/003335491012500609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weyant RJ, Manz M, Corby P. Dental caries status and need for dental treatment of Pennsylvania public school children in grades 1, 3, 9, and 11. Journal of Public Health Dentistry. 2004;64:136–144. doi: 10.1111/j.1752-7325.2004.tb02743.x. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988 – 94. Hyattsville, MD: 1994. [PubMed] [Google Scholar]
- 13.Westat Inc. National Health and Nutrition Examination Survey, III: Manual for dental examiners and dental records, Rev. ed. Rockville, MD: 1992. [Google Scholar]
- 14.Centers for Disease Control and Prevention. State Fluoridation Percentage Calculations and States Ranked by Fluoridation Percentage [Google Scholar]
- 15.National Survey of Children's Health, 2007. Data Resource Center for Child and Adolescent Health [Google Scholar]
- 16.Spencer N, Thanh TM, Louise S. Low income/socio-economic status in early childhood and physical health in later childhood/adolescence: A systematic review. Matern Child Health J. 2013;17:424–431. doi: 10.1007/s10995-012-1010-2. [DOI] [PubMed] [Google Scholar]
- 17.Sutcliffe P. A longitudinal clinical study of oral cleanliness and dental caries in school children. Archives of Oral Biology. 1973;18:765–770. doi: 10.1016/0003-9969(73)90048-4. [DOI] [PubMed] [Google Scholar]
- 18.Leone CW, Oppenheim FG. Physical and chemical aspects of saliva as indicators of risk for dental caries in humans. Journal of Dental Education. 2001;65:1054–1062. [PubMed] [Google Scholar]
- 19.Scheinin A, Makinen KK. Turku sugar studies I – XXI. Acta Odontologica Scandinavica. 1975;33(Suppl 70):1–351. doi: 10.3109/00016357609004651. [DOI] [PubMed] [Google Scholar]
- 20.Shimizu T, Ho B, Deeley K, Briseno-Ruiz J, Faraco IM, Jr, Schupack GI, et al. Enamel formation genes influence enamel microhardness before and after cariogenic challenge. PLoS ONE. 2012;7:e45022. doi: 10.1371/journal.pone.0045022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford D, Seow WK, Kazoullis S, Holcombe T, Newman B. A controlled study of risk factors for enamel hypoplasia in the permanent dentition. Pediatric Dentistry. 2009;31:382–388. [PubMed] [Google Scholar]
- 22.Needleman HL, Allred E, Bellinger D, Leviton A, Rabinowitz M, Iverson K. Antecedents and correlates of hypoplastic enamel defects of primary incisors. Pediatric Dentistry. 1992;14:158–166. [PubMed] [Google Scholar]
- 23.Rose G. Sick individuals and sick populations. International Journal of Epidemiology. 1985;14:32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 24.Perkins JM, Perkins HW, Craig DW. Misperceptions of peer norms as a risk factor for sugar-sweetened beverage consumption among secondary school students. J Am Diet Assoc. 2010;110:1916–1921. doi: 10.1016/j.jada.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz S, Diez-Roux R. Commentary: Causes of incidence and causes of cases - a Durkheimian perspective on Rose. International Journal of Epidemiology. 2001;30:435–439. doi: 10.1093/ije/30.3.435. [DOI] [PubMed] [Google Scholar]