Abstract
Background and purpose
Hip fracture (HF) in frail elderly patients is associated with poor physical recovery and death. There is often postoperative blood loss and the hemoglobin (Hb) threshold for red blood cell (RBC) transfusions in these patients is unknown. We investigated whether RBC transfusion strategies were associated with the degree of physical recovery or with reduced mortality after HF surgery.
Patients and methods
We enrolled 284 consecutive post-surgical HF patients (aged ≥ 65 years) with Hb levels < 11.3 g/dL (7 mmol/L) who had been admitted from nursing homes or sheltered housing. Allocation was stratified by residence. The patients were randomly assigned to either restrictive (Hb < 9.7 g/dL; < 6 mmol/L) or liberal (Hb < 11.3 g/dL; < 7 mmol/L) RBC transfusions given within the first 30 days postoperatively. Follow-up was at 90 days.
Results
No statistically significant differences were found in repeated measures of daily living activities or in 90-day mortality rate between the restrictive group (where 27% died) and the liberal group (where 21% died). Per-protocol 30-day mortality was higher with the restrictive strategy (hazard ratio (HR) = 2.4, 95% CI: 1.1–5.2; p = 0.03). The 90-day mortality rate was higher for nursing home residents in the restrictive transfusion group (36%) than for those in the liberal group (20%) (HR = 2.0, 95% CI: 1.1–3.6; p = 0.01).
Interpretation
According to our Hb thresholds, recovery from physical disabilities in frail elderly hip fracture patients was similar after a restrictive RBC transfusion strategy and after a liberal strategy. Implementation of a liberal RBC transfusion strategy in nursing home residents has the potential to increase survival.
Surgical blood loss leading to acute anemia is common in hip fracture patients (Kumar et al. 2011). The World Health Organization defines anemia as hemoglobin (Hb) levels < 12 g/dL in women and < 13 g/dL in men (WHO 2011). Postoperative anemia in elderly hip fracture patients is associated with reduced ambulation and functional independence (Halm et al. 2004, Foss and Kehlet 2006, Maraldi et al. 2006). Long-term care residents with Hb levels < 10 g/dL (6.2 mmol/L) showed worse performance of activities of daily living (ADL) than residents with levels < 13 g/dL (8.1 mmol/L) (Bailey et al. 2012). Physical recovery and self-scored energy levels after hip fracture repair increase with increasing Hb levels (Lawrence et al. 2003).
In elderly hip fracture patients, 90-day mortality rates vary between 5% and 27% (Foss and Kehlet 2005, Petersen et al. 2006, Bjorkelund et al. 2009, Gregersen et al. 2011), representing a 5- to 8-fold increase in mortality compared to elderly people with no hip fracture (Haentjens et al. 2010). The 90-day mortality rates for nursing home residents after hip fracture are higher in males than in females (32% vs. 18%). Predictors of early death following hip fracture include: residential status, number of comorbidities, functional impairment prior to fracture, cognitive decline, polypharmacy, poor nutritional status, previous hip fracture, delay in surgery, and anemia (van Dijk et al. 2005, Berry et al. 2009, Ryg et al. 2009, Kannegaard et al. 2010, Holvik et al. 2010, Juliebo et al. 2010, Onem et al. 2010, Baker et al. 2011, Kirkland et al. 2011, Moja et al. 2012, Schaller et al. 2012).
Red blood cell (RBC) transfusions are usually given for substantial perioperative blood loss or hemodynamic compromise. In Denmark, RBC transfusions are recommended when Hb levels are < 9.7 g/dL (6 mmol/L) (Danish Health and Medicine Authority 2008). Previous randomized controlled trials (RCTs) have compared RBC transfusion strategies in hip fracture patients with few frail elderly patients included (Foss et al. 2009, Parker 2013). Also, RBC transfusion strategies have been included in meta-analyses that combined the results of mixed populations with regard to age and disease (Carson et al. 2012, Salpeter et al. 2014). A large RCT compared transfusion strategies after surgery in high-risk hip fracture patients, but all the patients could walk independently before fracture. Only 10% of the latter population were nursing home residents, and no separate analysis was performed on this subgroup (Carson et al. 2011). Overall, the researchers found no associations between transfusion strategies, physical recovery, or survival.
Currently, there are no reports in the literature suggesting an optimal Hb target for RBC transfusions specifically for frail, elderly hip fracture patients, regardless of their walking ability. Our aim, therefore, was to examine how RBC transfusion strategies influence physical recovery and mortality in residents from nursing homes and sheltered housing facilities.
Patients and methods
Study design and patients
The present “Transfusion Requirements In Frail Elderly” (TRIFE) study of hip-fractured patients was designed as a prospective, assessor-blinded, randomized controlled trial. Eligible patients from the orthopedic surgical ward at Aarhus University Hospital were enrolled consecutively between January 18, 2010 and June 6, 2013. These patients (aged ≥ 65 years) had been admitted from nursing homes or sheltered housing facilities for unilateral hip fracture surgery and had postoperative Hb levels between 9.7 g/dL (6 mmol/L) and 11.3 g/dL (7 mmol/L) during the first 6 postoperative days. If the Hb value was below 9.7 g/dL on the first day after surgery, the patient was transfused according to the recommendations of the Danish Health and Medicine Authority for elderly hip fracture patients. The home addresses of the patients revealed their eligibility, and provided an unambiguous tool to recruit and allocate them to the 2 transfusion groups on admission to hospital. Hip fractures were categorized as 3 subtypes (International Code of Disease 10; ICD10) according to the location of the fracture line: (1) femoral neck (ICD-10 S72.0); (2) intertrochanteric (ICD-10 S72.1); or (3) subtrochanteric (ICD-10 S72.2). Exclusion criteria were: active cancer, pathological fractures, inability to understand or speak Danish without an interpreter, refusal of RBC transfusion (e.g. Jehovah’s Witness), fluid overload, irregular erythrocyte antibodies, or previous participation in the trial. The project manager enrolled the patients and assigned them to the interventions.
Randomization and blinding
After giving their informed consent, the patients were randomly assigned to either the restrictive RBC transfusion strategy (Hb < 9.7 g/dL; 6 mmol/L) according to the national guidelines, or the liberal strategy (Hb < 11.3 g/dL; 7 mmol/L) according to results of a previous observational study on tailored interventions that used the same liberal Hb criterion (Gregersen et al. 2011). Randomization was provided by an allocation concealment process in the web-based clinical trial-support system “TrialPartner” (Public Health and Quality Improvement, Central Denmark Region). This central computer program using permuted block sizes stratified the randomization according to sex and type of residence, and allocated each participant to one of the transfusion strategies. The project manager entered the patient’s civil registration number into the computer program, and passed on the randomization result to the electronic patient record (which was available to the hospital staff in the orthopedic and geriatric wards since they were to administer the transfusions during the intervention period. The participants, their relatives, and the endpoint assessors were blind as to the result of randomization and to information on the patients’ Hb levels.
Procedures
The standard venous Hb analysis was done by cyanmethemoglobin assay (inter-laboratory error: 0.2 g/dL) performed immediately upon admission and postoperatively. Hb was measured daily during the first 3 postoperative days, then at least once during the following 4–6 days, and at least once a week for the following 3 weeks. Blood tests were performed during hospitalization, in nursing homes, and in sheltered housing facilities by a multidisciplinary orthogeriatric team.
Transfusions, as necessary, were performed according to group assignments and no later than 24 h after Hb determination. Only 1 RBC unit was given initially, prior to further Hb measurement. Measurement was repeated after the transfusion until the Hb target was reached, with no more than 2 units per day being administered. In Denmark, 1 unit of RBCs is approximately 300 mL, with an erythrocyte concentration of ≥ 1.65 g/dL per unit and a leukocyte content of < 1,200 × 106. In acute situations, and between transfusions, venous Hb levels were measured with a portable HemoCue photometer (HemoCue, Mission Viejo, CA). All Hb results were evaluated on a daily basis by the project manager. The foregoing procedures continued for 30 days after HF surgery. The standard procedure of our Geriatric Department transferred sheltered housing residents from the orthopedic ward to the geriatric ward on the day after surgery, for approximately 1 week of physical training. Nursing home residents were generally discharged directly from the orthopedic ward to their nursing homes on the day after surgery, since most of them needed familiar surroundings to avoid a state of delirium. As previously described, the standard geriatric treatment program included early mobilization, iron supplementation, osteoporosis therapy, nutritional support, fluid therapy, and evaluation of medication. All such residents were visited by a multidisciplinary team immediately after discharge and within 30 days of surgery.
Measurements
The primary outcome was recovery from physical disabilities, with 3 tools being used to measure physical performance: (1) Modified Barthel index measured the basic self-care activities of daily living (ADL) performance ranging from 0 to 100 points (100 = best), assessing 10 domains—eating, transferring, personal care, toiletry, bathing, walking, managing stairs, dressing, bowel control, and bladder control; (2) New Mobility score ranging from 0 to 9 points (9 = best), assessing both indoor and outdoor walking abilities, and ability to go shopping; and (3) cumulated ambulation score, with a daily score from 0 to 6 points (6 = best), assessing getting in and out of bed, sitting-to-standing-to-sitting, and walking ability with an appropriate aid. Cognitive status was assessed by mini mental state examination (MMSE), ranging from 0 to 30 points (30 = no cognitive impairment).
2 occupational therapists (blinded assessors) assessed each patient’s physical and cognitive abilities (“prefracture”) and through the 90 days after surgery (days 10, 30, and 90). Prefracture assessments were performed retrospectively by asking the patient, care staff, and/or the patient’s relatives about the level of physical performance 14 days before the hip fracture. 1 assessor was appointed for each patient follow-up and visited the patients in their residences.
Secondary outcomes were 30-day and 90-day mortality. Dates of death within 90 days of surgery were obtained from the Danish Civil Registration System. Causes of death based on death certificates were obtained from the Danish Health and Medicine Authority.
After study recruitment was complete, the comprehensive geriatric assessment frailty index was used to determine whether nursing home and sheltered housing residents were equally frail. The frailty index embraced: (1) prefracture ADL dependency (measured by Modified Barthel index < 80); (2) severe comorbidity (measured by Charlson comorbidity index > 2); (3) cognitive dysfunction (measured by MMSE < 20); (4) malnutrition (measured by serum albumin < 34 g/L and body mass index < 18.5); and (5) polypharmacy, i.e. treatment with more than 7 prescribed drugs. Frailty was determined according to one, or more, of the foregoing criteria (Kristjansson et al. 2012).
Statistics
Sample size calculation was based on Geriatric Department data from an observational pilot study of nursing home patients after hip fracture surgery. Those with Hb levels between 9.7 g/dL (6 mmol/L) and 11.3 g/dL (7 mmol/L) during their first 2 postoperative days had shown better physical recovery when given more RBC transfusions. The patients’ Modified Barthel index scores had improved by 23% during 30 days of follow-up compared to a standard treatment applied to an identical population, conducted 1 year earlier. We assumed that the recovery of sheltered housing residents would similarly improve. To obtain 85% statistical power at p ≤ 0.05, we aimed to recruit 284 patients, allowing for a 10% probability of withdrawal.
Patients’ baseline characteristics and clinical outcomes were compared as follows: (1) intention to treat (ITT); (2) randomized study group assignment; and (3) residential group. Continuous variables were compared using Student’s t-test, categorical variables with Pearson’s chi-squared test or Fisher’s exact test, and non-normally distributed variables with Wilcoxon’s rank-sum test. Adjusted analyses were performed according to the slightly imbalanced baseline variable age and randomization stratification factors (sex and residence). These variables were not associated with any of the outcome variables; thus, results are presented with crude estimates.
Measurements of Hb concentration and logarithm-transformed Modified Barthel index summed scores were compared by analysis of variance (with repeated measurement). Likelihood ratio tests were used to test for parallel curves and equal means between the 2 groups. The models were checked with normal probability plots of the standardized residuals and scatter plots of the residuals versus predicted values. Furthermore, all pairwise differences between any 2 time points were checked with normal probability plots and for equal standard deviations and correlations (the compound symmetry model). In non-survivors, the missing physical ability values were set to zero (meaning no ability).
Modified Barthel index and cumulated ambulation score measured on day 10 were categorized and compared using Pearson’s chi-squared test or Fisher’s exact test. The median New Mobility scores were compared by Wilcoxon’s rank-sum test. Results are expressed as percentage or median with interquartile range (IQR).
The risk of death within 2 follow-up periods (30 or 90 days) were analyzed using a Cox proportional hazard regression model. Each patient was followed for the same time without censoring, and only death terminated the follow-up period. Time of death was recorded by date. The assumption of proportional hazards was checked graphically using “log-log” plots of the 2 survival curves. Results are expressed as hazard ratios (HRs) with 95% confidence intervals (CIs). Outcome measures for per-protocol analyses were similarly compared.
Any p-value ≤ 0.05 was considered statistically significant. Statistical analyses were performed with Stata software, version 13.0.
Ethics
At admission or (at the latest) on the day after surgery, the project manager assessed the patients’ cognitive capacities. Cognitive impairment was defined by: (1) a MMSE score of < 20; (2) a confusion assessment method result indicating delirium; or (3) a clinical cognitive evaluation undertaken by 2 independent healthcare professionals. Patients who were not impaired cognitively gave their written informed consent. Consents for impaired patients were given by a next of kin plus the relevant general practitioner. The trial was conducted in accordance with the ethical principles of the Declaration of Helsinki. The study protocol was approved by the Danish Data Protection Agency and the Central Denmark Region Ethical Committee. The trial was evaluated every 6 months by an independent safety-monitoring board. The study is registered at ClinicalTrials.gov, number NCT01102010.
Results
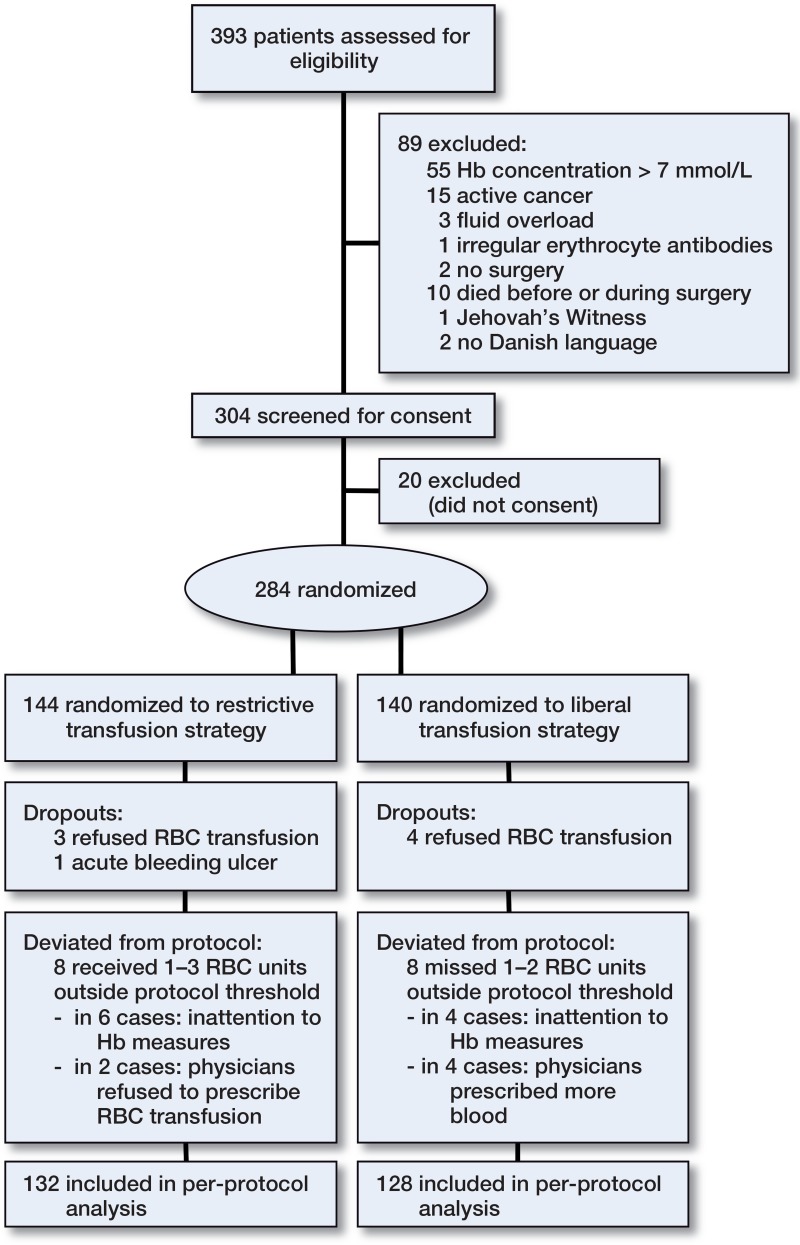
284 patients were enrolled (Figure 1). In terms of baseline characteristics and outcomes, 8 patients who dropped out of the study did not differ significantly from those who completed it, and 260 patients remained for the PP analysis.
Figure 1.
CONSORT flow diagram for enrollment, allocation, follow-up, and analysis
Baseline patient characteristics were well balanced between the transfusion groups, except from mean age (which was slightly lower in the restrictive strategy group), and a somewhat longer surgical waiting time in the liberal strategy group (Table 1). Overall, the data indicated that most of the elderly patients were frail with dependency in ADL, ambulation, and mobility before fracture: 57% had been substantially or completely dependent on personal support, 71% had been unable to walk independently without walking aids, and 12% had needed assistance when transferring from bed to chair. A statistically significantly higher proportion of nursing home patients (96%) were assessed as being frail, when compared to sheltered housing residents (78%) (p < 0.001).
Table 1.
Baseline characteristics of 284 frail elderly hip fracture patients
| Characteristics | Restrictive strategy (n = 144) | Liberal strategy (n = 140) |
|---|---|---|
| Socio-demographics | ||
| Female (%) | 108 (75) | 106 (76) |
| Mean age, years (SD) | 86 (6.8) | 88 (6.9) |
| Residence (%) | ||
| Nursing home | 89 (61) | 90 (64) |
| Sheltered housing | 55 (39) | 50 (36) |
| Physical ability before fracture Activities of daily livinga (%) | ||
| Independent or moderately dependent | 59 (41) | 63 (45) |
| Substantially dependent | 66 (46) | 59 (42) |
| Completely dependent | 19 (13) | 18 (12) |
| Transfer from bed to chair | ||
| Independent | 123 (85) | 127 (91) |
| Dependent | 21 (15) | 13 (9) |
| Walking ability (%) | ||
| Independent | 44 (30) | 39 (28) |
| Walking aids | 88 (61) | 90 (64) |
| Person support | 8 (5) | 7 (5) |
| None | 4 (3) | 4 (3) |
| Comorbid conditions | ||
| Comorbiditya (%) | ||
| Low | 33 (23) | 39 (28) |
| Moderate | 78 (54) | 75 (54) |
| Severe | 33 (23) | 26 (18) |
| Cardiovascular disease (%) | 34 (24) | 25 (18) |
| Dementiaa (%) | 46 (32) | 56 (40) |
| Underweighta (%) | 22 (15) | 23 (16) |
| Anemiab (%) | 70 (49) | 68 (49) |
| Prescribed medicine a (IQR) | 6 (4–9) | 6 (4–9) |
| Previous hip fracture (%) | 24 (17) | 33 (24) |
| Surgical treatment (%) | ||
| Internal fixation | 109 (76) | 112 (80) |
| Arthroplasty | 31 (21) | 26 (18) |
| Other | 4 (3) | 2 (2) |
| Waiting time for surgery, h (IQR) | 16 (10–24) | 19 (12–25) |
Variable used in the “comprehensive geriatric assessment frailty index”.
Anemia defined by World Health Organization as hemoglobin
< 12 g/dL in women and < 13 g/dL in men.
Physical ability
Patients’ physical abilities in both transfusion groups were impaired 10 days after hip fracture surgery, relative to prefracture levels (p < 0.001). Similar recovery 10 days after intervention was found in the 2 groups, according to Modified Barthel index, New Mobility score, cumulated ambulation score, transfer from bed to chair, or walking ability (Table 2).
Table 2.
Intention to treat: physical ability scores 10 days after hip fracture surgery compared in a restrictive transfusion group with a liberal group stratified in residents from nursing homes and sheltered housing and analyzed with Wilcoxon rank-sum test
| All residents (n = 284) |
Nursing homes (n = 179) |
Sheltered housing (n = 105) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Physical ability 10 days after surgery | Restrictive strategy (n = 144) | Liberal strategy (n = 140) | p-value | Restrictive strategy (n = 89) | Liberal strategy (n = 90) | p-value | Restrictive strategy (n = 55) | Liberal strategy (n = 50) | p-value |
| Modified Barthel indexa (%) | 0.6 | 0.4 | 1.0 | ||||||
| Independent or moderately dependent | 38 (26) | 32 (23) | 18 (20) | 15 (17) | 20 (36) | 17 (34) | |||
| Substantially dependent | 51 (35) | 58 (41) | 24 (27) | 33 (37) | 27 (49) | 25 (50) | |||
| Completely dependent | 55 (38) | 50 (36) | 47 (53) | 42 (46) | 8 (15) | 8 (16) | |||
| New Mobility scoreb median (IQR) | 1 (0–1) | 1 (0–1) | 0.5 | 1 (0–1) | 1 (0–1) | 0.8 | 1 (1–2) | 1 (1–2) | 0.5 |
| Cumulated ambulation scorec (%) | 0.5 | 0.2 | 0.2 | ||||||
| Walking ability | 19 (13) | 16 (11) | 4 (4) | 8 (9) | 16 (29) | 7 (14) | |||
| Sit-to-stand-to-sit | 65 (45) | 74 (53) | 37 (42) | 40 (44) | 30 (55) | 34 (68) | |||
| Bedridden | 56 (39) | 50 (36) | 48 (54) | 42 (47) | 9 (16) | 9 (18) | |||
| Transfer from bed to chair (%) | 0.3 | 1.0 | 0.2 | ||||||
| Independent | 25 (17) | 19 (14) | 10 (11) | 11 (12) | 15 (27) | 8 (16) | |||
| Dependent | 119 (83) | 121 (86) | 79 (89) | 79 (88) | 40 (73) | 42 (84) | |||
| Walking ability (%) | 0.9 | 0.7 | 0.7 | ||||||
| Independent | 1 (1) | 1 (1) | 1 (1) | 1 (1) | 0 (0) | 0 (0) | |||
| Walking aids | 25 (17) | 25 (18) | 7 (8) | 12 (13) | 18 (33) | 13 (26) | |||
| Person support | 59 (41) | 66 (47) | 33 (37) | 38 (42) | 26 (47) | 28 (56) | |||
| None | 59 (41) | 48 (34) | 48 (54) | 39 (43) | 11 (20) | 9 (18) | |||
Modified Barthel index score categories: “Independent/moderately dependent” in activities of daily living (ADL) (summed score: 100–50);
“Substantially dependent” in ADL (summed score: 49–25); and “Completely dependent” in ADL (summed score: 24–0).
New Mobility score categories (9 = best, 0 = worst): “High level” (summed score 9–6); “Low level” (summed score 5–0).
Cumulated ambulation score categories (6 = best, 0 = worst): “Independence” (summed score: 6); “Dependency” (summed score: 5–0).
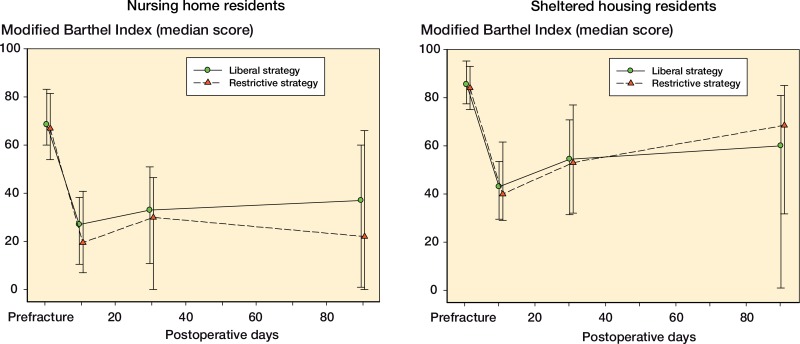
Overall, the repeated measurements of Modified Barthel index score, compared to prefracture levels, on days 10, 30, and 90 after surgery, were similar within transfusion groups, i.e. parallel curves (p = 0.2) and equal means (p = 0.3). For nursing home residents, the curves were parallel (p = 0.4) and the means were equal (p = 0.3) between transfusion groups. Likewise, for sheltered housing residents, the curves were parallel (p = 0.6) and the means were equal (p = 0.9) between transfusion groups (Figure 2). Similar results were found with per-protocol analyses.
Figure 2.
Intention to treat: repeated measurements on recovery from physical disabilities before fracture until postoperative days 10, 30 and 90, presented as median score with interquartile range, in residents from nursing homes and sheltered housing facilities.
Mortality
No statistically significant difference in 90-day mortality was found between the restrictive transfusion group (27%) and the liberal (21%) transfusion group when analyzed by intention to treat (Table 3). However, the per-protocol 30-day mortality rate was higher after restrictive transfusion. Frailty was associated with 90-day mortality (HR = 4.5, 95% CI: 1.1–19; p = 0.03), as was cardiovascular disease (HR = 0.5, 95% CI: 0.3–0.9; p = 0.01).
Table 3.
Hazards ratio of time to death within 30 and 90 days by intention-to-treat analysis and per-protocol analysis
| 30-day mortality |
90-day mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Restrictive strategy | Liberal strategy | Hazard ratio (95% CI) | p-value | Restrictive strategy | Liberal strategy | Hazard ratio (95% CI) | p-value | |
| Intention to treat, n | 144 | 140 | 144 | 140 | ||||
| All residents (%) | 21 (14) | 12 (8) | 1.8 (0.7–3.6) | 0.1 | 40 (27) | 30 (21) | 1.4 (0.9–2.2) | 0.2 |
| Nursing homes (%) | 16 (18) | 9 (10) | 1.9 (0.8–4.3) | 0.1 | 32 (36) | 18 (20) | 2.0 (1.1–3.6) | 0.01 |
| Sheltered housing (%) | 5 (9) | 3 (6) | 1.5 (0.4–6.4) | 0.6 | 8 (15) | 12 (24) | 0.6 (0.2–1.5) | 0.3 |
| Per-protocol, n | 132 | 128 | 132 | 128 | ||||
| All residents (%) | 21 (16) | 9 (7) | 2.4 (1.1–5.2) | 0.03 | 35 (27) | 26 (20) | 1.4 (0.8–2.3) | 0.2 |
| Nursing homes (%) | 16 (20) | 8 (10) | 2.2 (0.9–5.0) | 0.07 | 28 (35) | 17 (20) | 1.9 (1.0–3.4) | 0.04 |
| Sheltered housing (%) | 5 (10) | 1 (2) | 4.6 (0.5–39) | 0.2 | 7 (13) | 9 (19) | 0.7 (0.3–2.0) | 0.5 |
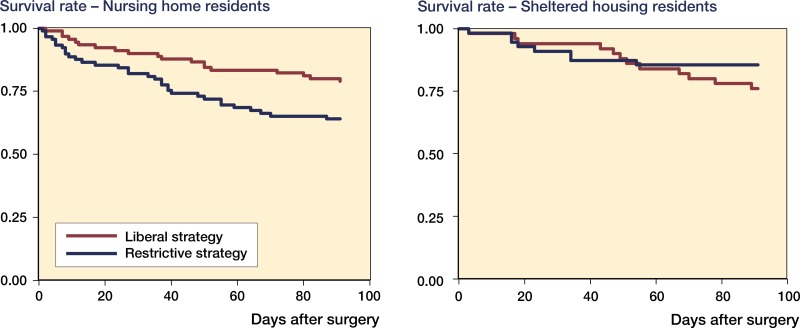
In a subgroup analysis, the 90-day mortality rate of nursing home residents was statistically significantly higher after restrictive transfusions than after liberal transfusions. Similar results were obtained with the per-protocol analyses. However, for sheltered housing residents 90-day mortality rates showed no statistically significant differences between transfusion groups (Figure 3).
Figure 3.
Kaplan-Meier plots of 90-day survival rates after hip fracture in residents from nursing homes and sheltered housing facilities, by intention-to-treat analysis.
The main cause of death for both transfusion groups was pneumonia (p = 0.11) (Table 4). Durations of hospital stay were equal within transfusion groups, i.e. a median of 2 days for both groups of nursing home residents, and medians of 11 days and 10 days for sheltered housing residents (p = 0.35).
Table 4.
Causes of death over 90 postoperative days in frail, elderly hip fracture patients
| Cause of deaths | Restrictive strategy (n = 40) | Liberal strategy (n = 30) | p-value |
|---|---|---|---|
| Pneumonia (%) | 18 (44) | 8 (27) | 0.1 |
| Stroke (%) | 2 (7) | 8 (27) | 0.02 |
| Heart failure (%) | 11 (28) | 3 (9) | 0.07 |
| Sepsis (%) | 5 (11) | 3 (9) | 0.7 |
| Dementia (%) | 4 (10) | 3 (9) | 1.0 |
| Liver failure (%) | 0 (0) | 5 (19) | - |
Red blood cell transfusions
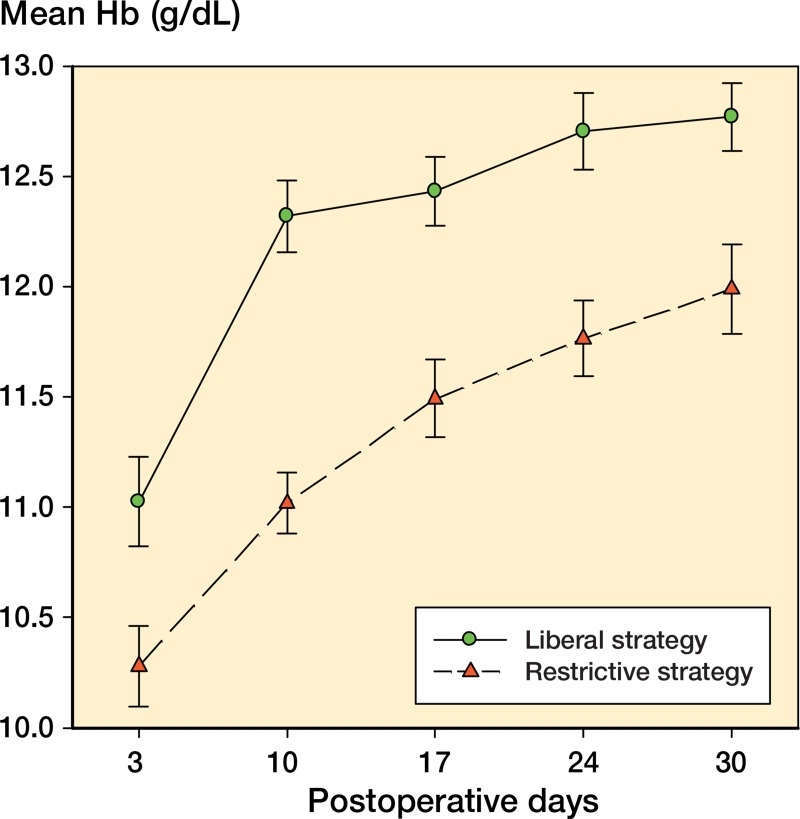
712 RBC transfusions were administered during the study, with 73% during the first postoperative week. The median number of RBC units per patient in the restrictive transfusion group was 1.0 (IQR 1–2) as opposed to 3.0 (IQR 2–5) in the liberal group. Repeated measurements showed maintained mean Hb levels of 11.3 g/dL (95% CI: 11.3–11.4) for the restrictive transfusion group and 12.2 g/dL (95% CI: 12.2–12.3) for the liberal group. Also, the Hb measurements of both transfusion groups showed parallel curves (p = 0.8) but unequal means (p < 0.001) (Figure 4). No complications were observed during, or after, RBC transfusions. No difference was found in iron supplementation (88% in the restrictive group and 87% in the liberal group).
Figure 4.
Mean hemoglobin concentrations (in g/dL) measured on days 3, 10, 17, 24, and 30 after hip fracture surgery (with 95% confidence intervals) according to blood transfusion strategy (liberal or restrictive).
Discussion
Our RCT data show that a liberal RBC transfusion strategy (Hb target < 11.3 g/dL; 7 mmol/L) pursued for 30 days after intervention was more beneficial than a restrictive strategy with a lower target (Hb < 9.7 g/dL; 6 mmol/L) for elderly hip-fractured patients admitted from nursing homes.
Physical ability
Physical abilities after surgery were not associated with RBC transfusion strategies during the first 10 days, when the majority of transfusions were completed. Half of all patients in each transfusion group were anemic before fracture surgery. It remains uncertain, however, whether the anemia was chronic or was caused by the fracture. Several studies have found an association in elderly subjects between reduced physical ability due to reduced muscle strength and chronic anemia (Penninx et al. 2004). Poor physical ability before fracture and (chronic) anemia are 2 of many factors that affect functional prognosis in nursing home residents (Onem et al. 2010). Furthermore, physical functional outcome in hip fracture patients appeared to be negatively influenced by cognitive impairment, comorbidity, and very old age.
Our results did not directly reproduce the findings that higher Hb levels are associated with better early functional recovery after hip fracture surgery. Also, very few of our patients regained their prefracture physical abilities during 3 months of follow-up. To expand our follow-up period to 1 year, when recovery would be expected to peak (Ortiz-Alonso et al. 2012), would probably have been of minor interest given a 1-year expected mortality rate of approximately 45% for nursing home residents (Beaupre et al. 2012).
The meta-analysis of Carson el al. (2012), which included several RCTs in various patient populations, concluded that RBC stocks can be saved without reducing functional recovery or increasing short-term mortality. The high-risk hip fracture patients who had been walking without human assistance before the trauma showed no differences in walking ability or short-term mortality in relation to liberal or restrictive RBC transfusion strategies post-surgery. Unfortunately, the researchers did not perform a subgroup analysis on the data from nursing home residents (Carson et al. 2011). Similarly, physical rehabilitation of Danish hip fracture patients who had lived in the community and walked independently before surgery was found to be unrelated to higher Hb levels (Foss et al. 2009).
Mortality
In our analyses, which took pre-surgical residential care needs into account, 30-day mortality but not 90-day mortality after hip fracture surgery was reduced by the liberal RBC transfusion strategy relative to the restrictive strategy. Foss et al. (2009) found that in elderly community-dwelling patients with independent walking function and intact cognitive status prior to hip fracture, a liberal transfusion strategy appeared to reduce cardiovascular events/deaths. In contrast, for patients in intensive care, Hébert et al. (1999) found that a restrictive transfusion strategy was at least as effective as a liberal strategy—except possibly for those with acute myocardial infarction and unstable angina. However, a recent pilot study of patients with acute coronary syndrome or unstable angina who were undergoing cardiac catheterization found that those treated with a restrictive strategy (Hb target 8 g/dL; 5 mmol/L) had more than twice the rate of major cardiac events and deaths compared to those treated with a liberal strategy (Hb target 10 g/dL; 6.2 mmol/L) (Carson et al. 2013).
In the present study, cardiovascular diseases were associated with 90-day mortality rates. In the foregoing studies, liberal RBC transfusion thresholds were similar to our restrictive threshold. Patient frailty was not the issue for RCTs with the previous transfusion strategies, despite the well-known fact that in nursing home residents, anemia is related to 90-day mortality (Berry et al. 2009). Nevertheless, in the future we need to look more deeply into the question of beneficial transfusion thresholds to determine whether the target groups consist of patients with cardiovascular diseases and hip fracture patients from nursing homes.
Postoperative anemia in surgical hip fracture patients is associated with delirium and nosocomial infections (Marcantonio et al. 1998, Izuel et al. 2008). In our study, we found no difference in the number of infections during the intervention period (unpublished data). Prolonged delirium and pneumonia are both associated with death (Holvik et al. 2010, Lee et al. 2011), and cognitive impairment and/or age ≥ 85 years are associated with higher incidences of delirium and mortality (Petersen et al. 2006, Bjorkelund et al. 2009). We found that stroke was a more frequent cause of death in the liberal transfusion group, whereas heart failure was more frequent (with borderline significance) in the restrictive transfusion group. However, if the 2 diagnostic categories were pooled together as cardiovascular diseases, no significant difference was found between the groups. This consideration should be investigated further, because information was obtained from death certificates only, and the use of death certificates based on the Danish Death Registry requires caution when interpreting the results. In Denmark, the autopsy rate is less than 10% of all deaths, and the quality of data on causes of death relies mainly upon the correctness of the physician’s notification (Helweg-Larsen 2011).
Nursing home residents
In a subgroup analyses, we looked specifically at the most frail patients, defined as those living in nursing homes. In contrast to previous studies, this included patients who were unable to walk independently, and we found that higher Hb levels reduced 90-day mortality.
The 90-day mortality rate in our nursing home residents who were given restrictive transfusions was rather high (36%), and higher than the 27% we had previously observed. Berry et al. (2009) found that the overall 90-day mortality rate in nursing home residents admitted to long-term care, in a rehabilitation center with geriatric specialists (Boston, USA), was 21% after hip fracture surgery—rather like the 20% in our liberal strategy group. However, we are unable to make further comparisons, since no data are available on the transfusion strategy for this group of nursing home residents.
The subgroup analyses were conducted according to type of residence, to avoid the possibility that potentially different levels of frailty would confuse our results. Assessment with the comprehensive geriatric assessment frailty index (which was developed for surgical cancer patients) showed that a large proportion of sheltered housing residents were not frail. There are nursing homes throughout the world, but the residents are probably not directly comparable in different countries. However, they generally require continual care and have other significant deficiencies, e.g. in activities of daily living and cognition (Tolson et al. 2013).
In Denmark, nursing home residents are easy to identify from their home addresses. We have previously reported that one-fifth of our hospital hip fracture patients, aged ≥ 65 years, normally reside in nursing homes (Gregersen et al. 2012). The prevalence of these patients in the orthopedic ward is relatively high, and they require evidence-based expertise.
We cannot exclude the fact that some patients living in their own homes are as frail as those in nursing homes, and there may be different criteria between countries for transferring patients to nursing homes. Thus, future studies should focus on patients’ degree of frailty as a selection criterion for RBC transfusions, instead of their home addresses, but for that purpose we would need a frailty index especially developed for elderly hip fracture patients.
RBC transfusion targets
Previous randomized controlled trials have set Hb targets in the 7- to 9-g/dL range for restrictive transfusion strategies, and in the 9- to 10-g/dL range for liberal transfusion strategies (Carson et al. 2012). The difference between the Hb targets of RBC transfusion strategies may not have been sufficient to yield more significant results. Instead, our restrictive strategy might have followed the restrictive threshold from the previous RCTs to make comparison between studies easier. However, this would have been unethical since we had already shown—in our previous observational study—a reduction in mortality with a liberal transfusion strategy as low as Hb 11.3 g/dL. Furthermore, our national guidelines recommend a Hb target as low as 9.7 g/dL in elderly hip fracture patients.
Strengths and limitations
Our power calculation was based on nursing home residents only. The large proportion of non-frail elderly patients admitted from sheltered housing facilities may have diluted our intervention effects. From the very beginning, our aim was to examine the effect of a more liberal blood transfusion strategy for the nursing home residents, since high mortality after hip fracture was almost exclusively determined by the higher death rate in these patients, but the ethical committee required us to include sheltered housing residents also. To compensate for a possible difference in the degree of frailty in these 2 residential groups, we stratified them in the randomization process. Nonetheless, our results show that the difference between them was greater than expected. Thus, we needed more patients than previously calculated in order to show a distinct difference between the transfusion groups.
No frail elderly patients with Hb levels below 9.7 g/dL were excluded during the first 6 days of recruitment, since transfusions made it possible for them to participate. However, 10 patients died intraoperatively and the Hb values of these patients were unknown. Furthermore, the blood test results were followed closely during the intervention period and RBC transfusions were accomplished within 24 hours (except for dying patients, for whom transfusions were considered unethical). No selection bias intruded, since during the entire study period daily assessments in the orthopedic ward continued for every hip fracture patient admitted from nursing homes or sheltered housing.
The Modified Barthel index was a sensitive physical assessment tool to measure changes in ADL over time, although the items eating, bowel control, and bladder control were less relevant to recovery. Our sample size calculation was based on the summed scores of the Modified Barthel index, and this was therefore our first choice of tool. Measurements from New Mobility score and cumulated ambulation score are presented in order to make our results comparable to studies using similar tools. The New Mobility score was not very useful, e.g. “ability to go shopping” is rarely an option for frail elderly people. Information on transfer and walking ability were more relevant to this population, but no significant differences were found. The protocol stated that a specific assessor would test a given patient throughout the 90 days of follow-up, but in some cases assessors were replaced due to vacations or illness. This could have distorted the results, although the RCT design would have distributed such confounding equally across both transfusion groups.
Conclusion
In frail elderly hip fracture patients, recovery was similar with a restrictive or a liberal RBC transfusion strategy according to our Hb tresholds. It should be determined whether a larger difference between the Hb thresholds of RBC transfusion strategies (a lower restrictive Hb threshold) may be associated with physical recovery. Implemention of a liberal RBC transfusion strategy in nursing home residents has the potential to increase survival. We therefore suggest that liberal RBC strategies should be investigated further in nursing home residents with hip fracture, for whom it may be life-saving. Also, we need to develop some means of identifying patients who would benefit from more liberal RBC transfusion strategies, and to specify optimal Hb targets for the transfusions required by frail elderly hip fracture patients. In general, the use of RBC transfusions should be restricted. However, we must accept that some hip fracture patients require more blood than specified by the recommendations.
Acknowledgments
MG (project manager) and EMD recruited the study participants. LCB ensured protocol compliance in the orthopedic ward, with MG and EMD doing likewise in the geriatric ward. MG registered data collected from the assessors, performed the statistical analyses, and prepared the manuscript. All the authors took part in structuring and writing of the manuscript.
We gratefully acknowledge the kind participation of patients, their relatives, and general practitioners. We also thank the staff of the orthopedic and geriatric wards. The Helga and Peter Korning Foundation provided a grant for medical equipment (HemoCue portable photometer). The costs of data collection, analysis, and preparation of the manuscript were borne by the Department of Geriatrics, Aarhus University Hospital.
No competing interests declared.
References
- Bailey RA, Reardon G, Wasserman MR, McKenzie RS, Hord RS. Association of anemia with worsened activities of daily living and health-related quality of life scores derived from the minimum data set in long-term care residents . Health and Qual Life Outcomes. 2012;10:129. doi: 10.1186/1477-7525-10-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker NL, Cook MN, Arrighi HM, Bullock R. Hip fracture risk and subsequent mortality among alzheimer’s disease patients in the United Kingdom. 1988–2007 . Age Ageing. 2011;40(1):49–54. doi: 10.1093/ageing/afq146. [DOI] [PubMed] [Google Scholar]
- Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR. Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: Prospective cohort study . J Am Geriatr Soc. 2012;60(7):1268–73. doi: 10.1111/j.1532-5415.2012.04033.x. [DOI] [PubMed] [Google Scholar]
- Berry SD, Samelson EJ, Bordes M, Broe K, Kiel DP. Survival of aged nursing home residents with hip fracture . J Gerontol A Biol Sci Med Sci. 2009;64(7):771–77. doi: 10.1093/gerona/glp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorkelund KB, Hommel A, Thorngren KG, Lundberg D, Larsson S. Factors at admission associated with 4 months outcome in elderly patients with hip fracture . AANA J. 2009;77(1):49–58. [PubMed] [Google Scholar]
- Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery . NEJM. 2011;365(26):2453–62. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson JL, Carless PA, Hebert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. The Cochrane Database of Systematic Reviews. 2012. 4, CD002042. [DOI] [PMC free article] [PubMed]
- Carson JL, Brooks MM, Abbott JD, Chaitman B, Kelsey SF, Triulzi DJ, et al. Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease . Am Heart J. 2013;165(6):964–71. doi: 10.1016/j.ahj.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danish Health and Medicine Authority Guidelines no. 10333 Blood transfusion 2008. Retrieved december/20, 2007. Available from http://www.sst.dk/Tilsyn/Transfusionsmedicin .
- Foss NB, Kehlet H. Mortality analysis in hip fracture patients: Implications for design of future outcome trials . Br J Anaesth. 2005;94(1):24–29. doi: 10.1093/bja/aei010. [DOI] [PubMed] [Google Scholar]
- Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture . J Bone Joint Surg Br. 2006;88(8):1053–59. doi: 10.1302/0301-620X.88B8.17534. [DOI] [PubMed] [Google Scholar]
- Foss NB, Kristensen MT, Jensen PS, Palm H, Krasheninnikoff M, Kehlet H. The effect of liberal versus restrictive transfusion tresholds on ambulation after hip fracture surgery . Transfusion. 2009;49:227–34. doi: 10.1111/j.1537-2995.2008.01967.x. [DOI] [PubMed] [Google Scholar]
- Gregersen M, Zintchouk D, Borris LC, Damsgaard EM. A geriatric multidisciplinary and tailor-made hospital-at-home method in nursing home residents with hip fracture . Geriatr Orthop Surg Rehabil. 2011;2(4):148–54. doi: 10.1177/2151458511421908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregersen M, Morch MM, Hougaard K, Damsgaard EM. Geriatric intervention in elderly patients with hip fracture in an orthopedic ward . J Inj Violence Res. 2012;4(2):45–51. doi: 10.5249/jivr.v4i2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: Excess mortality after hip fracture among older women and men . Ann Intern Med. 2010;152(6):380–90. doi: 10.1059/0003-4819-152-6-201003160-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, et al. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture . J Orthop Trauma. 2004;18(6):369–74. doi: 10.1097/00005131-200407000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebért PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care . NEJM. 1999;340(6):409–17. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- Helweg-Larsen K. The Danish Register of Causes of Death . Scand J Public Health. 2011;39(Suppl 7):26–29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- Holvik K, Ranhoff AH, Martinsen MI, Solheim LF. Predictors of mortality in older hip fracture inpatients admitted to an orthogeriatric unit in Oslo . Norway. J Aging Health. 2010;22(8):1114–31. doi: 10.1177/0898264310378040. [DOI] [PubMed] [Google Scholar]
- Izuel RM, Garcia Erce JA, Gomez-Barrera M, Cuenca Espierrez J, Abad Sazatornil R, Rabanaque Hernandez MJ. Relationship between allogeneic blood transfusion, iron deficiency and nosocomial infection in patients with hip fracture . 2008;131(17):647–52. doi: 10.1157/13128722. [Relacion de la transfusion y la ferropenia con la infeccion nosocomial en pacientes con fractura de cadera] Med Clin (Barc) [DOI] [PubMed] [Google Scholar]
- Juliebo V, Krogseth M, Skovlund E, Engedal K, Wyller TB. Medical treatment predicts mortality after hip fracture . J Gerontol A Biol Sci Med Sci. 2010;65(4):442–49. doi: 10.1093/gerona/glp199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B. Excess mortality in men compared with women following a hip fracture. national analysis of comedications, comorbidity and survival . Age Ageing. 2010;39(2):203–09. doi: 10.1093/ageing/afp221. [DOI] [PubMed] [Google Scholar]
- Kirkland LL, Kashiwagi DT, Burton MC, Cha S, Varkey P. The Charlson comorbidity index score as a predictor of 30-day mortality after hip fracture surgery . Am J Med Qual. 2011;26(6):461–67. doi: 10.1177/1062860611402188. [DOI] [PubMed] [Google Scholar]
- Kristjansson SR, Ronning B, Hurria A, Skovlund E, Jordhoy MS, Nesbakken A, et al. A comparison of two pre-operative frailty measures in older surgical cancer patients. J Geriatric Oncology. 2012;3(1):1–7. [Google Scholar]
- Kumar D, Mbako AN, Riddick A, Patil S, Williams P. On admission haemoglobin in patients with hip fracture . Injury. 2011;42(2):167–70. doi: 10.1016/j.injury.2010.07.239. [DOI] [PubMed] [Google Scholar]
- Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher hb level is associated with better early functional recovery after hip fracture repair . Transfusion. 2003;43(12):1717–22. doi: 10.1046/j.0041-1132.2003.00581.x. [DOI] [PubMed] [Google Scholar]
- Lee KH, Ha YC, Lee YK, Kang H, Koo KH. Frequency, risk factors, and prognosis of prolonged delirium in elderly patients after hip fracture surgery . Clin Orthop Relat Res. 2011;469(9):2612–20. doi: 10.1007/s11999-011-1806-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maraldi C, Volpato S, Cesari M, Cavalieri M, Onder G, Mangani I, et al. Anemia and recovery from disability in activities of daily living in hospitalized older persons . J Am Geriatr Soc. 2006;54(4):632–36. doi: 10.1111/j.1532-5415.2006.00664.x. [DOI] [PubMed] [Google Scholar]
- Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH. The association of intraoperative factors with the development of postoperative delirium . Am J Med. 1998;105(5):380–84. doi: 10.1016/s0002-9343(98)00292-7. [DOI] [PubMed] [Google Scholar]
- Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G, et al. Timing matters in hip fracture surgery: Patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients . PloS One. 2012;7(10) doi: 10.1371/journal.pone.0046175. e46175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onem Y, Terekeci H, Kucukardali Y, Sahan B, Solmazgul E, Senol MG, et al. Albumin, hemoglobin, body mass index, cognitive and functional performance in elderly persons living in nursing homes . Arch Gerontol Geriatr. 2010;50:1, 56–59. doi: 10.1016/j.archger.2009.01.010. [DOI] [PubMed] [Google Scholar]
- Ortiz-Alonso FJ, Vidan-Astiz M, Alonso-Armesto M, Toledano-Iglesias M, Alvarez-Nebreda L, Branas-Baztan F, et al. The pattern of recovery of ambulation after hip fracture differs with age in elderly patients . J Gerontol A Biol Sci Med Sci. 2012;67(6):690–97. doi: 10.1093/gerona/glr231. [DOI] [PubMed] [Google Scholar]
- Parker M. Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery . Injury. 2013;44(12):1916–18. doi: 10.1016/j.injury.2013.04.033. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Pahor M, Cesari M, Corsi AM, Woodman RC, Bandinelli S, et al. Anemia is associated with disability and decreased physical performance and muscle strength in the elderly . J Am Geriatr Soc. 2004;52(5):719–24. doi: 10.1111/j.1532-5415.2004.52208.x. [DOI] [PubMed] [Google Scholar]
- Petersen MB, Jorgensen HL, Hansen K, Duus BR. Factors affecting postoperative mortality of patients with displaced femoral neck fracture . Injury. 2006;37(8):705–11. doi: 10.1016/j.injury.2006.02.046. [DOI] [PubMed] [Google Scholar]
- Public Health and Quality Improvement, Central Denmark Region. TrialPartner. Retrieved Nov/24, 2014 Available from www.cfk.rm.dk/om+os/forskning+og+kvalitetsudvikling/datamanagement/trialpartner .
- Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P. Hip fracture patients at risk of second hip fracture: A nationwide population-based cohort study of 169,145 cases during 1977–2001 . J Bone Miner Res. 2009;24(7):1299–1307. doi: 10.1359/jbmr.090207. [DOI] [PubMed] [Google Scholar]
- Salpeter SR, Buckley JS, Chatterjee S. Impact of more restrictive blood transfusion strategies on clinical outcomes: A meta-analysis and systematic review . Am J Med. 2014;127(2):124. doi: 10.1016/j.amjmed.2013.09.017. 131.e3. [DOI] [PubMed] [Google Scholar]
- Schaller F, Sidelnikov E, Theiler R, Egli A, Staehelin HB, Dick W, et al. Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after hip fracture . Bone. 2012;51(3):347–52. doi: 10.1016/j.bone.2012.06.004. [DOI] [PubMed] [Google Scholar]
- Tolson D, Rolland Y, Katz PR, Woo J, Morley JE, Vellas B. An international survey of nursing homes. JAMDA. 2013;14(7):459–62. doi: 10.1016/j.jamda.2013.04.005. [DOI] [PubMed] [Google Scholar]
- van Dijk PT, Mehr DR, Ooms ME, Madsen R, Petroski G, Frijters DH, et al. Comorbidity and 1-year mortality risks in nursing home residents . J Am Geriatr Soc. 2005;53(4):660–65. doi: 10.1111/j.1532-5415.2005.53216.x. [DOI] [PubMed] [Google Scholar]
- WHO Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity 2011. Retrieved Apr/2, 2014. Available from www.who.int/vmnis/indicators/haemoglobin .