Abstract
Background and purpose
Open-wedge osteotomies of the distal radius create a void that is usually filled with either iliac crest bone graft or bone substitute. Previous studies have suggested that this is unnecessary. We investigated the safety of omitting the filling procedure.
Patients and methods
We included 15 patients with a dorsal malunion of a distal radius fracture. A palmar approach and angle-stable plates were used. The patients were followed until there was radiographic and clinical healing.
Results
Non-union occurred in 3 of the 15 patients. The study, which had been planned to include 25 patients, was then discontinued. 6 osteotomies created a trapezoid void (no cortical contact); 3 of these did not unite after the index procedure (p = 0.04), but did subsequently, after autogenous bone grafting. A trapezoid void was significantly associated with non-union (p = 0.04).
Interpretation
When a trapezoid defect is created, one should consider bone substitute or autogenous bone graft. This has been shown to be safe in other studies.
In some individuals, union of a distal radius fracture in a displaced position may cause pain and dysfunction in the affected wrist, which may be reduced by a corrective osteotomy. An open-wedge osteotomy creates a defect, and it is common practice to fill the void with an iliac crest bone graft (Prommersberger et al. 2002b, Ring et al. 2002, Krukhaug and Hove 2007). With modern osteosynthesis, the mechanical support of a cortical graft appears unnecessary and both structural and cancellous grafts have been shown to be sufficient (Ring et al. 2002). Harvesting of the graft can, however, cause persistent donor site morbidity (Silber et al. 2003, Sasso et al. 2005) and it prolongs the procedure. An alternative is to fill the void that has been created with bone substitute (Luchetti 2004, Abramo et al. 2008, Scheer and Adolfsson 2009, Abramo et al. 2010).
The excellent healing potential of the metaphyseal region of the distal radius (Prommersberger et al. 2002a) has made the need for a bone graft questionable, and in a series of 35 cases (Wieland et al. 2005) and more recently in a series of 22 cases (Mahmoud et al. 2012), no non-unions were reported, despite the fact that no bone graft was used.
The aim of this study was to conduct a consecutive series of osteotomies without using any void filler, and to compare the results with those from a previous cohort using tricalcium phosphate (TCP) as bone substitute (Scheer and Adolfsson 2009).
Patients and methods
Study population
Based on a previous study using bone substitute (Scheer and Adolfsson 2009) in which we observed some subsidence of the osteotomy (probably due to an inflammatory reaction around the TCP graft), we performed a sample size calculation based on the hypothesis that there would be no subsidence using no void filler. Based on this calculation, we aimed for enrollment of 25 patients.
16 consecutive patients with symptomatic malunited distal radius fractures were eligible for inclusion between June 2008 and November 2011. 1 patient declined participation and 15 were enrolled in the study. The inclusion criterion was a malunion of a nonoperatively treated dorsally displaced fracture involving the distal radius metaphysis with significant residual symptoms of pain and/or loss of forearm rotation in patients over the age of 18. Exclusion criteria were intraarticular malunions, concomitant carpal ligament lesions, chronic inflammatory disease, use of immune suppressants or warfarin, and inability to understand the information given. The study was discontinued after 3 non-unions. Median age of the patients was 56 (21–62) years, and 14 were women. Surgery was undertaken at median of 12 (4–48) months after the fracture. Preoperative measurements showed a median dorsal angulation (with the shaft of the radius as a reference) of 17° (0–32), positive ulnar variance of 2 (−2 to 6) mm, and a radial height of 8 (−1 to 14) mm.
Surgical procedure
2 experienced wrist surgeons performed all the procedures. The osteotomies were planned with the aid of radiographs of the uninjured side, aiming to restore the congruence of the distal radioulnar (DRU) joint. A palmar approach through the tendon sheath of the flexor carpi radialis (FCR) tendons was used. The superficial head of the pronator quadratus (PQ) was released in an L-shaped fashion. An angle-stable osteotomy plate (3.5 mm; Königsee, Aschau, Germany) was positioned, allowing the distal screws to be inserted parallel to the joint surface. The plate and screws were then temporarily removed. The osteotomy was created using an oscillating saw—with irrigation—along the path of the previous fracture. The dorsal periosteum was then released with an elevator. A further aim was to recreate the “gothic arc shape” of the distal radioulnar interosseous space as seen on the PA view, in order to optimize DRU joint congruence. The plate and distal screws were re-applied and the distal fragment was positioned using images of the contralateral wrist as a template, addressing shortening and malangulation.
Postoperatively, a dorsal wrist splint was kept on for 2 weeks. Immediate unloaded hand therapy was started. Manual labor and activities against resistance were not permitted for 8 weeks. The use of NSAIDs (Kurmis et al. 2012) within the first 4 weeks after surgery was not allowed.
Radiographic measurements
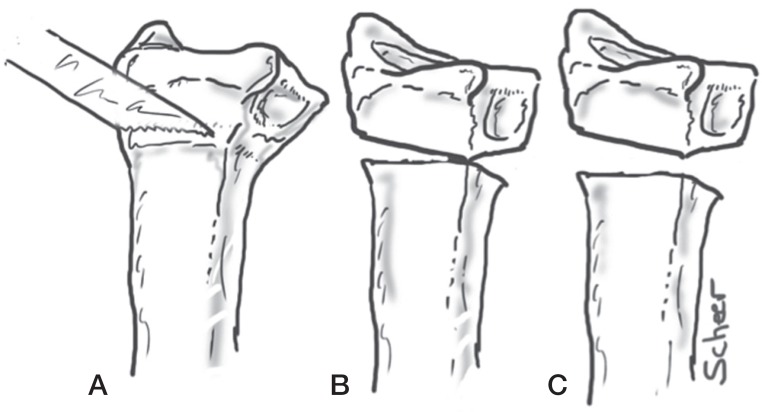
Standard posteroanterior (PA) and lateral radiographs were obtained preoperatively, immediately postoperatively, after 3 months, and then every 6–8 weeks until the osteotomy was judged to be healed (see below). Dorsal angulation was measured on lateral views using the long axis of the radius as a reference, and connecting the palmar and dorsal lips (Goldfarb et al. 2001). Ulnar variance was measured on the PA view using the method of perpendiculars (Steyers and Blair 1989). Radial height was measured on the PA view as the distance between 2 lines perpendicular to the long axis of the radius, one passing through the most distal ulnar head surface and the other at the tip of the radial styloid (Kreder et al. 1996). It was impossible to reliably assess the width of the osteotomy gap on plain radiographs, due to slight variations in rotation. A dichotomized variable was therefore chosen (presence of a trapezoid void or not), as proposed by Mahmoud et al 2012. The osteotomy void was classified as trapezoid if there was a cortical gap of at least 1 mm in the palmar cortex in the lateral view and in the ulnar and radial cortices in the PA view (Figure 1). The position of the osteotomy (distal–proximal) was measured on the lateral view, and expressed as the perpendicular distance from the cut surface of the palmar cortex to the center of the 2 most ulnar distal screws.
Figure 1.
Left radius, ulnopalmar view. The osteotomy will commonly pivot around the ulnopalmar corner to correct dorsal and radial malangulation as well as malrotation. A. Osteotomy done in line with the previous fracture. B. Triangular defect in 2 planes. C. Trapezoid defect in 2 planes.
Assessment of healing
The osteotomy was considered to be healed when there was no palpable tenderness over the osteotomy site and bridging callus with cortex formation was present in at least 3 of 4 cortices in the PA and lateral view (Dijkman et al. 2010).
Statistics
The Mann-Whitney U-test was used for group comparisons and loss of correction. Fisher’s exact test was used for proportions. Any p-values of 0.05 or less were considered significant.
Ethics
The study was approved by the Regional Ethics Committee of Linköping, Sweden (M29-08). Information about the study was given by one of the 2 authors, and written informed consent was obtained.
Results
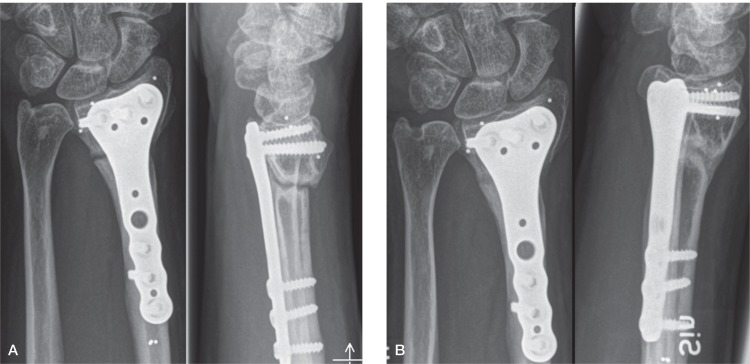
3 of the 15 osteotomies showed no evidence of clinical or radiographic healing after 6 months (Table 1). At an additional procedure, the non-unions were cleaned of fibrous tissue using a small dorsal approach. The opposing sclerotic surfaces were opened using a curette, and the void packed with non-structural autograft from the iliac crest. These all healed within 3 months (Figure 2). The 3 patients were not stastistically significantly older (p = 0.8) and had not had different time intervals between the fracture and the osteotomy from the cases that united after the index procedure (time intervals of 6, 8, and 14 months).
Table 1.
Cases with postoperative correction, additional factors, and outcome
| Correction |
|||||||
|---|---|---|---|---|---|---|---|
| Case | Age | Dorsal angle (°) | Ulnar variancea(mm) | Radial heighta(mm) | Trapezoid voidb | Smoking | Nonunion |
| 1 | 41 | 25 | 0 | 2 | |||
| 2 | 21 | 27 | 0 | 2 | |||
| 3 | 57 | 13 | 1 | 7 | Yes | ||
| 4 | 48 | 15 | 1 | −1 | |||
| 5 | 27 | 19 | 1 | 2 | |||
| 6 | 60 | 31 | 1 | 4 | Yes | Yes | Yes |
| 7 | 62 | 22 | 0 | 4 | Yes | ||
| 8 | 61 | 14 | 3 | 2 | Yes | ||
| 9 | 56 | 33 | 1 | −1 | |||
| 10 | 45 | 23 | 0 | 3 | Yes | Yes | |
| 11 | 49 | 8 | −2 | 0 | |||
| 12 | 56 | 40 | 4 | 10 | Yes | ||
| 13 | 53 | 32 | 1 | 4 | Yes | Yes | |
| 14 | 59 | 40 | 6 | 7 | Yes | ||
| 15 | 62 | 24 | 1 | 0 | |||
Negative values mean shortening of the radius in the PA view.
No cortical contact between the fragments.
Figure 2.
Non-union in case 13. A. 5 months postoperatively, with sclerosis of the cut surfaces. B. 3 months after revision, with non-structural iliac crest bone graft.
The defects in 6 of the 15 osteotomies were classified as being trapezoidal (Figure 1). A trapezoid void was associated with non-union (p = 0.044). 3 patients were smokers, 1 of whom had a trapezoid void that did not unite (Table 1). Measured on the lateral view, the center of the distal screws was positioned within 5 mm of the joint surface. The osteotomy started a median distance of 7 (4–13) mm proximal to the center of the distal screws. This position was not stastistically significantly different in the 3 non-unions when they were compared with the whole group or with the 3 other trapezoidal osteotomies.
No clinically important loss of correction was observed between the first postoperative radiograph and the one when the osteotomy had united. The dorsal angulation changed a median of 1° (p = 0.001), ulnar variance 0 mm, and radial height −0 mm. In the 3 non-unions, maximum loss of dorsal angulation was 4°, maximum loss of ulnar variance was 1 mm, and maximum loss of radial height was 1 mm.
Discussion
Our findings question the safety of not filling the void created by an open-wedge osteotomy of the distal radius. 3 non-unions out of 15 is an unacceptably high rate, considering that there are very few non-unions reported in most series using iliac crest autograft (Hove and Molster 1994, Flinkkila et al. 2000, Ring et al. 2002, Krukhaug and Hove 2007)—one estimation being about 1% (Prommersberger and Fernandez 2004)—or bone substitute (Luchetti 2004, Abramo et al. 2008, Scheer and Adolfsson 2009, Abramo et al. 2010).
Our results contrast with 4 other studies, which found no non-unions of distal radius osteotomies without the use of bone grafting or bone substitute in a total of 88 patients (Wieland et al. 2005, Mahmoud et al. 2012, Tarallo et al. 2014, Tiren and Vos 2014). Wieland et al. reported on 35 cases using dorsal pi-plates (Wieland et al. 2005). There is no information in the paper on whether or not trapezoid voids were created, but the authors clearly stated that they used a chisel rather than an oscillating saw.
Mahmoud et al. (2012) successfully treated 22 wrists using a palmar approach similar to ours. Only 3 of 22 of their osteotomies were trapezoidal in shape. About half of their patients were smokers, but how the osteotomy was created is not mentioned. The location of the osteotomies appears to have been similar to that in our study. This may be of importance, due to the possibility of different healing potential in different parts of the bone. In all our cases, the initial fracture extended into the metaphysis. 2 recent studies with 20 patients (Tarallo et al. 2014) and 11 patients (Tiren and Vos 2014) found similar good results, the latter paper clearly stating that there was cortical support of the osteotomies.
Bone healing following a fracture or an osteotomy is dependent on several factors, including cell differentiation, compromise of vascularity, and mechanical stability. Although there are few data on the subject of metaphyseal bone healing, there are some indications that it adheres to the same biomechanical principles as diaphyseal bone healing (Claes et al. 2011), even though bone formation may follow different paths (Aspenberg and Sandberg 2013). It appears that with large gaps, there may be less bone formation and less vascularization (Claes et al. 1997, Claes et al. 2003). All non-unions in our study were classified as having no cortical contact between the osteotomy fragments, a surrogate variable for gap size.
Vascularity is excellent in the metaphyseal area. The microcirculation may, however, be compromised by tobacco smoking (Meidinger et al. 2011, Moghaddam et al. 2011). In the present study, the only smoker with a trapezoid void had non-union (Table 1). The palmar approach to the distal radius includes reflection of the pronator quadratus muscle together with the periosteum. It cannot be ruled out that stripping of the soft tissues, particularly the well-vascularized muscle, could negatively influence the healing potential of the osteotomy.
We used an oscillating saw to perform the osteotomies. The thermal effect of the saw has been incriminated as a negative factor for bone healing (Toksvig-Larsen et al. 1991). The same method has, however, been used in several studies without adverse effects (Ring et al. 2002, Krukhaug and Hove 2007, Abramo et al. 2010) and it therefore appears unlikely that it would be of importance. The mechanical stability provided by the angle-stable locking plate used appears to be excellent, with minimal loss of correction, even in the cases that did not unite in 6 months.
The lack of a control group and the small size of the study population make any conclusions about the reason for the non-unions speculative, and there is possibly a combined effect of several factors. The conclusions must therefore be interpreted with caution.
Based on the results of this study, when an open-wedge osteotomy of the distal radius is performed, it may be safe not to fill the void if there is cortical contact between the fragments of the osteotomy. When a trapezoid defect is created, one should consider using bone substitute or autogenous bone graft.
Acknowledgments
JS and LA designed the study. JS collected data and performed the analyses. JS and LA both wrote the manuscript.
The research was funded by the County Council of Östergötland and by Linköping University, Sweden.
No competing interests declared.
References
- Abramo A, Tagil M, Geijer M, Kopylov P. Osteotomy of dorsally displaced malunited fractures of the distal radius: no loss of radiographic correction during healing with a minimally invasive fixation technique and an injectable bone substitute . Acta Orthop. 2008;79(2):262–8. doi: 10.1080/17453670710015085. [DOI] [PubMed] [Google Scholar]
- Abramo A, Geijer M, Kopylov P, Tagil M. Osteotomy of distal radius fracture malunion using a fast remodeling bone substitute consisting of calcium sulphate and calcium phosphate . J Biomed Mater Res B Appl Biomater. 2010;92(1):281–6. doi: 10.1002/jbm.b.31524. [DOI] [PubMed] [Google Scholar]
- Aspenberg P, Sandberg O. Distal radial fractures heal by direct woven bone formation . Acta Orthop. 2013;84(3):297–300. doi: 10.3109/17453674.2013.792769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claes L, Augat P, Suger G, Wilke HJ. Influence of size and stability of the osteotomy gap on the success of fracture healing . J Orthop Res. 1997;15(4):577–84. doi: 10.1002/jor.1100150414. [DOI] [PubMed] [Google Scholar]
- Claes L, Eckert-Hubner K, Augat P. The fracture gap size influences the local vascularization and tissue differentiation in callus healing . Langenbecks Arch Surg. 2003;388(5):316–22. doi: 10.1007/s00423-003-0396-0. [DOI] [PubMed] [Google Scholar]
- Claes L, Reusch M, Gockelmann M, Ohnmacht M, Wehner T, Amling M, et al. Metaphyseal fracture healing follows similar biomechanical rules as diaphyseal healing . J Orthop Res. 2011;29(3):425–32. doi: 10.1002/jor.21227. [DOI] [PubMed] [Google Scholar]
- Dijkman BG, Sprague S, Schemitsch EH, Bhandari M. When is a fracture healed? Radiographic and clinical criteria revisited . J Orthop Trauma. 2010;24(Suppl 1):S76–80. doi: 10.1097/BOT.0b013e3181ca3f97. [DOI] [PubMed] [Google Scholar]
- Flinkkila T, Raatikainen T, Kaarela O, Hamalainen M. Corrective osteotomy for malunion of the distal radius . Arch Orthop Trauma Surg. 2000;120(1-2):23–6. doi: 10.1007/pl00021237. [DOI] [PubMed] [Google Scholar]
- Goldfarb CA, Yin Y, Gilula LA, Fisher AJ, Boyer MI. Wrist fractures: what the clinician wants to know . Radiology. 2001;219(1):11–28. doi: 10.1148/radiology.219.1.r01ap1311. [DOI] [PubMed] [Google Scholar]
- Hove LM, Molster AO. Surgery for posttraumatic wrist deformity. Radial osteotomy and/or ulnar shortening in 16 Colles’ fractures . Acta Orthop Scand. 1994;65(4):434–8. doi: 10.3109/17453679408995488. [DOI] [PubMed] [Google Scholar]
- Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF. X-ray film measurements for healed distal radius fractures . J Hand Surg Am. 1996;21(1):31–9. doi: 10.1016/S0363-5023(96)80151-1. [DOI] [PubMed] [Google Scholar]
- Krukhaug Y, Hove LM. Corrective osteotomy for malunited extra-articular fractures of the distal radius: A follow-up study of 33 patients . Scand J Plast Reconstr Surg Hand Surg. 2007. pp. 1–7. [DOI] [PubMed]
- Kurmis AP, Kurmis TP, O’Brien JX, Dalen T. The effect of nonsteroidal anti-inflammatory drug administration on acute phase fracture-healing: a review . J Bone Joint Surg Am. 2012;94(9):815–23. doi: 10.2106/JBJS.J.01743. [DOI] [PubMed] [Google Scholar]
- Luchetti R. Corrective osteotomy of malunited distal radius fractures using carbonated hydroxyapatite as an alternative to autogenous bone grafting . J Hand Surg Am. 2004;29(5):825–34. doi: 10.1016/j.jhsa.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Mahmoud M, El Shafie S, Kamal M. Correction of dorsally-malunited extra-articular distal radial fractures using volar locked plates without bone grafting . J Bone Joint Surg Br. 2012;94(8):1090–6. doi: 10.1302/0301-620X.94B8.28646. [DOI] [PubMed] [Google Scholar]
- Meidinger G, Imhoff AB, Paul J, Kirchhoff C, Sauerschnig M, Hinterwimmer S. May smokers and overweight patients be treated with a medial open-wedge HTO? Risk factors for non-union . Knee Surg Sports Traumatol Arthrosc. 2011;19(3):333–9. doi: 10.1007/s00167-010-1335-6. [DOI] [PubMed] [Google Scholar]
- Moghaddam A, Zimmermann G, Hammer K, Bruckner T, Grutzner PA, von Recum J. Cigarette smoking influences the clinical and occupational outcome of patients with tibial shaft fractures . Injury. 2011;42(12):1435–42. doi: 10.1016/j.injury.2011.05.011. [DOI] [PubMed] [Google Scholar]
- Prommersberger KJ, Fernandez DL. Nonunion of distal radius fractures . Clin Orthop Relat Res. 2004;419:51–6. doi: 10.1097/00003086-200402000-00009. [DOI] [PubMed] [Google Scholar]
- Prommersberger KJ, Fernandez DL, Ring D, Jupiter JB, Lanz UB. Open reduction and internal fixation of un-united fractures of the distal radius: does the size of the distal fragment affect the result? . Chir Main. 2002a;21(2):113–23. doi: 10.1016/s1297-3203(02)00096-3. [DOI] [PubMed] [Google Scholar]
- Prommersberger KJ, Van Schoonhoven J, Lanz UB. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius . J Hand Surg [Br] 2002b;27(1):55–60. doi: 10.1054/jhsb.2001.0693. [DOI] [PubMed] [Google Scholar]
- Ring D, Roberge C, Morgan T, Jupiter JB. Osteotomy for malunited fractures of the distal radius: a comparison of structural and nonstructural autogenous bone grafts . J Hand Surg [Am] 2002;27(2):216–22. doi: 10.1053/jhsu.2002.32076. [DOI] [PubMed] [Google Scholar]
- Sasso RC, LeHuec JC, Shaffrey C. Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment . J Spinal Disord Tech. 2005;18:S77–81. doi: 10.1097/01.bsd.0000112045.36255.83. [DOI] [PubMed] [Google Scholar]
- Scheer JH, Adolfsson LE. Tricalcium phosphate bone substitute in corrective osteotomy of the distal radius . Injury. 2009;40(3):262–7. doi: 10.1016/j.injury.2008.08.013. [DOI] [PubMed] [Google Scholar]
- Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion . Spine. 2003;28(2):134–9. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- Steyers CM, Blair WF. Measuring ulnar variance: a comparison of techniques . J Hand Surg Am. 1989;14(4):607–12. doi: 10.1016/0363-5023(89)90175-5. [DOI] [PubMed] [Google Scholar]
- Tarallo L, Mugnai R, Adani R, Catani F. Malunited extra-articular distal radius fractures: corrective osteotomies using volar locking plate . J Orthop Traumatol. 2014;15(4):285–90. doi: 10.1007/s10195-014-0307-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiren D, Vos DI. Correction osteotomy of distal radius malunion stabilised with dorsal locking plates without grafting . Strategies Trauma Limb Reconstr. 2014;9(1):53–8. doi: 10.1007/s11751-014-0190-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toksvig-Larsen S, Ryd L, Lindstrand A. On the problem of heat generation in bone cutting. Studies on the effects on liquid cooling . J Bone Joint Surg Br. 1991;73(1):13–5. doi: 10.1302/0301-620X.73B1.1991747. [DOI] [PubMed] [Google Scholar]
- Wieland AW, Dekkers GH, Brink PR. Open wedge osteotomy for malunited extraarticular distal radius fractures with plate osteosynthesis without bone grafting. Eur J Trauma. 2005;31(2):148–53. [Google Scholar]