SUMMARY
Oncologic resection of head and neck cancers often results in complex reconstructive problems that can require local, regional, or free flaps. Herein, we present a case of a 67-year-old female with a history of floor of mouth cancer who had a second primary carcinoma in the left side of pharynx, 9 years after initial therapy. She underwent a wide oncologic resection requiring laryngopharyngeal reconstruction. Significant scar formation on the left side, due to previous surgery and radiotherapy, prevented us from harvesting an ipsilateral flap. Therefore, we used a right sided supraclavicular artery island flap for reconstruction of the contralateral defect. The patient healed completely with hyperbaric oxygen therapy and conservative local wound care. Supraclavicular artery island flap is a viable option for poor microvascular surgical candidates. It is easy and quick to harvest, and significantly decreases operative times. It is thus a versatile option for contralateral laryngopharyngeal reconstruction.
KEY WORDS: Head and neck reconstruction, Laryngopharyngeal defect, Supraclavicular artery island flap
RIASSUNTO
La resezione dei tumori della regione testa-collo spesso comporta complessi problemi ricostruttivi che possono necessitare di lembi locali, regionali o liberi. Presentiamo il caso di una donna di 67 anni con storia pregressa di tumore del pavimento buccale, che a 9 anni dalla prima neoplasia ha presentato un secondo carcinoma primitivo del faringe. La paziente è stata sottoposta ad un'ampia resezione che ha richiesto una ricostruzione faringo-laringea. La presenza di un ampia area cicatriziale omolaterale dovuta al precedente intervento chirurgico e alla successiva radioterapia ci ha impedito di prendere un lembo ipsilaterale. Pertanto, per la ricostruzione del difetto, abbiamo usato un lembo sovraclaveare ad isola controlaterale. La completa restitutio ad integrum è stata ottenuta con l'ausilio di ossigenoterapia iperbarica e terapia locale della ferita chirurgica. Il lembo sovraclaveare ad isola è un opzione interessante e percorribile in quei pazienti che per condizioni locali e generali siano candidati sub-ottimali al lembo microvascolare. Il lembo è inoltre di facile e rapida preparazione, e consente una significativa riduzione dei tempi operatori. Per tali motivi rappresenta un opzione versatile per la ricostruzione faringo-laringea controlaterale.
Introduction
Reconstruction of complex head and neck surgical defects remains one of the most challenging aspects of head and neck surgical oncology. The goal of reconstruction is not only limited to cover the defect, but also to restore anatomical function with similar skin colour and texture match at the recipient site 1. The ideal surgical reconstruction should have the lowest morbidity with minimal fistula or stricture rates, and allow early swallowing and speech rehabilitation. Oncologic resection of head and neck cancers often results in complex reconstructive problems that require dependable local, regional, or free flaps. Free tissue transfer has revolutionised reconstructive surgery but remains a complex procedure requiring microvascular equipment and surgeon expertise, availability of recipient vessels and a patient who can tolerate major surgery 2. Since advanced cancer patients are debilitated and malnourished, quick and simple reconstructions with local flaps are usually preferred 1. Supraclavicular artery island flap (SCAIF) is a safe, reliable, versatile, regional fasciocutaneous flap for the reconstruction of head and neck defects. It can be harvested easily and quickly with minimal donor-site morbidity.
The aim of this study is to evaluate the feasibility and efficacy of SCAIF for the reconstruction of a contralateral laryngopharyngeal defect. To the best of our knowledge, this is the first case demonstrating the use of SCAIF to reconstruct the opposite side.
Materials and methods
Preoperative evaluation
A 67-year-old woman with a history of floor of mouth cancer presented for evaluation of a pharyngeal mass. She had been treated with partial glossectomy and partial mandibulectomy with bilateral selective neck dissection as well as radiation therapy 10 years ago. One year after the operation, during regular follow-up a neck recurrence was detected and she underwent left radical neck dissection with intraoperative radiation therapy. During long term follow-up, she presented with a second primary carcinoma in the left side of pharynx 9-year after initial therapy. On endoscopic examination, the inferior oropharynx demonstrated a left posterior oropharyngeal lesion extending to the left pyriform sinus, approximately 3 × 3 cm in size. The larynx was intact with normal true vocal cord mobility bilaterally. The patient agreed to proceed with surgery. Total tumour resection with partial laryngopharyngectomy was planned. Since the patient had previously undergone left radical neck dissections as well as radiation therapy, the significant scarring on her left side limited to harvest a left sided flap. The decision was to use a right sided supraclavicular island flap for reconstruction of the left sided laryngopharyngeal defect.
Surgical technique
Under operative conditions, with the use of previous neck incision scar, sub-platysmal flaps were elevated and midline anterior pharyngotomy was performed at the level of the vallecula. This gave us good visualisation of the tumour. Resection included left pyriform sinus, left upper cervical oesophagus, up to the parapharyngeal tissues and prevertebral fascia together with the tonsillar fossa as well as lateral and posterior pharyngeal wall. After total tumour excision and confirmation of negative surgical margins with frozen sections, reconstruction was started.
A Doppler probe was used to identify the right supraclavicular vessels coursing from the transverse cervical pedicle in the triangle demarcated by the clavicle, sternocleidomastoid and external jugular vein. (Fig. 1) An ellipse shaped flap was planned out according to the pharyngeal defect.
Fig. 1.
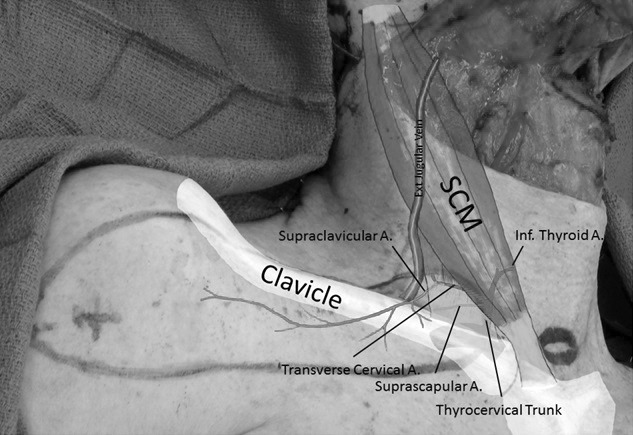
The origin of supraclavicular artery is demonstrated in the triangle formed by clavicle, SCM and external jugular vein. SCM: sternocleidomastoid muscle; Ext: external; inf.: inferior; A.: artery.
The skin, subcutaneous tissue, and the fascia down to the deltoid and pectoralis major muscles were incised. Further dissection was continued in the subfascial plane over the deltoid muscle and the flap was raised in the distal to proximal direction. A 3-4 cm pre-vertebral space tunnel was created at the level of larynx to transpose the right SCAIF to the left sided surgical defect. (Fig. 2) A diameter of approximately 3 cm of soft tissue was maintained around the origin of supraclavicular artery. A proximal portion of the skin paddle which would be lying under the tunnel was deepithelialised. The flap was advanced through the tunnel, behind the larynx into the left laryngopharyngeal defect. (Fig. 3) A tension free reconstruction of the pharynx was achieved all the way to base of tongue. (Figs. 4, 5) The donor site was closed primarily by extensive subcutaneous undermining and approximation of wound edges.
Fig. 2.

View of the pre-vertebral space tunnel at the level of larynx to transpose the right SCAIF to the left sided surgical defect. SCAIF: supraclavicular artery island flap.
Fig. 3.

Transposition of the flap through the tunnel.
Fig. 4.

View of laryngopharyngeal defect after flap transposition was completed.
Fig. 5.

The final position of the flap before suturing.
The patient recovered well postoperatively. She was initially monitored in the intensive care unit, but had no perioperative complications and was transferred to the floor on postoperative first day. She developed pharyngocutaneous fistula that healed completely in a couple of weeks with hyperbaric oxygen treatment and conservative local wound care.
Discussion
Extensive cancer resections of the face and neck often result in complex reconstructive problems that affect functional and aesthetic outcomes. Oro- and hypopharyngeal reconstructions can be a challenge due to their functional complexity and exposure to saliva and digestive enzymes 3.
For surgical reconstruction of pharyngeal defects, the ideal flap should allow early speech and swallowing function rehabilitation with minimal fistula and stricture rates 4.
Microsurgical transplantation of free flaps (radial forearm, anterolateral thigh, and fibula flap) provides pliable thin vascularised tissue to fill large defects, though they lack colour match to the face and neck. In addition, these flaps need trained surgeons for microsurgical techniques and special postoperative monitoring. High-risk patients (those with advanced age, advanced tumours, poor nutrition, or multiple medical issues) are not always good candidates for potentially prolonged microsurgery; therefore, regional flaps remain the preferred technique in these complicated cases 5.
Microsurgical reconstruction may be severely hampered in patients with a history of prior neck dissection and/ or irradiation, as in our patient, or contraindicated in patients with poor clinical conditions. In this context, The SCAIF is an ideal flap with a thin pliable tissue with superior texture and colour match for face and neck reconstruction 5. Although fasciocutaneous flaps based on the supraclavicular artery have been described for several decades, the use of has it recently popularised among head and neck surgeons. In 1997, Pallua et al. found that the supraclavicular artery island flap was both reliable and safe for releasing post-burn neck contractures after resecting cervical scars 3. In 2000, they demonstrated the use of the flap to reconstruct skin defects of the cheek, chin, and neck 1. Di Benedetto et al. in 2005, reported SCAIF as reliable for covering oral cavity defects after oncologic resections 4. Liu et al. described the use of this flap for functional pharyngeal reconstructions 5.
The SCAIF is a viable option for poor microvascular surgical candidates, or for those who do not wish to have a free tissue transfer. It can also serve an excellent first option in many other types of lower face and neck reconstructions, leaving major free flap surgeries and their higher associated costs as a backup option. SCAIF is easy and quick to harvest, and significantly decreases operative times. Flap donor site is in the same operative field and which can be closed primarily with minimal morbidity. The thin pedicle allows easy transfer of the island flap, which can be tunneled into a defect in the head and neck. The pedicle helps to fill the defect created by the neck dissection and covers the vessels of the neck 3. It is a versatile flap that should be kept as a valid option for head and neck reconstruction.
There are some limitations on the use of SCAIF that it cannot be used in patients undergoing radical neck dissection in whom the supraclavicular artery has been damaged. In addition, because of the variability in the vascular pattern, this flap cannot be used in patients with vascular anomalies or those with damage to the transverse vessels resulting from previous neck dissection 3 5. For successful use of the extensive pedicled SCAIF, consideration of vascular anatomy is extremely important, and preoperative assessment is essential.
As patients with advanced tumour usually present with impaired clinical conditions, shorter hospital stay with minimal surgical morbidity is preferred in their treatment. The SCAIF provides adequate tissue to perform even quite large and complex reconstructions. In our patient, prior radical neck dissection and extensive neck radiation on the lesion side resulted in severe fibrosis, vascular injury and tissue adhesions. Excessive scarring and muscle fibrosis can lead to formation of oropharyngeal stricture. This prevented us from using an ipsilateral SCAIF or other locoregional flaps, such as pectoralis major flap and deltopectoral flap. Therefore, our reconstructive method of choice was contralateral SCAIF.
Conclusions
SCAIF is a feasible and reliable local fasciocutaneous flap option with exceptional skin colour and texture match. Easy and quick harvest, minimal donor site morbidity and shorter operative time make it an ideal flap alternative for laryngopharyngeal and cutaneous reconstructions. Although technically challenging, the use of SCAIF in reconstruction of contralateral laryngopharyngeal defects is a convenient technique and should be reserved for selected cases.
References
- 1.Pallua N, Noah EM. The tunneled supraclavicular island flap: an optimized technique for head and neck reconstruction. Plast Reconstr Surg. 2000;105:842–851. doi: 10.1097/00006534-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Hanasono MM, Barnea Y, Skoracki RJ. Microvascular surgery in the previously operated and irradiated neck. Microsurgery. 2009;29:1–7. doi: 10.1002/micr.20560. [DOI] [PubMed] [Google Scholar]
- 3.Pallua N, Machens HG, Rennekampff O, et al. The fasciocutaneous supraclavicular artery island flap for releasing postburn mentosternal contractures. Plast Reconstr Surg. 1997;99:1878–1884. doi: 10.1097/00006534-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Benedetto G, Auinati A, Pierangeli M, et al. From the "charretera" to the supraclavicular fascial island flap: revisitation and further evolution of a controversial flap. Plast Reconstr Surg. 2005;115:70–76. [PubMed] [Google Scholar]
- 5.Liu PH, Chiu ES. Supraclavicular artery flap: a new option for pharyngeal reconstruction. Ann Plast Surg. 2009;62:497–501. doi: 10.1097/SAP.0b013e31818c9d7d. [DOI] [PubMed] [Google Scholar]


