SUMMARY
Obstructive sleep apnoea syndrome (OSAS) is associated with severe cerebro-cardiovascular morbidity and mortality. It is an independent risk factor for atherosclerosis, arterial thrombosis and metabolic syndrome, and recently has been associated with an increased incidence of cancer and death. A causal link between OSAS and atherosclerosis has been partially established. Recent research on atherosclerosis in OSAS has focused on thrombotic tendency and blood viscosity, providing new insight into disease mechanisms. Hypoxia is a critical pathophysiological element in OSAS that leads to intensive sympathetic activity, in association with inflammation, oxidative stress and procoagulant activity. Hypoxia and the induction of oxidative stress can simultaneously represent an underlying mechanism in the pathogenesis of cancer development and progression. This mini-review will discuss the latest findings on the association and potential relationship between OSA and pathological vascular sequelae.
KEY WORDS: Atherosclerosis, Cancer, Chronic intermittent hypoxia, Obstructive sleep apnoea, Sleep disruption
RIASSUNTO
La sindrome delle apnee ostruttive durante il sonno è associata ad un aumento della morbilità e mortalità cerebro-cardiovascolare. Si tratta di un fattore di rischio indipendente per aterosclerosi precoce, trombosi vascolare e sindrome metabolica e di recente è stata anche associata ad un aumento dell'incidenza di cancro. Un nesso di causalità tra OSAS ed aterosclerosi è parzialmente fondata ma non completamente chiarita. Una recente ricerca su aterosclerosi precoce in OSAS ha messo in correlazione la tendenza alla trombosi e la viscosità del sangue, fornendo una nuova visione dei meccanismi della malattia. L'ipossia intermittente notturna cronica tipica dell'OSAS insieme alle alterazioni macro e micro strutturali del sonno e la conseguente induzione ematica di stress ossidativo infiammatorio cronico cellulare con alterazioni genetiche possono contemporaneamente allo sviluppo di aterosclerosi precoce, rappresentare anche un meccanismo sottostante a lungo termine che induce atipie cellulari e patogenesi e progressione del cancro
Introduction
Increased atherosclerosis with cardiovascular morbidity and mortality is associated with obstructive sleep apnoea syndrome (OSAS); the association persists after controlling for diabetes, hypertension, smoking and dyslipidaemia 1. OSAS is characterised by recurrent episodes of complete or partial collapse of the upper airways during sleep, and can induce apnoea or hypopnoea, respectively, with recurrent episodes of intermittent hypoxia and higher carbon dioxide levels, leading to possible frequent interruption of sleep 2. The association between OSAS, cardiovascular disease and coagulation abnormalities was suspected for many years and is supported by large scale epidemiological and prospective studies 3-5. The mechanisms that mediate this association are not completely understood. The prognostic factors have not been determined, and studies to identify which patients are at higher risk have given controversial and disappointing results. Moreover, OSAS has been emerged as independently and strongly associated with cancer incidence and mortality 6. Current data suggest that inflammatory processes leading to endothelial dysfunction play a central pathogenic role in OSAS-related complications. Chronic intermittent hypoxia (CIH) and sleep disruption are considered important causes of cerebro-cardio-vascular diseases in OSAS patients. Oxidative stress induced by CHI is an important physiological mechanism of the disease 7. Increased blood clotting, caused by changes in the rheological properties (flow properties) of blood and plasma, seems to be an important factor linking OSAS to cardiovascular complications (CV) 8. CIH may be responsible for increased blood hypercoagulability (platelet activation and decreased fibrinolytic activity) which predisposes patients to thrombotic events 9. In addition, it is well known that chronic hypoxia plays an important role in regulating various stages of cancer formation and progression 6.
This review provides a critical analysis of the current evidence of an association between OSAS and haemostatic alterations, vascular remodelling/atherosclerosis and cancer. The aim is to discuss the contributing factors and potential mechanisms that may be responsible for this association.
Effects of chronic nocturnal intermittent hypoxia/sleep fragmentation: mechanisms of vascular remodelling in atherosclerosis
OSAS, via the chronic intermittent hypoxia and sleep disruption, can trigger the development of systemic inflammation 10, oxidative stress 11, endothelial dysfunction 12 and metabolic syndrome 13. Atherosclerosis is a chronic inflammatory disease that maintains a silent course for several decades before reaching clinical significance. The majority of studies have demonstrated a considerable mortality rate in OSAS, which is associated with the severity of atherosclerosis. The incidence of CV events, i.e. stroke, myocardial infarction, or CV death, is very high 14, with an odds ratio (OR) of CV events or mortality varying in magnitude from 2 to 7 for moderate to severe OSAS. This finding was confirmed by a subsequent study on 202 consecutive patients who were investigated with electron-beam computer tomography 15. Patients were asymptomatic in terms of their coronary artery disease (CAD) and were investigated by an overnight-sleep study, with a prevalence of OSAS of 76%. Coronary artery calcification (CAC) was found in 67% of OSAS patients and in 31% of non-OSAS patients (p ≤ 0.001). The median CAC score was 9 in OSAS patients and 0 in non-OSAS patients (p ≤ 0.001), strongly supporting the theory that OSAS is an independent risk factor for CAC.
CIH and sleep disruption leads to systemic hypertension due to the activation of the sympathetic system in patients on a high-cholesterol diet. The sympathetic hyperactivity determines haemodynamic alteration and high blood pressure, as well as cardiovascular inflammation (increased cell adhesion molecules, endothelial cell dysfunction, prothrombotic factor activation) and vascular remodelling 16. OSAS is also associated with insulin resistance and glucose intolerance, which are known risk factors for atherosclerosis 17. CIH can lead to insulin resistance and glucose intolerance in obese patients with dyslipidaemia 18. The intermittent hypoxia is a major stimulus for oxidative stress with the production of reactive oxygen species (ROS) that contributes to the generation of systemic inflammation characterised by inflammatory cell proliferation and cytokine/chemokine production 19<?> Moreover, CIH may trigger the activation of pro-inflammatory transcription factors including hypoxic inducible factor (HIF)-1α and nuclear factor (NF)-κB, which also share some gene products, such as inducible nitric oxide synthase 20. However, the role of HIF-1α is still controversial in OSAS studies 21. The transcriptional reprogramming induced by CIH includes the induction of cell adhesion molecules, such as intercellular adhesion molecule-1 (ICAM-1) and selectins, cytokines, such as tumour necrosis factor-α (TNF-α) and interleukin-6 (IL-6), chemokines, such as IL-8, and Creactive protein (CRP) 22. Other researchers have reported that CIH increases lipid peroxidation in the myocardial tissue of rats 23, and activates inflammatory pathways in vitro 24. Recently, it has been demonstrated that CIH significantly increased sizes of atherosclerotic lesions, and the mRNA levels of both cyclooxygenase (COX)-1 and thromboxane synthase (TXBS) 25. Lesion size was correlated with levels of COX-1 and TXBS mRNA, and treatment with the selective COX- 1 inhibitor SC-560 reduced lesion progression in intermittent hypoxia mice. This study has demonstrated, for the first time, that the activation of the COX-1 pathway in response to CIH is associated with increased atherosclerotic lesions in mice. In addition, in OSAS patients with cardiovascular risk factors an increase in urinary excretion of 11-dehydrothromboxane B2 (11-dTXB2) was observed, supporting the emerging role for COX-1 in CIH-induced vascular changes.
Detailed analysis of hypercoagulability in OSAS
Some studies have demonstrated considerable changes in haemostatic system components in OSAS patients, including platelet activation and increased plasma levels of tissue factor, von Willebrand factor (vWF) and fibrinogen 26 27. CIH and sleep disruption are a critical pathophysiological issue triggering greater sympathetic nervous system activity in association with the levels of markers of inflammation, such as oxidative stress and procoagulant activity. Hypercoagulability has been shown to be a risk factor for cardiovascular morbidity and mortality in OSAS patients 28. One possible explanation for the increase in blood coagulability is that during apnoea, desaturation triggers inflammatory factors, catecholamine and increased plasma levels of tissue factor as well as platelet aggregation, which alter capillary blood flow due to an increased sympathetic activity and a broader micro-endothelial damage, resulting in blood coagulability. Recently, one study has demonstrated increased pulmonary artery hypertension (PAH) in OSAS patients, which could be correlated with a genotypic heterogeneity with the plasminogen activator inhibitor-1 (PAI-1) 5G/5G polymorphism, possibly in relation with the severity of hypoxaemia and apnoea 29. vWF, a glycoprotein that plays an important role in stopping the escape of blood from vessels (haemostasis) following vascular injury, works by mediating the adherence of platelets to one another and to sites of vascular damage, preventing factor-VIII degradation. At present, the relation between OSAS and vWF is controversial, with some data showing an increase of vWF in patients with OSAS, and other data showing no significant differences between controls and patients 30 31. Increased levels of clotting factors XIIa (FXIIa) and VIIa (FVIIa), thrombin and antithrombin (TAT) has been shown in patients with OSAS. TAT is marker of thrombin turnover and indicates a tendency to blood coagulation disorders. TAT increased in patients with severe nocturnal desaturation, and FVIIa was found to be reduced in patients who practiced continuous positive airway pressure (CPAP) therapy 32.
Both FVIIa and FXIIa have been associated with increased mortality from CV diseases. The observed increase in the clotting factors in OSAS suggest that CIH may predispose to hypercoagulability 33. Robinson et al. 34 have found that serum levels of these clotting factors were not improved after one month of treatment with optimal CPAP therapy. A possible explanation may be that the short-term treatment with CPAP therapy was not able to facilitate the improvement of sympathetic activity and CIH. Since there are no long-term studies, the role of CPAP therapy remains unclear. Although not consistently 35 36, some studies have found a correlation between platelet activation and OSAS. The cause of the increased platelet activation in OSAS patients remains unclear, but the severity of OSAS seems to influence platelet aggregation as a function of nocturnal hypoxic time. A possible interpretation is the release/activation of catecholamines during oxygen desaturation, triggering more intensive platelet activation. OSAS patients have indeed increased levels of urinary adrenaline/noradrenaline that correlate with the degree of oxygen desaturation and apnoea index during sleep 37. The therapeutic use of CPAP treatment on platelet aggregation is controversial. CPAP therapy decreases urinary adrenaline/noradrenaline by enhancing its elimination from the blood. The study by Hui et al. 38 found that platelet aggregation decreases after one day for up to three months of treatment with CPAP therapy in patients with severe OSAS, without changes in the control group. Oga et al. 39 found that one month of treatment with CPAP is insufficient and only after 90 days of treatment with CPAP can a reduction in platelet activation be demonstrated. Therefore, data from the literature indicate that treatment with CPAP improves platelet aggregation, but the duration of therapy remains uncertain. Platelet activation results in the shedding of sub-microscopic membrane vesicles, known as platelet-derived microparticles (PDMPs), which are less than 1.5 μm in diameter and enriched in pro-coagulant platelet proteins. The membrane of PDMPs embraces all the properties of the activated platelet membrane, including the ability to bind to the components of pro-coagulant complexes, such as factor V (Va) and VIII (VIIIa). Plasma PDMPs have been shown to be amplified in patients with acute coronary syndrome, suggesting that PDMPs may play a role in the pathogenesis of arterial thrombosis in OSAS patients 40 41. Increased levels of the pro-coagulation factors soluble CD40 ligand (sCD40L) and soluble P-selectin (sP-selectin) have been demonstrated in OSAS patients in correlation with the degree of nocturnal desaturation. CPAP therapy reduces their plasma levels. CD40L and sP-selectin appear in plasma during the early stages of blood coagulation and are well-known indicators of thrombogenic conditions, such as disseminated intravascular coagulation (DIC). Furthermore, levels of sCD40L and sP-selectin are increased in patients with hypertension, hyperlipidaemia and diabetes mellitus 42 43.
Blood viscosity is defined as the internal resistance of the blood to shear forces. Blood viscosity is determined by plasma viscosity, haematocrit (volume fraction of erythrocytes, which constitutes 99.9% of the cellular elements) and the mechanical behaviour of erythrocytes. Increased blood clotting caused by changes in the rheological properties of blood and plasma seems to be an important factor linking OSAS and cardiovascular complications 44. Hyperviscosity is a potential mechanism for increased coagulability in OSAS 45 46, but the studies on this issue are limited by the small sample size and the absence of well-matched controls.
PAI-1, a member of the serine protease inhibitor family, inhibits fibrinolytic activity by binding to tissue type plasminogen activator (tPA). It was demonstrated that higher apnoeahypopnoea index (AHI)/hs and Nadir SaO2% were both associated with a higher concentration of circulating PAI-1 in a group of OSAS patients 47. Increased concentrations of PAI-1 in OSAS predicted the occurrence of acute myocardial infarction in middle-aged men and women with a high prevalence of coronary heart disease 48 49. However, many uncertainties still remain as to the independent effects of OSAS on increased blood coagulability, largely due to the common co-existence of other CV risk factors and the incomplete normalisation of coagulation after CPAP treatment 50.
Venous thromboembolism and OSAS
There are limited data in the literature that have shown a relationship between venous thromboembolism (VTE) and pulmonary embolism (PE) in association with a coagulation- related clinical problem. The above studies are not extensive nor do they have a control group 51 52. These data suggest a high prevalence of OSAS in patients with PE. A retrospective study 53 showed a percentage higher than in the general population, accounting for 15.5% of OSAS in patients with VTE. The study is, however, limited due to incomplete instrumental diagnostics, since data on polysomnography is missing. A review 54 of the current considerable evidence demonstrates that OSAS is associated with a procoagulant state, although the relationship between OSAS and individual clotting factors are uncertain. More clinical studies are needed in order to better control for confounding factors such as cardiovascular morbidity and mortality, demonstrating that a hypercoagulability state is induced by OSAS before the onset of cardiovascular disorders
CHI and cancer: future perspectives for research
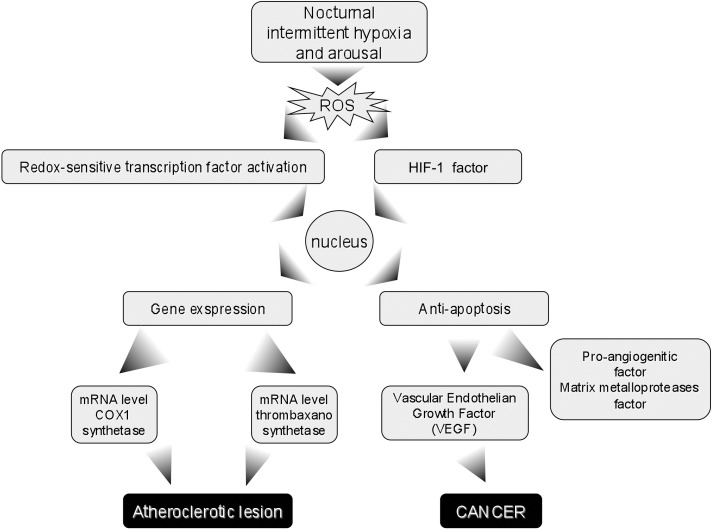
CIH and sleep disruption are known to trigger pathophysiological pathways leading to systemic disease. In fact, OSAS has been associated with diseases with a high inflammatory potential, such as psoriasis and other autoimmune disorders 55. The potential mechanisms involved in hypoxia- driven cancer development and progression have been previously investigated 56. Moreover, it has been shown that nocturnal intermittent hypoxia can regulate different stages of cell differentiation and proliferation. Cellular hypoxia (also present in cancer) and the adaptive response is related to a family of transcription factors, the most significant being HIF-1, which activates the transcription of genes that play a fundamental role in angiogenesis and genetic modification, with the formation of cancer-related stem cells 57. The HIF-1 pathway has been associated with a considerable increase in ROS generation during periods of hypoxia/reoxygenation, which may play an important role in modifying gene expression by regulating the activity of some redox-sensitive transcription factors. These include activator protein (AP)-1, which may play a key role in carcinogenesis through the induction of apoptotic inhibitory factors, matrix metalloproteases and pro-angiogenic factors including vascular endothelial growth factor (VEGF).
A recent animal model study has spurred an emerging pathophysiological hypothesis linking OSAS to cancer. The authors have demonstrated that when mice are exposed to intermittent hypoxia mimicking OSAS, the frequency of melanoma was twice high as in normal controls 58.
These promising results in experimental animals have encouraged studies on humans with the aim of evaluating the potential link between OSAS and cancer. Two independent large-scale clinical studies have recently investigated this possible relation. The first assessed the association between OSAS and cancer in a cohort of patients from Wisconsin (USA) (1,522 subjects), and showed a significant increase in the likelihood of cancer death in patients with severe OSAS 59. Another database, called the Spanish Sleep Network, involved 5,000 patients with a median 5-year follow-up and found that OSA is associated with increased incidence of cancer. These two studies reported an increased cancer incidence and mortality in OSAS patients compared with those who do not have OSAS, also after adjustment for important confounders (age, sex, smoking, alcohol consumption and body mass index). In this context, it can be hypothesised that nocturnal intermittent hypoxia and consequent sleep disruption may play a key role in cancer development (Fig. 1). It would be important to determine whether the OSAS-cancer combination gives rise to a specific histological type of tumour, since different types of malignant cells have different adaptive responses to intermittent hypoxia. The identification of confounding factors will also be significant. A key issue that deserves further study is the potential role of CPAP therapy in cancer risk associated with OSA, and to investigate whether the effect of anti-cancer drugs is changed following treatment of CPAP.
Fig. 1.
Potential biological pathways mediating the development of atherosclerosis and cancer in sleep apnoea.
Conclusions and future guidelines
The available data highlight that patients with OSAS experience a pro-coagulant condition that may represent a contributing factor in the development and progression of vascular diseases. The potential for anticoagulant and antiplatelet drugs to decrease morbidity/mortality is worth further investigation. Broad randomised studies will be necessary to provide greater statistic power in order to determine whether the treatment of OSAS with CPAP/drugs can stop or even reverse vascular remodelling, atherosclerosis progression and, ultimately, reduce the rate of cardiovascular disease. The possible relationship between OSAS and cancer is a good gateway for further research and an opportunity to perform international clinical studies that can answer the many open questions still remaining.
References
- 1.McNicholas WT, Bonsigore MR. Management Committee of EU COST ACTION B26. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29:156–178. doi: 10.1183/09031936.00027406. [DOI] [PubMed] [Google Scholar]
- 2.Eckert DJ, Malhotra A, Jordan AS. Mechanisms of apnea. Prog Cardiovasc Dis. 2009;51:313–323. doi: 10.1016/j.pcad.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-yrs follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 4.Marshall NS, Wong KK, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–1085. [PMC free article] [PubMed] [Google Scholar]
- 5.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132–e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim R, Kapur VK. Emerging from the shadows: a possible link between sleep apnea and cancer. J Clin Sleep Med. 2014;10:363–364. doi: 10.5664/jcsm.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lavie L. Oxidative stress--a unifying paradigm in obstructive sleep apnea and comorbidities. Prog Cardiovasc Dis. 2009;51:303–312. doi: 10.1016/j.pcad.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Bairey Merz CN, Alberts MJ, Balady GJ, et al. ACCF/AHA/ ACP 2009 competence and training statement: a curriculum on prevention of cardiovascular disease: a report of the American College of Cardiology Foundation/American Heart Association/ American College of Physicians Task Force on Competence and Training (Writing Committee to Develop a Competence and Training Statement on Prevention of Cardiovascular Disease): developed in collaboration with the American Academy of Neurology; American Association of Cardiovascular and Pulmonary Rehabilitation; American College of Preventive Medicine; American College of Sports Medicine; American Diabetes Association; American Society of Hypertension; Association of Black Cardiologists; Centers for Disease Control and Prevention; National Heart, Lung, and Blood Institute; National Lipid Association; and Preventive Cardiovascular Nurses Association. Circulation. 2009;120:e100–e126. doi: 10.1161/CIRCULATIONAHA.109.192640. [DOI] [PubMed] [Google Scholar]
- 9.Känel R, Dimsdale JE. Hemostatic alterations in patients with obstructive sleep apnea and the implications for cardiovascular disease. Chest. 2003;124:1956–1967. doi: 10.1378/chest.124.5.1956. [DOI] [PubMed] [Google Scholar]
- 10.Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. 2005;112:2660–2667. doi: 10.1161/CIRCULATIONAHA.105.556746. [DOI] [PubMed] [Google Scholar]
- 11.Lavie L, Lavie P. Molecular mechanisms of cardiovascular disease in OSAHS: the oxidative stress link. Eur Respir J. 2009;33:1467–1484. doi: 10.1183/09031936.00086608. [DOI] [PubMed] [Google Scholar]
- 12.Jelic S, Padeletti M, Kawut SM, et al. Inflammation, oxidative stress, and repair capacity of the vascular endothelium in obstructive sleep apnea. Circulation. 2008;117:2270–2278. doi: 10.1161/CIRCULATIONAHA.107.741512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tanno S, Tanigawa T, Saito I, et al. Sleep-related intermittent hypoxemia and glucose intolerance: a community-based study. Sleep Med. 2014;pii:S1389–S9457. doi: 10.1016/j.sleep.2014.05.027. 00277-9. [DOI] [PubMed] [Google Scholar]
- 14.Martínez-García MA, Soler-Cataluña JJ, Ejarque-Martínez L, et al. Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med. 2009;180:36–41. doi: 10.1164/rccm.200808-1341OC. [DOI] [PubMed] [Google Scholar]
- 15.Sorajja D, Gami AS, Somers VK, et al. Independent association between obstructive sleep apnea and subclinical coronary artery disease. Chest. 2008;133:927–933. doi: 10.1378/chest.07-2544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavie L. Oxidative stress in obstructive sleep apnea and intermittent hypoxia - Revisited - The bad ugly and good: Implications to the heart and brain. Sleep Med Rev. 2014:S1087- 0792(14)00077-X–S1087- 0792(14)00077-X. doi: 10.1016/j.smrv.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Lam DC, Lam KS, Ip MS. Obstructive sleep apnoea, insulin resistance and adipocytokines. Clin Endocrinol (Oxf) 2015;82:165–177. doi: 10.1111/cen.12597. [DOI] [PubMed] [Google Scholar]
- 18.Drager LF, Yao Q, Hernandez KL, et al. Chronic intermittent hypoxia induces atherosclerosis via activation of adipose angiopoietin- like 4. Am J Respir Crit Care Med. 2013;188:240–248. doi: 10.1164/rccm.201209-1688OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Testelmans D, Tamisier R, Barone-Rochette G, et al. Profile of circulating cytokines: impact of OSA, obesity and acute cardiovascular events. Cytokine. 2013;62:210–216. doi: 10.1016/j.cyto.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 20.Toffoli S, Roegiers A, Feron O, et al. Intermittent hypoxia is an angiogenic inducer for endothelial cells: role of HIF-1. Angiogenesis. 2009;12:47–67. doi: 10.1007/s10456-009-9131-y. [DOI] [PubMed] [Google Scholar]
- 21.Ryan S, McNicholas WT. Inflammatory cardiovascular risk markers in obstructive sleep apnoea syndrome. Cardiovasc Hematol Agents Med Chem. 2009;7:76–81. doi: 10.2174/187152509787047685. [DOI] [PubMed] [Google Scholar]
- 22.Chen L, Einbinder E, Zhang Q, et al. Oxidative stress and left ventricular function with chronic intermittent hypoxia in rats. Am J Respir Crit Care Med. 2005;172:915–920. doi: 10.1164/rccm.200504-560OC. [DOI] [PubMed] [Google Scholar]
- 23.Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. 2005;112:2660–2667. doi: 10.1161/CIRCULATIONAHA.105.556746. [DOI] [PubMed] [Google Scholar]
- 24.Burioka N1, Koyanagi S, Fukuoka Y, et al. Influence of intermittent hypoxia on the signal transduction pathways to inflammatory response and circadian clock regulation. Life Sci. 2009;85:372–378. doi: 10.1016/j.lfs.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Gautier-Veyret E, Arnaud C, Bäck M, et al. Intermittent hypoxia- activated cyclooxygenase pathway: role in atherosclerosis. Eur Respir J. 2013;42:404–413. doi: 10.1183/09031936.00096512. [DOI] [PubMed] [Google Scholar]
- 26.El Solh AA, Akinnusi ME, Berim IG, et al. Hemostatic implications of endothelial cell apoptosis in obstructive sleep apnea. Sleep Breath. 2008;12:331–337. doi: 10.1007/s11325-008-0182-x. [DOI] [PubMed] [Google Scholar]
- 27.Akinnusi ME, Paasch LL, Szarpa KR, et al. Impact of nasal continuous positive airway pressure therapy on markers of platelet activation in patients with obstructive sleep apnea. Respiration. 2009;77:25–31. doi: 10.1159/000158488. [DOI] [PubMed] [Google Scholar]
- 28.Tkacova R, McNicholas WT, Javorsky M, et al. Nocturnal intermittent hypoxia predicts prevalent hypertension in the European Sleep Apnoea Database cohort study. Eur Respir J. 2014;44:931–941. doi: 10.1183/09031936.00225113. [DOI] [PubMed] [Google Scholar]
- 29.Toraldo DM, Nuccio F, Mauro S, et al. Frequency of human leukocyte antigens, plasminogen activator inhibitor-1 and methylenetetrahydrofolate reductase gene polymorphisms in obstructive sleep apnea-hypopnea syndrome with or without pulmonary artery hypertension. J Sleep Disorders Ther. 2013;2:131–131. [Google Scholar]
- 30.Robinson GV, Pepperell JC, Segal HC, et al. Circulating cardiovascular risk factors in obstructive sleep apnoea: data from randomised controlled trials. Thorax. 2004;59:777–782. doi: 10.1136/thx.2003.018739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Känel R, Loredo JS, Ancoli-Israel S, et al. Association between sleep apnea severity and blood coagulability: Treatment effects of nasal continuous positive airway pressure. Sleep Breath. 2006;10:139–146. doi: 10.1007/s11325-006-0060-3. [DOI] [PubMed] [Google Scholar]
- 32.Peker Y, Redline S. Update in sleep medicine 2013. Am J Respir Crit Care Med. 2014;189:1345–1350. doi: 10.1164/rccm.201403-0497UP. [DOI] [PubMed] [Google Scholar]
- 33.Basner RC. Cardiovascular morbidity and obstructive sleep apnea. N Engl J Med. 2014;370:2339–2341. doi: 10.1056/NEJMe1404501. [DOI] [PubMed] [Google Scholar]
- 34.Robinson GV, Pepperell JC, Segal HC, et al. Circulating cardiovascular risk factors in obstructive sleep apnoea: data from randomised controlled trials. Thorax. 2004;59:777–782. doi: 10.1136/thx.2003.018739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rångemark C, Hedner JA, Carlson JT, et al. Platelet function and fibrinolytic activity in hypertensive and normotensive sleep apnea patients. Sleep. 1995;18:188–194. doi: 10.1093/sleep/18.3.188. [DOI] [PubMed] [Google Scholar]
- 36.Reinhart WH, Oswald J, Walter R, et al. Blood viscosity and platelet function in patients with obstructive sleep apnea syndrome treated with nasal continuous positive airway pressure. Clin Hemorheol Microcirc. 2002;27:201–207. [PubMed] [Google Scholar]
- 37.Hui DS, Ko FW, Fok JP, et al. The effects of nasal continuous positive airway pressure on platelet activation in obstructive sleep apnea syndrome. Chest. 2004;125:1768–1775. doi: 10.1378/chest.125.5.1768. [DOI] [PubMed] [Google Scholar]
- 38.Oga T, Chin K, Tabuchi A, et al. Effects of obstructive sleep apnea with intermittent hypoxia on platelet aggregability. J Atheroscler Thromb. 2009;16:862–869. doi: 10.5551/jat.2188. [DOI] [PubMed] [Google Scholar]
- 39.Mills PJ, Kennedy BP, Loredo JS, et al. Effects of nasal continuous positive airway pressure and oxygen supplementation on norepinephrine kinetics and cardiovascular responses in obstructive sleep apnea. J Appl Physiol. 2006;100:343–348. doi: 10.1152/japplphysiol.00494.2005. [DOI] [PubMed] [Google Scholar]
- 40.Phillips CL, McEwen BJ, Morel-Kopp MC, et al. Effects of continuous positive airway pressure on coagulability in obstructive sleep apnoea: a randomized, placebo-controlled crossover study. Thorax. 2012;67:639–644. doi: 10.1136/thoraxjnl-2011-200874. [DOI] [PubMed] [Google Scholar]
- 41.Shamsuzzaman A, Amin RS, Calvin AD, et al. Severity of obstructive sleep apnea is associated with elevated plasma fibrinogen in otherwise healthy patients. Sleep Breath. 2014;18:751–756. doi: 10.1007/s11325-014-0938-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weinreich G, Wessendorf TE, Erdmann T, et al. Recall (HNR) study group. Association of obstructive sleep apnoea with subclinical coronary atherosclerosis. Atherosclerosis. 2013;231:191–197. doi: 10.1016/j.atherosclerosis.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 43.Toraldo DM, Peverini F, Benedetto M, et al. Obstructive sleep apnea syndrome: blood viscosity, blood coagulation abnormalities, and early atherosclerosis. Lung. 2013;191:1–7. doi: 10.1007/s00408-012-9427-3. [DOI] [PubMed] [Google Scholar]
- 44.Steiner S, Jax T, Evers S, et al. Altered blood rheology in obstructive sleep apnea as a mediator of cardiovascular risk. Cardiology. 2005;104:92–96. doi: 10.1159/000086729. [DOI] [PubMed] [Google Scholar]
- 45.Tazbirek M, Slowinska L, Skoczynski S, et al. Short-term continuous positive airway pressure therapy reverses the pathological influence of obstructive sleep apnea on blood rheology parameters. Clin Hemorheol Microcirc. 2009;41:241–249. doi: 10.3233/CH-2009-1175. [DOI] [PubMed] [Google Scholar]
- 46.Lima AM, Franco CM, Castro CM, et al. Effects of nasal continuous positive airway pressure treatment on oxidative stress and adiponectin levels in obese patients with obstructive sleep apnea. Respiration. 2010;79:370–376. doi: 10.1159/000227800. [DOI] [PubMed] [Google Scholar]
- 47.Ren W, Wang Z, Hua F, et al. Plasminogen activator inhibitor- 1 regulates LPS-induced TLR4/MD-2 pathway activation and inflammation in alveolar macrophages. Inflammation. 2015;38:384–393. doi: 10.1007/s10753-014-0042-8. [DOI] [PubMed] [Google Scholar]
- 48.Barceló A, Llompart E, Barbé F, et al. Plasminogen activator inhibitor-I (PAI-I) polymorphisms in patients with obstructive sleep apnoea. Respir Med. 2002;96:193–196. doi: 10.1053/rmed.2001.1239. [DOI] [PubMed] [Google Scholar]
- 49.Känel R, Loredo JS, Ancoli-Israel S, et al. Elevated plasminogen activator inhibitor 1 in sleep apnea and its relation to the metabolic syndrome: an investigation in 2 different study samples. Metabolism. 2007;56:969–976. doi: 10.1016/j.metabol.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 50.Steiropoulos P, Tsara V, Nena E, et al. Effect of continuous positive airway pressure treatment on serum cardiovascular risk factors in patients with obstructive sleep apnea-hypopnea syndrome. Chest. 2007;132:843–851. doi: 10.1378/chest.07-0074. [DOI] [PubMed] [Google Scholar]
- 51.Ambrosetti M, Lucioni A, Ageno W, et al. Is venous thromboembolism more frequent in patient with obstructive sleep apnea syndrome! Thromb Haemost. 2004;2:1858–1860. doi: 10.1111/j.1538-7836.2004.00913.x. [DOI] [PubMed] [Google Scholar]
- 52.Epstein MD, Segal LN, Ibrahim SM, et al. Snoring and the risk of obstructive sleep apnea in patients with pulmonary embolism. Sleep. 2010;33:1069–1074. doi: 10.1093/sleep/33.8.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bosanquet JP, Bade BC, Zia MF, et al. Patients with venous thromboembolism appear to have higher prevalence of obstructive sleep apnea than general population. Clin Appl Thromb Hemost. 2011;17:E119–E124. doi: 10.1177/1076029610389023. [DOI] [PubMed] [Google Scholar]
- 54.Liak C, Fitzpatrick M. Coagulability in obstructive sleep apnea. Can Respir J. 2011;18:338–348. doi: 10.1155/2011/924629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kang JH, Lin HC. Obstructive sleep apnea and the risk of autoimmune diseases: a longitudinal population-based study. Sleep Med. 2012;13:583–588. doi: 10.1016/j.sleep.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 56.Carmelites P, Dor Y, Herbert JM, et al. Role of HIF-1a in hypoxia mediatedapoptosis, cell proliferation and tumour angiogenesis. Nature. 1998;394:485–490. doi: 10.1038/28867. [DOI] [PubMed] [Google Scholar]
- 57.Semenza G.L. Oxygen sensing, homeostasis and disease. N Engl J Med. 2011;365:537–547. doi: 10.1056/NEJMra1011165. [DOI] [PubMed] [Google Scholar]
- 58.Almendros I, Montserrat JM, Ramírez J, et al. Intermittent hypoxia enhances cancer progression in a mouse model of sleep apnoea. Eur Respir J. 2012;39:215–217. doi: 10.1183/09031936.00185110. [DOI] [PubMed] [Google Scholar]
- 59.Nieto FJ, Peppard PE, Young T, et al. Sleep disordered breathing and cancer mortality: Results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2012;186:190–194. doi: 10.1164/rccm.201201-0130OC. [DOI] [PMC free article] [PubMed] [Google Scholar]