SUMMARY
Juvenile nasopharyngeal angiofibroma (JNA) is a disease of adolescent males characterised by high vascularity with local aggressiveness. This analysis was intended to see the effectiveness of radiation in locally advanced JNA. We included patients treated from 1990-2012. A total of 31 patients met study criteria. Median age was 16 years (range: 12-33 years). Radiation was used for refractory, residual or unresectable locally advanced disease. The median radiation dose was 30 Gy (range: 30-45 Gy). Median follow-up was 36 months (Range: 1-271 months). The median progression-free survival [PFS] was not reached. PFS at 3, 5 and 10 years was 91.7, 70.7 and 70.7% respectively. Three patients progressed at 38, 43 and 58 months after completion of treatment and opted for alternative therapy. One patient developed squamous cell carcinoma of the nasal ale 15 years after radiation.
KEY WORDS: Juvenile, Nasopharyngeal, Angio-fibroma, Radiotherapy
RIASSUNTO
L'angiofibroma nasofaringeo giovanile (Juvenile Nasopharyngeal angiofibroma o JNA) è una patologia tipica dei ragazzi in età adolescenziale nota per essere riccamente vascolarizzata e localmente aggressiva. L'obiettivo dello studio è stato quello di valutare l'efficacia del trattamento radioterapico nell'angiofibroma nasofaringeo localmente avanzato. Abbiamo arruolato pazienti trattati in un periodo compreso tra il 1990 ed il 2012. 31 pazienti sono risultati confacenti ai criteri di inclusione dello studio, con un'età media di 16 anni (range: 12-33 anni). Il trattamento radioterapico è stato effettuato in pazienti con malattia localmente avanzata residua, refrattaria ai precedenti trattamenti o non resecabile. La dose media somministrata era di 30 Gray (range: 30-45 Gray) con un follow-up medio di 36 mesi (range: 1-271mesi). A 3, 5 e 10 anni si è registrata una percentuale di sopravvivenza libera da progressione del 91.7, 70.7 e 70.7%, rispettivamente. La progressione è avvenuta in tre pazienti rispettivamente 38, 43 e 58 mesi dopo aver completato il trattamento e gli stessi hanno dunque optato per un trattamento alternativo. Un paziente ha sviluppato un carcinoma squamo cellulare dell'ala nasale 15 anni dopo il trattamento radioterapico.
Introduction
Juvenile nasopharyngeal angiofibroma (JNA) is a benign, locally aggressive tumour found commonly in young boys 1 2. The internal maxillary artery is the most common vascular source of JNAs followed by the ascending pharyngeal artery. Intracranial involvement has been reported to occur in 10% to 37% of all cases 3 4. Staging is based on anatomic tumour extension, and the Radkowski system of staging is used most frequently. Over the years surgical excision has remained standard treatment 5. Transnasal endoscopic resection is generally used in early stages, while advanced cases require craniofacial approaches 6. The availably of pre-operative embolisation has helped surgeons in reducing bleeding during surgery and improve outcomes of surgery 7. However, surgery alone in advanced stages has reported high recurrence rates especially if resection is not complete, and there is little consensus regarding the management of such patients. The high rate of recurrence in cases has paved way for adjuvant radiotherapy, especially in patients with residual disease after surgery. There is also much debate regarding early postoperative radiotherapy vs. delayed radiotherapy on progression. There is also a group of patients in whom surgery is not feasible where an option of radical radiotherapy is an option. The long term morbidity associated with radiotherapy has remained a concern 8. In recent years the introduction of conformal radiotherapy has made it possible to deliver radiation with precision and minimal morbidity 9 10. Herein, we present data on patients with stage III JNA treated with radiotherapy at our institute by conformal techniques.
Materials and methods
We performed a retrospective review of patients with JNA undergoing radiotherapy in our institute from 1990 to 2012. Data regarding clinical features, treatment details and outcomes of 31 patients were recorded in a predesigned proforma. Data was analysed and categorical variables were summarised by frequency (%) and quantitative variables were summarised by median and range. The survival analysis of the data was done using Kaplan- Meier test.
Radiotherapy
A customised thermoplastic cast was used for immobilisation. A CECT simulation was done using a Philips™ CT scanner with 3 mm slice thickness following intravenous contrast injection [1 mg/kg body weight]. Whole cranium and the paranasal sinus were scanned. In the pre-ICRU era, radiotherapy was delivered to residual disease with 1 cm expansion. Thereafter, the GTV was delineated as evident on the planning CT scan. An isotropic expansion of 5 mm was added to form the PTV. The planning was done using the Eclipse treatment planning system version 6.5 (Varian Medical Systems, Palo Alto, CA) or Pinnacle treatment planning system version 9.0. Treatment was delivered by 3D conformal radiotherapy [3D-CRT] in 30 patients, while for one it was by conventional technique. During radiotherapy planning first priority was given to achieve a conformal dose distribution to the PTV followed by maximal sparing of the optic structures.
Response assessment and follow-up
The patients were followed at one month after completion of radiation and subsequently every three months with clinical examination and endoscopy. A contrast-enhanced CECT of the head and face was ordered once in a year.
Results
Patient characteristics
Median age of this cohort of patients was 16 years (range: 12-33 years). Epistaxis was the commonest presenting symptom found in 24 [77.4%] patients followed by nasal blockade (n = 19) and proptosis (n = 12). Ophthalmic evaluation revealed vision abnormalities in 14 (45.1%) patients. All patients were thoroughly evaluated with contrast enhancing CT scan or contrast enhanced MRI. Imaging revealed gross intracranial extension in 19 (61.2%), orbital involvement in eight [25.8%] and cavernous sinus involvement in 12 (38.7%) patients. All the patients were in Radkowski stage III (Table I). The clinical characteristics are summarised in Table II.
Table I.
Radowski's modification of Sessions' classification.
| Stage | Tumour extent |
|---|---|
| Ia | Limited to the posterior nares and/or nasopharyngeal vault |
| Ib | Involving the posterior nares and/or nasopharyngeal vault with involvement of at least one paranasal sinus |
| IIa | Minimal lateral extension to the pterygomaxillary fossa |
| IIb | Full occupation of the pterygomaxillary fossa with or without superior erosion orbital bones |
| IIc | Extension into the infratemporal fossa or extension posterior to the pterygoid plates |
| IIIa | Erosion of the base of the skull (middle cranial fossa/base of pterygoids) – minimal intracranial extension |
| IIIb | Extensive intracranial extension with or without extension into the cavernous sinus |
Table II.
Patient characteristics.
| Characteristics | (N = 31) |
|---|---|
| Age | |
| Median | 16 years |
| Range | 12-33 years |
| Symptoms | |
| Epistaxis | 24 |
| Nasal blockade | 19 |
| Proptosis | 12 |
| Loss of vision | 14 |
| Stage | |
| III | 31 |
| Surgery | |
| Yes | 22 |
| No | 9 |
Surgery
Surgery was done in 22 patients (70.9%). Lateral rhinotomy was the most common surgical approach. Since complete excision of the tumour was difficult in most cases, decompression of the tumour was done in the majority of cases undergoing surgery.
Radiotherapy
Radiotherapy was given with radical intent in 10 patients and postoperative radiotherapy was given in 10 patients. It was given in a salvage or recurrent setting in 11 patients. The radiation dose of 30-50 Gy (median 32.5 Gy) was prescribed at 1.8-2 Gy per fraction. A two field technique (anterior + lateral) or a three field technique was used for treatment delivery. Since the dose required was less that optimal, sparing of organs at risk without compromising coverage of PTV could be achieved in most of cases using 3D-CRT. The dosimetric characteristics are summarised in Table III.
Table III.
Dosimetry of 3D-conformal plan [OAR-Organ at risk].
| OAR | Dmax Gy (Median) and Range |
|---|---|
| Brainstem | 31.06 [10.40-49.84] |
| Eye | 30.67 [4.56-47.00] |
| Optic nerve | 32.50 [2.71-52.21] |
| Optic chiasm | 31.13 [20.47-50.06] |
| Spinal Cord | 20.68 [3.99-40.01] |
All patients tolerated the prescribed dose without grade III or Grade IV acute toxicity. Grade II mucosal reaction was the most common acute toxicity followed by Grade I skin reaction and grade II conjunctival reaction.
Survival outcomes
Median follow-up was 36 months (range 1-271 months). Three patients were found to have progressive disease, while three patients showed features of slow regression documented in MRI/CECT scan done every three months suggestive of disease control. Hence, disease control could be achieved in 28 patients (90.3%). The median progression-free survival (PFS) was not reached. PFS at 3, 5 and 10 years was 91.7%, 70.7% and 70.7% respectively. The survival curve is shown in Fig. 2. One patient developed squamous cell carcinoma of the nasal ale 9 years after diagnosis of JNA in the radiation field likely due to radiation-induced second malignancy. The patient underwent surgical salvage and was disease-free at seven years after the salvage treatment.
Fig. 2.
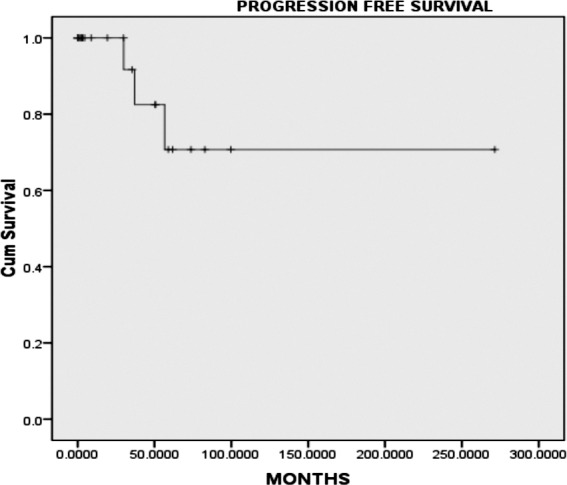
Kaplan-Meier survival curve (progression-free survival).
Fig. 1.
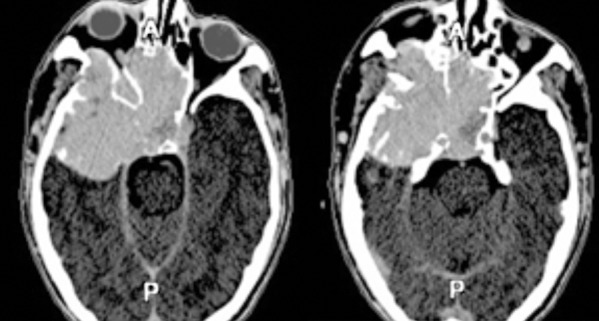
Axial CECT image of a case of JNA with intracranial extension.
Discussion
Management of locally advanced JNA has long remained a challenge. Gross total excision is always attempted whenever possible for long term disease control. However, the presence of skull base involvement or intracranial extension makes most patients not amenable for complete surgical resection 12. In advanced JNA with intracranial extension, even after surgical resection, recurrence is high due to incomplete excision. Tyagi et al., in a review of 10 patients, reported residual disease in 80% patients after surgical excision with 30% subsequent recurrence 13. Fagan et al. reported 37.5% recurrence after surgical excision for JNA with intracranial extension 14. In the present series, 32.25% patients were deemed unresectable. The remaining 32.25% of patients underwent surgery but developed recurrence during follow-up. The remaining patients had R1 resection. This shows the difficulty of surgical excision in locally advanced JNA and therefore, the importance of adjuvant/salvage local therapy. Preoperative embolisation is generally undertaken 24-72 hours prior to resection and rationale is that occluding the responsible artery will decrease intraoperative bleeding and decrease the tumour size. Endoscopic resection may be associated with significantly lower intraoperative blood loss and lower recurrence rate compared to open resection 15.
The use of adjuvant/salvage/radical radiation has remained controversial owing to its anticipated long term morbidity and second primary neoplasm. In the last two decades the introduction of sophisticated radiation delivery technique has allowed investigators to use radiation and limit morbidity. In a review, Reddy et al. reported the efficacy of radiation in 10 patients with intracranial extension 10. A total of 30 Gy was delivered with customised field design with megavoltage X rays. After a median follow-up of 2.5 years, the authors reported 85% local control. The authors reported the occurrence of basal cell carcinoma in one patient 14 years after radiation. The authors concluded that a moderate dose of radiation can confer long term disease control for such cases. In our study, the local control rate was 90.3% at a median after a median follow-up of 12 months. Lee et al., in a retrospective review, analysed treatment outcomes of 27 patients treated with radiotherapy and reported 85% local control 8. In this study, the radiation dose ranged from 30-55 Gy. However, the radiation dose was restricted to 36-40 Gy for patients treated after 1999. The authors reported a 15% long term complication rate including cataract, hypopituitarism and temporal lobe necrosis (TLN) and growth retardation in one case each. However, the patient with TLN received a cumulative dose of 75 Gy over three years. In our study, no grade III or IV radiation-induced toxicity was noted.
Long term disease control has reached a new horizon, but the long term morbidity remains an area of concern (Table IV). The introduction of conformal radiotherapy has evolved as a promising treatment approach for locally advanced cohorts of JNA. Beriwal et al., in a report of two cases, showed the promising results in JNA treated with intensity modulated radiotherapy (IMRT) 9. Subsequently, two large series published by Chakraborty et al. and Kuppersmith et al. investigated the effectiveness of radiation when delivered with the conformal technique 16 17. Chakraborty et al., in a larger series of eight patients treated by conformal radiotherapy (7 planned with IMRT, one 3DCRT) reported progressive resolution in seven cases after a median follow-up of 17 months 16. The authors reported 87.5% actual control at two years with excellent sparing of organs at risk. Another series reported long term disease control in excess of 70-100%. Kuppersmith et al. reported on in a series of three patients treated with highly conformal IMRT aimed at limiting radiation doses to the optic nerves, optic chiasm, brainstem, brain, spinal cord, lens, retina, mandible and parotid 17. The dose delivered ranged from 34-45 Gy. The authors highlighted excellent sparing of critical normal organs as well as excellent disease control.
Table IV.
Summary of the published data of JNA treated with radiation.
| Author/Year | Number/Age | Stage IIIB | Dose (Gy) | Setting of RT | Result/Implication or late toxicity |
|---|---|---|---|---|---|
| Cummings et al., 1984 | 55 | 17 | 30-35 | Inoperable disease | LC 80%; 1 thyroid CA, 1 basal cell carcinoma 2 cataracts, Hypo-pituitarism |
| Robinson et al., 1989 | 10 | 30 | 30-40 | NA | 4-year LC of 100%, 1 -Cataract |
| McGahan et al., 1989 | 15 | 100 | 32-46 | Radical: 10 Salvage: 5 |
2-year LC of 73.33% Dose greater than 40 Gy allow improved LC |
| Fields et al., 1990 | 13 | 15 | 36.6-52 | Salvage RT | 11-year LC of 85%, xerostomia and caries |
| Reddy et al., 2001 | 15 | 67 | 30-35 | Inoperable disease | 5-year LC of 85% 3-cataracts, delayed transient CNS syndrome- 1 patient, a basal cell carcinoma of the skin - 1 |
| Lee et al., 2002 | 27. Mean 8 years (8-22) |
85 | 30-55 | Inoperable disease | 85, Long term complication 15% |
| Chakraborty et al., 2010 | 8 | 100 | 30-46 | Inoperable disease | 2-year LC of 87.5%; minimal acute and late side effects |
| Present series, 2014 | 31, Median age 16 (12-330) |
100 | 30-50 (median 32.5) |
Salvage:11 PORT (R1 resection): 10 Radical: 10 |
5-year PFS were 91.7%; SCC nasal ale-1 |
Reddy et al. reported on basal cell carcinoma in one patient 14 years after radiation 10. In our study, we also found one patient with squamous cell carcinoma (SCC) of the nasal ale. However, this patient was disease free after successful salvage surgery.
The major limitations of the present study are the retrospective nature of the analysis and short follow-up. However, we achieved good local control with very limited toxicity in these advanced cases of JNA.
Conclusions
Radiotherapy can be considered as a feasible option in stage III JNA with a local control rate of 90.3% at 1 year. The estimated 3- and 5-year median PFS were 91.7 and 70.7%, respectively. Moderate doses of radiation (30-45 Gy) delivered by the conformal technique can achieve durable disease control with limited morbidity.
References
- 1.Gullane PJ, Davidson J, O'Dwyer T, et al. Juvenile angiofibroma: a review of the literature and a case series report. Laryngoscope. 1992;102:928–933. doi: 10.1288/00005537-199208000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Wiatrak BJ, Koopman CF, Turrisi AT. Radiation therapy as an alternative to surgery in the management of intracranial juvenile nasopharyngeal angiofibroma. Int J Pediatr Otorhinolaryngol. 1993;28:51–56. doi: 10.1016/0165-5876(93)90146-t. [DOI] [PubMed] [Google Scholar]
- 3.Harwood AR, Cummings BJ, Fitzpatrick PJ. Radiotherapy for unusual tumors in the head and neck. J Otolaryngol. 1984;13:391–394. [PubMed] [Google Scholar]
- 4.Jafek BW, Krekorian EA, Kirsch WM, et al. Juvenile nasopharyngeal angiofibroma: management of intracranial extension. Head Neck Surg. 1979;2:119–128. doi: 10.1002/hed.2890020207. [DOI] [PubMed] [Google Scholar]
- 5.Leong SC. A systematic review of surgical outcomes for advanced juvenile nasopharyngeal angiofibroma with intracranial involvement. Laryngoscope. 2013;123:1125–1131. doi: 10.1002/lary.23760. [DOI] [PubMed] [Google Scholar]
- 6.Marshall AH, Bradley PJ. Management dilemmas in the treatment and follow-up of advanced juvenile nasopharyngeal angiofibroma. ORL J Otorhinolaryngol Relat Spec. 2006;68:273–278. doi: 10.1159/000093218. [DOI] [PubMed] [Google Scholar]
- 7.Moulin G, Chagnaud C, Gras R, et al. Juvenile nasopharyngeal angiofibroma: comparison of blood loss during removal in embolized group versus nonembolized group. Cardiovasc Intervent Radiol. 1995;18:158–161. doi: 10.1007/BF00204142. [DOI] [PubMed] [Google Scholar]
- 8.Lee JT, Chen P, Safa A, et al. The role of radiation in the treatment of advanced juvenile angiofibroma. Laryngoscope. 2002;112:1213–1220. doi: 10.1097/00005537-200207000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Beriwal S, Eidelman A, Micaily B. Three-dimensional conformal radiotherapy for treatment of extensive juvenile angiofibroma: Report on two cases. ORL J Otorhinolaryngol Relat Spec. 2003;65:238–241. doi: 10.1159/000073124. [DOI] [PubMed] [Google Scholar]
- 10.Reddy KA, Mendenhall WM, Amdur RJ, et al. Long-term results of radiation therapy for juvenile nasopharyngeal angiofibroma. Am J Otolaryngol. 2001;22:172–175. doi: 10.1053/ajot.2001.23458. [DOI] [PubMed] [Google Scholar]
- 11.Herman P, Lot G, Chapot R, et al. Long-term follow-up of juvenile nasopharyngeal angiofibromas: analysis of recurrences. Laryngoscope. 1999;109:140–147. doi: 10.1097/00005537-199901000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Patil RN, Agarwal AK, Prakash B, et al. Clinical records: extra-nasopharyngeal extensions of angiofibroma. J Laryngol Otol. 1982;96:1053–1064. doi: 10.1017/s002221510009349x. [DOI] [PubMed] [Google Scholar]
- 13.Tyagi I, Syal R, Goyal A. Staging and surgical approaches in large juvenile angiofibroma – study of 95 cases. Int J Pediatr Otorhinolaryngol. 2006;70:1619–1627. doi: 10.1016/j.ijporl.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Fagan JJ, Snyderman CH, Carrau RL, et al. Nasopharyngeal angiofibromas: Selecting a surgical approach. Head Neck. 1997;19:391–399. doi: 10.1002/(sici)1097-0347(199708)19:5<391::aid-hed5>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 15.Boghani Z, Husain Q, Vivek V, et al. Juvenile nasopharyngeal angiofibroma: a systematic review and comparison of endoscopic, endoscopic-assisted, and open resection in 1047 cases. Laryngoscope. 2013;123:859–869. doi: 10.1002/lary.23843. [DOI] [PubMed] [Google Scholar]
- 16.Chakraborty S, Ghoshal S, Patil VM, et al. Conformal radiotherapy in the treatment of advanced juvenile nasopharyngeal angiofibroma with intracranial extension: an institutional experience. Int J Radiat Oncol Biol Phys. 2011;80:1398–1404. doi: 10.1016/j.ijrobp.2010.04.048. [DOI] [PubMed] [Google Scholar]
- 17.Kuppersmith RB, Teh BS, Donovan DT, et al. The use of intensity modulated radiotherapy for the treatment of extensive and recurrent juvenile angiofibroma. Int J Pediatr Otorhinolaryngol. 2000;52:261–268. doi: 10.1016/s0165-5876(00)00297-4. [DOI] [PubMed] [Google Scholar]


