SUMMARY
Previous studies have suggested that risk factors for ischaemic vascular disease, such as cigarette smoking, hypertension and hyperlipidaemia, can also be considered risk factors for the development of idiopathic sudden sensorineural hearing loss (ISSNHL). In this study, we have evaluated the hypothesis that these factors can influence hearing threshold recovery in patients affected by ISSNHL. A total of 141 subjects who suffered an episode of ISSNHL were included. All subjects were assessed with tonal audiometry, auditory brainstem responses and MRI to exclude retrocochlear pathology. Hearing tests were conducted at ISSNHL onset (t = 0) and after 30 days. Patients were divided into three classes according to the presence/absence of one or more cardiovascular risk factors including: history of smoking, total serum cholesterol/triglycerides, history of hypertension and diabetes mellitus. Values of hearing threshold recovery were estimated and comparisons were conducted across the three risk factor classes. 75% of patients affected by ISSNHL showed a threshold recovery. However, the threshold recovery was found to be class-independent (average recovery value of 18 dB HL per classes) and also independent of age and gender. Even if cardiovascular risk factors have been found to be involved in the pathogenesis of ISSNHL, the present study suggests that these factors do not have any significant influence on the threshold recovery in ISSNHL.
KEY WORDS: Idiopathic sudden sensorineural hearing loss, Cardiovascular risk factors, Threshold recovery
RIASSUNTO
Diversi studi in letteratura hanno già suggerito che i fattori di rischio per la patologia ischemica vascolare, tra cui il fumo di sigaretta, l'ipertensione e l'iperlipidemia, sono anche fattori di rischio per lo sviluppo dell'ipoacusia improvvisa idiopatica (ISSNHL). In questo studio, abbiamo valutato l'ipotesi che questi fattori possano anche avere un ruolo nel recupero della soglia uditiva, in un gruppo di pazienti affetti da ISSNHL. 141 soggetti affetti da ISSNHL sono stati inclusi in questo studio. Tutti i pazienti sono stati valutati con audiometria tonale, potenziali evocati uditivi (ABR) e risonanza magnetica per escludere patologia retrococleare. L'audiometria tonale è stata eseguita all'esordio dell'ISSNHL e quindi dopo 30 giorni. I pazienti sono stati suddivisi in tre classi in base alla presenza/assenza di uno o più fattori di rischio cardiovascolare. I fattori di rischio cardiovascolare esaminati sono stati: storia di fumo, colesterolo totale e trigliceridi, ipertensione e diabete mellito. Il recupero di soglia uditiva è stata valutato e poi confrontato attraverso le tre classi dei fattori di rischio. Nelle tre diverse classi di rischio cardiovascolare, il 75% dei pazienti affetti da ISSNHL ha mostrato un recupero di soglia. Il recupero di soglia è risultato essere indipendente dalla classe di rischio di appartenenza (valore di recupero medio di 18 dB HL per classe) e anche indipendente da età e sesso. Anche se i fattori di rischio cardiovascolare sono risultati essere coinvolti nella patogenesi dell'ISSNHL, i dati del presente studio hanno mostrato che questi fattori non hanno però influenza significativa sul recupero soglia in un gruppo di soggetti affetti da ISSNHL.
Introduction
Idiopathic sudden sensorineural hearing loss (ISSNHL) is an acute inner ear disorder, mostly unilateral. It has been reported that ISSNHL has an overall incidence of 5-20 per 100,000 and that it is more frequent in western countries 1-7. The differential diagnosis for ISSNHL includes more than 100 potential aetiologies 1 3. Cases with a potentially discoverable aetiology fall into one of several categories including infectious, autoimmune, traumatic, vascular, neoplastic, metabolic and neurologic diseases. In a metaanalysis of 23 studies of ISSNHL, the most frequent causes were identified as infectious, vascular, haematologic, otologic, traumatic and neoplastic factors 1 3.
In support of the vascular occlusion thesis, impaired cochlear perfusion is the most widely reported hypothesis 7. The cochlea has a terminal capillary bed and is not supplied by collateral vessels that can restore blood flow in ischaemic regions. Moreover, since cochlear hair cells have a high metabolic activity, they are particularly vulnerable to hypoxic or ischaemic damage 7. A number of studies in the literature have found that risk factors for ischaemic vascular disease, including cigarette smoking, hypertension, and hyperlipidaemia, are also risk factors for the development of ISSNHL 8. Cochlear microvascular disorders can be related to increased plasma viscosity, to microembolic and/or thrombotic events 9.
In a previous publication 7, we studied the relation between the occurrence of ISSNHL and cardiovascular risk factors within this same group of subjects affected by ISSNHL; we have found a significant correlation between the risk of ISSNHL and diabetes when matching ISSNHL subjects with a group from the general population. However, we did not study the relationship between audiological features of ISSNHL and cardiovascular risk factors, which is the topic of this investigation. In this study, we analysed cardiovascular risk factors in a group of patients affected by ISSNHL; we then evaluated the hypothesis that these factors could influence hearing threshold recovery.
Materials and methods
This study analysed data retrospectively. A total of 141 subjects (75 M and 66 F), aged between 16 and 89 years (mean age 54 ± 15.8) who suffered an episode of ISSNHL were included in the analysis. Cases presenting other causes of hearing loss (either progressive or fluctuating) were excluded.
All patients were queried about medical history and were assessed by tonal audiometry and auditory brainstem responses (ABR). Medical resonance imaging (MRI) was used to exclude a retrocochlear pathology. Pure tone audiometry was performed within a sound-proof cabin (model E2X2, roll 01008 220V 10A; Mercury, Milan, Italy) using an Amplaid audiometer (Amplaid, Milan, Italy) calibrated to ISO 9001 standards. The audiometric procedure was performed using headphones to assess air conduction and a bone vibrator for bone conduction. The better ear was evaluated first. An ascending method using 5 dB steps was utilised to calculate hearing threshold. Air conduction hearing thresholds were assessed at 125, 250, 500, 1000, 2000, 4000 and 8000 Hz. Bone conduction hearing thresholds were assessed with the use of a masking, white, contralateral noise, at 250, 500, 1000, 2000 and 4000 Hz. Data on the ABR procedures are presented in the Appendix (section A1).
Hearing assessment was performed at the onset of ISSNHL (t = 0) and after 30 days (t = 30d). Each patient was classified into a hearing loss (HL) group, according to a pure tone average (PTA) value, estimated from hearing threshold levels at 0.5, 1, 2, 4 kHz. The HL groups were defined according to a modified method from Clark 10 as follows: normal hearing (-10-15 dB HL); slight hearing loss (16-25 dB HL); moderate hearing loss (26- 55 dB HL); severe hearing loss (56-90 dB HL); and profound hearing loss (> 90 dB HL).
All subjects were treated with: (i) betametasone 4 mg IM for 3 days and then betametasone 1.5 mg IM for 3 days with gastroprotection; and (ii) glycerol 10% in 250 ml per day for 5 days. Steroid therapy (either system or intratympanic) is considered the best treatment option for ISSNHL by the American Academy of Otolaryngology 11. Alternatively, osmotic diuretics have been also proposed for treatment of ISSNHL 12, but are not considered as standard therapy by the American Academy of Otolaryngology 11.
The cardiovascular risk factors considered in this study, included: (i) history of smoking; (ii) total serum cholesterol and triglycerides; (iii) history of hypertension and (iv) diabetes mellitus. Subjects with a history of diagnosed diabetes or who were receiving oral hypoglycaemic drugs or insulin, were defined as diabetic. For those who were not diagnosed with diabetes and who were not taking any antidiabetic medications, the value of fasting blood glucose was used to assess the presence of diabetes, according to American Diabetes Association guidelines (> 126 mg/dl) [Expert Committee on the Diagnosis and Classification of Diabetes Mellitus, 1997]. Patients with a history of diagnosed hypertension or who were taking medications for high blood pressure were considered as hypertensive. Total cholesterol and triglyceride values were determined using standardised commercial enzymatic tests after overnight fasting.
In order to assess the effects of cardiovascular risk factors on hearing threshold recovery, patients were divided into the following three classes according to the presence/ absence of one or more cardiovascular risk factors (i.e. smoking, hypertension, cholesterol, diabetes, previous ischaemia, triglycerides, LDL):
Risk class 1: subjects with no risk factors (no smoking history, cholesterol < 190 mg/dl, LDL < 120 mg/dl, TG < 180 mg/dl, no diabetes, no previous ischaemic episodes, regular blood pressure values).
Risk class 2: subjects with a single risk factor (cholesterol > 190 mg/dl, TG > 180 mg/dl, or smoking history, hypertension, diabetes).
Risk class 3: subjects with two or more risk factors (cholesterol > 190 mg/dl, TG > 180 mg/dl and/or smoking history, diabetes, hypertension).
The definition of "hearing recovery" criteria represents a critical problem that has been acknowledged in previous publications. Several criteria have been proposed in the literature, such as: (i) PTA improvement of 30 dB HL or 50% recovery 11; and (ii) a less conservative criterion of 10 dB HL PTA improvement 11. In this study, the threshold- recovery was calculated by PTA (t = 30d) – PTA (t = 0). This value was considered important if it was ≥ 10 dB HL.
Regarding the hearing threshold levels prior to the onset of ISSNHL, since an audiogram prior to the onset of ISSNHL was not available, the initial hearing level values refer to the un-affected ear. The decision to use these data was based on multiple observations from patients during the first audiometric evaluation. patients have stated that before the ISSNHL incident, they could not perceive hearing differences between the two ears. In this context, the degree of recovery was based on the hearing threshold values of the un-affected ear.
Auditory brainstem responses (ABR) procedure
Abrasive paste was used to clean the skin and electrodes were placed using an electrolytic paste and adhesive tape on the vertex and right and left mastoids. Stimuli were given monoaurally by an earphone and consisted of 0.1 ms clicks with alternating polarity starting at the maximum intensity of 90 dB nHL (120 dB SPL), starting from the better ear. Signals were differentially amplified (50000), filtered (5000–8000 Hz), and sent to a computer for analogue-todigital conversion, displaying and averaging. In presence of doubtful results two or more registrations were performed in order to obtain a well recognisable wave V, in order to exclude a retrocochlear pathology.
The clinical protocol for this study dictated that whenever the ABR traces were not reliable (i.e. no detectable responses), the patient should assessed with a cerebral MRI. As a safe guard and following the guidelines of the Academy of Otolaryngology-Head and Neck Surgery 11 all the patients participating in this study, underwent cerebral MRI to exclude retrocochlear pathology.
Statistical analysis
The characteristics of the sample were assessed using descriptive statistics by age, gender and degree of hearing loss with SPSS (version 16 for Windows). The presence of significant differences in hearing loss, or functional recovery, was investigated with the analysis of variance.
Moreover, a logistic regression model was used to assess the probability of threshold recovery, on the basis of the analysed variables and the presence of one or more cardiovascular risk factors.
Statistical significance was considered at p < 0.05.
Results
From the analysed variables (age, gender, PTA, threshold recovery), significant differences were observed only for age. Different patterns of threshold recovery were observed in the three risk-factor classes, but these differences were not statistically significant. The latter was also confirmed by a logistic regression model.
Descriptive statistics of the studied sample
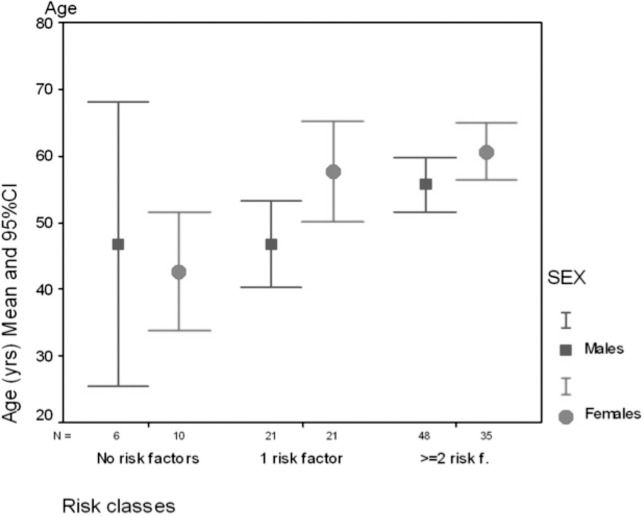
Figure 1 shows the distribution of age, gender and cardiovascular risk factors of the 141 patients. The data show a slight gender effect on age. The average age of female subjects was higher than it males and is affected by ISSNHL.
Fig. 1.
Distribution of cardiovascular risk factors by age and gender. There is a statistically significant difference between the average age of class 1 (no risk factors) and class 3 (two or more risk factors).
ANOVA analyses on age and cardiovascular risk factors show that there is a statistically significant difference between the average age of class 1 (no risk factors) and class 3 (two or more risk factors). The latter was significantly higher.
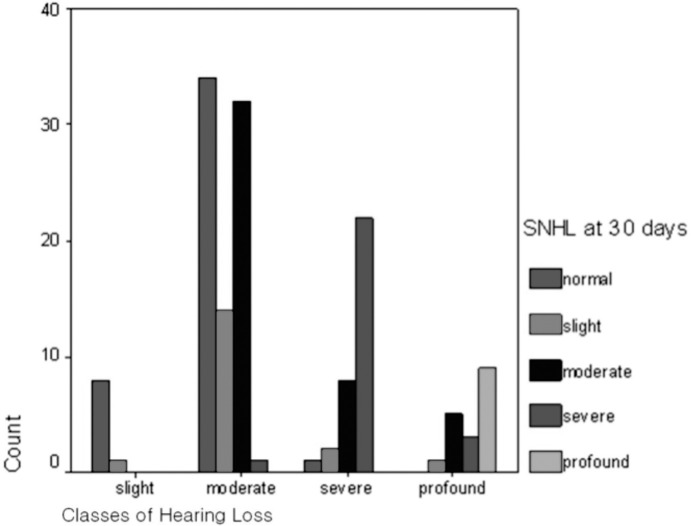
Figure 2A depicts the pure tone average values (1-4.0 kHz) at onset across the three risk classes. As expected, no significant differences were observed. Figure 2B expands the hearing loss data (at t = 0) in terms of slight, moderate, severe and profound losses.
Fig. 2.
A. PTA values (PTA = average of 0.5-4 kHz) for the three risk classes at onset (t = 0). B. Distribution of PTA values (PTA = average of 0.5-4 kHz) at t = 0 by risk-class and grade of hearing loss (slight, moderate, severe, profound).
Threshold recovery across risk classes
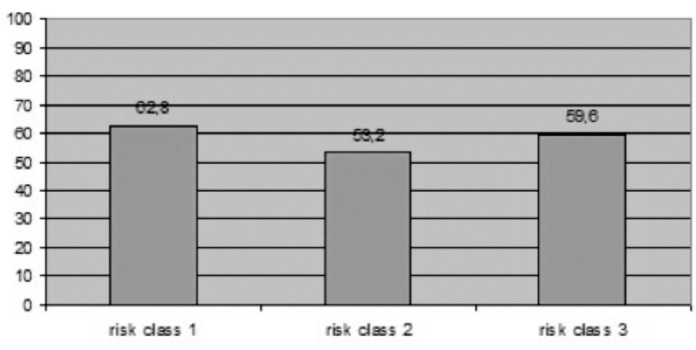
Figure 3 shows hearing loss distribution data at 30 days. For visual clarity, cases are classified according to the value of the threshold-recovery as worse, unchanged or better. Risk classes 2 and 3 show almost identical values in the "unchanged" and "better" groups.
Fig. 3.
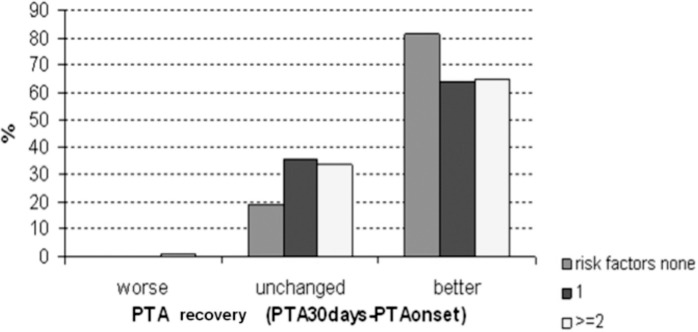
Percentage of PTA (PTA = average of 0.5-4 kHz) threshold recovery at 30 days across the three risk classes. The data are presented as cases with improved threshold (better); cases with no threshold improvement (unchanged); and cases presenting a threshold deterioration. The classification outcome for cases belonging to risk-classes 2 and 3 is very similar.
Considering all patients, there was threshold recovery in 75% of cases; in about the 20% of the patients, no PTA changes were observed across the 30 day period; there was only one case, in risk class 3, where the PTA showed deterioration. Analytically, in risk class 1 (no risk factors), 80% of subjects presented changes in their hearing threshold, while in risk classes 2 and 3 only 65% of patients presented PTA changes.
The estimated amount of threshold-recovery was very similar across the three risk classes, with average values of: 18.75 ± 16.9 (class 1), 18.9 ± 19.1 (class 2) and 18.85 ± 19.4 (class 3). No statistically significant differences were found across these three threshold recovery values.
Patterns of threshold recovery
The patterns of threshold recovery across the three riskclasses were different. In particular:
50% of subjects affected by profound ISSNHL (9 of 18), improved their hearing and moved to a lower threshold class (i.e. they moved from the profound to the severe or moderate hearing-loss group).
33.3% of those with severe ISSNHL at onset (11 of 33), moved to a moderate or a slight hearing-loss class.
59.3% of those with moderate ISSNHL at onset (48 of 81), improved their hearing and moved to a lower threshold class. The only outlier-value from this group originates from one subject classified in risk-class 3, who presented a threshold deterioration at the 30-day control.
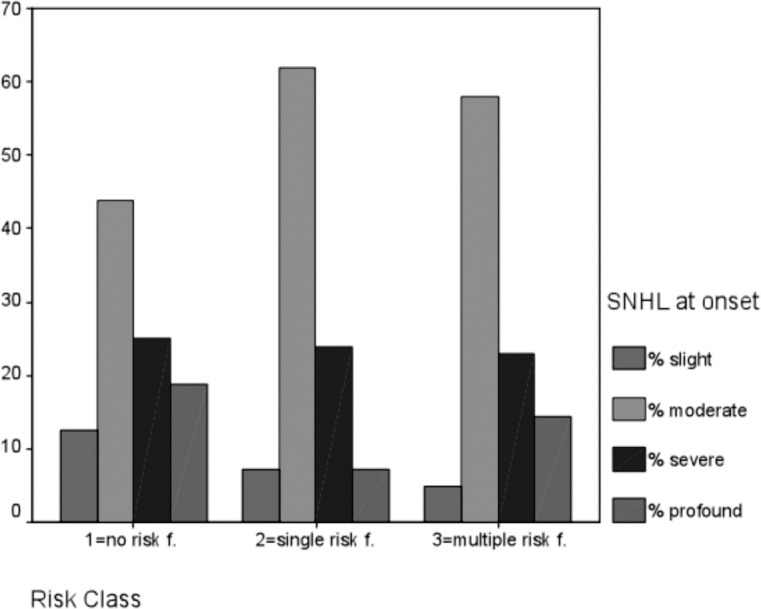
These observations suggest that "better recovery" is a function of the initial residual hearing capacity. In this context, it can be hypothesised that better-hearing ears recover more threshold, than the worse-hearing ears (assuming no-age effects). These findings are summarised in Figure 4 (distributional data) and Table I. The latter shows the data expressed in a cross-tabulation format, which facilitates the observation of distribution changes within each hearing loss category, at 30 days. Additional details on the crosstabulation are provided in the legend of Table I.
Fig. 4.
Distribution of the PTA (PTA = average of 0.5-4 kHz) threshold recovery at 30 days. The data suggest that better recovery is a function of the initial hearing-loss classification. In this context, it can be hypothesised that betterhearing ears recover more of the lost threshold than worse-hearing ears.
Table I.
Cross-tabulation of ISSNHL grade at onset (t = 0) and after 30 days. The table shows the overall classification changes over the observed 30-day period. The rows of the table provide information on the re-distribution of patients (slight, moderate, etc.). The columns show data on the composition of a certain group, that is where its members are coming from at 30 days.
For example, the distribution of the 33 severe cases at onset (group total under the "Total" right-hand column) changes at 30 days (read data from row 3 in the table) as follows; 1 case moves to the normal category; 2 cases move to the slight HL category; 8 cases move to the moderate HL category; and 22 cases remain in the severe category.
The 33 severe HL cases at t = 0 became 26 (see total under the "severe" column) at 30 days. This number is composed from contributions of the following groups: 1 case from the moderate group showed a threshold deterioration and was moved to the severe group; 22 cases from the severe group were classified into the same category; 3 cases from the profound group moved to the severe HL category.
| ISSNHL grade at 30 days: all subjects | |||||||
|---|---|---|---|---|---|---|---|
| Normal | Slight | Moderate | Severe | Profound | Total | ||
| ISSNHL grade at onset | Slight | 88.9% (8) | 11.1% (1) | – | – | – | 6.4% (9) |
| Moderate | 42.0% (34) | 17.3% (14) | 39.5% (32) | 1.2% (1) | – | 57.5% (81) | |
| Severe | 3.0% (1) | 6.1% (2) | 24.2% (8) | 66.7% (22) | – | 23.4% (33) | |
| Profound | – | 5.6% (1) | 27.8% (5) | 16.7% (3) | 50.0% (9) | 12.7% (18) | |
| Total ISSNHL at 30 days | 30.5% (43) | 12.8% (18) | 31.9% (45) | 18.4% (26) | 6.4% (9) | 100% (141) | |
The analysis of variance did not suggest any significant effects between the variables "threshold recovery" and "risk-class". Nevertheless, the behaviour of each riskclass in terms of threshold recovery was different. Analytical data are presented only for risk-classes 2 and 3, since the patients from risk-class 1 did not present any cardiovascular risk factors.
The data from risk-class 2 are summarised in Table II. The percentage of profound cases at t = 0 was 7.1% which decreased to 2.3% at t = 30d, due to reclassification of two subjects in the slight and moderate HL groups. The percentage of moderate and severe cases at t = 0, was 61.90% and 23.80%, respectively. At t = 30d, the percentages changed to 45.2% and 14.3% due to re-classification of subjects to the normal and slight hearing-loss categories. No cases with threshold deterioration were seen.
Table II.
Cross-tabulation of ISSNHL grade considering only the subjects in risk class 2.
| ISSNHL grade at 30 days: Class 2 only | |||||||
|---|---|---|---|---|---|---|---|
| Normal | Slight | Moderate | Severe | Profound | Total | ||
| ISSNHL grade at onset | Slight | 100.0%(3) | 0% (0) | – | – | – | 7.1% (3) |
| Moderate | 34.6%(9) | 11.5% (3) | 53.8% (14) | – | – | 61.9% (26) | |
| Severe | – | – | 40% (4) | 60% (6) | – | 23.9% (10) | |
| Profound | – | 33.3% (1) | 33.3% (1) | – | 33.3% (1) | 7.1% (3) | |
| Total ISSNHL at 30 days | 25.6%(12) | 9.5% (4) | 45.2% (19) | 14.3% (6) | 2.3% (1) | 100% (42) | |
The data from risk-class 3 are summarised in Table III. The percentage of profound cases at t = 0 was 14.4%, which decreased to 7.2% at t = 30d due to reclassification of four subjects in the moderate and 2 subjects in the severe HL groups. The percentage of moderate and severe cases at t = 0 was 57.9% and 22.9%, respectively. At t = 30d, these percentages changed to 28.9% and 20.5%. Interestingly, the only subject from the studied population who showed threshold deterioration at the 30-day control (from moderate to severe) belongs to this group.
Table III.
Cross-tabulation of ISSNHL grade considering only subjects in risk class 3.
| ISSNHL grade at 30 days: Class 3 only | |||||||
|---|---|---|---|---|---|---|---|
| Normal | Slight | Moderate | Severe | Profound | Total | ||
| SSNHL grade at onset | Slight | 100.0% (4) | 0% (0) | – | – | – | 4.8% (4) |
| Moderate | 45.8% (22) | 16.7% (8) | 35.4% (17) | 2.1% (1) | – | 57.9% (48) | |
| Severe | – | 10.5% (2) | 15.8% (3) | 73.7% (14) | – | 22.9% (19) | |
| Profound | – | – | 33.3% (4) | 16.7% (2) | 50.0% (6) | 14.4% (12) | |
| Total ISSNHL at 30 days | 31.3% (26) | 10% (10) | 28.9% (24) | 20.5% (17) | 7.2% (6) | 100% (83) | |
Discussion
The pathogenesis of ISSNHL is still unknown, even if viral infections and vascular occlusions are among the most common mechanisms advocated. Concerning the viral hypothesis, although some studies have been able to demonstrate viral infection in patients with ISSNHL, the specific and direct pathogenic role of viral infections in inner ear structural damage has not yet been definitively demonstrated 1 13. In support of the vascular occlusion thesis, impaired cochlear perfusion is the widely reported hypothesis although the location of the cochlea in the temporal bone makes the identification of a thrombotic occlusion difficult 1 14. Previous studies have evaluated the possible role of different cardiovascular and thrombophilic factors in the pathogenesis of ISSNHL 15-20. In a previous publication 7, we have studied the relation between the occurrence of ISSNHL and cardiovascular risk factors within this same group of subjects affected by ISSNHL; we found significant correlation between the risk of ISSNHL and diabetes when matching ISSNHL subjects with a group from the general population. However, we did not study the relationship between the audiological features of the ISSNHL subjects and cardiovascular risk factors.
If little is known about the pathogenetic mechanisms that cause ISSNHL, even less information is available on the biological mechanism of threshold recovery. It has been reported that threshold recovery in ISSNHL depends on many factors, including: (i) HL duration; (ii) associated HL symptoms; and (iii) audiogram characteristics. Generally, patients with higher hearing thresholds at the onset of ISSNHL recover less in comparison to patients with initial mild losses 1 21. The audiogram shape has also been shown to significantly impact hearing recovery. Data from the literature show that patients with low-frequency or mid-frequency hearing losses present higher rates of recovery in comparison to patients with flat or sloping-down audiometric profiles 1 22. Additional factors that contribute to better recovery post-ISSNHL, are: (i) younger age; (ii) male gender; (iii) less time elapsed between the onset of hearing loss and beginning of treatment; and (iv) upward-sloping audiogram shape 22.
Comorbid symptoms and signs have also been investigated as prognostic indicators for ISSNHL. In some studies, complaints of imbalance or vertigo have been associated with a poorer prognosis for hearing recovery following ISSNHL 1 23. This association was found to be non-significant in other studies 1 4-6. Tinnitus has been investigated as an ISSNHL indicator, but the available data are not conclusive 1. So far, no experimental data are available on the mechanisms underlying the physiopathological process of ISSNHL, its onset, the induced damage and possible recovery from ISSNHL. Thus, there are no means to predict the degree of hearing recovery following ISSNHL.
Conclusions
In conclusion, the data of the present study show that:
Subjects in risk class 3 have a higher average age than the other two groups;
Across all risk classes, 75% of patients affected by ISSNHL show recovery of hearing threshold;
The hearing threshold recovery has the same average value (18 dB HL) across the three risk classes and is independent of age, gender and cardiovascular risk class of origin. In this context, a subject belonging to riskgroup 3 (two or more risk factors) and to risk-group 2 (a single risk factor) has the same possibility to have hearing threshold recovery compared with those belonging to risk class 1 (subjects with no cardiovascular risk factors). This conclusion was also confirmed by the application of the logistic regression model.
The data from the two studies we have conducted (one on the occurrence of ISSNHL and cardiovascular risk factors 7 and this study on hearing recovery after ISSNHL and cardiovascular risk factors), suggest that cardiovascular risk factors are involved in the occurrence/pathogenesis of ISSNHL, but that these factors do not seem to have any significant influence on the biological mechanism responsible for threshold recovery in ISSNHL.
References
- 1.Zadeh MH, Storper IS, Spitzer JB. Diagnosis and treatment of sudden-onset sensorineural hearing loss: A study of 51 patients. Otolaryngol Head Neck Surg. 2003;128:92–98. doi: 10.1067/mhn.2003.50. [DOI] [PubMed] [Google Scholar]
- 2.Byl FM., Jr. Sudden hearing loss: Eight years' experience and suggested prognostic table. Laryngoscope. 1984;94(5 Pt1):647–661. [PubMed] [Google Scholar]
- 3.Chau JK, Lin JR, Atashband S, et al. Systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. Laryngoscope. 2010;120:1011–1021. doi: 10.1002/lary.20873. [DOI] [PubMed] [Google Scholar]
- 4.Fetterman BL, Saunder JE, Luxford WM. Prognosis and treatment of sudden sensorineural hearing loss. Am J Otol. 1996;17:529–536. [PubMed] [Google Scholar]
- 5.Nosrati-Zarenoe R, Arlinger S, Hultcrantz E. Idiopathic sudden sensorineural hearing loss: results drawn from the Swedish national database. Acta Otolaryngol. 2007;127:1168–1175. doi: 10.1080/00016480701242477. [DOI] [PubMed] [Google Scholar]
- 6.Nosrati-Zareno R, Hansson M, Hultcrantz E. Assessment of diagnostic approaches to idiopathic sudden sensorineural hearing loss and their influence on treatment and outcome. Acta Otolaryngol. 2010;130:384–391. doi: 10.1080/00016480903161541. [DOI] [PubMed] [Google Scholar]
- 7.Aimoni C, Bianchini C, Borin M, et al. Diabetes, cardiovascular risk factors and idiopathic sudden sensorineural hearing loss: a case-control study. Audiol Neurootol. 2010;15:111–115. doi: 10.1159/000231636. [DOI] [PubMed] [Google Scholar]
- 8.Capaccio P, Ottaviani F, Cuccarini V, et al. Genetic and acquired prothrombotic risk factors and sudden hearing loss. Laryngoscope. 2007;117:547–551. doi: 10.1097/MLG.0b013e31802f3c6a. [DOI] [PubMed] [Google Scholar]
- 9.Marcucci R, Alessandrello Liotta A, Cellai AP, et al. Cardiovascular and thrombophilic risk factors for idiopathic sudden sensorineural hearing loss. J Thromb Haemost. 2005;3:929–934. doi: 10.1111/j.1538-7836.2005.01310.x. [DOI] [PubMed] [Google Scholar]
- 10.Clark JG. Uses and abuses of hearing loss classification. Asha. 1981;23:493–500. [PubMed] [Google Scholar]
- 11.Stachler RJ, Chandrasekhar SS, Archer SM American Academy of Otolaryngology-Head and Neck Surgery, authro. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146(3 Suppl):S1–S35. doi: 10.1177/0194599812436449. [DOI] [PubMed] [Google Scholar]
- 12.Filipo R, Barbara M, Cordier A, et al. Osmotic drugs in the treatment of cochlear disorders: a clinical and experimental study. Acta Otolaryngol. 1997;117:229–231. doi: 10.3109/00016489709117777. [DOI] [PubMed] [Google Scholar]
- 13.Kuhn M, Heman-Ackah SE, Shaikh JA, et al. Sudden sensorineural hearing loss: a review of diagnosis, treatment, and prognosis. Trends Amplif. 2011;15:91–105. doi: 10.1177/1084713811408349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mattox DE, Lyles CA. Idiopathic sudden sensorineural hearing loss. Am J Otol. 1989;10:242–247. [PubMed] [Google Scholar]
- 15.Ciccone MM, Cortese F, Pinto M, et al. Endothelial function and cardiovascular risk in patients with idiopathic sudden sensorineural hearing loss. Atherosclerosis. 2012;225:511–516. doi: 10.1016/j.atherosclerosis.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 16.Ballesteros F, Tassies D, Reverter JC, et al. Idiopathic sudden sensorineural hearing loss: classic cardiovascular and new genetic risk factors. Audiol Neurootol. 2012;17:400–408. doi: 10.1159/000341989. [DOI] [PubMed] [Google Scholar]
- 17.Lin RJ, Krall R, Westerberg BD, et al. Systematic review and meta-analysis of the risk factors for sudden sensorineural hearing loss in adults. Laryngoscope. 2012;122:624–635. doi: 10.1002/lary.22480. [DOI] [PubMed] [Google Scholar]
- 18.Körpinar S, Alkan Z, Yiğit O, et al. Factors influencing the outcome of idiopathic sudden sensorineural hearing loss treated with hyperbaric oxygen therapy. Eur Arch Otorhinolaryngol. 2011;268:41–47. doi: 10.1007/s00405-010-1336-6. [DOI] [PubMed] [Google Scholar]
- 19.Mosnier I, Stepanian A, Baron G, et al. Cardiovascular and thromboembolic risk factors in idiopathic sudden sensorineural hearing loss: a case-control study. Audiol Neurootol. 2011;16:55–66. doi: 10.1159/000312640. [DOI] [PubMed] [Google Scholar]
- 20.Cadoni G, Scorpecci A, Cianfrone F, et al. Serum fatty acids and cardiovascular risk factors in sudden sensorineural hearing loss: a case-control study. Ann Otol Rhinol Laryngol. 2010;119:82–88. doi: 10.1177/000348941011900203. [DOI] [PubMed] [Google Scholar]
- 21.Xenellis J, Karapatsas I, Papadimitriou N, et al. Idiopathic sudden sensorineural hearing loss: Prognostic factors. J Laryngol Otol. 2006;120:718–724. doi: 10.1017/S0022215106002362. [DOI] [PubMed] [Google Scholar]
- 22.Chang NC, Ho KY, Kuo WR. Audiometric patterns and prognosis in sudden sensorineural hearing loss in Southern Taiwan. Otolaryngol Head Neck Surg. 2005;133:916–922. doi: 10.1016/j.otohns.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Ben-David J, Luntz M, Podoshin L, et al. Vertigo as a prognostic sign in sudden sensorineural hearing loss. International Tinnitus Journal. 2002;8:127–128. [PubMed] [Google Scholar]