SUMMARY
Acquired stenosis of the external auditory canal may be caused by a variety of insults, all sharing a common pathogenesis, namely a cascade of inflammatory changes leading to medial canal fibrosis. Previous surgery (canaloplasty or meatoplasty) and radiotherapy, especially if associated with a history of parotid surgery extended to the external auditory canal, have been implicated as possible causes. The literature offers advice on the management of stenosis consequent to otosurgery for congenital and acquired defects, but nothing on forms secondary to radiotherapy to the head and neck region. The proposed solutions are often cumbersome and difficult to fabricate, and therefore expensive. The aim of this paper, in which the cases of four patients are reported, is to present a new technique initially used for the most severe form – i.e. external auditory canal stenosis after surgery and radiotherapy – and then extended to forms due to different causes. This new technique involves the use of a series of surgical steel tubes of increasing dimension commonly used for tissue expansion in a body piercing practice called stretching and known as ear stretching tunnels or ear stretchers. This innovative approach proved effective in solving external auditory canal stenosis in our patients, with the least discomfort for the patient and the lowest cost. We consider this new solution to be feasible and practical and are convinced that it provides a new approach to an old problem. Further studies are needed to increase the number of clinical cases to verify how long the ear stretcher should be kept in place for the stenosis to stabilise, and to establish whether surgery is always necessary after ear stretcher application and, if so, the best timing for surgery.
KEY WORDS: External auditory canal stenosis, Ear-Stretcher, Parotid surgery, Radiotherapy
RIASSUNTO
La stenosi acquisita del condotto uditivo esterno (CUE) può essere causata da molti insulti con una patogenesi comune che è rappresentata da una cascata di alterazioni infiammatorie che portano alla fibrosi della porzione mediale del condotto. Un precedente intervento chirurgico, cioè canoloplastica o meatoplastica e la radioterapia (RT), soprattutto se associata con precedente chirurgia parotidea estesa al CUE, sono state messe in relazione a questo problema. In Letteratura abbiamo trovato consigli su come gestire le stenosi conseguenti a otochirurgia per difetti congeniti e acquisiti, ma nulla per quelle secondarie a radioterapia applicata al distretto testa e collo; le soluzioni proposte, spesso non sono maneggevoli e sono difficili da fabbricare, perciò sono costose. Il nostro obiettivo è quello di presentare, attraverso l'esposizione dei casi di quattro pazienti, un nuovo metodo utilizzato per la prima volta per la condizione peggiore, ovvero stenosi del condotto uditivo esterno dopo intervento chirurgico e radioterapia, e poi esteso anche alla stenosi di origine diversa. Questa nuova tecnica utilizza una serie di tubi di acciaio chirurgico di diametro crescente solitamente usati in una pratica di espansione cutanea del body piercing chiamata "stretching" e conosciuti come "ear stretching tunnels" o "ear stretchers". Questo approccio innovativo si è dimostrato efficace nel risolvere la stenosi del condotto uditivo esterno nei nostri pazienti, con il più basso costo e il minimo disagio per il paziente. Pensiamo che questa nuova soluzione sia pratica e dimostri come il contributo di tutti sia essenziale nella ricerca di nuovi approcci a vecchi problemi. Ulteriori studi sono necessari per aumentare il numero di casi clinici, per verificare quanto tempo lo "stretcher" debba essere mantenuto in sede ovvero in quanto tempo la stenosi si stabilizza, in modo da definire se l'intervento sia sempre necessario dopo l'applicazione dello "stretcher" e quale sia il momento giusto per effettuarlo.
Introduction
Stenosis of the external auditory canal (EAC) can be congenital, due to abnormalities of the first gill cleft, or acquired as a result of inflammation, trauma and the effects of radiotherapy (RT), all sharing a common pathogenesis, namely a cascade of inflammatory changes leading to medial canal fibrosis 1. Inflammatory causes of EAC stenosis are chronic and relapsing otitis externa, perichondritis and periostitis. EAC tumours can cause EAC stenosis and their excision can lead to postoperative restenosis (traumatic cause). RT for the treatment of head and neck cancers including those affecting the temporal bone area can induce pathological changes in the EAC that can be divided into: bony changes (resorption, fibrosis, empty lacunae, sequestration) and soft tissue changes (ulceration of the epithelial lining, thickening of the epithelium in the canal and in the tympanic membrane, subepithelial fibrosis, atrophy of ceruminous glands) 2. These changes may appear clinically as a persistent otitis externa, with otorrhoea and otalgia, resulting in EAC stenosis that prevents adequate examination and cleaning of the ear and is associated with hearing loss. RT, especially if associated with previous parotid surgery, has been related to EAC stenosis 3.
Different stenting materials have been successfully used to prevent early, but not delayed, EAC stenosis, including absorbable gelatine sponge (Gelfoam®), backing strips and expandable wicks. Postoperative care is not, however, commonly discussed in the literature. After removal of the packing material about 1 week postoperatively, if the canal is oedematous, it may be necessary to place a Pope wick; in addition, ototopical antibiotic/steroid drops may help to prevent early restenosis 1. Postoperative EAC restenosis is the most common complication after surgery on the EAC. The use of stents can provide a solution to this problem.
Table I.
Hearing outcomes are presented as the mean of threshold by air conduction (TAC) and threshold by bone conduction (TBC) before and after insertion of the stretcher. ABG pre and post indicate the air-bone gap before and after insertion of the stretcher, respectively; Δ ABG indicates the difference between air-bone gaps before and after insertion of the stretcher.
| Patient n | TAC pre | TBC pre | TAC post | TBC post | ABG pre | ABG post | Δ ABC |
|---|---|---|---|---|---|---|---|
| 1 | 23.8 | 16 | 19.6 | 16 | 7.8 | 3.6 | 4.2 |
| 2 | 87.9 | 49 | 69.2 | 49 | 38.9 | 20.2 | 18.7 |
| 3 | 89.6 | 46.5 | 75 | 46.5 | 43.1 | 28.5 | 14.6 |
| 4 | 71.7 | 57 | 60.8 | 57 | 14.7 | 3.8 | 10.9 |
Materials and methods
Technique
Our approach was to use a surgical steel tube that allowed progressive expansion of the stenotic EAC using devices of increasing dimension called ear stretching tunnels or ear stretchers. These are surgical steel tissue expanders (Fig. 1) commonly used in a body piercing practice called stretching and involving the progressive and gradual expansion of a skin area; this process can be applied to every piercing site, but the earlobe is the most frequently involved. Dilatation of the piercing hole is obtained gradually, usually 1 mm per month for the earlobe, by pushing a taper (conical rod) as far as it will go through the piercing hole and replacing it with a stretching tunnel of the appropriate size to be worn between stretches. The history of earlobe stretching is very old: it is a ritual that has been practised by indigenous peoples all over the world since ancient times. Tribes in various countries (Africa, Eurasia, America) have practised this ritual for cultural, religious and traditional aesthetic purposes. Bone, horn, wood and stone were generally carved for earlobe stretching. King Tutankhamen is one of the earliest individuals known to have stretched earlobes. Although ear stretchers are commercially available in different materials (surgical steel, nickel-free titanium and glass), we decided to test only surgical steel stretchers to keep our clinical records uniform.
Fig. 1.

Commercially-available ear stretching kit including surgical steel tapers and tunnels of increasing gauges.
Case 1
In July 2012, a 47-year-old Caucasian man was referred to our ENT Department by his general practitioner because of a sudden increase in volume of a lateral neck mass, which had developed three months earlier. The mass was painless, located behind the right rising branch of the jaw, 30-40 mm in size, with a parenchymatous texture, fixed to deep tissues and covered by normal skin. Fine-needle aspiration biopsy (FNAB) of the mass was positive for squamous cell carcinoma. The patient underwent further investigations consisting of panendoscopy of the upper aerodigestive tract, computed tomography (CT) and magnetic resonance imaging (MRI) of the head, neck and chest, total body positron emission tomography (PET)-CT, and electroneurography (ENG) of the facial nerve. Clinical-radiological staging was right parotid carcinoma with EAC erosion and dermal infiltration. Therefore, a right radical parotidectomy and ipsilateral modified radical neck dissection type III (levels II-IV) were carried out. The tumour was leaning against the EAC, adherent to the cortical mastoid and the bony part of the EAC. These structures were drilled for oncological eradication. Part of the concha, cartilaginous EAC and skin were removed, and the deficiency of the submeatus region was filled with a temporo-occipital flap. Gelfoam® was used to protect the tympanic membrane (TM), and a silastic foil was fashioned containing a haemostatic plug (Pope wick) to maintain the patency of the new and shorter EAC. The patient had a regular postoperative course except for the onset of delayed facial nerve palsy. The final histological examination was undifferentiated adenocarcinoma of the parotid gland with squamous aspects and neoplastic neurotropism, pT3 N0 R0 M0 G3. Adjuvant radiation therapy, 60 Gy in 30 days, was planned. The patient began RT during which he developed an EAC stenosis due to hypodermic oedema. The stenosis grew so tight that it precluded retention of the Pope wick. Two weeks after the end of RT the EAC diameter was 2 mm (Fig. 2A). Corpuscular serum otorrhoea, eczema and subcontinuous fullness were associated with the EAC stenosis. The TM was no longer visible. Initially, a 2-mm stiff perforated silicon tube was placed, but it was expelled every 4-6 days. Thereafter, a 2.5-mm surgical steel ear stretching tube was used. This second device was retained in the stenotic EAC for one month, after which it was replaced with a 3.2-mm tube for 3 months, and then with a 4-mm tube that is still in place (Fig. 2B).
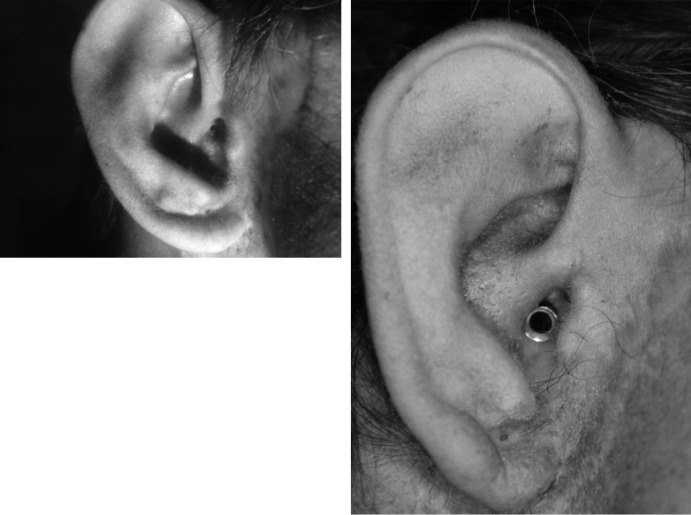
Fig. 2.
A: External auditory canal (EAC) diameter two weeks after the end of RT (2 mm), the tympanic membrane is not visible; B: 4-mm stretcher placed in the right EAC: it can be seen that it is self-retaining and aesthetically pleasing as it does not protrude from the EAC.
The patient does not come to our clinic for medications because he is able to manage them autonomously, and only comes for his monthly follow-up appointments. Thanks to the ear stretcher, he no longer complains of otorrhoea, fullness, or hearing deficit; cultural buffers are negative for infection, and half of the TM is again visible (Fig. 3). His last follow-up visit was in May 2014, for an overall follow-up period of 21 months. One year has passed since the ear stretcher was positioned, and we think it should be kept in place for at least one year after the end of RT. We decided against an early surgical approach due to the risk of relapse and the expected local effects of RT that could influence surgical outcome. Surgical correction of the stenosis could be proposed 2 years after the first operation.
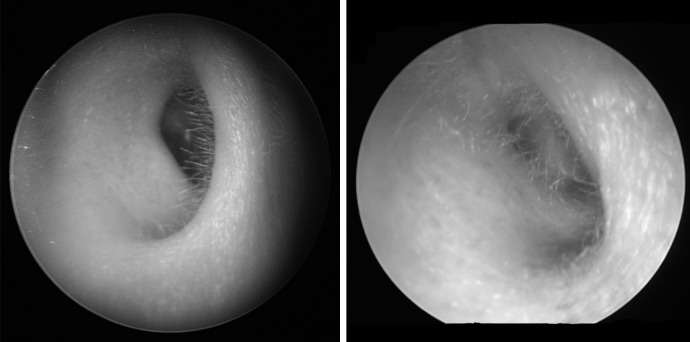
Fig. 3.
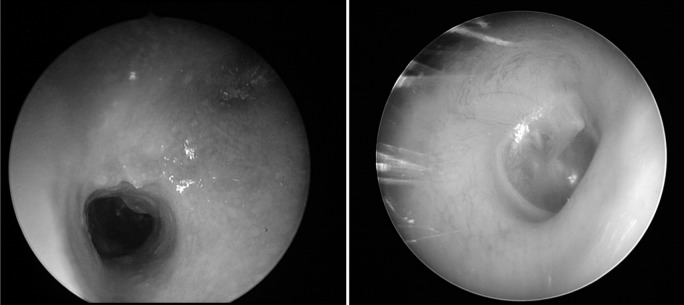
A: EAC stenosis after removal of the stretcher; B: beyond the remaining stenosis the ear is clean and the tympanic membrane is visible again.
Encouraged by this good result, we decided to extend the use of this new device in different situations.
Case 2
The second patient who was treated with an ear stretcher was a 90-year-old man who underwent surgery in August 2013 for a squamous cell carcinoma of the ear infiltrating the skin and the external part of the parotid gland. A subtotal amputation of the ear was performed, maintaining only the bony portion of the EAC with its skeletonisation up to the TM. Adjuvant RT was excluded because of the patient's general condition. To avoid local complications, in the operating room we covered the residual bony canal with a temporal muscle flap over which we positioned a silastic foil with a Pope wick inside. Finally, the skin defect was closed directly. One week after surgery we inserted an ear stretching tunnel into the EAC which had already started to narrow in the sutured skin area, reaching a diameter of 3.2 mm. EAC patency was checked during the monthly oncological follow-up visits, the last of which took place in January 2014 since the patient died in February 2014; during that visit the diameter was 4 mm.
Case 3
The third patient was a 60-year-old woman with an EAC stenosis (3.5 mm in diameter) consequent to frequent otitis externa (Fig. 4A). During October 2013 she underwent canaloplasty with removal of the scar tissue, underlying epithelium and the epithelial part of the TM. The preoperative CT scan demonstrated the absence of chronic otitis or middle ear illness, undamaged ossicular chain, normal ventilation of the mastoid and normal appearance of the scutum so that only exploratory myringotomy was sufficient. Bone drilling was not required because the bony part of the EAC was not stenotic. Tiersch fragments taken from the supraclavicular area were used to cover the bone. Gelfoam® was positioned over the TM, and silastic foil with a Pope wick was placed inside the EAC. One week later an ear stretcher of 4 mm was inserted to avoid narrowing. Her follow-up visits are scheduled every 3 months, and on her last visit in May 2014 the EAC appeared patent (Fig. 4B).
Fig. 4.
A: EAC before the insertion of the stretcher, it appears narrowed and the TM is difficult to visualise; B: EAC after the use of stretcher, the diameter is larger and the TM is simpler to visualise.
Case 4
The fourth patient we treated was a 90-year-old man with a squamous cell carcinoma of the concha. In November 2013, after amputation of the concha and antitragus with superficial parotidectomy and selective lateral neck dissection, the defect was rebuilt by transposition of a muscular- skin island flap based on the retroauricular muscle; an advancement flap was used for the skin defect of the mastoid region. Histological examination was pT1N0. To avoid stenosis of the distal tract of the cartilaginous canal, we adopted the same procedure as used in the other three cases, starting with a 2.5-mm diameter ear stretcher progressively replaced with larger stretchers. During monthly oncological follow-up examinations, the last of which took place in May 2014, the EAC did not appear to be narrowing; the stretcher now in place is 4 mm in diameter.
Discussion
A brief review of the literature revealed the lack of innovative solutions for the management of EAC stenosis. Furthermore, we found no advice on the treatment of post-RT EAC stenosis, but only on the management of post-surgical stenosis. As reported by Carls et al., we observed that the combination of high-dose radiation and previous parotid surgery is related to the risk of EAC stenosis (p = 0.0059), with a higher incidence during the earliest period after RT 3.
Paparella and Kurkjian introduced the basic surgical principles of excising the fibrous plug, enlarging the cartilaginous and bony canal, and then re-covering it. Since then, modifications of this technique have been introduced primarily to address the most common postoperative complication, i.e. restenosis 4.
The use of soft stents with injection of triamcinolone may be advantageous in the meatus that is beginning to stenose. Several splints and expanding techniques have been described; some of the problems encountered include availability of the materials, costs, expertise in fabrication and patient compliance.
A case report by Miller described the use of an expanding cellulose wick for EAC narrowing, changed monthly for 4 months. Otologic drops of a mixture of steroids were used to reduce scar formation. One year later the EAC size was normal 5. A Foley catheter was used to maintain the patency of the EAC after resection of a preauricular squamous carcinoma and after ear reconstruction in microtia 6. A North American group presented 6 cases of patients treated with medium-density viscosity dental impression material as an initial support device after surgery, followed by a hard, acrylic, removable stent to be worn for the following few months to maintain patency and prevent restenosis 7. The Jerusalem Hospital group described meatal stenosis after mastoidectomy in 3 patients; to prevent it, they inserted an Optosil® template after surgery, which was left in place for the first postoperative week, and then replaced with an acrylic stent worn during most of the day for a period of 6 months, until epithelisation occurred around it 8. Savion et al. produced an acrylic resin conformer to solve a stenosis of the cartilaginous part of the EAC, with the possibility to gradually dilate it by using progressively larger speculi 9.
Our approach was to use a surgical steel tube that allowed progressive expansion of the stenotic EAC, by using devices of increasing dimension called ear stretching tunnels or ear stretchers. The idea was borrowed from the world of tattoos and body piercing, since these are surgical steel tissue expanders (Fig. 1) commonly used in a body piercing practice called stretching and involving the progressive and gradual expansion of a skin area, for example the earlobe. Dilatation of the piercing hole is obtained gradually (usually 1 mm per month) by pushing a taper as far as it will go through the piercing hole and then replacing it with a stretching tunnel of the appropriate size to be worn between stretches.
Although ear stretchers are commercially available in different materials (surgical steel, nickel-free titanium and glass), we decided to test only surgical steel stretchers to ensure that our clinical records were uniform.
In our experience, despite the limited number of patients treated, the use of an ear stretcher made it possible to preserve ventilation of the EAC, resulting in auditory improvement, reduced otorrhoea and secretion stasis, and thus preventing local infection. Because the principal morbidity of the EAC stenosis is hearing loss, we decided to objectively assess the efficacy of the new proposed treatment by comparing the auditory examinations before and after the insertion of the stretcher. The hearing outcomes were evaluated using the criteria stated by the Committee on Hearing and Equilibrium Guidelines 10, and closure of the air-bone gap was considered. In all 4 patients we obtained closure of the air-bone gap.
In our cases, the aetiology of EAC stenosis was different: consequent to repeated inflammation, to surgery alone or to a combination of surgery and RT. The use of an ear stretcher can be helpful in patients who have developed EAC stenosis as a consequence of surgery, because a second operation to resolve the condition after canaloplasty or meatoplasty could in itself lead to a worsening of the stenosis.
The possible disadvantages of the use of an ear stretcher include the following:
it is not an approved medical device, so patients would have to buy it themselves;
it may cause minimal discomfort at night because it is rigid and the tragus presses against it;
its small size could make it difficult to handle for an elderly patient, but the device can easily be managed by the patient's caregivers;
in the case of RT, the expected results are inferior since RT worsens EAC stenosis; however, we think this problem is common to all of the previously used devices.
In our opinion, the advantages of the ear stretcher, also in comparison with other stenting devices, are as follows:
it is made of surgical steel and therefore it is nickel-free and cannot cause allergic reactions;
it is non-degradable because of the prevalence of chrome which has antioxidant and noncorrosive properties so that the patient can also wear it while bathing;
compared to the Foley catheter, it is safer as it is not porous and micro-organisms are less likely to colonize its surface; it is easily sterilisable; it is hard and incompressible, ensuring constant patency of the duct; it is aesthetically pleasing because it does not protrude from the EAC and it is self-retaining, while the Foley catheter is larger and needs to be fixed all around the auricle. This feature ensures good patient compliance;
it is a cost-saving method that cuts direct and indirect costs. Ear stretchers are on sale at any tattoo shop and are very cheap; they come in different shapes and sizes so they do not need to be produced ex-novo and are readily adaptable to every EAC. Ear stretchers are handy and practical, and positioned within minutes in expert hands, so that outpatient follow-up visits are shorter; once inserted, they remain in place so that close follow-up is not necessary. Patients can individually clean the ear stretcher by removing it when it is obstructed by horny scales and sterilising it by boiling. For this reason, this method is also time saving (indirect costs).
the use of an ear stretcher is compatible with patients' personal hobbies and we think it is important not to alter patients' quality of life.
In conclusion, maintaining EAC patency is a basic component of the postoperative management of patients with EAC stenosis consequent to surgery with or without RT who are awaiting reconstructive surgery after local stabilisation. Our experience, albeit based on only 4 patients with a limited follow-up period, suggests that the surgical steel ear stretcher borrowed from body piercing practice can be successfully used to expand stenoses due to different causes.
Acknowledgements
The authors thank Itala Mary Ann Brancaleone, MA, RSA Dip TEFLA, teacher of Medical English at the University of Trieste, for her support in editing the manuscript.
References
- 1.Luong A, Roland PS. Acquired external auditory canal stenosis: assessment and management. Curr Opin Otolaryngol Head Neck Surg. 2005;13:273–276. doi: 10.1097/01.moo.0000172821.04946.30. [DOI] [PubMed] [Google Scholar]
- 2.Adler M, Hawke M, Berger G, et al. Radiation effects on the external auditory canal. J Otolaryngol. 1985;14:226–232. [PubMed] [Google Scholar]
- 3.Carls JL, Mendenhall WM, Morris CG, et al. External auditory canal stenosis after radiation therapy. Laryngoscope. 2002;112:1975–1978. doi: 10.1097/00005537-200211000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Paparella MM, Kurkjian JM. Surgical treatment for chronic stenosing external otitis. Laryngoscope. 1966;56:232–245. doi: 10.1288/00005537-196602000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Miller GW. Treatment of acute ear canal stenosis with an expanding cellulose wick. Arch Otolaryngol. 1978;104:55–56. doi: 10.1001/archotol.1978.00790010059013. [DOI] [PubMed] [Google Scholar]
- 6.Karanth SK, Mokai NJ. Silicone Foley's catheter: a useful splint in ear surgery. Indian J Plast Surg. 2008;41:51–54. doi: 10.4103/0970-0358.41111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weber PC, Davis B, Adkins WY., Jr Canal atresia reconstruction with dental impression material. Am J Otolaryngol. 1999;20:236–240. doi: 10.1016/s0196-0709(99)90006-6. [DOI] [PubMed] [Google Scholar]
- 8.Hocwald E, Sichel JI, Sela M, et al. Prevention of post-mastoidectomy meatal stenosis by an acrylic prosthesis. Laryngoscope. 2002;112:1892–1894. doi: 10.1097/00005537-200210000-00036. [DOI] [PubMed] [Google Scholar]
- 9.Savion I, Good J, Sharon-Buller A. An acrylic resin conformer for the prevention of external auditory meatus stenosis. Laryngoscope. 2005;115:2006–2009. doi: 10.1097/01.mlg.0000180175.81906.5e. [DOI] [PubMed] [Google Scholar]
- 10.Monsell EM. New and revised reporting guidelines from the Committee on Hearing and Equilibrium. American Academy of Otolaryngology Head and Neck surgery Foundation, Inc. Otolaryngol-Head Neck Surg. 1995;113:176–178. doi: 10.1016/S0194-5998(95)70100-1. [DOI] [PubMed] [Google Scholar]