Abstract
Pain can have negative effects leading to prolonged hospital stays. Determining the presence of uncontrolled and untreated pain in patients with cognitive impairments such as delirium, dementia, and delirium superimposed on dementia (DSD) is challenging. One tool commonly suggested for use in assessment of pain in older adults with cognitive impairment is the Pain Assessment In Advanced Dementia (PAINAD) scale. Proper use of the PAINAD scale as part of a comprehensive pain management plan can help reduce the likelihood of a patient experiencing unrecognized and untreated pain. Using an individual example, this article illustrates best practices in pain assessment and management for a woman experiencing DSD during an acute hospitalization.
Mrs. V. is a 94-year-old woman who sustained a fall with a right hip fracture at home. Her medical history includes hypertension, left knee arthroplasty, arthritis, osteoporosis, and tonsillectomy. Her family has stated that lately she has been forgetting things, such as birthday cards, the mail, eating meals, and various other activities that are part of her normal routine. They mentioned that the possibility of dementia was discussed during a previous hospitalization.
Upon admission to the hospital, Mrs. V. verbally rates her pain a 10 of 10, and she is moaning and yelling out. She is given 4 mg of morphine intravenously in the emergency department and is prepared for surgery that morning. Following surgery with general anesthesia, she is admitted to an acute care of the elderly (ACE) unit. Upon awakening from surgery, she states her pain is 8 of 10 on a 0 to 10 verbal pain intensity scale. Mrs. V. is started on a regimen of alternating as-needed oral and intravenous pain medications.
As the night progresses, Mrs. V. becomes very agitated. Mrs. V.’s daughter states, “This is not my mother; she never acts like this.” Upon hearing this information, the nurses on the ACE unit assess Mrs. V. and become concerned about the possibility of delirium superimposed on dementia (DSD). Notably, several factors could be contributing to signs of delirium including general anesthesia, postoperative pain, pain medications, altered serum laboratory values, and environmental changes. By now, Mrs. V.’s pain has not been addressed for 6 hours. When asked about her pain, Mrs. V. says, “Get away from me; it is none of your business.” The nurses observe that Mrs. V. is grimacing with movement, striking out, and her emotional state fluctuates by the minute. However, the nurses are able to console her for several minutes at a time. Her vital signs reveal tachycardia, hypertension, and tachypnea. Mrs. V. is started on a pain regimen of scheduled hydrocodone (Vicodin®) 5 mg every 8 hours. Mrs. V. became oriented, cooperative, and attentive by morning.
BACKGROUND
Chronic pain affects more than 30% of older adults living in the community (Reyes-Gibby, Aday, & Cleeland, 2002), and among approximately 50% of adults who are admitted to the hospital in pain, 19% report that pain is moderate or extremely severe (Desbiens et al., 1996). Two biological changes associated with aging may play a role in the undertreatment and underreporting of pain in older adults. First, as people age, pathophysiological changes occur in the pain fiber systems. Age-associated decreases in pain fibers may lead to elevated sensory thresholds and decreased affective reports of pain (Gøransson, Mellgren, Lindal, & Omdal, 2004). Second, as people age, the prevalence of cognitive impairment increases. Among older adults who are 65 and older, approximately 11% have Alzheimer’s disease (AD) and among those ages 85 and older, 32% have AD (Alzheimer’s Association, 2013).
A frequent form of cognitive impairment among hospitalized older adults is delirium. The prevalence of delirium is 50% in the general hospital setting (Inouye et al., 1999) and may increase to 80% in critical care (Inouye, 2006). Determining the presence of delirium can be difficult because delirium can present in several ways such as hyperactive, hypoactive, or mixed. Patients typically display inattention, exhibit disorganized thinking, or experience disturbance in the sleep-wake cycle (Burns, Gallagley, & Byrne, 2004). Unfortunately, cognitive syndromes such as delirium or dementia generally do not develop singularly. Delirium affects approximately 50% of hospitalized patients with dementia (Fick, Kolanowski, Waller, & Inouye, 2005) and leads to a condition termed delirium superimposed on dementia (DSD). Adverse events are associated with DSD, including accelerated decline in cognitive functional abilities, greater need for institutionalization, rehospitalization, and increased mortality (Fick, Agostini, & Inouye, 2002). Determining baseline cognitive status in someone with possible DSD is critical in establishing a formal diagnosis (Fick, Steis, Mion, & Walls, 2011) (Table 1).
TABLE 1. DELIRIUM ASSESSMENT IN THE PRESENCE OF DEMENTIA.
| Delirium Indicatorsa |
Description of Delirium Indicator |
Method of Assessment for Delirium Indicator |
Notes Regarding Dementia Versus Delirium |
|---|---|---|---|
| Acute onset | Delirium symptoms develop in hours or days |
Ask caregiver: Before this event/illness, what was the patient’s behavior usu- ally like? Focus on the individual’s ability to perform activities of daily living (ADLs) and instrumental ADLs (e.g., using the telephone, managing bank account). |
Changes in dementia are slow, occurring over months to years. |
| Fluctuating course | Symptoms wax/wane over 24-hour period |
Assess: Does lethargy/restlessness alternate over several hours? Are there periods of lucidness with confusion? |
In dementia, some behaviors may fluctuate, but thinking and memory change slowly over time. |
| Inattention | Difficulty focusing | Assess: Does the patient focus attention on you when you are speaking? Is there eye contact? Do you need to repeat your question/directions? Ask the patient to state the days of the week backward. |
In dementia, individuals are able to focus on speaker until advanced stages. |
| Disorganized thinking |
Rambling, nonsense speech | Assess: Does the patient make sense when responding to you? Ask patient: “What would you do if you found a stamped envelope on the sidewalk?” “What would you do if your home was on fire?” |
In early stages of dementia, in- dividuals are able to make sense when responding. |
| Altered level of alertness |
Can be hypo- or hyper-alert | Assess: Is lethargy or somnolence (hypo-alert) or restless, agitated (hyper-alert) behavior different from baseline? |
Level of alertness is not altered in dementia. |
Delirium is marked by acute onset, fluctuating course, inattention, and either (a) disorganized thinking or (b) altered level of alertness. Visual and/or auditory hallucinations may be present. Baseline should be established by the primary caregiver.
PAIN AND COGNITIVE IMPAIRMENT
Pain in older adults with dementia, delirium, or DSD can develop from various sources. Regardless of whether pain is acute or chronic, untreated pain can lead to negative outcomes, such as sleep disturbances, impaired ambulation, depression, refusal of care, worsening cognitive impairment, and agitation (American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons, 2009). Overall, untreated pain leads to increased suffering and a diminished quality of life (Husebo et al., 2008). When compared to people without a dementia diagnosis, and despite evidence that older adults with mild and moderate dementia can reliably report severe pain, individuals with dementia receive fewer orders for opioid pain medications (Monroe, Carter, Feldt, Dietric, & Cowan, 2013). Additionally, individuals with worsening cognitive impairment consistently receive less pain medication in the presence of conditions known to be painful in people who are cognitively intact (Monroe & Carter, 2010; Monroe et al., 2013; Morrison et al., 2003).
Untreated pain can be a risk factor for developing delirium, and the ability to remain attentive can diminish as pain level increases (Crombez, Eccleston, Baeyens, & Eelen, 1998; Eccleston & Crombez, 1999). For example, suboptimal postoperative pain management has been associated with increased risk for developing delirium and prolonged hospital stays (Schreier, 2010; Vaurio, Sands, Wang, Mullen, & Leung, 2006). Conversely, appropriately treated pain is associated with a decreased risk for or delayed development of delirium. When compared to hospitalized older adults who received little or no opioid medication and developed moderate to severe delirium, those who received opioid pain treatment developed only mild delirium (Robinson, Rich, Weitzel, Vollmer, & Eden, 2008), demonstrating that appropriately used opioid or non-narcotic medications may reduce, diminish, or resolve delirium.
PAIN ASSESSMENT IN ADULTS WITH LIMITED ABILITY TO COMMUNICATE
Regardless of cognitive status, it is important to provide a systematic, consistent method when assessing pain to ensure adequate pain management. A Hierarchy of Pain Assessment Techniques has been recommended to provide a structure in assessing and treating pain (Elliott & Horgas, 2009; Mentes, Teer, & Cadogan, 2004; Pasero & McCaffery, 2000). The Hierarchy of Pain Assessment Techniques includes:
First, attempt to promote a self-report of pain from the patient.
Identify any conditions or procedures that may cause pain.
Use a behavioral assessment scale. Use the same scale consistently on the patient throughout admission.
Discuss with family members changes in the patient’s behavior that may indicate pain.
Attempt a trial of an analgesic medication.
By attempting to obtain a self-report, searching for potential causes of pain, looking for behavioral cues, and encouraging family member involvement, a comprehensive approach to assessing pain can be used in patients with cognitive impairment.
To help identify pain in adults with limited ability to communicate, nurses need tools that are reliable, valid, and easy to use. The Pain Assessment In Advanced Dementia (PAINAD) scale has been recommended for use in nursing homes and has also been suggested for use in hospitalized adults (Monroe & Mion, 2012), including individuals with DSD (Warden, Hurley, & Volicer, 2003). The PAINAD scale demonstrates adequate psychometric properties and provides a clinically relevant and easy-to-use pain assessment tool for individuals with advanced dementia (Warden et al., 2003). The PAINAD scale may be useful in assessing behaviors associated with pain in patients with cognitive impairments ranging from mild to severe, especially when the ability to communicate has been lost.
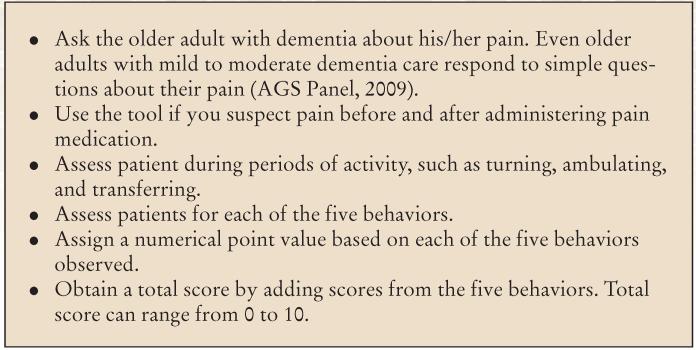
The PAINAD scale assesses five behaviors: breathing, negative vocalization, facial expression, body language, and the ability to be consoled (Figure and Table 2). Each of the five indicators is scored on a range from 0 (not present) to 2 (completely present) based on direct observation for a total score that ranges from 0 to 10 (Warden et al., 2003). Nurses should be careful not to compare the 0 to 10 score on the PAINAD scale with a 0 to 10 score on a verbal pain intensity scale. Pain experts have posited that without self-report, pain intensity is not possible (Pasero & McCaffery, 2005). For example, because of some pathological disorders (e.g., AD, myasthenia gravis, amyotrophic lateral sclerosis), some patients may not possess the ability to behaviorally respond to pain. Furthermore, some medications such as statins, antiarrhythmic agents, corticosteroid agents, colchicine, chloroquine agents, immunomodulator agents, antiviral agents, antifungal/antibacterial agents, oncology drugs, gastrointestinal drugs, or neurological/psychiatric drugs may cause muscle weakness (reviewed in Mor, Wortmann, Mitnick, & Pillinger, 2011).
Figure.
How to use the Pain Assessment in Advanced Dementia (PAINAD) scale. Adapted from Warden, V., Hurley, A.C., & Volicer, L. (2003). Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. Journal of the American Medical Directors Association, 4, 9-15.
TABLE 2. PAIN ASSESSMENT IN ADVANCED DEMENTIA (PAINAD) SCALE.
| Items | Score = 0 | Score = 1 | Score = 2 | Score |
|---|---|---|---|---|
| Breathing (independent of vocalization) |
Normal |
|
|
|
| Negative vocalization | None |
|
|
|
| Facial expression | Smiling or inexpressive |
|
|
|
| Body language | Relaxed |
|
|
|
| Consolability | No need to console |
|
|
|
| Total |
Note. Total scores range from 0 to 10 (based on a scale of 0 to 2 for each of five items), with a higher score indicating more behaviors indicating pain (0 = no observable pain to 10 = highest observable pain).
Adapted from Warden, V., Hurley, A.C., & Volicer, L. (2003). Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. Journal of the American Medical Directors Association, 4, 9-15.
Thus, it is plausible that many comorbidities and/or medications can alter one’s ability to behaviorally respond to pain. Guidelines for scoring the PAINAD scale indicate a score of 2 as a proxy for “likely pain” that requires an intervention such as the administration of a mild opioid agent (Zwakhalen, van der Steen, & Najim, 2011). In contrast, a numeric (verbal) rating scale score of 2 of 10 would likely indicate using a nonpharmacological technique such as repositioning or administration of a nonnarcotic analgesic agent (e.g., acetaminophen [Tylenol®]). Nevertheless, Mosele et al. (2012) assert that the PAINAD scale can be used as a valid proxy for pain intensity.
In Mrs. V.’s case, she is a patient diagnosed with a right hip fracture following a fall at home. She has a long documented history of arthritic pain in both knees. Her fluctuating cognitive impairment plays a critical role in her inability to consistently verbally rate her pain on the numeric scale. During hospitalization, she became more agitated and showed signs of pain. She was unable to verbally rate pain and her PAINAD score was 8:
Occasional labored breathing (breathing independent of vocalization) = 1
Repeated troubled calling out, moaning (negative vocalization) = 2
Facial grimacing (facial expression) = 2
Pulling or pushing away, striking out (body language) = 2
Distraction (consolability) = 1
Total score = 8
Mrs. V. was treated by scheduling her pain medication, which is recommended for postsurgical older adults (Asher, 2004). One study found that older patients who used oral opioid analgesic agents on a scheduled basis were at decreased risk of developing delirium compared with those who used intravenous patient-controlled analgesia management of pain (Vaurio et al., 2006). By morning, Mrs. V. was alert and oriented, and her pain was reduced.
INDIVIDUAL EXAMPLE DISCUSSION
During Mrs. V.’s admission, she was diagnosed with a hip fracture secondary to a fall at home, dementia, and noted chronic pain related to arthritis. Opioid agents were given to her in the emergency department to assist with immediate pain control prior to surgery. Mrs. V. was admitted to the ACE unit sedated from the anesthesia and pain medication with a Richmond Agitation-Sedation Scale (RASS) score of 2, indicating she can be briefly aroused, maintaining eye contact for less than 2 seconds (Sessler et al., 2002). Overnight, Mrs. V. was restless and her mental state began to fluctuate—she was delirious based on her fluctuating mental status, disorganized thinking, and inattention. Mrs. V. has DSD. Pain was addressed once the PAINAD scale was completed, on which Mrs. V. scored an 8. She was given hydrocodone/acetaminophen 5/500 mg and monitored through behavioral observations, vital signs, and continued use of the PAINAD scale. By consistently using the PAINAD scale, Mrs. V.’s pain was reduced.
NURSING IMPLICATIONS
When possible, clinicians should use a combination of subjective and objective reports to help identify pain in patients with dementia, delirium, or DSD. Using a consistent nonverbal pain assessment tool, such as the PAINAD scale, is important and allows clinicians to more accurately manage pain throughout the continuum of care. The recommended frequency of use of the PAINAD scale for patients who have acute pain, in addition to those who have chronic pain, is at least every 4 hours (Horgas & Miller, 2008). A notable limitation of behavioral tools is that they lack a verbal report of pain, and some have suggested that without a verbal report, pain intensity cannot be determined (Pasero & McCaffery, 2005). Clinicians should use discretion when assigning an intensity score to a behavioral score—the 0 to 10 score of the PAINAD scale is not the same as the 0 to 10 verbal descriptive pain intensity scale. However, when used as one part of a comprehensive approach to pain management in older adults with dementia, the PAINAD scale can help reduce the likelihood of experiencing unrecognized and untreated pain. Nurses are the key health care providers often responsible for assessing pain, and their critical thinking skills are essential in using the PAINAD scale as one component of a comprehensive pain management plan in patients with delirium, dementia, or DSD.
Acknowledgments
The clinical example used in this article emerged from a project that was partially supported by a grant from the National Institute of Nursing Research/National Institute of Health (NIH/NINR) (5 R01 NR011042), and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH/NINR.
Footnotes
The authors have disclosed no potential conflicts of interest, financial or otherwise.
Contributor Information
Ms. Christina May Paulson, Vanderbilt University Medical Center.
Dr. Todd Monroe, Vanderbilt University School of Nursing, Nashville, Tennessee.
Dr. Lorraine C. Mion, Vanderbilt University School of Nursing, Nashville, Tennessee.
REFERENCES
- Alzheimer’s Association Alzheimer’s disease facts and figures. 2013 doi: 10.1016/j.jalz.2013.02.003. Retrieved from http://www.alz.org/downloads/Facts_Figures_2013.pdf. [DOI] [PubMed]
- American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons Pharmacological management of persistent pain in older persons. Journal of the American Geriatrics Society. 2009;57:1331–1346. doi: 10.1111/j.1532-5415.2009.02376.x. doi:10.1111/j.1532-5415.2009.02376.x. [DOI] [PubMed] [Google Scholar]
- Asher ME. Surgical considerations in the elderly. Journal of Perianesthesia Nursing. 2004;19:406–414. doi: 10.1016/j.jopan.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Burns A, Gallagley A, Byrne J. Delirium. Journal of Neurology, Neurosurgery, and Psychiatry. 2004;75:362–367. doi: 10.1136/jnnp.2003.023366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crombez G, Eccleston C, Baeyens F, Eelen P. When somatic information threatens, catastrophic thinking enhances attentional interference. Pain. 1998;75:187–198. doi: 10.1016/s0304-3959(97)00219-4. doi:10.1016/S0304-3959(97)00219-4. [DOI] [PubMed] [Google Scholar]
- Desbiens NA, Wu AW, Broste SK, Wenger NS, Connors AF, Jr, Lynn J, Fulkerson W. Pain and satisfaction with pain control in seriously ill hospitalized adults: Findings from the SUPPORT research investigations. For the SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. Critical Care Medicine. 1996;24:1953–1961. doi: 10.1097/00003246-199612000-00005. [DOI] [PubMed] [Google Scholar]
- Eccleston C, Crombez G. Pain demands attention: A cognitive-affective model of the interruptive function of pain. Psychological Bulletin. 1999;125:356–366. doi: 10.1037/0033-2909.125.3.356. [DOI] [PubMed] [Google Scholar]
- Elliott AF, Horgas AL. Effects of an analgesic trial in reducing pain behaviors in community-dwelling older adults with dementia. Nursing Research. 2009;58:140–145. doi: 10.1097/NNR.0b013e318199b599. doi:10.1097/NNR.0b013e318199b599. [DOI] [PubMed] [Google Scholar]
- Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: A systematic review. Journal of the American Geriatrics Society. 2002;50:1723–1732. doi: 10.1046/j.1532-5415.2002.50468.x. [DOI] [PubMed] [Google Scholar]
- Fick DM, Kolanowski AM, Waller JL, Inouye SK. Delirium superimposed on dementia in a community-dwelling managed care population: A 3-year retrospective study of occurrence, costs, and utilization. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2005;60:748–753. doi: 10.1093/gerona/60.6.748. [DOI] [PubMed] [Google Scholar]
- Fick DM, Steis MR, Mion LC, Walls JL. Computerized decision support for delirium superimposed on dementia in older adults. Journal of Gerontological Nursing. 2011;37(4):39–47. doi: 10.3928/00989134-20100930-01. doi:10.3928/00989134-20100930-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gøransson LG, Mellgren SI, Lindal S, Omdal R. The effect of age and gender on epidermal nerve fiber density. Neurology. 2004;62:774–777. doi: 10.1212/01.wnl.0000113732.41127.8f. doi:10.1212/01.WNL.0000113732.41127.8F. [DOI] [PubMed] [Google Scholar]
- Horgas A, Miller L. Pain assessment in people with dementia. American Journal of Nursing. 2008;108:62–71. doi: 10.1097/01.NAJ.0000325648.01797.fc. doi:10.1097/01.NAJ.0000325648.01797.fc. [DOI] [PubMed] [Google Scholar]
- Husebo BS, Strand LI, Moe-Nilssen R, Borgehusebo S, Aarsland D, Ljunggren AE. Who suffers most? Dementia and pain in nursing home patients: A crosssectional study. Journal of the American Medical Directors Association. 2008;9:427–433. doi: 10.1016/j.jamda.2008.03.001. doi:10.1016/j.jamda.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Inouye SK. Delirium in older persons. New England Journal of Medicine. 2006;354:1157–1165. doi: 10.1056/NEJMra052321. doi:10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- Inouye SK, Bogardus ST, Jr., Charpentier PA, Leo-Summers L, Acampora D, Holford TR, Cooney LM., Jr. A multicomponent intervention to prevent delirium in hospitalized older patients. New England Journal of Medicine. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. doi:10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- Mentes JC, Teer J, Cadogan MP. The pain experience of cognitively impaired nursing home residents: Perceptions of family members and certified nursing assistants. Pain Management Nursing. 2004;5:118–125. doi: 10.1016/j.pmn.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Monroe T, Carter M. A retrospective pilot study of African-American and Caucasian nursing home residents with dementia who died from cancer. Journal of Pain and Symptom Management. 2010;40(4):e1–e3. doi: 10.1016/j.jpainsymman.2010.06.007. doi:10.1016/j.jpainsymman.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe TB, Carter MA, Feldt KS, Dietrich MS, Cowan RL. Pain and hospice care in nursing home residents with dementia and terminal cancer. Geriatrics & Gerontology International. 2013;13:1018–1025. doi: 10.1111/ggi.12049. doi:10.1111/ggi.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe TB, Mion LC. Patients with advanced dementia: How do we know if they are in pain? Geriatric Nursing. 2012;33:226–228. doi: 10.1016/j.gerinurse.2012.03.008. doi:10.1016/j.gerinurse.2012.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe TB, Misra SK, Habermann RC, Dietrich MS, Cowan RL, Simmons SF. Pain reports and pain medication treatment in nursing home residents with and without dementia. Geriatrics & Gerontology International. 2013 doi: 10.1111/ggi.12130. Advance online publication. doi:10.1111/ggi.12130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor A, Wortmann RL, Mitnick HJ, Pillinger MH. Drugs causing muscle disease. Rheumatic Disease Clinics of North America. 2011;37:219–231. doi: 10.1016/j.rdc.2011.01.005. doi:10.1016/j.rdc.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Morrison RS, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, Siu AL. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103:303–311. doi: 10.1016/S0304-3959(02)00458-X. [DOI] [PubMed] [Google Scholar]
- Mosele M, Inelmen E, Toffanello E, Girardi A, Coin A, Sergi G, Manzato E. Psychometric properties of the pain assessment in advanced dementia scale compared to self assessment of pain in elderly patients. Dementia and Geriatric Cognitive Disorders. 2012;34:38–43. doi: 10.1159/000341582. doi:10.1159/000341582. [DOI] [PubMed] [Google Scholar]
- Pasero C, McCaffery M. Pain control: When patients can’t report pain. American Journal of Nursing. 2000;100(9):22–23. [PubMed] [Google Scholar]
- Pasero C, McCaffery M. No self-report means no pain-intensity rating: Assessing pain in patients who cannot provide a report. American Journal of Nursing. 2005;105(10):50–53. doi: 10.1097/00000446-200510000-00032. [DOI] [PubMed] [Google Scholar]
- Reyes-Gibby CC, Aday L, Cleeland C. Impact of pain on self-rated health in the community-dwelling older adults. Pain. 2002;95:75–82. doi: 10.1016/s0304-3959(01)00375-x. [DOI] [PubMed] [Google Scholar]
- Robinson S, Rich C, Weitzel T, Vollmer C, Eden B. Delirium prevention for cognitive, sensory, and mobility impairments. Research and Theory for Nursing Practice. 2008;22:103–113. doi:10.1891/0889-7182.22.2.103. [PubMed] [Google Scholar]
- Schreier AM. Nursing care, delirium, and pain management for the hospitalized older adult. Pain Management Nursing. 2010;11:177–185. doi: 10.1016/j.pmn.2009.07.002. doi:10.1016/j.pmn.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Elswick RK. The Richmond Agitation–Sedation Scale: Validity and reliability in adult intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2002;166:1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- Vaurio LE, Sands LP, Wang Y, Mullen EA, Leung JM. Postoperative delirium: The importance of pain and pain management. Anesthesia and Analgesia. 2006;102:1267–1273. doi: 10.1213/01.ane.0000199156.59226.af. doi:10.1213/01.ane.0000199156.59226.af. [DOI] [PubMed] [Google Scholar]
- Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. Journal of the American Medical Directors Association. 2003;4:9–15. doi: 10.1097/01.JAM.0000043422.31640.F7. [DOI] [PubMed] [Google Scholar]
- Zwakhalen SM, van der Steen JT, Najim MD. Which score most likely represents pain on the observational PAINAD pain scale for patients with dementia? Journal of the American Medical Directors Association. 2011;13:384–389. doi: 10.1016/j.jamda.2011.04.002. doi:10.1016/j.jamda.2011.04.002. [DOI] [PubMed] [Google Scholar]