Abstract
The release of reactive oxygen species (ROS) and the generation of oxidative stress are considered critical factors for the pathogenesis of diabetes mellitus (DM), a disorder that is growing in prevalence and results in significant economic loss. New therapeutic directions that address the detrimental effects of oxidative stress may be especially warranted to develop effective care for the millions of individuals that currently suffer from DM. The mechanistic target of rapamycin (mTOR), silent mating type information regulation 2 homolog 1 (S. cerevisiae) (SIRT1), and Wnt1 inducible signaling pathway protein 1 (WISP1) are especially justified to be considered treatment targets for DM since these pathways can address the complex relationship between stem cells, trophic factors, impaired glucose tolerance, programmed cell death pathways of apoptosis and autophagy, tissue remodeling, cellular energy homeostasis, and vascular biology that greatly impact the biology and disease progression of DM. The translation and development of these pathways into viable therapies will require detailed understanding of their proliferative nature to maximize clinical efficacy and limit adverse effects that have the potential to lead to unintended consequences.
1. Oxidative Stress, Cellular Survival, and Programmed Cell Death
Oxidative stress can significantly negatively impact cellular survival and longevity and lead to programmed cell death [1–4]. The generations of reactive oxygen species (ROS) that result in oxidative stress include nitrogen based free radical species such as nitric oxide and peroxynitrite as well as superoxide free radicals, hydrogen peroxide, and singlet oxygen [5]. ROS can result in DNA damage, mitochondrial and other organelle injury, protein misfolding, and neuronal synaptic dysfunction [6–10]. Protective pathways serve to alleviate damage from ROS and involve vitamins B, C, D, and K [11–15], coenzyme Q10 [16], glutathione peroxidase [15, 17], and superoxide dismutase [8, 9, 18–26].
Oxidative stress can lead to the induction of programmed cell death through apoptosis and autophagy [27–31]. Apoptosis has an early phase with the loss of plasma membrane lipid phosphatidylserine (PS) asymmetry and a later phase that leads to genomic DNA degradation [32–34]. Blockade of the early phase with membrane PS externalization is vital for cellular survival since membrane PS externalization can direct inflammatory cells to engulf and remove injured cells [35–37] that may be functional and available for repair [8]. The later phase of cell death with apoptosis leads to the destruction of cellular DNA [1, 38–42].
Autophagy is another pathway of programmed cell death that permits cells to recycle cytoplasmic components while removing dysfunctional organelles for tissue remodeling [30, 34, 43–45]. Of the three categories for autophagy, microautophagy employs the invagination of lysosomal membranes for the sequestration and digestion of cytoplasmic components [34]. In chaperone-mediated autophagy, cytosolic chaperones transport cytoplasmic components across lysosomal membranes. The most prevalent category of autophagy is macroautophagy that consists of the sequestration of cytoplasmic proteins and organelles into autophagosomes. These autophagosomes then combine with lysosomes for degradation and are subsequently recycled for future cellular processes [27, 46–49].
2. Diabetes Mellitus and Clinical Implications
Diabetes Mellitus (DM) is affecting a greater proportion of the world's population each year such that the World Health Organization predicts that DM will be the seventh leading cause of death by the year 2030 [50]. As of the year 2013, almost 350 million individuals are estimated to suffer from DM. In the United States, twenty-one million individuals have DM [51] and an additional eight million individuals are estimated to be presently undiagnosed with DM [52, 53]. The costs of caring for individuals with DM are significant. The United States in the year 2012 spent $8,915 per person for healthcare and approximately seventeen percent of the country's Gross Domestic Product per the Centers for Medicare and Medicaid Services (CMS) [54]. In relation to DM, $176 billion was spent for direct medical costs and another $69 billion in lost finances resulted from reduced productivity.
Early diagnosis and proper care of individuals with DM also may be crucial for extending human longevity by modulating epigenetic changes in age-related genes involved with DM and other degenerative disorders [55–59]. The presence of impaired glucose tolerance in the young raises additional concerns for the future development of DM in these individuals [60]. Obesity is another risk factor for the development of DM [29, 60–63]. Obesity results in cellular oxidative stress and insulin resistance [64, 65], altered trophic factor release [66–69], lipid-induced impairment of pancreatic β-cells [42], and dysfunctional protein tyrosine phosphatase signaling [63, 70].
In insulin dependent (Type 2) DM, defective insulin secretion can result from impaired β-cell function, oxidative stress [29, 71], the absence of inhibitory feedback through plasma glucagon levels, chronic exposure to free fatty acids [72], lipotoxicity [42], and hyperglycemia [8]. Type 2 DM is the most prevalent subtype for this disorder occurring in ninety percent of individuals that are usually over the age of 40. A progressive deterioration of glucose tolerance occurs with early β-cell compensation that is followed by a decrease in pancreatic β-cell mass with insulin resistance and impaired insulin secretion [29].
In contrast to Type 2 DM, Type 1 DM is an autoimmune disorder with the presence of alleles of the human leukocyte antigen (HLA) class II genes within the major histocompatibility complex (MHC). Type 1 DM occurs in approximately 5–10% of patients with DM [29]. Activation of T-cell clones that are capable of recognizing and destroying pancreatic β-cells to result in insulin deficiency may not always lead to programmed cell death but rather relies upon the necrotic death of β-cells [73]. Destruction of pancreatic β-cells with inflammatory infiltration of the islets of Langerhans results in the loss of insulin production and regulation. Almost all patients with Type 1 DM have increased titers of autoantibodies (Type 1A DM). However, approximately 10% of Type 1 DM individuals do not have serum autoantibodies and are considered to have maturity-onset diabetes of the young (MODY) that can be a result of β-cell dysfunction with autosomal-dominant inheritance (Type 1B DM). Type 1 and Type 2 DM may have common links since approximately 10% of individuals with Type 2 DM may have elevated serum autoantibodies similar to Type 1 DM [74] and insulin resistance also may be a component of Type 1 DM in some patients [75–77].
DM essentially affects all systems of the body. In the vascular system, high glucose leads to the loss of endothelial cells [69, 71, 78–82], fosters endothelial cell senescence [83], prevents angiogenesis [84], impairs mobilization of bone marrow endothelial progenitor cells [85], injures the neuroglialvascular unit injury [86], and results in diffuse vascular disease [27, 81, 83, 84, 87–89]. DM results in additional vascular events that result in cardiac disease [46, 90–97], atherosclerosis [2], and renal disorders [61, 98–101]. DM leads to immune system dysfunction [12, 96, 102–105], liver disorders [106–109], stroke [7, 14, 59, 87, 110, 111], Alzheimer's disease [68, 75, 112, 113], psychiatric disease [114, 115], visual loss [86, 116–118], and peripheral nerve impairment [88].
3. Diabetes Mellitus, Oxidative Stress, and Programmed Cell Death
Progressive disease in the body that occurs during DM is mediated to a significant extent through the release of ROS and oxidative stress [8, 14, 29, 119–123]. Patients with Type 2 DM have serum markers of oxidative stress with ischemia-modified albumin [124]. Acute rises in serum glucose as well as chronic elevations can result in the release of ROS during DM [125]. In addition, some studies suggest that treatment with antioxidants may limit the prevention of cardiovascular disease during DM [14].
In cell culture models of DM, elevated glucose levels result in oxidative stress and cell injury in cardiomyocytes [93, 97, 126], endothelial cells [78–80, 85, 86, 127], and neurons [21, 71, 116, 128, 129]. Oxidative stress also results in elevated glutathione levels and increased lipid peroxidation in murine animal models of Type 2 DM [92]. Advanced glycation end products (AGEs), entities that foster complications in DM [91], lead to the release of ROS and caspase activation [122].
At the cellular level, uncoupling proteins (UCPs), a family of carrier proteins found in the inner membrane of mitochondria and consist of the mammalian members UCP1, UCP2, UCP3, UCP4, and UCP5, can significantly influence cell survival in DM [76, 120, 130]. UCPs uncouple oxygen consumption through the respiratory chain from ATP synthesis [48, 76, 120, 131]. Subsequently, this leads to oxidative stress as UCPs disperse a proton electrochemical potential gradient across the mitochondrial inner membrane resulting in the activation of substrate oxidation and dissipation of oxidation energy as heat instead of ATP [76, 120]. Uncoupling of respiration by UCPs modulates ATP synthesis, fatty acid release, and glucose oxidation. Overexpression of UCP in skeletal muscle of mice enhances responsiveness to insulin, improves glucose transport in skeletal muscle, and increases resistance to obesity [132]. In addition, skeletal muscle respiratory uncoupling can improve insulin sensitivity in obesity [133]. In regards to UCP3, it can stimulate insulin uptake [134], can facilitate fatty acid oxidation, and can limit ROS production [135]. However, it should be recognized that not all UCPs are beneficial. Overexpression of UCP2 in isolated pancreatic islets leads to decreased ATP levels and reduced glucose-stimulated insulin secretion. Loss of UCP2 improves insulin secretion and decreases hyperglycemia in leptin-deficient mice [136].
Closely tied to the role of UCPs is the impairment of mitochondrial dysfunction that can occur during oxidative stress [2, 5, 6, 137, 138]. Skeletal muscle mitochondria in patients with Type 2 DM have been reported to be smaller than those in control subjects [139]. Decreased mitochondrial proteins and mitochondrial DNA in adipocytes also have been associated with the development of Type 2 DM [140]. Exposure of glucolipotoxicity to pancreatic β-cells promotes oxidative stress and mitochondrial dysfunction with cytochrome c release, caspase activation, and apoptosis [141]. Mitochondrial dysfunction leads to the opening of the mitochondrial membrane permeability transition pore, release of cytochrome c, and subsequent caspase activation [27, 78, 80, 82, 127, 141, 142].
The pathways of programmed cell death that involve apoptosis [14, 82, 88, 143, 144] and autophagy [8, 34, 61, 145] also regulate cell survival during DM and oxidative stress. For example, “highly oxidized glycated” low density lipoproteins that are formed during DM result in oxidative stress in human retinal capillary pericytes with subsequent induction of apoptosis and autophagy [116]. Current studies also suggest that the programmed cell death pathway of necroptosis may not significantly contribute to cell injury during DM, but future work may change this perspective [146]. In murine models of Type 1 DM, necroptosis may have less than an essential role in cell survival during DM [73]. In relation to apoptosis, apoptotic cell death during DM occurs in pancreatic β-cells [147–149], cardiomyocytes [46, 93, 96], endothelial cells [79, 83, 84, 127, 150], renal cells [151–153], and neurons [21, 114, 128, 154].
Autophagy may be cytoprotective as well as detrimental to cell survival during DM. During elevated glucose, autophagy can impair endothelial progenitor cells, lead to mitochondrial oxidative and endoplasmic reticulum stress [155], and prevent the formation of new blood vessels [27]. Increased activity of autophagy has been associated with loss of cardiac and liver tissue in diabetic rats during attempts to achieve glycemic control through diet modification [156]. AGEs also have been shown to lead to the induction of autophagy and vascular smooth muscle proliferation that can cause atherosclerosis [89] as well as cardiomyopathy [126]. Yet, under some conditions, autophagy may be less of a significant mediator of cell injury [157] and it may actually be beneficial. Autophagy may be required to eliminate misfolded proteins and nonfunctioning mitochondria to avert β-cell dysfunction and the onset of DM [141]. Loss of autophagy with haploinsufficiency of an essential Atg7 gene in murine models of obesity can lead to increased insulin resistance with elevated lipids and inflammation [47]. Autophagy also may improve insulin sensitivity during high fat diets in mice [65] and autophagy has been associated with exercise in mice that regulates glucose homeostasis [158]. Pathways of autophagy and apoptosis also can work in unison to modulate cell survival. Induction of autophagy may protect cardiomyocytes from apoptotic cell death during DM [46].
4. Mechanistic Target of Rapamycin
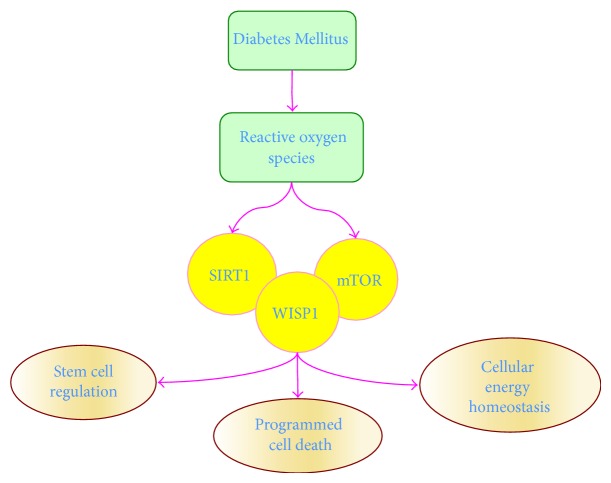
The mechanistic target of rapamycin (mTOR), also termed the mammalian target of rapamycin and FK506-binding protein 12-rapamycin complex-associated protein 1, is a principal pathway in DM that can significantly affect apoptosis and autophagy [2, 91, 159, 160] (Figure 1). mTOR is a 289-kDa serine/threonine protein kinase. It is encoded by a single gene FRAP1 [161–163] and is a component of the protein complexes mTOR Complex 1 (mTORC1) and mTOR Complex 2 (mTORC2) [164, 165]. mTORC1 consists of Raptor (Regulatory-Associated Protein of mTOR), the proline rich Akt substrate 40 kDa (PRAS40), Deptor (DEP domain-containing mTOR interacting protein), and mammalian lethal with Sec13 protein 8 (mLST8). mTORC2 consists of Rictor (Rapamycin-Insensitive Companion of mTOR), Deptor, mLST8, the mammalian stress-activated protein kinase interacting protein (mSIN1), and the protein observed with Rictor-1 (Protor-1) [165, 166].
Figure 1.
Oxidative stress in Diabetes Mellitus impacts pathways of stem cell proliferation, programmed cell death, and cellular energy homeostasis. Diabetes Mellitus (DM) leads to the development of oxidative stress and the release of reactive oxygen species (ROS). Novel proliferative pathways for targeting new treatments against DM and the complications of this disorder are the mechanistic target of rapamycin (mTOR), silent mating type information regulation 2 homolog 1 (S. cerevisiae) (SIRT1), and Wnt1 inducible signaling pathway protein 1 (WISP1). Each of these pathways is intimately connected through shared signal transduction mechanisms that can oversee stem cell proliferation, programmed cell death that involves apoptosis and autophagy, and cellular energy homeostasis that can affect mitochondrial function and insulin sensitivity.
mTOR is a vital component of cytokine and growth factor signaling such as erythropoietin (EPO) [66, 167–171] (Table 1). EPO uses mTOR for cytoprotection [61, 91, 100, 165, 172]. Through mTOR, EPO protects vascular cells [67, 173], prevents cell injury during β-amyloid (Aβ) exposure [170], modulates bone homeostasis [167], promotes retinal progenitor cell survival during oxidant stress [169] and blocks retinal degeneration in models of polycystic kidney disease [86], promotes the neuronal phenotype of adult neuronal precursor cells [168], improves cognitive function in sepsis-associated encephalopathy [171], and limits cell injury during oxygen-glucose deprivation [174, 175]. In regards to cellular metabolism, EPO promotes wound healing during DM [102], maintains cellular mitochondrial function and energy metabolism [82], reduces the detrimental effects of obesity in animal models [69], limits high glucose-induced oxidative stress in renal tubular cells [151], and protects endothelial cells during experimental models of DM [78, 79].
Table 1.
Targeting mTOR, SIRT1, and WISP1 in Oxidative Stress and DM.
| Target | Actions |
|---|---|
| mTOR | Functions through trophic factors such as EPO to protect vascular cells, promotes neuronal precursors, and blocks retinal degeneration Functions through metformin during mTOR inhibition and AMPK activity to protect against cardiomyopathy, protect cortical brain tissue, and prevent endothelial senescence Promotes stem cell development, promotes pancreatic β-cell proliferation, and blocks vascular thrombosis |
|
| |
| SIRT1 | Promotes telomere elongation and genomic stability of induced pluripotent stem cells, prevents apoptosis in endothelial progenitor cells and mesenchymal stem cells, increases lifespan in higher organisms, and preserves angiogenesis Prevents insulin resistance through fat mobilization, mTOR signaling, and control of cellular inflammation Increases insulin signaling through PI 3-K and Akt and insulin release in pancreatic cells, promotes autophagy to protect embryonic stem cells during oxidative stress, in conjunction with AMPK activation protects endothelial cells during exposure to oxidized low density lipoproteins that can lead to atherosclerosis |
|
| |
| WISP1 | During pancreatic regeneration, WISP1 is one of several genes that are over-expressed, suggesting that WISP1 may be reparative during DM Promotes vascular smooth muscle proliferation that may be important for tissue repair, activates PI 3-K and Akt pathways to protect cells against oxidative stress and programmed cell death Oversees vascular senescence, modulates AMPK activity that may be sometimes detrimental, maintains the integrity of SIRT1 and prevent its degradation during oxidative stress |
AMPK: AMP activated protein kinase; Akt: protein kinase B; EPO: erythropoietin; mTOR: mechanistic target of rapamycin; PI 3-K: phosphoinositide 3 –kinase; SIRT1: silent mating type information regulation 2 homolog 1 (S. cerevisiae); WISP1: wnt1 inducible signaling pathway protein 1.
Cytokines and growth factors are not the only agents that rely upon the regulation of mTOR in DM to impact cellular survival. Metformin, an agent that controls hyperglycemia in DM, inhibits mTOR activity and promotes autophagy. Metformin oversees mTOR activity through AMP activated protein kinase (AMPK). AMPK controls the activity of the hamartin (tuberous sclerosis 1)/tuberin (tuberous sclerosis 2) (TSC1/TSC2) complex that is an inhibitor of mTORC1 [176]. AMPK phosphorylates TSC2 as well as Raptor to block the activity of mTOR and the complex mTORC1 during energy stress [177]. By activating AMPK to inhibit mTOR, metformin prevents cell loss during hypoxia [178], reduces cardiomyopathy in experimental models of DM [179], increases cardiomyocyte cell survival [46], and protects cortical brain tissue during cerebral ischemia [110]. Through mTOR inhibition, metformin prevents endothelial cell senescence [83], blocks neuronal apoptotic cell death [180], and prevents androgen upregulation during prostate cancer [181]. AMPK activity can be protective against hypoxia [178], promote autophagy to reduce memory impairment [182], and reduce oxidative stress that can lead to vascular hypertension [183]. Yet, AMPK activity is not consistently beneficial and can cause aberrant Aβ stress [184] and Aβ toxicity [185], cardiac tissue hypertrophy [186], and neuroinflammation [187].
Independently, mTOR activation controls stem cell development [2, 16, 165, 176, 188–190], promotes pancreatic β-cell proliferation [149], prevents apoptosis, limits insulin resistance, blocks vascular thrombosis in patients with metabolic syndrome [191], and prevents pathways associated with atherosclerosis [192] (Table 1). In addition, mTOR activation through application of glucagon-like peptide-1 agonists can protect pancreatic β- cells from cholesterol mediated apoptotic cell injury [72]. mTOR also functions through the epidermal growth factor receptor to prevent neuronal apoptotic cell loss during DM [154].
5. Silent Mating Type Information Regulation 2 Homolog 1 (S. cerevisiae)
Silent mating type information regulation 2 homolog 1 (S. cerevisiae) (SIRT1), also known as NAD-dependent deacetylase sirtuin-1, is a member of the Sirtuin family and plays a significant role in cellular metabolism and DM (Figure 1). As histone deacetylases, sirtuins transfer acetyl groups from ε-N-acetyl lysine amino acids on the histones of DNA to regulate cellular transcription [193–195]. SIRT1 can modulate cellular metabolism [105, 196–198] and may be critical for the development of new therapies for DM [29, 52, 193, 199]. SIRT1 is one of seven mammalian homologues of the yeast silent information regulator-2 (Sir2) that control posttranslational changes of proteins for cellular growth and maintenance [83, 127, 199, 200]. SIRT1 is dependent upon NAD+ as a substrate [105, 193, 201, 202] and through nicotinamide phosphoribosyltransferase (NAMPT) catalyzes the conversion of nicotinamide to nicotinamide mononucleotide [12]. Nicotinamide mononucleotide is subsequently converted to NAD+ by the nicotinamide/nicotinic acid mononucleotide adenylyltransferase (NMNAT) enzyme family [203]. NMNAT can control the deacetylating activity of SIRT1. NAMPT activity increases cellular NAD levels and enhances the activity of SIRT1 transcription. Mammalian forkhead transcription factors can also influence SIRT1 activity [193, 204–206]. Mammalian forkhead transcription factors bind to the SIRT1 promoter region, a cluster of five putative core binding repeat motifs (IRS-1) and a forkhead-like consensus-binding site (FKHD-L) [207]. This binding fosters the ability of forkhead transcription factors, such as FoxO1, to control SIRT1 transcription and increase SIRT1 expression [208].
SIRT1 importantly modulates stem cell survival that may ultimately influence cellular protection during DM as well as other cellular toxic environments [7, 48, 209]. Recent work suggests that stem cell strategies may be effective for maintaining glucose homeostasis during DM in animal models [210, 211]. SIRT1 is required for telomere elongation and genomic stability of induced pluripotent stem cells [212] (Table 1). During oxidative stress, SIRT1 prevents apoptosis through the induction of autophagy in endothelial progenitor cells [213]. SIRT1 can regulate autophagic flux [214] to promote the transition of muscle stem cells from a quiescence state to an active state [215]. Mesenchymal stem cells with SIRT1 overexpression lead to increased blood vessel density in the area of cardiac infarcts, reduced cardiac remodeling, and improved cardiac performance in rodent models [216]. Increased SIRT1 expression also enhances the survival of cardiomyoblasts [217]. These studies of cardiovascular protection suggest an important role for angiogenesis especially since patients with Type 2 DM show a downregulation of endothelial progenitor cells that has been associated with decreased SIRT1 protein levels [218]. In particular, SIRT1 prevents senescence and impaired differentiation in endothelial progenitor cells [219] and is necessary for the angiogenic properties of human mesenchymal stem cells [220]. SIRT1 also is necessary for endothelial progenitor cell mobilization and vascular repair during DM in mice [196]. SIRT1 can preserve angiogenesis in rodent models of DM with bone marrow-derived early outgrowth cells [221]. In addition, SIRT1 may function in conjunction with growth factors to foster improved cardiac performance during glucose depletion through the activation of aged mesenchymal stem cells [222].
In some cases, a limited activity of SIRT1 may be required for optimal stem cell function. SIRT1 can be a negative regulator of subventricular zone and hippocampal neural precursors in murine animal models. Knockdown of SIRT1 does not eliminate neural precursor numbers but increases the production of neurons in the subventricular zone and the hippocampus [223]. Absence of SIRT1 with the induction of heat shock protein-70 (HSP70) also is necessary to promote neural differentiation, maturation of embryonic cortical neurons [224], and the differentiation of human embryonic stem cells into motoneurons [225]. Neuronal differentiation also can be driven through the microRNA miR-34a that leads to decreased SIRT1 expression and DNA-binding of p53. However, a minimum level of SIRT1 may be necessary for some cells since increased expression of SIRT1 can increase the astrocytic subpopulation of cells that are necessary to support neuronal cell populations [226].
In mature and differentiated cells, SIRT1 can prevent insulin resistance through a number of mechanisms that involve fat mobilization [197], mTOR signaling [227], and control of cellular inflammation [228] (Table 1). SIRT1 can increase insulin signaling in insulin-sensitive organs through pathways that involve phosphoinositide 3-kinase (PI 3-K) and protein kinase B (Akt) [32, 127, 200, 229–231]. SIRT1 also can stimulate glucose-dependent insulin secretion from pancreatic β-cells by repressing UCP2 [232]. Loss of SIRT1 can lead to insulin resistance and excessive hepatic lipid accumulation [197]. Gene deletion or pharmacological inhibition of SIRT1 can impair insulin signaling by interfering with insulin stimulated insulin receptor phosphorylation and glycogen synthase [233]. Overexpression of SIRT1 has been shown to decrease hepatic steatosis and improve insulin sensitivity [108]. Interestingly, SIRT1 has been shown to increase lifespan in higher organisms such as Drosophila and offer protection against oxidative stress [234], and it is used by EPO to prevent cell injury during oxidative stress and DM. EPO can increase endogenous cellular SIRT1 activity and promote the subcellular nuclear trafficking of SIRT1 to result in endothelial cell protection during oxidative stress [200]. EPO is able to maintain adipose cell energy homeostasis and protect against metabolic disorders such as DM through SIRT1 [198].
SIRT1 promotes cellular survival during oxidative stress and DM by preventing the induction of apoptotic pathways. Loss of SIRT1 activity in human mesenchymal stem cells leads to reduced cellular proliferation with increased apoptosis [220]. Absence of SIRT1 in mouse cochlear neurons and in the auditory cortex also is associated with hearing loss [235]. Decreased levels of SIRT1 that occurs in smokers and chronic obstructive disease patients lead to endothelial progenitor cell dysfunction with apoptotic cell death [236]. In contrast, SIRT1 activation can prevent neuronal apoptosis in models of traumatic brain injury [237]. SIRT1 activation can protect endothelial progenitor cells against apoptosis [238] and enhance skeletal myoblast survival [239] during tumor necrosis factor-α (TNF-α) exposure. SIRT1 can prevent the externalization of membrane PS residues during apoptosis [32, 127, 200, 240]. As a result of the cytoprotective capacity of SIRT1, mechanisms that can block SIRT1 degradation are vital. Pathways involving Wnt signaling have been shown to prevent SIRT1 degradation and block caspase activation [241–244]. Decreased levels of SIRT1 activity can be the result of apoptotic pathways associated with p38 [245] and c-Jun N-terminal kinase-1 (JNK1) [106]. Caspase degradation of SIRT1 [246] also can lead to further activation of caspases [246, 247]. As described, loss of SIRT1 activity can yield significant consequences for cellular protection. Absent or insufficient SIRT1 activity can be detrimental for vascular cells [127, 200, 248], prevent protection against cardiovascular disease [249], and lead to neuronal injury [231, 243, 250]. Yet, in some cases, a reduction in SIRT1 activity may be necessary to promote cellular survival such as in studies involving trophic factors with insulin growth factor-1 [251].
Autophagy also is another significant component in determining cell survival with SIRT1. SIRT1 promotes autophagy in mitochondria [252] that may be required to maintain a healthy mitochondrial pool associated with cellular metabolism [253]. SIRT1 activation is able to limit apoptotic cell injury and improve cognition through the induction of autophagy in models of cognitive loss that employ chronic intermittent hypoxia hypercapnia exposure [254]. SIRT1 leads to the induction of autophagy for chondrocyte survival during oxidative stress. Loss of autophagy through knockdown of the forkhead transcription factors FoxO1 and FoxO3 depletes SIRT1 activity and results in chondrocyte cell death [18]. However, in some scenarios, SIRT1 protection has been reported to involve the downregulation of autophagy. SIRT1 blocks cell injury through the inhibition of autophagy in pulmonary models of oxidative stress during exposure to cigarette smoke in bronchial epithelial cells [255, 256].
Intimately tied to the ability of SIRT1 to modulate autophagy are the pathways of AMPK and mTOR (Table 1). AMPK increases NAMPT during glucose restriction leading to increased NAD+ [257] and decreased levels of the SIRT1 inhibitor nicotinamide [60]. Resveratrol, an activator of SIRT1, can enhance AMPK activity through SIRT1 dependent and independent mechanisms [258, 259]. Once active, AMPK can phosphorylate TSC2 and inhibit mTORC1 activity [8, 165]. Through AMPK activity, SIRT1 inhibits mTOR. As a result, SIRT1 promotes autophagy to protect embryonic stem cells during oxidative stress [190]. SIRT1 has been shown to inhibit mTOR signaling to promote neuronal growth [260] and assist with mesangial cell proliferation during high glucose exposure [261]. AMPK also can increase the cellular NAD+/NADH ratio leading to the deacetylation of downstream SIRT1 targets that include the peroxisome proliferator-activated receptor-gamma coactivator 1 (PGC-1α), FoxO1 [94], and FoxO3a [258]. SIRT1 upregulation with AMPK activation promotes autophagy that is necessary for endothelial cell protection during exposure to oxidized low density lipoproteins that can lead to atherosclerosis [206]. SIRT1 also uses AMPK for the regulation of insulin sensitivity. Endothelial cell protection from oxidized low density lipoproteins requires SIRT1 as well as AMPK activation [206, 262]. SIRT1 activation with AMPK also may be necessary to protect against spatial memory impairment in combined experimental models of DM and Alzheimer's disease. Loss of SIRT1 and AMPK activities can lead to cognitive loss, oxidative stress, and neuronal cell apoptosis [112].
6. Wnt1 Inducible Signaling Pathway Protein 1
The CCN family member Wnt1 inducible signaling pathway protein 1 (WISP1) has cellular signaling pathways linked to mTOR and SIRT1 that highlight the significance of WISP1 in DM (Figure 1). The CCN family of proteins consists of six secreted extracellular matrix associated proteins and are defined by the first three members of the family that include cysteine-rich protein 61, connective tissue growth factor, and Nephroblastoma overexpressed gene [263]. Members of this family such as WISP1 contain four cysteine-rich modular domains that include insulin-like growth factor-binding domain, thrombospondin domain, von Willebrand factor type C module, and C-terminal cysteine knot-like domain [264]. The WISP1 gene was identified in a mouse mammary epithelial cell line [265] and subsequently demonstrated to modulate gastric tumor growth [266]. WISP1 is a matricellular protein [267] and a downstream target of the wingless pathway Wnt1 that has broad cellular effects to control programmed cell death, stem cell growth, immunity, nervous, cardiovascular, and musculoskeletal system development, and tumorigenesis [79, 268–280]. WISP1 can control cell survival through pathways that involve autophagy [34, 157], apoptosis [243, 281–283], and caspase activation [243, 282, 284]. During oxidative stress, WISP1 can upregulate PI 3-K and Akt [157, 243, 284] and protect against Aβ exposure [185], cardiomyocyte injury [282], and DNA damage [281] (Table 1). Through Akt, WISP1 also leads to fibroblast proliferation in airway remodeling [285], vascular smooth muscle proliferation [286], inhibitory phosphorylation of glycogen synthase kinase-3β (GSK-3β) [157, 282, 284, 285], and the maintenance of β-catenin that can prevent apoptotic cell death [36, 269, 274, 287, 288].
Similar to pathways involving mTOR and SIRT1, a portion of the protective capacity of WISP1 may rely upon stem cell oversight. WISP1 can influence induced pluripotent stem cell reprogramming [289]. WISP1 is differentially regulated during stem cell migration and stem cell differentiation. WISP1 expression is increased during stem cell migration [290] and repressed in adipose-derived stem cells during hepatic differentiation [291]. WISP1 expression that may be associated with inflammation and obesity is increased during human adipocyte differentiation [292]. During pancreatic regeneration, WISP1 is one of several genes that are overexpressed, suggesting that WISP1 may be reparative during DM [293]. WISP1 also may be vital for therapeutic strategies against vascular disease in DM. WISP1 leads to vascular smooth muscle proliferation that may be important for tissue repair as well as affect restenosis following vascular grafting [286, 294]. WISP1 may provide support for vascular repair and regeneration during saphenous vein crush injury [295]. WISP1 also oversees cellular senescence [296] and does not lead to excessive cellular proliferation in aging vascular cells [297] that can lead to atherosclerosis (Table 1).
In regards to mTOR and WISP1 [264, 275], WISP1 activates and phosphorylates mTOR. WISP1 also leads to the activation of the mTOR signaling pathways of p70 ribosomal S6 kinase (p70S6K) and the eukaryotic initiation factor 4E-binding protein 1 (4EBP1) [91, 174]. WISP1 increases mTOR activity by antagonizing the inhibitory actions of the mTOR component proline rich Akt substrate 40 kDa (PRAS40) [298]. WISP1 also oversees the posttranslational phosphorylation of AMPK that is involved in glucose homeostasis [164, 165, 299, 300]. WISP1 controls AMPK activation by differentially decreasing phosphorylation of TSC2 at Ser1387, a target of AMPK, and increasing phosphorylation of TSC2 at Thr1462, a target of Akt [185]. The ability of WISP1 to modulate AMPK activity is vital for the regulation of cellular metabolism during DM [300]. AMPK activity can reduce insulin resistance and lessen oxidative stress through activation of autophagy [65]. AMPK also may prevent myocardial ischemia in experimental models of DM [301], promote proper metabolic function of cells [302], and place limits on adipocyte differentiation, lipid accumulation, and obesity [262]. Yet, the level of AMPK activity is a significant consideration in DM. In some experimental models of Type 2 DM, AMPK activation can lead to apoptosis in pancreatic islet cells [303].
WISP1 also regulates cellular metabolism through its protective actions over SIRT1. WISP1 increases SIRT1 activity and fosters SIRT1 nuclear translocation [243] to block apoptotic cell injury [127, 200, 304]. WISP1 controls the mammalian forkhead transcription factor FoxO3a that is involved in cellular metabolism to block caspase activity [42, 94, 107, 305, 306] and prevent the degradation of SIRT1 during oxidative stress [243] (Table 1). As previously described, Wnt signaling that involves WISP1 is vital to prevent SIRT1 degradation, prevent caspase activation, and promote cellular survival [241–244].
7. Conclusions
Oxidative stress is a significant mediator of multisystem disease in the body during DM. Clinical studies and experimental models point to cell injury that involves both apoptosis and autophagy during DM as a result of oxidative stress and the release of ROS. Given that DM is predicted to become the seventh leading cause of death by the year 2030, the need for new therapeutic opportunities to treat DM and its complications becomes increasingly acute. One exciting strategy for consideration is mTOR. mTOR activation oversees stem cell development, fosters pancreatic β-cell proliferation, limits insulin resistance, and can prevent pathways that may lead to atherosclerosis. Protective cytokines and growth factors such as EPO rely upon mTOR for vascular cell protection, neuronal cell survival, and bone homeostasis. Furthermore, EPO can lead to wound healing during DM, maintains cellular mitochondrial function and energy metabolism, and reduces the detrimental effects of obesity in animal models. Yet, inhibitory pathways of mTOR that involve AMPK also have a critical role during DM. AMPK activity can reduce insulin resistance and lessen oxidative stress through activation of autophagy. In addition, metformin, an agent that controls hyperglycemia in DM, activates AMPK and inhibits mTOR activity to promote autophagy and cytoprotection. Metformin reduces cardiomyopathy in experimental models of DM, prevents endothelial cell senescence, and prevents neuronal apoptotic cell death. Interestingly, SIRT1 also relies upon AMPK for the regulation of insulin sensitivity and to induce autophagy that is necessary for endothelial cell protection during exposure to oxidized low density lipoproteins that can lead to atherosclerosis. Yet, AMPK activity is not consistently beneficial and can lead to Aβ stress, Aβ toxicity, cardiac tissue hypertrophy, and neuroinflammation. In some experimental models of Type 2 DM, AMPK activation can lead to apoptosis in pancreatic islet cells. SIRT1 importantly modulates stem cell survival, blocks apoptotic cell injury, controls autophagy for mitochondrial pool maintenance, and limits oxidative stress that affects cellular survival during DM. Although SIRT1 can increase cell survival and preserve insulin signaling by blocking apoptotic pathways, SIRT1 also can foster autophagy and limit mTOR activation to preserve mitochondria, promote stem cell proliferation, and prevent insulin resistance. WISP1 incorporates the pathways of mTOR and SIRT1 to control stem cell migration as well as stem cell differentiation. WISP1 may offer protection against cell loss in DM since it is one of several transcripts that are expressed during pancreatic regeneration. WISP1 can activate PI 3-K, Akt, and mTOR to protect against Aβ exposure, cardiomyocyte injury, DNA damage, and oxidative stress. WISP1 also increases SIRT1 activity and maintains the integrity of SIRT1 during oxidative stress to prevent SIRT1 degradation. New insights that develop mTOR, SIRT1, and WISP1 as effective therapeutic strategies against DM offer great hope for the millions of individuals that presently suffer from this disabling disorder. Fruits of such investigations will weigh heavily upon careful analysis of the intricate and complex pathways controlled by the proliferative properties of mTOR, SIRT1, and WISP1 to achieve high clinical efficacy for patients with DM and limit adverse effects that can involve organ dysfunction, pancreatic cell loss, tumor growth, and inflammation.
Acknowledgments
This research was supported by the following grants to Kenneth Maiese: American Diabetes Association, American Heart Association, NIH NIEHS, NIH NIA, NIH NINDS, and NIH ARRA.
Conflict of Interests
The author declares no conflict of interests regarding the publication of this paper.
References
- 1.Chong Z. Z., Li F., Maiese K. Oxidative stress in the brain: novel cellular targets that govern survival during neurodegenerative disease. Progress in Neurobiology. 2005;75(3):207–246. doi: 10.1016/j.pneurobio.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Maiese K. mTOR: driving apoptosis and autophagy for neurocardiac complications of diabetes mellitus. World Journal of Diabetes. 2015;6(2):217–224. doi: 10.4239/wjd.v6.i2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peng S., Zhao S., Yan F., et al. HDAC2 selectively regulates FOXO3a-mediated gene transcription during oxidative stress-induced neuronal cell death. Journal of Neuroscience. 2015;35(3):1250–1259. doi: 10.1523/jneurosci.2444-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xin Y., Yuan B., Yu B., et al. Tet1-mediated DNA demethylation regulates neuronal cell death induced by oxidative stress. Scientific Reports. 2015;5, article 7645 doi: 10.1038/srep07645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwon S. H., Hong S. I., Ma S. X., Lee S. Y., Jang C. G. 3′,4′,7-trihydroxyflavone prevents apoptotic cell death in neuronal cells from hydrogen peroxide-induced oxidative stress. Food and Chemical Toxicology. 2015;80:41–51. doi: 10.1016/j.fct.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Harish G., Mahadevan A., Pruthi N., et al. Characterization of traumatic brain injury in human brains reveals distinct cellular and molecular changes in contusion and pericontusion. Journal of Neurochemistry. 2015 doi: 10.1111/jnc.13082. [DOI] [PubMed] [Google Scholar]
- 7.Maiese K. SIRT1 and stem cells: In the forefront with cardiovascular disease, neurodegeneration and cancer. World Journal of Stem Cells. 2015;7(2):235–242. doi: 10.4252/wjsc.v7.i2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maiese K., Chong Z. Z., Wang S., Shang Y. C. Oxidant stress and signal transduction in the nervous system with the PI 3-K, Akt, and mTOR cascade. International Journal of Molecular Sciences. 2012;13(11):13830–13866. doi: 10.3390/ijms131113830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palma H. E., Wolkmer P., Gallio M., et al. Oxidative stress parameters in blood, liver, and kidney of diabetic rats treated with curcumin and/or insulin. Molecular and Cellular Biochemistry. 2014;386(1-2):199–210. doi: 10.1007/s11010-013-1858-5. [DOI] [PubMed] [Google Scholar]
- 10.Zeldich E., Chen C. D., Colvin T. A., et al. The neuroprotective effect of Klotho is mediated via regulation of members of the redox system. The Journal of Biological Chemistry. 2014;289(35):24700–24715. doi: 10.1074/jbc.m114.567321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bowes Rickman C., Farsiu S., Toth C. A., Klingeborn M. Dry age-related macular degeneration: mechanisms, therapeutic targets, and imaging. Investigative Ophthalmology and Visual Science. 2013;54(14):ORSF68–ORSF80. doi: 10.1167/iovs.13-12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maiese K., Chong Z. Z., Hou J., Shang C. The vitamin nicotinamide: translating nutrition into clinical care. Molecules. 2009;14(9):3446–3485. doi: 10.3390/molecules14093446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miret J. A., Munné-Bosch S. Plant amino acid-derived vitamins: biosynthesis and function. Amino Acids. 2014;46(4):809–824. doi: 10.1007/s00726-013-1653-3. [DOI] [PubMed] [Google Scholar]
- 14.Xu Y.-J., Tappia P. S., Neki N. S., Dhalla N. S. Prevention of diabetes-induced cardiovascular complications upon treatment with antioxidants. Heart Failure Reviews. 2014;19(1):113–121. doi: 10.1007/s10741-013-9379-6. [DOI] [PubMed] [Google Scholar]
- 15.Yousef J. M., Mohamed A. M. Prophylactic role of B vitamins against bulk and zinc oxide nano-particles toxicity induced oxidative DNA damage and apoptosis in rat livers. Pakistan Journal of Pharmaceutical Sciences. 2015;28(1):175–184. [PubMed] [Google Scholar]
- 16.Zhang D., Yan B., Yu S., et al. Coenzyme Q10 inhibits the aging of mesenchymal stem cells induced by D-galactose through Akt/mTOR signaling. Oxidative Medicine and Cellular Longevity. 2015;2015:10. doi: 10.1155/2015/867293.867293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rjiba-Touati K., Ayed-Boussema I., Guedri Y., Achour A., Bacha H., Abid-Essefi S. Effect of recombinant human erythropoietin on mitomycin C-induced oxidative stress and genotoxicity in rat kidney and heart tissues. doi: 10.1177/0960327115577521. Human & Experimental Toxicology. In press. [DOI] [PubMed] [Google Scholar]
- 18.Akasaki Y., Alvarez-Garcia O., Saito M., Caramés B., Iwamoto Y., Lotz M. K. FOXO transcription factors support oxidative stress resistance in human chondrocytes. Arthritis & Rheumatology. 2014;66(12):3349–3358. doi: 10.1002/art.38868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gezginci-Oktayoglu S., Sacan O., Bolkent S., et al. Chard (Beta vulgaris L. var. cicla) extract ameliorates hyperglycemia by increasing GLUT2 through Akt2 and antioxidant defense in the liver of rats. Acta Histochemica. 2014;116(1):32–39. doi: 10.1016/j.acthis.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 20.Li R.-P., Wang Z.-Z., Sun M.-X., et al. Polydatin protects learning and memory impairments in a rat model of vascular dementia. Phytomedicine. 2012;19(8-9):677–681. doi: 10.1016/j.phymed.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Mao X.-Y., Cao D.-F., Li X., et al. Huperzine A ameliorates cognitive deficits in streptozotocin-induced diabetic rats. International Journal of Molecular Sciences. 2014;15(5):7667–7683. doi: 10.3390/ijms15057667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moghaddasi M., Javanmard S. H., Reisi P., Tajadini M., Taati M. The effect of regular exercise on antioxidant enzyme activities and lipid peroxidation levels in both hippocampi after occluding one carotid in rat. Journal of Physiological Sciences. 2014;64(5):325–332. doi: 10.1007/s12576-014-0322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muley M. M., Thakare V. N., Patil R. R., Kshirsagar A. D., Naik S. R. Silymarin improves the behavioural, biochemical and histoarchitecture alterations in focal ischemic rats: a comparative evaluation with piracetam and protocatachuic acid. Pharmacology Biochemistry and Behavior. 2012;102(2):286–293. doi: 10.1016/j.pbb.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Srivastava A., Shivanandappa T. Prevention of hexachlorocyclohexane-induced neuronal oxidative stress by natural antioxidants. Nutritional Neuroscience. 2014;17(4):164–171. doi: 10.1179/1476830513y.0000000075. [DOI] [PubMed] [Google Scholar]
- 25.Vishwas D. K., Mukherjee A., Haldar C., Dash D., Nayak M. K. Improvement of oxidative stress and immunity by melatonin: an age dependent study in golden hamster. Experimental Gerontology. 2013;48(2):168–182. doi: 10.1016/j.exger.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Zhou Q., Liu C., Liu W., et al. Rotenone induction of hydrogen peroxide inhibits mTOR-mediated S6K and 4E-BP1/eIF4E pathways, leading to neuronal apoptosis. Toxicological Sciences. 2014;143(1):81–96. doi: 10.1093/toxsci/kfu211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim K. A., Shin Y. J., Akram M., et al. High glucose condition induces autophagy in endothelial progenitor cells contributing to angiogenic impairment. Biological and Pharmaceutical Bulletin. 2014;37(7):1248–1252. doi: 10.1248/bpb.b14-00172. [DOI] [PubMed] [Google Scholar]
- 28.Liu Y., Shi S., Gu Z., et al. Impaired autophagic function in rat islets with aging. Age. 2013;35(5):1531–1544. doi: 10.1007/s11357-012-9456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maiese K., Chong Z. Z., Shang Y. C., Wang S. Novel directions for diabetes mellitus drug discovery. Expert Opinion on Drug Discovery. 2013;8(1):35–48. doi: 10.1517/17460441.2013.736485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakka V. P., Prakash-babu P., Vemuganti R. Crosstalk between endoplasmic reticulum stress, oxidative stress, and autophagy: potential therapeutic targets for acute CNS injuries. Molecular Neurobiology. 2014 doi: 10.1007/s12035-014-9029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang H., Duan C., Yang H. Defective autophagy in Parkinson's disease: lessons from genetics. Molecular Neurobiology. 2015;51(1):89–104. doi: 10.1007/s12035-014-8787-5. [DOI] [PubMed] [Google Scholar]
- 32.Fong Y., Lin Y., Wu C., et al. The antiproliferative and apoptotic effects of sirtinol, a sirtuin inhibitor on human lung cancer cells by modulating Akt/beta-catenin-Foxo3a axis. The Scientific World Journal. 2014;2014:8. doi: 10.1155/2014/937051.937051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guo X., Chen Y., Liu Q., et al. Ac-cel, a novel antioxidant, protects against hydrogen peroxide-induced injury in PC12 cells via attenuation of mitochondrial dysfunction. Journal of Molecular Neuroscience. 2013;50(3):453–461. doi: 10.1007/s12031-013-9955-1. [DOI] [PubMed] [Google Scholar]
- 34.Maiese K., Chong Z. Z., Shang Y. C., Wang S. Targeting disease through novel pathways of apoptosis and autophagy. Expert Opinion on Therapeutic Targets. 2012;16(12):1203–1214. doi: 10.1517/14728222.2012.719499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schutters K., Reutelingsperger C. Phosphatidylserine targeting for diagnosis and treatment of human diseases. Apoptosis. 2010;15(9):1072–1082. doi: 10.1007/s10495-010-0503-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wei L., Sun C., Lei M., et al. Activation of Wnt/beta-catenin pathway by exogenous Wnt1 protects SH-SY5Y cells against 6-hydroxydopamine toxicity. Journal of Molecular Neuroscience. 2013;49(1):105–115. doi: 10.1007/s12031-012-9900-8. [DOI] [PubMed] [Google Scholar]
- 37.Williams C. J., Dexter D. T. Neuroprotective and symptomatic effects of targeting group III mGlu receptors in neurodegenerative disease. Journal of Neurochemistry. 2014;129(1):4–20. doi: 10.1111/jnc.12608. [DOI] [PubMed] [Google Scholar]
- 38.Zhao Z. C., Li F., Maiese K. Attempted cell cycle induction in post-mitotic neurons occurs in early and late apoptotic programs through Rb, E2F1, and caspase 3. Current Neurovascular Research. 2006;3(1):25–39. doi: 10.2174/156720206775541741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Favaloro B., Allocati N., Graziano V., di Ilio C., de Laurenzi V. Role of apoptosis in disease. Aging. 2012;4(5):330–349. doi: 10.18632/aging.100459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Folch J., Junyent F., Verdaguer E., et al. Role of cell cycle re-entry in neurons: a common apoptotic mechanism of neuronal cell death. Neurotoxicity Research. 2012;22(3):195–207. doi: 10.1007/s12640-011-9277-4. [DOI] [PubMed] [Google Scholar]
- 41.Nguyen A. Q., Cherry B. H., Scott G. F., Ryou M. G., Mallet R. T. Erythropoietin: powerful protection of ischemic and post-ischemic brain. Experimental Biology and Medicine. 2014;239(11):1461–1475. doi: 10.1177/1535370214523703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shao S., Yang Y., Yuan G., Zhang M., Yu X. Signaling molecules involved in lipid-induced pancreatic beta-cell dysfunction. DNA and Cell Biology. 2013;32(2):41–49. doi: 10.1089/dna.2012.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cai Z., Yan L. J. Rapamycin, autophagy, and Alzheimer's disease. Journal of Biochemical and Pharmacological Research. 2013;1(2):84–90. [PMC free article] [PubMed] [Google Scholar]
- 44.Chen W., Sun Y., Liu K., Sun X. Autophagy: a double-edged sword for neuronal survival after cerebral ischemia. Neural Regeneration Research. 2014;9(12):p. 1210. doi: 10.4103/1673-5374.135329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen Y., Liu X., Yin Y., et al. Unravelling the multifaceted roles of Atg proteins to improve cancer therapy. Cell Proliferation. 2014;47(2):105–112. doi: 10.1111/cpr.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.He C., Zhu H., Li H., Zou M.-H., Xie Z. Dissociation of Bcl-2-Beclin1 complex by activated AMPK enhances cardiac autophagy and protects against cardiomyocyte apoptosis in diabetes. Diabetes. 2013;62(4):1270–1281. doi: 10.2337/db12-0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lim Y., Lim H., Hur K. Y., et al. Systemic autophagy insufficiency compromises adaptation to metabolic stress and facilitates progression from obesity to diabetes. Nature Communications. 2014;5:p. 4934. doi: 10.1038/ncomms5934. [DOI] [PubMed] [Google Scholar]
- 48.Maiese K. Programming apoptosis and autophagy with novel approaches for diabetes mellitus. Current Neurovascular Research. 2015;12(2):173–188. doi: 10.2174/1567202612666150305110929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vakifahmetoglu-Norberg H., Xia H., Yuan J. Pharmacologic agents targeting autophagy. Journal of Clinical Investigation. 2015;125(1):5–13. doi: 10.1172/jci73937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization. Global Status Report on Noncommunicable Diseases 2010. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 51.Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. Atlanta, Ga, USA: US Department of Health and Human Services; 2014. [Google Scholar]
- 52.Esser N., Paquot N., Scheen A. J. Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert Opinion on Investigational Drugs. 2015;24(3):283–307. doi: 10.1517/13543784.2015.974804. [DOI] [PubMed] [Google Scholar]
- 53.Maiese K. Diabetic stress: new triumphs and challenges to maintain vascular longevity. Expert Review of Cardiovascular Therapy. 2008;6(3):281–284. doi: 10.1586/14779072.6.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Centers for Medicare and Medicaid Services. National Health Expenditure Projections 2012–2022. Centers for Medicare and Medicaid Services; 2013. http://www.cms.gov. [PubMed] [Google Scholar]
- 55.Harrison I. F., Dexter D. T. Epigenetic targeting of histone deacetylase: therapeutic potential in Parkinson's disease? Pharmacology and Therapeutics. 2013;140(1):34–52. doi: 10.1016/j.pharmthera.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 56.Maiese K. Epigenetics in the cerebrovascular system: changing the code without altering the sequence. Current Neurovascular Research. 2014;11(1):1–3. doi: 10.2174/1567202610999131204122451. [DOI] [PubMed] [Google Scholar]
- 57.Teschendorff A. E., West J., Beck S. Age-associated epigenetic drift: implications, and a case of epigenetic thrift? Human Molecular Genetics. 2013;22(R1):R7–R15. doi: 10.1093/hmg/ddt375.ddt375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.West J., Beck S., Wang X., Teschendorff A. E. An integrative network algorithm identifies age-associated differential methylation interactome hotspots targeting stem-cell differentiation pathways. Scientific Reports. 2013;3, article 1630 doi: 10.1038/srep01630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xiao F. H., He Y. H., Li Q. G., Wu H., Luo L. H., Kong Q. P. A genome-wide scan reveals important roles of DNA methylation in human longevity by regulating age-related disease genes. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0120388.e0120388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maiese K., Chong Z. Z., Shang Y. C., Hou J. Novel avenues of drug discovery and biomarkers for diabetes mellitus. Journal of Clinical Pharmacology. 2011;51(2):128–152. doi: 10.1177/0091270010362904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jia G., Aroor A. R., Martinez-Lemus L. A., Sowers J. R. Invited review: over-nutrition, mTOR signaling and cardiovascular diseases. The American Journal of Physiology—Regulatory, Integrative and Comparative Physiology. 2014 doi: 10.1152/ajpregu.00262.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rutter M. K., O'Donnell C. J., Massaro J. M., Fox C. S., Hoffmann U. Fasting glucose, obesity, and coronary artery calcification in community-based people without diabetes. Diabetes Care. 2012;35(9):1944–1950. doi: 10.2337/dc11-1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu E., Schwab M., Marette A. Role of protein tyrosine phosphatases in the modulation of insulin signaling and their implication in the pathogenesis of obesity-linked insulin resistance. Reviews in Endocrine and Metabolic Disorders. 2014;15(1):79–97. doi: 10.1007/s11154-013-9282-4. [DOI] [PubMed] [Google Scholar]
- 64.Himmetoglu S., Teksoz S., Zengin K., Yesim T., Taskn M., Dincer Y. Serum levels of fetuin a and 8-hydroxydeoxyguanosine in morbidly obese subjects. Experimental and Clinical Endocrinology and Diabetes. 2013;121(8):505–508. doi: 10.1055/s-0033-1345162. [DOI] [PubMed] [Google Scholar]
- 65.Liu Y., Palanivel R., Rai E., et al. Adiponectin stimulates autophagy and reduces oxidative stress to enhance insulin sensitivity during high fat diet feeding in mice. Diabetes. 2014;64(1):36–48. doi: 10.2337/db14-0267. [DOI] [PubMed] [Google Scholar]
- 66.Maiese K., Chong Z. Z., Shang Y. C., Wang S. Erythropoietin: new directions for the nervous system. International Journal of Molecular Sciences. 2012;13(9):11102–11129. doi: 10.3390/ijms130911102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Maiese K., Li F., Chong Z. Z. New avenues of exploration for erythropoietin. Journal of the American Medical Association. 2005;293(1):90–95. doi: 10.1001/jama.293.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.White M. F. IRS2 integrates insulin/IGF1 signalling with metabolism, neurodegeneration and longevity. Diabetes, Obesity and Metabolism. 2014;16(supplement 1):4–15. doi: 10.1111/dom.12347. [DOI] [PubMed] [Google Scholar]
- 69.Zhang Y., Wang L., Dey S., et al. Erythropoietin action in stress response, tissue maintenance and metabolism. International Journal of Molecular Sciences. 2014;15(6):10296–10333. doi: 10.3390/ijms150610296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chong Z. Z., Maiese K. The Src homology 2 domain tyrosine phosphatases SHP-1 and SHP-2: diversified control of cell growth, inflammation, and injury. Histology and Histopathology. 2007;22(11):1251–1267. doi: 10.14670/hh-22.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu Q., Li J., Cheng R., et al. Nitrosative stress plays an important role in wnt pathway activation in diabetic retinopathy. Antioxidants and Redox Signaling. 2013;18(10):1141–1153. doi: 10.1089/ars.2012.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou J., Wu J., Zheng F., Jin M., Li H. Glucagon-like peptide-1 analog-mediated protection against cholesterol-induced apoptosis via mammalian target of rapamycin activation in pancreatic betaTC-6 cells. Journal of Diabetes. 2015;7(2):231–239. doi: 10.1111/1753-0407.12177. [DOI] [PubMed] [Google Scholar]
- 73.Zhao Y., Scott N. A., Fynch S., et al. Autoreactive T cells induce necrosis and not BCL-2-regulated or death receptor-mediated apoptosis or RIPK3-dependent necroptosis of transplanted islets in a mouse model of type 1 diabetes. Diabetologia. 2015;58(1):140–148. doi: 10.1007/s00125-014-3407-5. [DOI] [PubMed] [Google Scholar]
- 74.Pietropaolo M., Barinas-Mitchell E., Pietropaolo S. L., Kuller L. H., Trucco M. Evidence of islet cell autoimmunity in elderly patients with type 2 diabetes. Diabetes. 2000;49(1):32–38. doi: 10.2337/diabetes.49.1.32. [DOI] [PubMed] [Google Scholar]
- 75.Kapogiannis D., Boxer A., Schwartz J. B., et al. Dysfunctionally phosphorylated type 1 insulin receptor substrate in neural-derived blood exosomes of preclinical Alzheimer's disease. The FASEB Journal. 2015;29(2):589–596. doi: 10.1096/fj.14-262048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maiese K., Morhan S. D., Zhao Z. C. Oxidative stress biology and cell injury during Type 1 and Type 2 diabetes mellitus. Current Neurovascular Research. 2007;4(1):63–71. doi: 10.2174/156720207779940653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Orchard T. J., Olson J. C., Erbey J. R., et al. Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh epidemiology of diabetes complications study. Diabetes Care. 2003;26(5):1374–1379. doi: 10.2337/diacare.26.5.1374. [DOI] [PubMed] [Google Scholar]
- 78.Chong Z. Z., Hou J., Shang Y. C., Wang S., Maiese K. EPO relies upon novel signaling of Wnt1 that requires Akt1, FoxO3a, GSK-3β, and βcatenin to foster vascular integrity during experimental diabetes. Current Neurovascular Research. 2011;8(2):103–120. doi: 10.2174/156720211795495402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhao Z. C., Yan C. S., Maiese K. Vascular injury during elevated glucose can be mitigated by erythropoietin and Wnt signaling. Current Neurovascular Research. 2007;4(3):194–204. doi: 10.2174/156720207781387150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hou J., Chong Z. Z., Shang Y. C., Maiese K. FOXO3a governs early and late apoptotic endothelial programs during elevated glucose through mitochondrial and caspase signaling. Molecular and Cellular Endocrinology. 2010;321(2):194–206. doi: 10.1016/j.mce.2010.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schaffer S. W., Jong C. J., Mozaffari M. Role of oxidative stress in diabetes-mediated vascular dysfunction: unifying hypothesis of diabetes revisited. Vascular Pharmacology. 2012;57(5-6):139–149. doi: 10.1016/j.vph.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 82.Wang L., Di L., Noguchi C. T. Erythropoietin, a novel versatile player regulating energy metabolism beyond the erythroid system. International Journal of Biological Sciences. 2014;10(8):921–939. doi: 10.7150/ijbs.9518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Arunachalam G., Samuel S. M., Marei I., Ding H., Triggle C. R. Metformin modulates hyperglycaemia-induced endothelial senescence and apoptosis through SIRT1. British Journal of Pharmacology. 2014;171(2):523–535. doi: 10.1111/bph.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen J.-X., Tuo Q., Liao D.-F., Zeng H. Inhibition of protein tyrosine phosphatase improves angiogenesis via enhancing Ang-1/Tie-2 signaling in diabetes. Experimental Diabetes Research. 2012;2012:10. doi: 10.1155/2012/836759.836759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barthelmes D., Zhu L., Shen W., Gillies M. C., Irhimeh M. R. Differential gene expression in Lin-/VEGF-R2+ bone marrow-derived endothelial progenitor cells isolated from diabetic mice. Cardiovascular Diabetology. 2014;13(1, article 42) doi: 10.1186/1475-2840-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Busch S., Kannt A., Kolibabka M., et al. Systemic treatment with erythropoietin protects the neurovascular unit in a rat model of retinal neurodegeneration. PLoS ONE. 2014;9(7) doi: 10.1371/journal.pone.0102013.e102013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Alexandru N., Popov D., Georgescu A. Platelet dysfunction in vascular pathologies and how can it be treated. Thrombosis Research. 2012;129(2):116–126. doi: 10.1016/j.thromres.2011.09.026. [DOI] [PubMed] [Google Scholar]
- 88.Gomes M., Negrato C. Alpha-lipoic acid as a pleiotropic compound with potential therapeutic use in diabetes and other chronic diseases. Diabetology & Metabolic Syndrome. 2014;6(1):p. 80. doi: 10.1186/1758-5996-6-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hu P., Lai D., Lu P., Gao J., He H. ERK and Akt signaling pathways are involved in advanced glycation end product-induced autophagy in rat vascular smooth muscle cells. International Journal of Molecular Medicine. 2012;29(4):613–618. doi: 10.3892/ijmm.2012.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aragno M., Mastrocola R., Ghé C., et al. Obestatin induced recovery of myocardial dysfunction in type 1 diabetic rats: underlying mechanisms. Cardiovascular Diabetology. 2012;11, article 129 doi: 10.1186/1475-2840-11-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chong Z. Z., Maiese K. Mammalian target of rapamycin signaling in diabetic cardiovascular disease. Cardiovascular Diabetology. 2012;11, article 45 doi: 10.1186/1475-2840-11-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Das A., Durrant D., Koka S., Salloum F. N., Xi L., Kukreja R. C. Mammalian target of rapamycin (mTOR) inhibition with rapamycin improves cardiac function in type 2 diabetic mice: potential role of attenuated oxidative stress and altered contractile protein expression. The Journal of Biological Chemistry. 2014;289(7):4145–4160. doi: 10.1074/jbc.m113.521062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ling S., Birnbaum Y., Nanhwan M. K., et al. Dickkopf-1 (DKK1) phosphatase and tensin homolog on chromosome 10 (PTEN) crosstalk via microRNA interference in the diabetic heart. Basic Research in Cardiology. 2013;108(3, article 352) doi: 10.1007/s00395-013-0352-2. [DOI] [PubMed] [Google Scholar]
- 94.Maiese K., Chong Z. Z., Shang Y. C., Hou J. FoxO proteins: cunning concepts and considerations for the cardiovascular system. Clinical Science. 2009;116(3):191–203. doi: 10.1042/cs20080113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Maiese K., Hou J., Chong Z. Z., Shang Y. C. A fork in the path: developing therapeutic inroads with FoxO proteins. Oxidative Medicine and Cellular Longevity. 2009;2(3):119–129. doi: 10.4161/oxim.2.3.8916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Portbury A. L., Ronnebaum S. M., Zungu M., Patterson C., Willis M. S. Back to your heart: ubiquitin proteasome system-regulated signal transduction. Journal of Molecular and Cellular Cardiology. 2012;52(3):526–537. doi: 10.1016/j.yjmcc.2011.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang C., Zhang L., Chen S., et al. The prevention of diabetic cardiomyopathy by non-mitogenic acidic fibroblast growth factor is probably mediated by the suppression of Oxidative stress and damage. PLoS ONE. 2013;8(12) doi: 10.1371/journal.pone.0082287.e82287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Coca S. G., Ismail-Beigi F., Haq N., Krumholz H. M., Parikh C. R. Role of intensive glucose control in development of renal end points in type 2 diabetes mellitus: systematic review and meta-analysis. Archives of Internal Medicine. 2012;172(10):761–769. doi: 10.1001/archinternmed.2011.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hao J., Li F., Liu W., et al. Phosphorylation of PRAS40-Thr246 involved in renal lipid accumulation of diabetes. Journal of Cellular Physiology. 2014;229(8):1069–1077. doi: 10.1002/jcp.24533. [DOI] [PubMed] [Google Scholar]
- 100.Hao J., Zhu L., Li F., et al. Phospho-mTOR: a novel target in regulation of renal lipid metabolism abnormality of diabetes. Experimental Cell Research. 2013;319(14):2296–2306. doi: 10.1016/j.yexcr.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 101.Kashihara N., Haruna Y., Kondeti V. K., Kanwar Y. S. Oxidative stress in diabetic nephropathy. Current Medicinal Chemistry. 2010;17(34):4256–4269. doi: 10.2174/092986710793348581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hamed S., Bennett C. L., Demiot C., Ullmann Y., Teot L., Desmoulière A. Erythropoietin, a novel repurposed drug: an innovative treatment for wound healing in patients with diabetes mellitus. Wound Repair and Regeneration. 2014;22(1):23–33. doi: 10.1111/wrr.12135. [DOI] [PubMed] [Google Scholar]
- 103.Hao J., Shen W., Tian C., et al. Mitochondrial nutrients improve immune dysfunction in the type 2 diabetic Goto-Kakizaki rats. Journal of Cellular and Molecular Medicine. 2009;13(4):701–711. doi: 10.1111/j.1582-4934.2008.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.John C. M., Ramasamy R., Al Naqeeb G., Al-Nuaimi A. H. D., Adam A. Enhanced CD4+CD25+ regulatory T cells with splenic proliferation and protection against oxidative stress by nicotinamide in gestational diabetes. Current Medicinal Chemistry. In press. [PubMed] [Google Scholar]
- 105.Maiese K., Chong Z. Z., Shang Y. C., Wang S. Translating cell survival and cell longevity into treatment strategies with SIRT1. Romanian Journal of Morphology and Embryology. 2011;52(4):1173–1185. [PMC free article] [PubMed] [Google Scholar]
- 106.Gao Z., Zhang J., Kheterpal I., Kennedy N., Davis R. J., Ye J. Sirtuin 1 (SIRT1) protein degradation in response to persistent c-Jun N-terminal Kinase 1 (JNK1) activation contributes to hepatic steatosis in obesity. Journal of Biological Chemistry. 2011;286(25):22227–22234. doi: 10.1074/jbc.M111.228874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kousteni S. FoxO1, the transcriptional chief of staff of energy metabolism. Bone. 2012;50(2):437–443. doi: 10.1016/j.bone.2011.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Li Y., Xu S., Giles A., et al. Hepatic overexpression of SIRT1 in mice attenuates endoplasmic reticulum stress and insulin resistance in the liver. The FASEB Journal. 2011;25(5):1664–1679. doi: 10.1096/fj.10-173492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Singh A. B., Singh N., Akanksha, Jayendra, Maurya R., Srivastava A. K. Coagulanolide modulates hepatic glucose metabolism in C57BL/KsJ-db/db mice. Human and Experimental Toxicology. 2012;31(10):1056–1065. doi: 10.1177/0960327112438289. [DOI] [PubMed] [Google Scholar]
- 110.Jiang T., Yu J., Zhu X., et al. Acute metformin preconditioning confers neuroprotection against focal cerebral ischaemia by pre-activation of AMPK-dependent autophagy. British Journal of Pharmacology. 2014;171(13):3146–3157. doi: 10.1111/bph.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Maiese K., Zhao Z. C., Hou J., Yan C. S. Erythropoietin and oxidative stress. Current Neurovascular Research. 2008;5(2):125–142. doi: 10.2174/156720208784310231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Du L.-L., Chai D.-M., Zhao L.-N., et al. AMPK activation ameliorates Alzheimer's disease-like pathology and spatial memory impairment in a streptozotocin-induced Alzheimer's disease model in rats. Journal of Alzheimer's Disease. 2015;43(3):775–784. doi: 10.3233/JAD-140564. [DOI] [PubMed] [Google Scholar]
- 113.Maiese K., Chong Z. Z., Shang Y. C. Raves and risks for erythropoietin. Cytokine and Growth Factor Reviews. 2008;19(2):145–155. doi: 10.1016/j.cytogfr.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aksu I., Ates M., Baykara B., et al. Anxiety correlates to decreased blood and prefrontal cortex IGF-1 levels in streptozotocin induced diabetes. Neuroscience Letters. 2012;531(2):176–181. doi: 10.1016/j.neulet.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 115.Reagan L. P. Diabetes as a chronic metabolic stressor: causes, consequences and clinical complications. Experimental Neurology. 2012;233(1):68–78. doi: 10.1016/j.expneurol.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fu D., Wu M., Zhang J., et al. Mechanisms of modified LDL-Induced pericyte loss and retinal injury in diabetic retinopathy. Diabetologia. 2012;55(11):3128–3140. doi: 10.1007/s00125-012-2692-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lee K., Hu Y., Ding L., et al. Therapeutic potential of a monoclonal antibody blocking the Wnt pathway in diabetic retinopathy. Diabetes. 2012;61(11):2948–2957. doi: 10.2337/db11-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Maiese K. Novel applications of trophic factors, Wnt and WISP for neuronal repair and regeneration in metabolic disease. Neural Regeneration Research. 2015;10(4):518–528. doi: 10.4103/1673-5374.155427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bagul P. K., Banerjee S. K. Insulin resistance, oxidative stress and cardiovascular complications: role of sirtuins. Current Pharmaceutical Design. 2013;19(32):5663–5677. doi: 10.2174/13816128113199990372. [DOI] [PubMed] [Google Scholar]
- 120.Liu J., Li J., Li W.-J., Wang C.-M. The role of uncoupling proteins in diabetes mellitus. Journal of Diabetes Research. 2013;2013:7. doi: 10.1155/2013/585897.585897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Peng Y., Huang S., Cheng B., et al. Mesenchymal stem cells: a revolution in therapeutic strategies of age-related diseases. Ageing Research Reviews. 2013;12(1):103–115. doi: 10.1016/j.arr.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 122.Weinberg E., Maymon T., Weinreb M. AGEs induce caspase-mediated apoptosis of rat BMSCs via TNFalpha production and oxidative stress. Journal of Molecular Endocrinology. 2014;52(1):67–76. doi: 10.1530/jme-13-0229. [DOI] [PubMed] [Google Scholar]
- 123.Yang H., Jin X., Lam C. W. K., Yan S.-K. Oxidative stress and diabetes mellitus. Clinical Chemistry and Laboratory Medicine. 2011;49(11):1773–1782. doi: 10.1515/CCLM.2011.250. [DOI] [PubMed] [Google Scholar]
- 124.Kurban S., Mehmetoglu I., Yerlikaya H. F., Gönen S., Erdem S. Effect of chronic regular exercise on serum ischemia-modified albumin levels and oxidative stress in type 2 diabetes mellitus. Endocrine Research. 2011;36(3):116–123. doi: 10.3109/07435800.2011.566236. [DOI] [PubMed] [Google Scholar]
- 125.Monnier L., Mas E., Ginet C., et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. Journal of the American Medical Association. 2006;295(14):1681–1687. doi: 10.1001/jama.295.14.1681. [DOI] [PubMed] [Google Scholar]
- 126.Lee Y., Hong Y., Lee S. R., Chang K. T. Autophagy contributes to retardation of cardiac growth in diabetic rats. Laboratory Animal Research. 2012;28(2):99–107. doi: 10.5625/lar.2012.28.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hou J., Chong Z. Z., Shang Y. C., Maiese K. Early apoptotic vascular signaling is determined by Sirt1 through nuclear shuttling, forkhead trafficking, bad, and mitochondrial caspase activation. Current Neurovascular Research. 2010;7(2):95–112. doi: 10.2174/156720210791184899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Das F., Dey N., Venkatesan B., Kasinath B. S., Ghosh-Choudhury N., Choudhury G. G. High glucose upregulation of early-onset Parkinson's disease protein DJ-1 integrates the PRAS40/TORC1 axis to mesangial cell hypertrophy. Cellular Signalling. 2011;23(8):1311–1319. doi: 10.1016/j.cellsig.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhao Z., Huang G., Wang B., Zhong Y. Inhibition of NF-kappaB activation by Pyrrolidine dithiocarbamate partially attenuates hippocampal MMP-9 activation and improves cognitive deficits in streptozotocin-induced diabetic rats. Behavioural Brain Research. 2013;238(1):44–47. doi: 10.1016/j.bbr.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 130.Zhang B.-C., Li W.-M., Zhu M.-Y., Xu Y.-W. Association of TCF7L2 gene polymorphisms with type 2 diabetes mellitus in Han Chinese population: a meta-analysis. Gene. 2013;512(1):76–81. doi: 10.1016/j.gene.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 131.Criscuolo F., Mozo J., Hurtaud C., Nübel T., Bouillaud F. UCP2, UCP3, avUCP, what do they do when proton transport is not stimulated? Possible relevance to pyruvate and glutamine metabolism. Biochimica et Biophysica Acta. 2006;1757(9-10):1284–1291. doi: 10.1016/j.bbabio.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 132.Li B., Nolte L. A., Ju J.-S., et al. Skeletal muscle respiratory uncoupling prevents diet-induced obesity and insulin resistance in mice. Nature Medicine. 2000;6(10):1115–1120. doi: 10.1038/80450. [DOI] [PubMed] [Google Scholar]
- 133.Bernal-Mizrachi C., Weng S., Li B., et al. Respiratory uncoupling lowers blood pressure through a leptin-dependent mechanism in genetically obese mice. Arteriosclerosis, Thrombosis, and Vascular Biology. 2002;22(6):961–968. doi: 10.1161/01.ATV.0000019404.65403.71. [DOI] [PubMed] [Google Scholar]
- 134.Huppertz C., Fischer B. M., Kim Y.-B., et al. Uncoupling protein 3 (UCP3) stimulates glucose uptake in muscle cells through a phosphoinositide 3-kinase-dependent mechanism. The Journal of Biological Chemistry. 2001;276(16):12520–12529. doi: 10.1074/jbc.m011708200. [DOI] [PubMed] [Google Scholar]
- 135.Darcy MacLellan J., Gerrits M. F., Gowing A., Smith P. J. S., Wheeler M. B., Harper M.-E. Physiological increases in uncoupling protein 3 augment fatty acid oxidation and decrease reactive oxygen species production without uncoupling respiration in muscle cells. Diabetes. 2005;54(8):2343–2350. doi: 10.2337/diabetes.54.8.2343. [DOI] [PubMed] [Google Scholar]
- 136.Zhang C.-Y., Baffy G., Perret P., et al. Uncoupling protein-2 negatively regulates insulin secretion and is a major link between obesity, β cell dysfunction, and type 2 diabetes. Cell. 2001;105(6):745–755. doi: 10.1016/s0092-8674(01)00378-6. [DOI] [PubMed] [Google Scholar]
- 137.Pérez-Gallardo R. V., Noriega-Cisneros R., Esquivel-Gutiérrez E., et al. Effects of diabetes on oxidative and nitrosative stress in kidney mitochondria from aged rats. Journal of Bioenergetics and Biomembranes. 2014;46(6):511–518. doi: 10.1007/s10863-014-9594-4. [DOI] [PubMed] [Google Scholar]
- 138.Zhang X., Dong S., Qin Y., Bian X. Protective effect of erythropoietin against myocardial injury in rats with sepsis and its underlying mechanisms. Molecular Medicine Reports. 2015;11(5):3317–3329. doi: 10.3892/mmr.2015.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kelley D. E., He J., Menshikova E. V., Ritov V. B. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes. 2002;51(10):2944–2950. doi: 10.2337/diabetes.51.10.2944. [DOI] [PubMed] [Google Scholar]
- 140.Choo H.-J., Kim J.-H., Kwon O.-B., et al. Mitochondria are impaired in the adipocytes of type 2 diabetic mice. Diabetologia. 2006;49(4):784–791. doi: 10.1007/s00125-006-0170-2. [DOI] [PubMed] [Google Scholar]
- 141.Liu Z., Stanojevic V., Brindamour L. J., Habener J. F. GLP1-derived nonapeptide GLP1(28-36)amide protects pancreatic beta-cells from glucolipotoxicity. Journal of Endocrinology. 2012;213(2):143–154. doi: 10.1530/joe-11-0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Noriega-Cisneros R., Cortés-Rojo C., Manzo-Avalos S., et al. Mitochondrial response to oxidative and nitrosative stress in early stages of diabetes. Mitochondrion. 2013;13(6):835–840. doi: 10.1016/j.mito.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 143.Damasceno D. C., Sinzato Y. K., Bueno A., et al. Mild diabetes models and their maternal-fetal repercussions. Journal of Diabetes Research. 2013;2013:9. doi: 10.1155/2013/473575.473575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Maiese K., Chong Z. Z., Hou J., Shang Y. C. Oxidative stress: biomarkers and novel therapeutic pathways. Experimental Gerontology. 2010;45(3):217–234. doi: 10.1016/j.exger.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yamada E., Singh R. Mapping autophagy on to your metabolic radar. Diabetes. 2012;61(2):272–280. doi: 10.2337/db11-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Maiese K. Taking aim at Alzheimer's disease through the mammalian target of rapamycin. Annals of Medicine. 2014;46(8):587–596. doi: 10.3109/07853890.2014.941921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Choi D., Schroer S. A., Lu S. Y., et al. Erythropoietin protects against diabetes through direct effects on pancreatic beta cells. The Journal of Experimental Medicine. 2010;207(13):2831–2842. doi: 10.1084/jem.20100665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Deng X., Cheng J., Zhang Y., Li N., Chen L. Effects of caloric restriction on SIRT1 expression and apoptosis of islet beta cells in type 2 diabetic rats. Acta Diabetologica. 2010;47(1):S177–S185. doi: 10.1007/s00592-009-0159-7. [DOI] [PubMed] [Google Scholar]
- 149.Miao X.-Y., Gu Z.-Y., Liu P., et al. The human glucagon-like peptide-1 analogue liraglutide regulates pancreatic beta-cell proliferation and apoptosis via an AMPK/mTOR/P70S6K signaling pathway. Peptides. 2013;39(1):71–79. doi: 10.1016/j.peptides.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 150.Hamed S., Ullmann Y., Egozi D., et al. Fibronectin potentiates topical erythropoietin-induced wound repair in diabetic mice. Journal of Investigative Dermatology. 2011;131(6):1365–1374. doi: 10.1038/jid.2011.15. [DOI] [PubMed] [Google Scholar]
- 151.Dang J., Jia R., Tu Y., Xiao S., Ding G. Erythropoietin prevents reactive oxygen species generation and renal tubular cell apoptosis at high glucose level. Biomedicine and Pharmacotherapy. 2010;64(10):681–685. doi: 10.1016/j.biopha.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 152.Nakazawa J., Isshiki K., Sugimoto T., et al. Renoprotective effects of asialoerythropoietin in diabetic mice against ischaemia-reperfusion-induced acute kidney injury. Nephrology. 2010;15(1):93–101. doi: 10.1111/j.1440-1797.2009.01170.x. [DOI] [PubMed] [Google Scholar]
- 153.Toba H., Sawai N., Morishita M., et al. Chronic treatment with recombinant human erythropoietin exerts renoprotective effects beyond hematopoiesis in streptozotocin-induced diabetic rat. European Journal of Pharmacology. 2009;612(1–3):106–114. doi: 10.1016/j.ejphar.2009.03.065. [DOI] [PubMed] [Google Scholar]
- 154.Kimura R., Okouchi M., Kato T., et al. Epidermal growth factor receptor transactivation is necessary for glucagon-like peptide-1 to protect PC12 cells from apoptosis. Neuroendocrinology. 2013;97(4):300–308. doi: 10.1159/000345529. [DOI] [PubMed] [Google Scholar]
- 155.Martino L., Masini M., Novelli M., et al. Palmitate activates autophagy in INS-1E β-cells and in isolated rat and human pancreatic islets. PLoS ONE. 2012;7(5) doi: 10.1371/journal.pone.0036188.e36188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lee J., Jin M., Han S., et al. Diet control to achieve euglycemia induces significant loss of heart and liver weight via increased autophagy compared with ad libitum diet in diabetic rats. Experimental & Molecular Medicine. 2014;46(8):p. e111. doi: 10.1038/emm.2014.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wang S., Chong Z. Z., Shang Y. C., Maiese K. WISP1 (CCN4) autoregulates its expression and nuclear trafficking of beta-catenin during oxidant stress with limited effects upon neuronal autophagy. Current Neurovascular Research. 2012;9(2):91–101. doi: 10.2174/156720212800410858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.He C., Bassik M. C., Moresi V., et al. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature. 2012;481(7382):511–515. doi: 10.1038/nature10758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Chong Z. Z., Shang Y. C., Maiese K. Cardiovascular disease and mTOR signaling. Trends in Cardiovascular Medicine. 2011;21(5):151–155. doi: 10.1016/j.tcm.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Johnson S. C., Sangesland M., Kaeberlein M., Rabinovitch P. S. Modulating mTOR in aging and health. Interdisciplinary Topics in Gerontology. 2015;40:107–127. doi: 10.1159/000364974. [DOI] [PubMed] [Google Scholar]
- 161.Maiese K. Cutting through the complexities of mTOR for the treatment of stroke. Current Neurovascular Research. 2014;11(2):177–186. doi: 10.2174/1567202611666140408104831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Neasta J., Barak S., Hamida S. B., Ron D. mTOR complex 1: a key player in neuroadaptations induced by drugs of abuse. Journal of Neurochemistry. 2014;130(2):172–184. doi: 10.1111/jnc.12725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Tang Z., Baykal A. T., Gao H., et al. MTor is a signaling hub in cell survival: a mass-spectrometry-based proteomics investigation. Journal of Proteome Research. 2014;13(5):2433–2444. doi: 10.1021/pr500192g. [DOI] [PubMed] [Google Scholar]
- 164.Chong Z. Z., Shang Y. C., Zhang L., Wang S., Maiese K. Mammalian target of rapamycin: hitting the bull's-eye for neurological disorders. Oxidative Medicine and Cellular Longevity. 2010;3(6):374–391. doi: 10.4161/oxim.3.6.14787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Maiese K., Chong Z. Z., Shang Y. C., Wang S. mTOR: on target for novel therapeutic strategies in the nervous system. Trends in Molecular Medicine. 2013;19(1):51–60. doi: 10.1016/j.molmed.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chong Z. Z., Shang Y. C., Wang S., Maiese K. Shedding new light on neurodegenerative diseases through the mammalian target of rapamycin. Progress in Neurobiology. 2012;99(2):128–148. doi: 10.1016/j.pneurobio.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kim J., Jung Y., Sun H., et al. Erythropoietin mediated bone formation is regulated by mTOR signaling. Journal of Cellular Biochemistry. 2012;113(1):220–228. doi: 10.1002/jcb.23347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Marfia G., Madaschi L., Marra F., et al. Adult neural precursors isolated from post mortem brain yield mostly neurons: an erythropoietin-dependent process. Neurobiology of Disease. 2011;43(1):86–98. doi: 10.1016/j.nbd.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 169.Sanghera K. P., Mathalone N., Baigi R., et al. The PI3K/Akt/mTOR pathway mediates retinal progenitor cell survival under hypoxic and superoxide stress. Molecular and Cellular Neuroscience. 2011;47(2):145–153. doi: 10.1016/j.mcn.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 170.Shang Y. C., Chong Z. Z., Wang S., Maiese K. Prevention of β-amyloid degeneration of microglia by erythropoietin depends on Wnt1, the PI 3-K/mTOR pathway, Bad, and Bcl-xL. Aging. 2012;4(3):187–201. doi: 10.18632/aging.100440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wang G.-B., Ni Y.-L., Zhou X.-P., Zhang W.-F. The AKT/mTOR pathway mediates neuronal protective effects of erythropoietin in sepsis. Molecular and Cellular Biochemistry. 2014;385(1-2):125–132. doi: 10.1007/s11010-013-1821-5. [DOI] [PubMed] [Google Scholar]
- 172.Wang H., Zhang Q., Wen Q., et al. Proline-rich Akt substrate of 40 kDa (PRAS40): a novel downstream target of PI3k/Akt signaling pathway. Cell Signal. 2012;24(1):17–24. doi: 10.1016/j.cellsig.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 173.Chong Z. Z., Kang J.-Q., Maiese K. Erythropoietin is a novel vascular protectant through activation of AKt1 and mitochondrial modulation of cysteine proteases. Circulation. 2002;106(23):2973–2979. doi: 10.1161/01.cir.0000039103.58920.1f. [DOI] [PubMed] [Google Scholar]
- 174.Chong Z. Z., Shang Y. C., Wang S., Maiese K. PRAS40 is an integral regulatory component of erythropoietin mTOR signaling and cytoprotection. PLoS ONE. 2012;7(9) doi: 10.1371/journal.pone.0045456.e45456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Shang Y. C., Chong Z. Z., Wang S., Maiese K. Erythropoietin and Wnt1 govern pathways of mTOR, Apaf-1, and XIAP in inflammatory microglia. Current Neurovascular Research. 2011;8(4):270–285. doi: 10.2174/156720211798120990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Maiese K. Driving neural regeneration through the mammalian target of rapamycin. Neural Regeneration Research. 2014;9(15):p. 1413. doi: 10.4103/1673-5374.139453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Gwinn D. M., Shackelford D. B., Egan D. F., et al. AMPK phosphorylation of raptor mediates a metabolic checkpoint. Molecular Cell. 2008;30(2):214–226. doi: 10.1016/j.molcel.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Sheng B., Liu J., Li G. H. Metformin preconditioning protects Daphnia pulex from lethal hypoxic insult involving AMPK, HIF and mTOR signaling. Comparative Biochemistry and Physiology B: Biochemistry and Molecular Biology. 2012;163(1):51–58. doi: 10.1016/j.cbpb.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 179.Xie Z., Lau K., Eby B., et al. Improvement of cardiac functions by chronic metformin treatment is associated with enhanced cardiac autophagy in diabetic OVE26 mice. Diabetes. 2011;60(6):1770–1778. doi: 10.2337/db10-0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ullah I., Ullah N., Naseer M. I., Lee H. Y., Kim M. O. K. Neuroprotection with metformin and thymoquinone against ethanol-induced apoptotic neurodegeneration in prenatal rat cortical neurons. BMC Neuroscience. 2012;13(1, article 11) doi: 10.1186/1471-2202-13-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Malaguarnera R., Sacco A., Morcavallo A., et al. Metformin inhibits androgen-induced IGF-IR up-regulation in prostate cancer cells by disrupting membrane-initiated androgen signaling. Endocrinology. 2014;155(4):1207–1221. doi: 10.1210/en.2013-1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zhu Z., Yan J., Jiang W., et al. Arctigenin effectively ameliorates memory impairment in Alzheimer's disease model mice targeting both β-amyloid production and clearance. Journal of Neuroscience. 2013;33(32):13138–13149. doi: 10.1523/jneurosci.4790-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cheng P.-W., Ho W.-Y., Su Y.-T., et al. Resveratrol decreases fructose-induced oxidative stress, mediated by NADPH oxidase via an AMPK-dependent mechanism. British Journal of Pharmacology. 2014;171(11):2739–2750. doi: 10.1111/bph.12648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Salminen A., Kaarniranta K., Haapasalo A., Soininen H., Hiltunen M. AMP-activated protein kinase: a potential player in Alzheimer's disease. Journal of Neurochemistry. 2011;118(4):460–474. doi: 10.1111/j.1471-4159.2011.07331.x. [DOI] [PubMed] [Google Scholar]
- 185.Shang Y. C., Chong Z. Z., Wang S., Maiese K. Tuberous sclerosis protein 2 (TSC2) modulates CCN4 cytoprotection during apoptotic amyloid toxicity in microglia. Current Neurovascular Research. 2013;10(1):29–38. doi: 10.2174/156720213804806007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kang S., Chemaly E. R., Hajjar R. J., Lebeche D. Resistin promotes cardiac hypertrophy via the AMP-activated protein kinase/mammalian target of rapamycin (AMPK/mTOR) and c-Jun N-terminal kinase/insulin receptor substrate 1 (JNK/IRS1) pathways. Journal of Biological Chemistry. 2011;286(21):18465–18473. doi: 10.1074/jbc.m110.200022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Russo E., Andreozzi F., Iuliano R., et al. Early molecular and behavioral response to lipopolysaccharide in the WAG/Rij rat model of absence epilepsy and depressive-like behavior, involves interplay between AMPK, AKT/mTOR pathways and neuroinflammatory cytokine release. Brain, Behavior, and Immunity. 2014;42:157–168. doi: 10.1016/j.bbi.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 188.Benyoucef A., Calvo J., Renou L., et al. The SCL/TAL1 transcription factor represses the stress protein DDiT4/REDD1 in human hematopoietic stem/progenitor cells. Stem Cells. 2015 doi: 10.1002/stem.2028. [DOI] [PubMed] [Google Scholar]
- 189.Hartman N. W., Lin T. V., Zhang L., Paquelet G. E., Feliciano D. M., Bordey A. mTORC1 targets the translational repressor 4E-BP2, but not S6 kinase 1/2, to regulate neural stem cell self-renewal in vivo. Cell Reports. 2013;5(2):433–444. doi: 10.1016/j.celrep.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 190.Ou X., Lee M. R., Huang X., Messina-Graham S., Broxmeyer H. E. SIRT1 positively regulates autophagy and mitochondria function in embryonic stem cells under oxidative stress. Stem Cells. 2014;32(5):1183–1194. doi: 10.1002/stem.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Pasini E., Flati V., Paiardi S., et al. Intracellular molecular effects of insulin resistance in patients with metabolic syndrome. Cardiovascular Diabetology. 2010;9, article 46 doi: 10.1186/1475-2840-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Peng N., Meng N., Wang S., et al. An activator of mTOR inhibits oxLDL-induced autophagy and apoptosis in vascular endothelial cells and restricts atherosclerosis in apolipoprotein E−/− mice. Scientific Reports. 2014;4, article 5519 doi: 10.1038/srep05519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Chong Z. Z., Shang Y. C., Wang S., Maiese K. SIRT1: new avenues of discovery for disorders of oxidative stress. Expert Opinion on Therapeutic Targets. 2012;16(2):167–178. doi: 10.1517/14728222.2012.648926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Oblong J. E. The evolving role of the NAD+/nicotinamide metabolome in skin homeostasis, cellular bioenergetics, and aging. DNA Repair. 2014;23:59–63. doi: 10.1016/j.dnarep.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 195.Patel S. A., Velingkaar N. S., Kondratov R. V. Transcriptional control of antioxidant defense by the circadian clock. Antioxidants and Redox Signaling. 2014;20(18):2997–3006. doi: 10.1089/ars.2013.5671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Albiero M., Poncina N., Tjwa M., et al. Diabetes causes bone marrow autonomic neuropathy and impairs stem cell mobilization via dysregulated p66Shc and Sirt1. Diabetes. 2014;63(4):1353–1365. doi: 10.2337/db13-0894. [DOI] [PubMed] [Google Scholar]
- 197.Caron A. Z., He X., Mottawea W., et al. The SIRT1 deacetylase protects mice against the symptoms of metabolic syndrome. The FASEB Journal. 2014;28(3):1306–1316. doi: 10.1096/fj.13-243568. [DOI] [PubMed] [Google Scholar]
- 198.Wang L., Teng R., Di L., et al. PPARalpha and Sirt1 mediate erythropoietin action in increasing metabolic activity and browning of white adipocytes to protect against obesity and metabolic disorders. Diabetes. 2013;62(12):4122–4131. doi: 10.2337/db13-0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gong H., Pang J., Han Y., et al. Age-dependent tissue expression patterns of Sirt1 in senescence-accelerated mice. Molecular Medicine Reports. 2014;10(6):3296–3302. doi: 10.3892/mmr.2014.2648. [DOI] [PubMed] [Google Scholar]
- 200.Hou J., Wang S., Shang Y. C., Chong Z. Z., Maiese K. Erythropoietin employs cell longevity pathways of SIRT1 to foster endothelial vascular integrity during oxidant stress. Current Neurovascular Research. 2011;8(3):220–235. doi: 10.2174/156720211796558069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Duan W. Sirtuins: from metabolic regulation to brain aging. Frontiers in Aging Neuroscience. 2013;5, article 36 doi: 10.3389/fnagi.2013.00036.article 36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Srivastava S., Haigis M. C. Role of sirtuins and calorie restriction in neuroprotection: implications in alzheimer's and parkinson's diseases. Current Pharmaceutical Design. 2011;17(31):3418–3433. doi: 10.2174/138161211798072526. [DOI] [PubMed] [Google Scholar]
- 203.Li F., Chong Z. Z., Maiese K. Cell life versus cell longevity: the mysteries surrounding the NAD+ precursor nicotinamide. Current Medicinal Chemistry. 2006;13(8):883–895. doi: 10.2174/092986706776361058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Chen S., Xiao X., Feng X., et al. Resveratrol induces Sirt1-dependent apoptosis in 3T3-L1 preadipocytes by activating AMPK and suppressing AKT activity and survivin expression. Journal of Nutritional Biochemistry. 2012;23(9):1100–1112. doi: 10.1016/j.jnutbio.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 205.Chong Z. Z., Wang S., Shang Y. C., Maiese K. Targeting cardiovascular disease with novel SIRT1 pathways. Future Cardiology. 2012;8(1):89–100. doi: 10.2217/fca.11.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Jin X., Chen M., Yi L., et al. Delphinidin-3-glucoside protects human umbilical vein endothelial cells against oxidized low-density lipoprotein-induced injury by autophagy upregulation via the AMPK/SIRT1 signaling pathway. Molecular Nutrition & Food Research. 2014;58(10):1941–1951. doi: 10.1002/mnfr.201400161. [DOI] [PubMed] [Google Scholar]
- 207.Maiese K., Chong Z. Z., Shang Y. C. OutFOXOing disease and disability: the therapeutic potential of targeting FoxO proteins. Trends in Molecular Medicine. 2008;14(5):219–227. doi: 10.1016/j.molmed.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Xiong S., Salazar G., Patrushev N., Alexander R. W. FoxO1 mediates an autofeedback loop regulating SIRT1 expression. Journal of Biological Chemistry. 2011;286(7):5289–5299. doi: 10.1074/jbc.M110.163667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Martin A., Tegla C. A., Cudrici C. D., et al. Role of SIRT1 in autoimmune demyelination and neurodegeneration. Immunologic Research. 2015;61(3):187–197. doi: 10.1007/s12026-014-8557-5. [DOI] [PubMed] [Google Scholar]
- 210.Czubak P., Bojarska-Junak A., Tabarkiewicz J., Putowski L. A modified method of insulin producing cells' generation from bone marrow-derived mesenchymal stem cells. Journal of Diabetes Research. 2014;2014:7. doi: 10.1155/2014/628591.628591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Schulz T. C., Young H. Y., Agulnick A. D., et al. A scalable system for production of functional pancreatic progenitors from human embryonic stem cells. PLoS ONE. 2012;7(5) doi: 10.1371/journal.pone.0037004.e37004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.De Bonis M. L., Ortega S., Blasco M. A. SIRT1 is necessary for proficient telomere elongation and genomic stability of induced pluripotent stem cells. Stem Cell Reports. 2014;2(5):690–706. doi: 10.1016/j.stemcr.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Chen J., Xavier S., Moskowitz-Kassai E., et al. Cathepsin cleavage of sirtuin 1 in endothelial progenitor cells mediates stress-induced premature senescence. The American Journal of Pathology. 2012;180(3):973–983. doi: 10.1016/j.ajpath.2011.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Mazzoccoli G., Tevy M. F., Borghesan M., Vergini M. R. D., Vinciguerra M. Caloric restriction and aging stem cells: the stick and the carrot? Experimental Gerontology. 2014;50(1):137–148. doi: 10.1016/j.exger.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 215.Tang A. H., Rando T. A. Induction of autophagy supports the bioenergetic demands of quiescent muscle stem cell activation. The EMBO Journal. 2014;33(23):2782–2797. doi: 10.15252/embj.201488278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Liu X., Chen H., Zhu W., et al. Transplantation of SIRT1-engineered aged mesenchymal stem cells improves cardiac function in a rat myocardial infarction model. The Journal of Heart and Lung Transplantation. 2014;33(10):1083–1092. doi: 10.1016/j.healun.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 217.Passariello C. L., Zini M., Nassi P. A., Pignatti C., Stefanelli C. Upregulation of SIRT1 deacetylase in phenylephrine-treated cardiomyoblasts. Biochemical and Biophysical Research Communications. 2011;407(3):512–516. doi: 10.1016/j.bbrc.2011.03.049. [DOI] [PubMed] [Google Scholar]
- 218.Balestrieri M. L., Servillo L., Esposito A., et al. Poor glycaemic control in type 2 diabetes patients reduces endothelial progenitor cell number by influencing SIRT1 signalling via platelet-activating factor receptor activation. Diabetologia. 2013;56(1):162–172. doi: 10.1007/s00125-012-2749-0. [DOI] [PubMed] [Google Scholar]
- 219.Lemarié C. A., Shbat L., Marchesi C., et al. Mthfr deficiency induces endothelial progenitor cell senescence via uncoupling of eNOS and downregulation of SIRT1. American Journal of Physiology—Heart and Circulatory Physiology. 2011;300(3):H745–H753. doi: 10.1152/ajpheart.00321.2010. [DOI] [PubMed] [Google Scholar]
- 220.Chiara B., Ilaria C., Antonietta C., et al. SIRT1 inhibition affects angiogenic properties of human MSCs. BioMed Research International. 2014;2014:12. doi: 10.1155/2014/783459.783459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Yuen D. A., Zhang Y., Thai K., et al. Angiogenic dysfunction in bone marrow-derived early outgrowth cells from diabetic animals is attenuated by SIRT1 activation. Stem Cells Translational Medicine. 2012;1(12):921–926. doi: 10.5966/sctm.2012-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Choudhery M. S., Khan M., Mahmood R., et al. Mesenchymal stem cells conditioned with glucose depletion augments their ability to repair-infarcted myocardium. Journal of Cellular and Molecular Medicine. 2012;16(10):2518–2529. doi: 10.1111/j.1582-4934.2012.01568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Saharan S., Jhaveri D. J., Bartlett P. F. SIRT1 regulates the neurogenic potential of neural precursors in the adult subventricular zone and hippocampus. Journal of Neuroscience Research. 2013;91(5):642–659. doi: 10.1002/jnr.23199. [DOI] [PubMed] [Google Scholar]
- 224.Liu D. J., Hammer D., Komlos D., Chen K. Y., Firestein B. L., Liu A. Y.-C. SIRT1 knockdown promotes neural differentiation and attenuates the heat shock response. Journal of Cellular Physiology. 2014;229(9):1224–1235. doi: 10.1002/jcp.24556. [DOI] [PubMed] [Google Scholar]
- 225.Zhang Y., Wang J., Chen G., Fan D., Deng M. Inhibition of Sirt1 promotes neural progenitors toward motoneuron differentiation from human embryonic stem cells. Biochemical and Biophysical Research Communications. 2011;404(2):610–614. doi: 10.1016/j.bbrc.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 226.AranhaMá M. M., Santos D. M., Solá S., Steer C. J., RodriguesCecí C. M. P. MiR-34a regulates mouse neural stem cell differentiation. PLoS ONE. 2011;6(8) doi: 10.1371/journal.pone.0021396.e21396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Wang R.-H., Kim H.-S., Xiao C., Xu X., Gavrilova O., Deng C.-X. Hepatic Sirt1 deficiency in mice impairs mTorc2/Akt signaling and results in hyperglycemia, oxidative damage, and insulin resistance. Journal of Clinical Investigation. 2011;121(11):4477–4490. doi: 10.1172/JCI46243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Guo R., Liu B., Wang K., Zhou S., Li W., Xu Y. Resveratrol ameliorates diabetic vascular inflammation and macrophage infiltration in db/db mice by inhibiting the NF-kappaB pathway. Diabetes and Vascular Disease Research. 2014;11(2):92–102. doi: 10.1177/1479164113520332. [DOI] [PubMed] [Google Scholar]
- 229.Fröjdö S., Durand C., Molin L., et al. Phosphoinositide 3-kinase as a novel functional target for the regulation of the insulin signaling pathway by SIRT1. Molecular and Cellular Endocrinology. 2011;335(2):166–176. doi: 10.1016/j.mce.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 230.Sundaresan N. R., Pillai V. B., Wolfgeher D., et al. The deacetylase SIRT1 promotes membrane localization and activation of Akt and PDK1 during tumorigenesis and cardiac hypertrophy. Science Signaling. 2011;4(182):p. ra46. doi: 10.1126/scisignal.2001465. [DOI] [PubMed] [Google Scholar]
- 231.Zhang J., Feng X., Wu J., et al. Neuroprotective effects of resveratrol on damages of mouse cortical neurons induced by β-amyloid through activation of SIRT1/Akt1 pathway. BioFactors. 2014;40(2):258–267. doi: 10.1002/biof.1149. [DOI] [PubMed] [Google Scholar]
- 232.Bordone L., Motta M. C., Picard F., et al. Sirt1 regulates insulin secretion by repressing UCP2 in pancreatic beta cells. PLoS Biology. 2006;4(2, article e31) doi: 10.1371/journal.pbio.0040031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Sun C., Zhang F., Ge X., et al. SIRT1 improves insulin sensitivity under insulin-resistant conditions by repressing PTP1B. Cell Metabolism. 2007;6(4):307–319. doi: 10.1016/j.cmet.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 234.Balan V., Miller G. S., Kaplun L., et al. Life span extension and neuronal cell protection by Drosophila nicotinamidase. Journal of Biological Chemistry. 2008;283(41):27810–27819. doi: 10.1074/jbc.m804681200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Xiong H., Dai M., Ou Y., et al. SIRT1 expression in the cochlea and auditory cortex of a mouse model of age-related hearing loss. Experimental Gerontology. 2014;51(1):8–14. doi: 10.1016/j.exger.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 236.Paschalaki K. E., Starke R. D., Hu Y., et al. Dysfunction of endothelial progenitor cells from smokers and chronic obstructive pulmonary disease patients due to increased dna damage and senescence. Stem Cells. 2013;31(12):2813–2826. doi: 10.1002/stem.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zhao Y., Luo P., Guo Q., et al. Interactions between SIRT1 and MAPK/ERK regulate neuronal apoptosis induced by traumatic brain injury in vitro and in vivo. Experimental Neurology. 2012;237(2):489–498. doi: 10.1016/j.expneurol.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 238.Du G., Song Y., Zhang T., et al. Simvastatin attenuates TNF-α-induced apoptosis in endothelial progenitor cells via the upregulation of SIRT1. International Journal of Molecular Medicine. 2014;34(1):177–182. doi: 10.3892/ijmm.2014.1740. [DOI] [PubMed] [Google Scholar]
- 239.Saini A., Al-Shanti N., Sharples A. P., Stewart C. E. Sirtuin 1 regulates skeletal myoblast survival and enhances differentiation in the presence of resveratrol. Experimental Physiology. 2012;97(3):400–418. doi: 10.1113/expphysiol.2011.061028. [DOI] [PubMed] [Google Scholar]
- 240.Wang T., Cui H., Ma N., Jiang Y. Nicotinamide-mediated inhibition of SIRT1 deacetylase is associated with the viability of cancer cells exposed to antitumor agents and apoptosis. Oncology Letters. 2013;6(2):600–604. doi: 10.3892/ol.2013.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Dong L., Zhou S., Yang X., Chen Q., He Y., Huang W. Magnolol protects against oxidative stress-mediated neural cell damage by modulating mitochondrial dysfunction and PI3K/Akt signaling. Journal of Molecular Neuroscience. 2013;50(3):469–481. doi: 10.1007/s12031-013-9964-0. [DOI] [PubMed] [Google Scholar]
- 242.Qi X.-F., Li Y.-J., Chen Z.-Y., Kim S.-K., Lee K.-J., Cai D.-Q. Involvement of the FoxO3a pathway in the ischemia/reperfusion injury of cardiac microvascular endothelial cells. Experimental and Molecular Pathology. 2013;95(2):242–247. doi: 10.1016/j.yexmp.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 243.Wang S., Chong Z. Z., Shang Y. C., Maiese K. WISP1 neuroprotection requires FoxO3a post-translational modulation with autoregulatory control of SIRT1. Current Neurovascular Research. 2013;10(1):54–69. doi: 10.2174/156720213804805945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Yang Y., Su Y., Wang D., et al. Tanshinol attenuates the deleterious effects of oxidative stress on osteoblastic differentiation via wnt/FoxO3a signaling. Oxidative Medicine and Cellular Longevity. 2013;2013:18. doi: 10.1155/2013/351895.351895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Hong E.-H., Lee S.-J., Kim J.-S., et al. Ionizing radiation induces cellular senescence of articular chondrocytes via negative regulation of SIRT1 by p38 kinase. Journal of Biological Chemistry. 2010;285(2):1283–1295. doi: 10.1074/jbc.M109.058628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Kozako T., Aikawa A., Shoji T., et al. High expression of the longevity gene product SIRT1 and apoptosis induction by sirtinol in adult T-cell leukemia cells. International Journal of Cancer. 2012;131(9):2044–2055. doi: 10.1002/ijc.27481. [DOI] [PubMed] [Google Scholar]
- 247.Balaiya S., Ferguson L. R., Chalam K. V. Evaluation of sirtuin role in neuroprotection of retinal ganglion cells in hypoxia. Investigative Ophthalmology and Visual Science. 2012;53(7):4315–4322. doi: 10.1167/iovs.11-9259. [DOI] [PubMed] [Google Scholar]
- 248.Marampon F., Gravina G. L., Scarsella L., et al. Angiotensin-converting-enzyme inhibition counteracts angiotensin II-mediated endothelial cell dysfunction by modulating the p38/SirT1 axis. Journal of Hypertension. 2013;31(10):1972–1983. doi: 10.1097/hjh.0b013e3283638b32. [DOI] [PubMed] [Google Scholar]
- 249.Kilic U., Gok O., Bacaksiz A., Izmirli M., Elibol-Can B., Uysal O. SIRT1 gene polymorphisms affect the protein expression in cardiovascular diseases. PLoS ONE. 2014;9(2) doi: 10.1371/journal.pone.0090428.e90428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Kim D.-W., Kim Y.-M., Kang S.-D., Han Y.-M., Pae H.-O. Effects of resveratrol and trans-3,5,4′-trimethoxystilbene on glutamate-induced cytotoxicity, heme oxygenase-1, and sirtuin 1 in HT22 neuronal cells. Biomolecules and Therapeutics. 2012;20(3):306–312. doi: 10.4062/biomolther.2012.20.3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Sansone L., Reali V., Pellegrini L., et al. SIRT1 silencing confers neuroprotection through IGF-1 pathway activation. Journal of Cellular Physiology. 2013;228(8):1754–1761. doi: 10.1002/jcp.24334. [DOI] [PubMed] [Google Scholar]
- 252.Jang S., Kang H. T., Hwang E. S. Nicotinamide-induced mitophagy: event mediated by high NAD+/NADH ratio and SIRT1 protein activation. Journal of Biological Chemistry. 2012;287(23):19304–19314. doi: 10.1074/jbc.m112.363747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Fang E. F., Scheibye-Knudsen M., Brace L. E., et al. Defective mitophagy in XPA via PARP-1 hyperactivation and NAD+/SIRT1 reduction. Cell. 2014;157(4):882–896. doi: 10.1016/j.cell.2014.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Min J. J., Huo X. L., Xiang L. Y., et al. Protective effect of Dl-3n-butylphthalide on learning and memory impairment induced by chronic intermittent hypoxia-hypercapnia exposure. Scientific Reports. 2014;4, article 5555 doi: 10.1038/srep05555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Chun P. Role of sirtuins in chronic obstructive pulmonary disease. Archives of Pharmacal Research. 2015;38(1):1–10. doi: 10.1007/s12272-014-0494-2. [DOI] [PubMed] [Google Scholar]
- 256.Shi J., Yin N., Xuan L.-L., Yao C.-S., Meng A.-M., Hou Q. Vam3, a derivative of resveratrol, attenuates cigarette smoke-induced autophagy. Acta Pharmacologica Sinica. 2012;33(7):888–896. doi: 10.1038/aps.2012.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Fulco M., Cen Y., Zhao P., et al. Glucose restriction inhibits skeletal myoblast differentiation by activating SIRT1 through AMPK-mediated regulation of Nampt. Developmental Cell. 2008;14(5):661–673. doi: 10.1016/j.devcel.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Cantó C., Auwerx J. Caloric restriction, SIRT1 and longevity. Trends in Endocrinology and Metabolism. 2009;20(7):325–331. doi: 10.1016/j.tem.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Herranz D., Serrano M. SIRT1: recent lessons from mouse models. Nature Reviews Cancer. 2010;10(12):819–823. doi: 10.1038/nrc2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Guo W., Qian L., Zhang J., et al. Sirt1 overexpression in neurons promotes neurite outgrowth and cell survival through inhibition of the mTOR signaling. Journal of Neuroscience Research. 2011;89(11):1723–1736. doi: 10.1002/jnr.22725. [DOI] [PubMed] [Google Scholar]
- 261.Zhang S., Cai G., Fu B., et al. SIRT1 is required for the effects of rapamycin on high glucose-inducing mesangial cells senescence. Mechanisms of Ageing and Development. 2012;133(6):387–400. doi: 10.1016/j.mad.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 262.Lai C.-S., Tsai M.-L., Badmaev V., Jimenez M., Ho C.-T., Pan M.-H. Xanthigen suppresses preadipocyte differentiation and adipogenesis through down-regulation of PPARγ and C/EBPs and modulation of SIRT-1, AMPK, and FoxO pathways. Journal of Agricultural and Food Chemistry. 2012;60(4):1094–1101. doi: 10.1021/jf204862d. [DOI] [PubMed] [Google Scholar]
- 263.Berschneider B., Königshoff M. WNT1 inducible signaling pathway protein 1 (WISP1): a novel mediator linking development and disease. International Journal of Biochemistry and Cell Biology. 2011;43(3):306–309. doi: 10.1016/j.biocel.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 264.Maiese K. WISP1: Clinical insights for a proliferative and restorative member of the CCN family. Current Neurovascular Research. 2014;11(4):378–389. doi: 10.2174/1567202611666140912115107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Pennica D., Swanson T. A., Welsh J. W., et al. WISP genes are members of the connective tissue growth factor family that are up-regulated in wnt-1-transformed cells and aberrantly expressed in human colon tumors. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(25):14717–14722. doi: 10.1073/pnas.95.25.14717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Davies S. R., Davies M. L., Sanders A., Parr C., Torkington J., Jiang W. G. Differential expression of the CCN family member WISP-1, WISP-2 and WISP-3 in human colorectal cancer and the prognostic implications. International Journal of Oncology. 2010;36(5):1129–1136. doi: 10.3892/ijo-00000595. [DOI] [PubMed] [Google Scholar]
- 267.Yeger H., Perbal B. The CCN family of genes: a perspective on CCN biology and therapeutic potential. Journal of Cell Communication and Signaling. 2007;1(3-4):159–164. doi: 10.1007/s12079-008-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Berwick D. C., Harvey K. The regulation and deregulation of Wnt signaling by PARK genes in health and disease. Journal of Molecular Cell Biology. 2014;6(1):3–12. doi: 10.1093/jmcb/mjt037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Chong Z. Z., Li F., Maiese K. Cellular demise and inflammatory microglial activation during β-amyloid toxicity are governed by Wnt1 and canonical signaling pathways. Cellular Signalling. 2007;19(6):1150–1162. doi: 10.1016/j.cellsig.2006.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Chong Z. Z., Shang Y. C., Hou J., Maiese K. Wnt1 neuroprotection translates into improved neurological function during oxidant stress and cerebral ischemia through AKT1 and mitochondrial apoptotic pathways. Oxidative Medicine and Cellular Longevity. 2010;3(2):153–165. doi: 10.4161/oxim.3.2.11758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Jian Y. C., Wang J. J., Dong S., et al. Wnt-induced secreted protein 1/CCN4 in liver fibrosis both in vitro and in vivo. Clinical Laboratory. 2014;60(1):29–35. doi: 10.7754/clin.lab.2013.121035. [DOI] [PubMed] [Google Scholar]
- 272.Klinke D. J., II Induction of Wnt-inducible signaling protein-1 correlates with invasive breast cancer oncogenesis and reduced type 1 cell-mediated cytotoxic immunity: a retrospective study. PLoS Computational Biology. 2014;10(1) doi: 10.1371/journal.pcbi.1003409.e1003409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Li F., Chong Z. Z., Maiese K. Winding through the WNT pathway during cellular development and demise. Histology and Histopathology. 2006;21(1–3):103–124. doi: 10.14670/hh-21.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Loilome W., Bungkanjana P., Techasen A., et al. Activated macrophages promote Wnt/beta-catenin signaling in cholangiocarcinoma cells. Tumor Biology. 2014;35(6):5357–5367. doi: 10.1007/s13277-014-1698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Maiese K., Li F., Chong Z. Z., Shang Y. C. The Wnt signaling pathway: aging gracefully as a protectionist? Pharmacology and Therapeutics. 2008;118(1):58–81. doi: 10.1016/j.pharmthera.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Ortiz-Masiá D., Cosín-Roger J., Calatayud S., et al. Hypoxic macrophages impair autophagy in epithelial cells through Wnt1: relevance in IBD. Mucosal Immunology. 2014;7(4):929–938. doi: 10.1038/mi.2013.108. [DOI] [PubMed] [Google Scholar]
- 277.Park H. Y., Toume K., Arai M. A., Koyano T., Kowithayakorn T., Ishibashi M. β-Sitosterol and flavonoids isolated from Bauhinia malabarica found during screening for Wnt signaling inhibitory activity. Journal of Natural Medicines. 2014;68(1):242–245. doi: 10.1007/s11418-013-0762-3. [DOI] [PubMed] [Google Scholar]
- 278.Saidak Z., Le Henaff C., Azzi S., Marty C., Marie P. J. Low-dose PTH increases osteoblast activity via decreased Mef2c/Sost in senescent osteopenic mice. Journal of Endocrinology. 2014;223(1):25–33. doi: 10.1530/JOE-14-0249. [DOI] [PubMed] [Google Scholar]
- 279.Thorfve A., Lindahl C., Xia W., et al. Hydroxyapatite coating affects the Wnt signaling pathway during peri-implant healing in vivo. Acta Biomaterialia. 2014;10(3):1451–1462. doi: 10.1016/j.actbio.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 280.van den Bosch M. H., Blom A. B., van Lent P. L., et al. Canonical Wnt signaling skews TGF-β Signaling in chondrocytes towards signaling via ALK1 and smad 1/5/8. Cellular Signalling. 2014;26(5):951–958. doi: 10.1016/j.cellsig.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 281.Su F., Overholtzer M., Besser D., Levine A. J. WISP-1 attenuates p53-mediated apoptosis in response to DNA damage through activation of the Akt kinase. Genes and Development. 2002;16(1):46–57. doi: 10.1101/gad.942902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Venkatesan B., Prabhu S. D., Venkatachalam K., et al. WNT1-inducible signaling pathway protein-1 activates diverse cell survival pathways and blocks doxorubicin-induced cardiomyocyte death. Cellular Signalling. 2010;22(5):809–820. doi: 10.1016/j.cellsig.2010.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.You Z., Saims D., Chen S., et al. Wnt signaling promotes oncogenic transformation by inhibiting c-Myc-induced apoptosis. Journal of Cell Biology. 2002;157(3):429–440. doi: 10.1083/jcb.200201110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Wang S., Chong Z. Z., Shang Y. C., Maiese K. Wnt1 inducible signaling pathway protein 1 (WISP1) blocks neurodegeneration through phosphoinositide 3 kinase/Akt1 and apoptotic mitochondrial signaling involving Bad, Bax, Bim, and Bcl-x L. Current Neurovascular Research. 2012;9(1):20–31. doi: 10.2174/156720212799297137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Yang M., Zhao X., Liu Y., Tian Y., Ran X., Jiang Y. A role for WNT1-inducible signaling protein-1 in airway remodeling in a rat asthma model. International Immunopharmacology. 2013;17(2):350–357. doi: 10.1016/j.intimp.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 286.Reddy V. S., Valente A. J., Delafontaine P., Chandrasekar B. Interleukin-18/WNT1-inducible signaling pathway protein-1 signaling mediates human saphenous vein smooth muscle cell proliferation. Journal of Cellular Physiology. 2011;226(12):3303–3315. doi: 10.1002/jcp.22676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Bayod S., Menella I., Sanchez-Roige S., et al. Wnt pathway regulation by long-term moderate exercise in rat hippocampus. Brain Research. 2014;1543:38–48. doi: 10.1016/j.brainres.2013.10.048. [DOI] [PubMed] [Google Scholar]
- 288.Borrell-Pagès M., Romero J. C., Badimon L. LRP5 negatively regulates differentiation of monocytes through abrogation of Wnt signalling. Journal of Cellular and Molecular Medicine. 2014;18(2):314–325. doi: 10.1111/jcmm.12190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Yang C.-S., Lopez C. G., Rana T. M. Discovery of nonsteroidal anti-inflammatory drug and anticancer drug enhancing reprogramming and induced pluripotent stem cell generation. Stem Cells. 2011;29(10):1528–1536. doi: 10.1002/stem.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Lough D., Dai H., Yang M., et al. Stimulation of the follicular bulge lgr5+ and lgr6+ stem cells with the gut-derived human alpha defensin 5 results in decreased bacterial presence, enhanced wound healing, and hair growth from tissues devoid of adnexal structures. Plastic and Reconstructive Surgery. 2013;132(5):1159–1171. doi: 10.1097/prs.0b013e3182a48af6. [DOI] [PubMed] [Google Scholar]
- 291.Heo J., Ahn E.-K., Jeong H.-G., et al. Transcriptional characterization of Wnt pathway during sequential hepatic differentiation of human embryonic stem cells and adipose tissue-derived stem cells. Biochemical and Biophysical Research Communications. 2013;434(2):235–240. doi: 10.1016/j.bbrc.2013.02.109. [DOI] [PubMed] [Google Scholar]
- 292.Murahovschi V., Pivovarova O., Ilkavets I., et al. WISP1 is a novel adipokine linked to inflammation in obesity. Diabetes. 2015;64(3):856–866. doi: 10.2337/db14-0444. [DOI] [PubMed] [Google Scholar]
- 293.Lim H. W., Lee J. E., Shin S. J., et al. Identification of differentially expressed mRNA during pancreas regeneration of rat by mRNA differential display. Biochemical and Biophysical Research Communications. 2002;299(5):806–812. doi: 10.1016/S0006-291X(02)02741-9. [DOI] [PubMed] [Google Scholar]
- 294.Liu H., Dong W., Lin Z., et al. CCN4 regulates vascular smooth muscle cell migration and proliferation. Molecules and Cells. 2013;36(2):112–118. doi: 10.1007/s10059-013-0012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Price R. M., Tulsyan N., Dermody J. J., Schwalb M., Soteropoulos P., Castronuovo J. J., Jr. Gene expression after crush injury of human saphenous vein: using microarrays to define the transcriptional profile. Journal of the American College of Surgeons. 2004;199(3):411–418. doi: 10.1016/j.jamcollsurg.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 296.Du J., Klein J. D., Hassounah F., Zhang J., Zhang C., Wang X. H. Aging increases CCN1 expression leading to muscle senescence. The American Journal of Physiology—Cell Physiology. 2014;306(1):C28–C36. doi: 10.1152/ajpcell.00066.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Marchand A., Atassi F., Gaaya A., et al. The Wnt/beta-catenin pathway is activated during advanced arterial aging in humans. Aging Cell. 2011;10(2):220–232. doi: 10.1111/j.1474-9726.2010.00661.x. [DOI] [PubMed] [Google Scholar]
- 298.Shang Y. C., Chong Z. Z., Wang S., Maiese K. Wnt1 inducible signaling pathway protein 1 (WISP1) targets PRAS40 to govern β-amyloid apoptotic injury of microglia. Current Neurovascular Research. 2012;9(4):239–249. doi: 10.2174/156720212803530618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Kopp C., Hosseini A., Singh S. P., et al. Nicotinic acid increases adiponectin secretion from differentiated bovine preadipocytes through G-protein coupled receptor signaling. International Journal of Molecular Sciences. 2014;15(11):21401–21418. doi: 10.3390/ijms151121401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Martínez de Morentin P. B., Martínez-Sánchez N., Roa J., et al. Hypothalamic mTOR: the rookie energy sensor. Current Molecular Medicine. 2014;14(1):3–21. doi: 10.2174/1566524013666131118103706. [DOI] [PubMed] [Google Scholar]
- 301.Paiva M. A., Rutter-Locher Z., Gonçalves L. M., et al. Enhancing AMPK activation during ischemia protects the diabetic heart against reperfusion injury. The American Journal of Physiology—Heart and Circulatory Physiology. 2011;300(6):H2123–H2134. doi: 10.1152/ajpheart.00707.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Jessen N., Koh H.-J., Folmes C. D., et al. Ablation of LKB1 in the heart leads to energy deprivation and impaired cardiac function. Biochimica et Biophysica Acta—Molecular Basis of Disease. 2010;1802(7-8):593–600. doi: 10.1016/j.bbadis.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Guan F. Y., Gu J., Li W., et al. Compound K protects pancreatic islet cells against apoptosis through inhibition of the AMPK/JNK pathway in type 2 diabetic mice and in MIN6 beta-cells. Life Sciences. 2014;107(1-2):42–49. doi: 10.1016/j.lfs.2014.04.034. [DOI] [PubMed] [Google Scholar]
- 304.Tanno M., Kuno A., Yano T., et al. Induction of manganese superoxide dismutase by nuclear translocation and activation of SIRT1 promotes cell survival in chronic heart failure. Journal of Biological Chemistry. 2010;285(11):8375–8382. doi: 10.1074/jbc.m109.090266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Kibbe C., Chen J., Xu G., Jing G., Shalev A. FOXO1 competes with carbohydrate response element-binding protein (ChREBP) and inhibits thioredoxin-interacting protein (TXNIP) transcription in pancreatic beta cells. Journal of Biological Chemistry. 2013;288(32):23194–23202. doi: 10.1074/jbc.M113.473082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Zhao Y., Yu Y., Tian X., et al. Association study to evaluate FoxO1 and FoxO3 gene in CHD in Han Chinese. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0086252.e86252 [DOI] [PMC free article] [PubMed] [Google Scholar]