Abstract
Objective
To assess attitudes and perceptions of United States survey respondents regarding prevalence, causes, and emotional effects of miscarriage.
Methods
We used a questionnaire consisting of 33 questions, administered in January of 2013 to men and women across the United States aged 18–69 years.
Results
Participants from 49 states completed the questionnaire: 45% male and 55% female (N=1084). Fifteen percent reported they or their partner suffered at least one miscarriage. Fifty-five percent of respondents believed that miscarriage occurred in 5% or less of all pregnancies. Commonly believed causes of miscarriage included a stressful event (76%), lifting a heavy object (64%), previous use of an intrauterine device (28%) or oral contraceptives (22%). Of those who had a miscarriage, 37% felt they had lost a child, 47% felt guilty, 41% reported feeling that they had done something wrong, 41% felt alone, and 28% felt ashamed. Nineteen percent fewer people felt they had done something wrong when a cause for the miscarriage was found. Seventy eight percent of all participants reported wanting to know the cause of their miscarriage, even if no intervention could have prevented it from occurring. Disclosures of miscarriages by public figures assuaged feelings of isolation for 28% of respondents. Level of education and gender had a significant impact on perceptions and understanding of miscarriage.
Conclusion
Respondents to our survey erroneously believed that miscarriage is a rare complication of pregnancy with majority believing that it occurred in 5% or less of all pregnancies. There were also widespread misconceptions about causes of miscarriage. Those who had suffered a miscarriage frequently felt guilty, isolated and alone. Identifying a potential cause of the miscarriage may have an effect on patients’ psychological and emotional responses.
INTRODUCTION
Miscarriage is the most common complication of pregnancy in the United States, occurring in 15–20% of clinically-recognized pregnancies, or 750,000–1,000,000 cases annually.1,2 Despite its frequency, miscarriage remains shrouded in shame and silence, even amongst friends and family, and its emotional impact has not been sufficiently investigated.3
The vast majority (60%) of miscarriages are due to aneuploidy.4–7 Other established causes of miscarriage include structural abnormalities in the uterus (such as fibroids or a uterine septum), thrombophilias (such as anti-phospholipid syndrome), endocrine disorders (such as hypothyroidism), and autoimmune disorders (such as anti-thyroid antibodies).8–14
In addition to physical complications, miscarriage can be an unexpected and emotionally devastating diagnosis for patients and their partners; women may suffer from psychological morbidity for months after the miscarriage, with effects lasting into subsequent pregnancies and levels of grief following a miscarriage were similar to those who suffered the loss of a close relative.15–20 In addition, one study found that women for whom a cause for the miscarriage could not be provided maintained significantly higher levels of anxiety four weeks post-miscarriage, longer than women for whom a diagnosis was determined.21 Researchers have examined how women cope with miscarriages and the ways in which these coping mechanisms may vary, yet the emotional burden of a miscarriage, particularly miscarriages that occur at an early gestational age, is often not recognized by healthcare professionals.22,23
Despite the prevalence of miscarriage, little is known regarding the public’s perception of the rate and causes of pregnancy loss. Because of the folklore surrounding miscarriage and the reluctance of those who experience a miscarriage to share that experience, there is a significant information gap between the medical diagnosis of miscarriage and the patient's personal experience.24 Insight into the public perception can help ensure that comprehensive care and education are delivered after a miscarriage occurs. We conducted a national cross-sectional survey assessing public perceptions of miscarriage to address these knowledge gaps.
MATERIALS AND METHODS
A 33-item survey was constructed to assess the public perceptions of miscarriage. Miscarriage was defined as a pregnancy loss occurring earlier than 20 weeks; an additional 10 items (for a total of 33) were specifically directed to those reporting a history of miscarriage. Both men and women were included in the survey. Men were eligible to answer the specific questions regarding miscarriage if they reported that their partner had suffered a miscarriage. (Appendix 1, available online at http://links.lww.com/xxx and Appendix 2, available online at http://links.lww.com/xxx)
The survey was posted online using Amazon.com Inc’s MTurk, a crowdsourcing web service. The full survey can be seen in Appendix 1 (http://links.lww.com/xxx) and Appendix 2 (http://links.lww.com/xxx). Both responders and requesters are anonymous, although individual responders can be linked through a unique identifier provided by Amazon. Requesters can post surveys that are visible only to responders who meet predefined criteria. All registered users of MTurk with an approval rating of greater than 85% (meaning 85% of their previous work on MTurk had been considered good) and have completed at least 50 prior tasks, were eligible to take the survey. These parameters were chosen to help improve data quality.
When responders login to the website they see a list of tasks available to them. Responders can read brief descriptions and preview the task prior to accepting the work. It is not possible to determine the number of people who previewed the survey and did not choose to take the survey, therefore we are unable to determine a view or participation rate. We had a 100 percent completion rate, meaning that all surveys that were started were submitted. The survey was voluntary, anonymous and respondents were given twenty five cents as monetary compensation. Anonymous survey responses have been validated in previous studies.25,26 The data were collected over a three day period. We collected data on demographic characteristics of respondents to quantify that their distribution was representative of the general U.S. population and if evidence of selection bias was observed.
The respondents were aware that the survey was part of a research study, but were not informed who was conducting it. At the beginning of the survey we posted “This is a voluntary research study about Pregnancy in the United States. All data will remain anonymous and you will receive a token of appreciation through MTurk. In accordance with MTurk policies, your identity will remain unknown and there is no way for researchers to match up your answers with your identity. You may stop answering questions at any time. Upon completion of the survey you will be paid $0.25 (25 cents).” This study was approved by the Albert Einstein College of Medicine Institutional Review Board.
The survey was written in hypertext markup language (HTML) and JavaScript. The usability and technical functionality was tested on 100 test participants prior to fielding the questionnaire. The survey was administered in one page with all the questions on that page. Participants were able to review their answers prior to submission. Batches of surveys were randomly divided such that half of the batches contained the question regarding “public figures” and half contained a question regarding “friends and family” to prevent respondents from directly comparing the two groups.
Two filters were used to increase data quality. The first filter was that if respondents answered the attention check question of “I had a fatal heart attack while watching TV with a “yes” or “maybe”, meaning they are reporting they have died, all of their responses were excluded from analysis. The second filter was a minimum time completion. The data of respondents who completed the survey in less than sixty seconds (meaning they completed the survey in less than 3 seconds a question) were excluded from analysis. Respondents were able to complete the survey only once. We were able to determine if a respondent answered the survey more than once by their unique ID string given by Mturk. If the unique ID string was seen twice in the database, the second set of data was excluded from analysis.
All survey data were preserved in the original format for analysis with the exception of the cause of miscarriage write-in responses. These were categorized as “Given a reason” and “Not given a reason” for describing whether medical staff gave them a reason for their miscarriage. The transformed variable was analyzed with the categorical variable, “feelings associated with the miscarriage,” using a chi-square test. Only four respondents did not answer this question and were excluded from the analysis of this question.
Ordinal data, such as income intervals or responses rated on the Likert scale, were analyzed using Mann-Whitney Wilcoxon (MWW) testing and proportional odds logistic regression in cases with multiple independent variables. After linearity was determined, continuous respondent attributes (e.g. age) were compared using t-tests. Non-ordinal proportions and odds ratios (OR) derived from contingency tables were analyzed using chi-squared testing or Fisher’s exact test where appropriate (e.g. small sample size). All other statistical testing was conducted as multivariate linear or logistic regression. All significance values were calculated for 2-sided 95% confidence intervals (CI) or p-value < 0.05. The software environment, R: A language and environment for statistical computing. (R Foundation for Statistical Computing, Vienna, Austria) was used for all analyses.
RESULTS
Men and women aged 18 years and older and located within the United States anonymously completed an online closed survey in January 2013 (n=1147). Fifty-seven responses were excluded for repeating the survey and six participants for answering yes to the filter item. No responses were excluded due to response time. These totaled to 6% of participants, leaving 1,084 valid respondents included in the analyses (94% usable response rate; 45% male and 55% female). There was 99% item completeness of data, missing data points were excluded from the individual analysis.
The socio-demographic distribution across gender, age, religion, geographic location, and household income (Table 1) were consistent with 2010 national census statistics.27 Race and ethnicity were not proportionately represented, with an under-representation of Blacks and Hispanics and an over-representation of Asians. Participants were from 49 out of 50 states with no one region over- or under-represented. Respondents had attained a higher level of education than the general public.28
Table 1.
Demographic Participant Characteristics n=1084
| No. (%) | P Value | |||
|---|---|---|---|---|
| Characteristic | Overall Sample | Sample reporting past miscarriage | Sample reporting no prior miscarriage | |
| Gender | ||||
| Male | 485 (45) | 39 (24) | 444 (48) | <.001 |
| Female | 594 (55) | 121 (76) | 470 (52) | |
| Marital Status | ||||
| Married | 409 (38) | 106 (66) | 303 (33) | vs. Married |
| Never Married | 580 (54) | 28 (18) | 552 (60) | <.001 |
| Divorced | 68 (6) | 19 (12) | 49 (5) | .76 |
| Separated or Widowed | 25 (2) | 7 (4) | 18 (2) | .81 |
| Race/Ethnicity | ||||
| White | 895 (78) | 139 (83) | 756 (77) | vs White |
| Black | 60 (5) | 11 (6) | 49 (5) | .69 |
| Hispanic | 68 (6) | 7 (4) | 61 (6) | .32 |
| Asian | 77(7) | 6(4) | 71(8) | .10 |
| Other | 48(4) | 5(3) | 43(5) | .45 |
| Religion | ||||
| Catholic | 152 (15) | 22 (14) | 130 (15) | <.001 |
| Protestant | 215 (20) | 40 (26) | 175 (19) | |
| Other Christian | 112 (10) | 32 (19) | 80 (9) | |
| Judaism | 22 (2) | 2 (1) | 20 (2) | |
| Islam | 11 (1) | 1 (1) | 10 (1) | |
| Buddhism | 28 (3) | 3 (2) | 25 (3) | |
| Other | 8 (1) | 2(2) | 6(1) | |
| Any religious affiliation | 544 (51) | 102 (64) | 442 (49) | <.001 |
| Unaffiliated (atheist/agnostic) | 518 (49) | 56 (36) | 462 (51) | |
| Education | ||||
| Attended Some High School | 12 (1) | 0 (0) | 12 (1) | .62* |
| Graduated High School | 110 (10) | 22 (14) | 88 (10) | |
| Attended Some College | 422 (39) | 53 (33) | 369 (40) | |
| Graduated College | 397 (37) | 62 (39) | 335 (36) | |
| Attended Graduate School | 128 (12) | 20 (13) | 108 (12) | |
| Attended Medical School | 10 (1) | 2 (1) | 8 (1) | |
| Annual Income*** | ||||
| < $ 19,999 | 185 (17) | 19 (12) | 166 (18) | 0.05* |
| $ 20,000–39,999 | 312 (29) | 44 (27) | 268 (29) | |
| $ 40,000–59,999 | 259 (24) | 45 (28) | 214 (23) | |
| $ 60,000–79,999 | 132 (13) | 20 (12) | 112 (12) | |
| $ 80,000–99,999 | 86 (8) | 15 (9) | 71 (8) | |
| $ 100,000–249,999 | 94(9) | 17 (11) | 77 (9) | |
| > $ 250,000 | 11 (1) | 1 (1) | 10 (1) | |
By proportional odds modeling unadjusted for age
Overall sample numbers when added together do not always equal the full sample of 1084 due to missing data points in that category.
US Dollars
Fifteen percent of respondents reported a history of miscarriage. Of those who reported they or their partner suffered a miscarriage, 75% were women. There was no significant difference in the prevalence of miscarriage by demographics. After accounting for age, neither income nor level of education was significantly related to a history of miscarriage.
A majority (55%) of participants incorrectly believed that miscarriages are uncommon (defined as less than 6% of all pregnancies); 10% of participants believed that fewer than 2% of all pregnancies end in miscarriage (Table 2). This misperception was more common among men; the odds of men reporting that miscarriages are uncommon was 2.5 [CI 1.87–3.15] that of women.
Table 2.
Frequency and causes of miscarriage n=1084
| No. (%) | |||||||
|---|---|---|---|---|---|---|---|
| Overall Sample | Sample reporting past miscarriage | Sample reporting no prior miscarriage | Men | Women | Sample reporting religious affiliation | Sample reporting no religions affiliation | |
| Percentage of Pregnancies that end in miscarriage | P value | <.001 | <.001 | .51 | |||
| 0.01 | 4(0.4) | 0 (0) | 4(0.4) | 1(0.2) | 3(1) | 4(1) | 0(0) |
| 0.1 | 15(1) | 1(1) | 14(2) | 11(2) | 4(1) | 6(1) | 9(2) |
| 1 | 89(8) | 7(4) | 82(9) | 55(11) | 28(6) | 44(8) | 45(9) |
| 5 | 489(45) | 47(29) | 442(48) | 259(53) | 183(38) | 250(46) | 230(44) |
| 25 | 399(37) | 82(51) | 318(35) | 129(27) | 220(46) | 211(39) | 182(35) |
| 50 | 76(7) | 19(12) | 57(6) | 26(5) | 41(9) | 29(5) | 46(9) |
| 75 | 11(1) | 5(3) | 6(1) | 4(1) | 5(1) | 3(1) | 6(1) |
| Most common cause of miscarriage | |||||||
| Lifestyle | 235(22) | 24(15) | 211(23) | 147(31) | 73(15) | 129(24) | 100(19) |
| Genetic | 337(31) | 67(42) | 270(29) | 113(23) | 183(38) | 167(31) | 167(32) |
| Medical Problems | 462(43) | 529(33) | 411(47) | 209(43) | 203(42) | 224(41) | 233(45) |
| Psych Issues | 24(2) | 6(4) | 18(2) | 7(2) | 13(3) | 9(2) | 12(2) |
| Punishment from God | 2(0.2) | 1(1) | 1(0.1) | 0(0) | 2(0.4) | 2(0.4) | 0 (0) |
| Destiny or Fate | 20(2) | 10(6) | 10(1) | 6(1) | 10(2) | 15(3) | 4 (1) |
Most participants (74%) correctly believed that pregnancy loss was most commonly the result of a genetic or medical problem (Table 2). Highly educated respondents, defined as those who graduated from college and/or received higher graduate education, were more likely to believe that the most common cause of miscarriage is genetic than those who were less educated (defined as those who have not completed college) (37.6% vs. 24.9%; p < 0.001). Level of education was significantly inversely associated with increased odds for reporting that miscarriages are not due to a genetic or medical problem (p < 0.001). Participants self-identified with Hispanic ethnicity were twice as likely (CI: 1.03–3.99) to disagree with the statement that genetic abnormalities can be a cause of miscarriage then those who identified as non-Hispanic.
Twenty-two percent of participants incorrectly believed that lifestyle choices, such as drug, alcohol, or tobacco use during pregnancy, are the single most common cause of miscarriage, more common than genetic or medical causes. Men were 2.6 times more likely to believe this than women (CI: 1.88–3.50; p < 0.001) (Table 2). Additionally, respondents who were less educated (defined as those who have not completed college) were twice as likely to believe lifestyle choices are the most common cause of miscarriage as higher educated respondents (28.9% vs. 14.4%; p-value < 0.001). Increasing level of education was significantly associated with decreased odds for this belief (p < 0.001).
An overwhelming majority of study participants (95%) correctly agreed that genetic abnormalities of the fetus may be a possible cause of miscarriage (Fig. 1). However, a majority of participants also believed that a stressful event (76%) or longstanding stress (74%) were also causes of miscarriage. A large number of respondents incorrectly agreed that lifting heavy objects (64%), having had a sexually transmitted disease in the past (41%), past use of an IUD (28%), past use of oral contraception (22%) or getting into an argument (21%) may all be potential causes for miscarriage.
Figure 1.
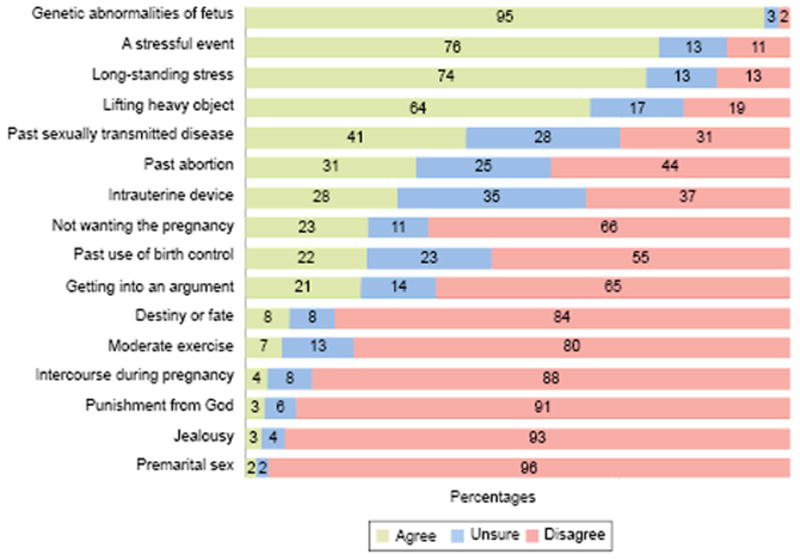
Respondent beliefs on the causes of miscarriage.
In addition to examining response trends within our total and gender-stratified study population, we also assessed differences among respondents by education level (Fig. 2). Those with less education were more likely to believe that lifting a heavy object, getting into an argument, or partaking in moderate exercise may cause miscarriage than those with higher levels of education (p < 0.001, p = 0.02, and p < 0.001, respectively).
Figure 2.
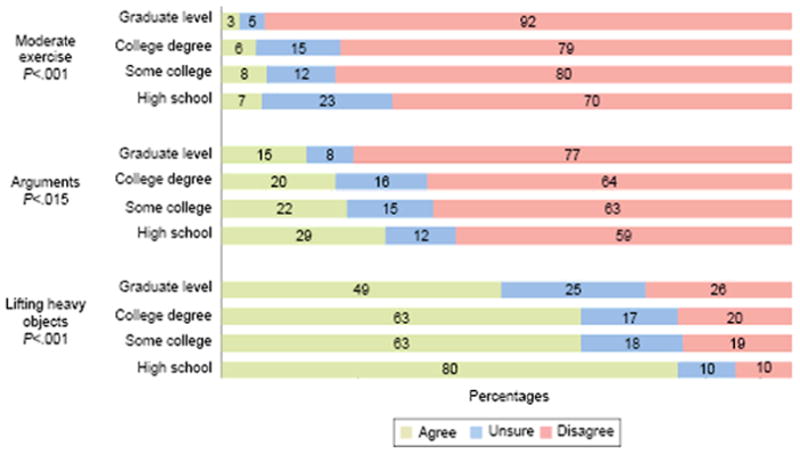
Respondent beliefs on the causes of miscarriage, by educational status.
Among all study participants (men and women) who reported a history of miscarriage, (either themselves or their partner), we asked an additional 10 questions regarding their experiences, emotional support, and emotional responses to miscarriage. Of those respondents who had experienced a miscarriage, 47% reported feeling guilty, 41% reported feeling that they did something wrong, 41% reported feeling alone, and 28% percent of reported feeling ashamed (Fig. 3).
Figure 3.
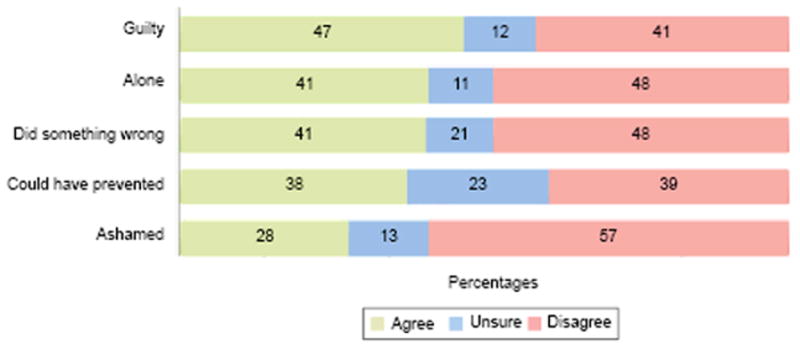
Self reported emotional response after experiencing miscarriage.
Over one third (38%) of those with a history of miscarriage felt that they could have prevented it and the majority of them reported that they were not given a cause for the miscarriage (57%). Over one third of all participants (36%), including those who had never experienced a pregnancy loss, reported that they would find a miscarriage to be extremely upsetting, equivalent to the loss of a child (Table 3). There were differences depending on religious affiliation, with those who associated themselves with any religion being twice as likely to report a miscarriage as emotionally similar to the loss of a child (48% vs. 23%, p <0.001). Most (74%) felt that they had received adequate emotional support from those they told. Only 45% felt that they had received adequate emotional support from the medical community, with 25% reporting they did not receive adequate support. Of those with an early pregnancy loss, 28% reported that disclosure of a miscarriage by celebrities assuaged their feelings of isolation; these numbers improved to 46% when friends disclosed their own miscarriage.
Table 3.
Participant responses n=1084
| No. (%) | |||||||
|---|---|---|---|---|---|---|---|
| Overall Sample | Sample reporting past miscarriage | Sample reporting no prior miscarriage | Men | Women | Sample reporting religious affiliation | Sample reporting no religious affiliation | |
| Emotional meaning of miscarriage | P value | .51 | .003 | <.001 | |||
| Extremely upsetting | 383(36) | 58(37) | 326(36) | 142(29) | 239(41) | 260(48) | 119(23) |
| Very upsetting | 328(31) | 52(33) | 276(30) | 171(35) | 156(27) | 144(27) | 174(34) |
| Moderately upsetting | 264(25) | 34(22) | 230(25) | 121(25) | 142(24) | 108(20) | 154(30) |
| Minimally upsetting | 72(7) | 11(7) | 61(7) | 42(9) | 30(5) | 25(4) | 46(9) |
| Not upsetting at all | 25(2) | 3(2) | 22(2) | 8(2) | 17(3) | 6(1) | 18(4) |
| Would like to know cause of miscarriage if can not prevent future miscarriage | P value | .25 | .52 | .71 | |||
| Strongly Like to know | 502(47) | 71(44) | 432(47) | 217(45) | 283(48) | 261(48) | 233(45) |
| Like to know | 335(31) | 50(31) | 285(31) | 155(32) | 179(30) | 157(29) | 172(34) |
| Unsure | 150(14) | 21(13) | 129(14) | 73(15) | 76(13) | 83(15) | 65(13) |
| Not Like to Know | 49(5) | 7(4) | 42(5) | 18(4) | 31(5) | 24(4) | 25(5) |
| Strongly Not Like to know | 39(4) | 12(8) | 27(3) | 17(4) | 22(4) | 20(4) | 19(4) |
A majority of participants (88%) would want to know the cause of the miscarriage if there is something that they could do to prevent it from happening in the future. In addition, a majority of respondents (78%) would still want to know the cause of the miscarriage even if there was nothing they could do to prevent the current pregnancy loss from occurring (Table 3).
We hypothesized that certain emotions, such as feeling alone or guilty, experienced by patients after a miscarriage were due to misperceptions regarding the possible causes for their pregnancy loss. When respondents who had experienced an early pregnancy loss were given a reason for the miscarriage, as opposed to being told “ it just happens, or we don’t know”, 19% fewer felt as though they had done something wrong (OR 0.45; CI 0.18–0.85). The other variables queried (feeling guilty, ashamed, alone, or that the respondent could have prevented the miscarriage) were not statistically significantly different.
Discussion
This is a national survey that provides insight into public perceptions of the incidence and causes of miscarriage and builds on prior work looking at the emotional effects of miscarriage in the U.S.21–23 We found that a majority of participants erroneously believed that miscarriages are an uncommon complication of pregnancy, occurring in less than 6% of all pregnancies in the United States. This misperception may foster the alienation that patients feel as they experience a miscarriage. Many participants also erroneously believed that past use of birth control, use of an IUD, or even lifting a heavy object may result in a miscarriage. Moreover, three out of four participants believed that a stressful event may cause a miscarriage. These beliefs may lead patients to a false sense of responsibility and contribute to the widespread sense of guilt felt after a miscarriage. These beliefs are likely compounded when no cause for the patient’s miscarriage is identified.
Previous studies have found increased levels of anxiety and depression in the months after a miscarriage.19,20 Our study is consistent with this finding, showing that the emotional and psychological effect on the woman or expectant father of a miscarriage can be perceived as the loss of a child.23 Unfortunately, only 45% of the participants who experienced miscarriage felt that they had received adequate emotional support from the medical community. This emotional burden may be under-appreciated by healthcare professionals and the community at large. These feelings may be partially ameliorated when public figures and friends reveal that they had a miscarriage. Our data could encourage friends and public figures to share their losses and use their stature to help combat feelings of shame, secrecy, and isolation. These results also suggest a need to enhance the emotional and educational support provided by the medical community to a couple experiencing pregnancy loss.
Our study was a cross-sectional survey of the US public. Since it is not possible to determine how many people previewed our survey without completing it, there is the potential for non-responder bias. It is possible that those who responded felt stronger about issues related to miscarriage. The incidence of miscarriage among respondents to our survey was 15%, which is within national levels of 15–20%.1 In addition, socio-demographic data, including age, gender, and household income mirrored national consensus data. However, our participants had a higher proportion of White and Asian respondents and a lower proportion of Black and Hispanic respondents than the national population, thus limiting the generalizability of our study to the US as whole. We had a higher proportion of people who had attended or finished college, yet our respondents still displayed belief in many misconceptions. Male responses might have led to higher estimates of misperceptions of causes and lower estimates of guilt or sense of responsibility for the miscarriage.
Our data suggest that patients who have suffered miscarriage may benefit from further counseling by providers, identification of the cause, and revelations from friends and celebrities. Health-care providers have an important role in assessing and educating all pregnant patients about known prenatal risk factors, diminishing concerns about unsubstantiated but prevalent myths, and, among those who experience a miscarriage, acknowledging and dissuading feelings of guilt and shame.
Supplementary Material
Acknowledgments
Supported by the Department of OB/GYN, Albert Einstein College of Medicine/Montefiore Medical Center (NIH NICHD HD068546).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Presented at the International Federation of Fertility Societies and The American Society for Reproductive Medicine Joint Conference on October 16th 2013, Boston, MA.
Contributor Information
Jonah Bardos, Program for Early and Recurrent Pregnancy Loss (PEARL), Department of Obstetrics & Gynecology and Women’s Health, Albert Einstein College of Medicine, New York, NY, Department of Obstetrics & Gynecology and Women’s Health, Mount Sinai Medical Center New York, NY.
Daniel Hercz, University of Sydney Medical School, Sydney, Australia.
Jenna Friedenthal, Program for Early and Recurrent Pregnancy Loss (PEARL), Department of Obstetrics & Gynecology and Women’s Health, Albert Einstein College of Medicine, New York, NY, Department of Obstetrics & Gynecology, New York University Langone Medical Center, New York, NY.
Stacey A. Missmer, Department of Obstetrics, Gynecology and Reproductive Biology, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, Department of Epidemiology, Harvard School of Public Health, Boston, MA.
Zev Williams, Program for Early and Recurrent Pregnancy Loss (PEARL), Department of Obstetrics & Gynecology and Women’s Health, Albert Einstein College of Medicine, New York, NY, Department of Obstetrics and Gynecology, Montefiore Medical Center, New York, NY.
References
- 1.Katz VL. Spontaneous and recurrent abortion: etiology, diagnosis, treatment. In: Katz VL, Lentz GM, Lobo RA, Gershenson DM, editors. Comprehensive Gynecology. 6. Philadelphia (PA): Elsevier Mosby; 2012. pp. 335–359. [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Center for Health Statistics, National Vital Statistics Reports. 7. Vol. 60. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 3.Kluger-Bell K. Unspeakable Losses: Healing from Miscarriage, Abortion and Other Pregnancy Losses. New York (NY): William Morrow Paperbacks; 2000. [Google Scholar]
- 4.American College of Obstetricians and Gynecologists. FAQ 100. Washington, D.C: American College of Obstetricians; 2013. [Google Scholar]
- 5.Benn P. Prenatal diagnosis of chromosomal abnormalities through amniocentesis. In: Milunsky A, editor. Genetic disorders and the fetus. 6. Baltimore (MD): The Johns Hopkins University Press; 2010. p. 199. [Google Scholar]
- 6.Hertig A, Sheldon W. Minimal criteria required to prove prima facie case of traumatic abortion or miscarriage: an analysis of 1000 spontaneous abortions. Ann Surg. 1943;117:596–606. doi: 10.1097/00000658-194304000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacobs PA, Hassold T. Chromosome abnormalities: origin and etiology in abortions and live births. In: Vogel F, Sperling K, editors. Human genetics. Berlin: Springer-Verlag; 1987. pp. 233–44. [Google Scholar]
- 8.Branch DW, Gibson M, Silver RM. Recurrent miscarriage. N Engl J Med. 2010;363:1740–7. doi: 10.1056/NEJMcp1005330. [DOI] [PubMed] [Google Scholar]
- 9.Fritz M, Speroff L. Recurrent early pregnancy loss 0030. In: Fritz M, Speroff L, editors. Clinical Gynecological Endocrinology and Infertility. 8. Philadelphia (PA): Lippincott Williams & Wilkins; 2011. pp. 1192–1220. [Google Scholar]
- 10.Alijotas-Reig J, Garrido-Gimenez C. Current concepts and new trends in the diagnosis and management of recurrent miscarriage. Obstetrical and Gynecological Survey. 2013;68:445–466. doi: 10.1097/OGX.0b013e31828aca19. [DOI] [PubMed] [Google Scholar]
- 11.Stagnaro-Green A, Glinoer D. Thyroid autoimmunity and the risk of miscarriage. Best Practice & Research Clinical Endocrinology & Metabolism. 2004;18:167–181. doi: 10.1016/j.beem.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A. Increased pregnancy loss rate in thyroid antibody negative women with TSH levels between 2.5 and 5.0 in the first trimester of pregnancy. J Clin Endocrinol Metabol. 2010;95:E44–E48. doi: 10.1210/jc.2010-0340. [DOI] [PubMed] [Google Scholar]
- 13.Mukhopadhaya N, Asante GP, Manyonda IT. Uterine fibroids: impact on fertility and pregnancy loss. Obstetrics Gynaecology Reprod Med. 2007;17:311–317. [Google Scholar]
- 14.Rey E, Kahn SR, David M, Shrier I. Thrombophilic disorders and fetal loss: a meta-analysis. Lancet. 2003;361:901–8. doi: 10.1016/S0140-6736(03)12771-7. [DOI] [PubMed] [Google Scholar]
- 15.Lee C, Slade P. Miscarriage as a traumatic event: a review of the literature and new implications for intervention. J Psychosomatic Research. 1996;40:235–244. doi: 10.1016/0022-3999(95)00579-x. [DOI] [PubMed] [Google Scholar]
- 16.Foyouzi N, Cedars M, Huddleston H. Cost-effectiveness of cytogenetic evaluation of products of conception in the patient with a second pregnancy loss. Fertility and Sterility. 2012;98:151–155. doi: 10.1016/j.fertnstert.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 17.Brier N. Anxiety after miscarriage: a review of the empirical literature and implications for clinical practice. Birth. 2004;31:138–142. doi: 10.1111/j.0730-7659.2004.00292.x. [DOI] [PubMed] [Google Scholar]
- 18.Cumming G, Klein S, Bolsover D, Lee A, Alexander D, Maclean M. The emotional burden of miscarriage for women and their partners: trajectories of anxiety and depression over 13 months. British Journal of Obstetrics Gynaecology. 2007;114:1138–1145. doi: 10.1111/j.1471-0528.2007.01452.x. [DOI] [PubMed] [Google Scholar]
- 19.Nikcevic A, Tunkel S, Nicolaides K. Psychological Outcomes Following Missed Abortions and Provision of Follow-Up Care. Ultrasound in Obstetrics & Gynecology. 1998;11:123–28. doi: 10.1046/j.1469-0705.1998.11020123.x. [DOI] [PubMed] [Google Scholar]
- 20.Nikcevic A, Tinkel S, Kuczmierczyk A, Nicolaides K. Investigation of the Cause of Miscarriage and Its Influence on Women's Psychological Distress. BJOG: an International Journal of Obstetrics and Gynaecology. 1999;106:808–13. doi: 10.1111/j.1471-0528.1999.tb08402.x. [DOI] [PubMed] [Google Scholar]
- 21.Nikcevic A, Kuczmierczyk A, Nicolaides K. The influence of medical and psychological interventions on women's distress after miscarriage. J Psychosomatic Research. 2007;63:283–90. doi: 10.1016/j.jpsychores.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Van P. Conversations, coping, & connectedness: a qualitative study of women who have experienced involuntary pregnancy loss. Omega (Westport) 2012;65:71–85. doi: 10.2190/OM.65.1.e. [DOI] [PubMed] [Google Scholar]
- 23.Brier N. Understanding and managing the emotional reactions to a miscarriage. Obstet Gynecol. 1999;93:151–5. doi: 10.1016/s0029-7844(98)00294-4. [DOI] [PubMed] [Google Scholar]
- 24.Schaffir J. Do Patient associate adverse pregnancy outcomes with folkloric beliefs? Arch Women’s Mental Health. 2007;10:301–304. doi: 10.1007/s00737-007-0201-0. [DOI] [PubMed] [Google Scholar]
- 25.Ramo D, Liu H, Prochaska J. Reliability and validity of young adults' anonymous online reports of marijuana use and thoughts about use. J Psychology of Addictive Behaviors. 2012;26:801–811. doi: 10.1037/a0026201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramo D, Hall S, Prochaska J. Reliability and validity of self-reported smoking in an anonymous online survey with young adults. Health Psychol. 2011;30:693–701. doi: 10.1037/a0023443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.United States Census Bureau. Census Data—General information. Available at: http://www.census.gov/2010census/ Retrieved March 18, 2013.
- 28.United States Census Bureau. Census Data General information. Available at : https://www.census.gov/hhes/socdemo/education/about/index.html. Retrieved June 2, 2014.
- 29.Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertility and Sterility. 2012;98:1103–1111. doi: 10.1016/j.fertnstert.2012.06.048. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


