Noninvasive diagnosis of liver fibrosis: The importance of being reimbursed
To the Editor:
With great interest, we read the article by Kan et al (1) in the March 2015 issue of the Journal, reporting the results of a survey of 422 patients evaluating the preference and willingness to pay for transient elastography versus liver biopsy in British Columbia. The topic explored by these authors is sound given that, despite both liver biopsy and transient elastography are approved in Canada for liver fibrosis staging, only liver biopsy is covered under all provincial health care plans. As of 2013, Quebec is the only province reimbursing transient elastography (Fibroscan, Echosens, France) in Canada. In a recent study (2), we showed that liver fibrosis diagnosis is systematically required by the majority of Canadian physicians managing patients with chronic liver diseases. However, 46.2% of Canadian physicians still use liver biopsy as primary diagnostic tool. In France, where Fibroscan and Fibrotest (LabCorp, USA) have been reimbursed since 2007, liver biopsy is still systematically performed by only 4% of hepatologists (3). Major obstacles for Canadian physicians to implement noninvasive methods include difficult access to transient elastography (42.3%) and concerns about reimbursement policies (14.4%). On the other hand, most Canadian physicians (82.6%) consider noninvasive diagnostic tools for liver fibrosis to be accurate and reliable (2). The study by Kan et al (1) has the invaluable merit of providing the patient’s perspective in terms of discomfort experienced and acceptability of transient elastography versus liver biopsy. Importantly, almost one-half of the respondents were also liver biopsy experienced. The vast majority (95.4%) of patients prefer transient elastography to liver biopsy if both tests are available at no cost. Moreover, 75.3% of patients are willing to pay for transient elastography instead of undergoing a liver biopsy at no cost. The results of our survey conducted among physicians and of the current survey among patients point toward the same direction: the necessity of harmonizing common reimbursement policies for liver fibrosis diagnosis across Canada. There are several other reasons supporting the implementation of transient elastography instead of liver biopsy. First, liver biopsy is an invasive procedure with risks for complications. A population-based study involving 4275 patients conducted in Canada showed that significant biopsy-related complications occurred in 0.75% of patients and the median direct cost of a hospitalization for complications was $4,579 (4). Second, liver biopsy results are often limited by methodological flaws, including sampling variability, and intra- and interobserver variation. Mehta et al (5) argued that the ideal surrogate will never attain the maximal diagnostic accuracy, expressed as area under the curve (AUC), because of the intrinsic limitations of the reference standard. By considering a spectrum of accuracies of the biopsy plus a spectrum of prevalence of substantial fibrosis, they demonstrated that even under optimal conditions and with a perfect marker, it is not possible to achieve an AUC ≥0.90 when assessing substantial fibrosis. As such, liver biopsy should not be considered as the gold standard, but rather as the best available standard for staging liver fibrosis. Third, in current era of implementation of screening strategies for hepatitis C in baby boomers, an invasive and costly tool to stage liver fibrosis is a major limitation. Canadian guidelines for the management of chronic hepatitis C state that all patients should be considered for antiviral treatment and, at the same time, all patients should undergo an evaluation for liver fibrosis staging (6). We read these lines as a conditio sine qua non: if we screen patients for hepatitis C, we should offer treatment, and if we offer treatment, we should first screen for liver fibrosis stage. To us, liver biopsy is not a feasible screening tool and may pose a barrier to identification of patients with advanced liver fibrosis in urgent need of treatment. In our centre, a screening strategy using transient elastography revealed occult cirrhosis without any clinical sign in 12% of all patients with chronic liver disease and in 37% of all cirrhotic patients (7). Importantly, only 36% of patients with occult cirrhosis receive the recommended surveillance for hepatocellular carcinoma and esophageal varices. Screening and early identification of these patients through noninvasive methods would be beneficial to allow application of recommended surveillance protocols for portal hypertension and hepatoma, and potentially enable third-party payers to appropriately prioritize the cost-effective use of newer, potent and costly therapies for hepatitis C to prevent future decompensation. Fourth, emerging data show that it is not just a matter of diagnosis. Transient elastography and other noninvasive tests have a better prognostic value than liver histology to predict clinical outcomes, including death, decompensation and need for liver transplantation, in chronic viral hepatitis and nonalcoholic fatty liver disease (8,9). Repeated measures over time by noninvasive tools are feasible and inexpensive. Noninvasive methods for liver fibrosis enable serial monitoring and longitudinal assessment for prognostication and risk stratification. Fifth, an equitable reimbursement policy across the country can increase the number of patients with chronic liver diseases undergoing the recommended screening for liver fibrosis. Reimbursement for transient elastography in Quebec led to >50% increase in the number of examinations performed in our centre (Figure 1). This obviously translates into a concomitant reduction in the number of liver biopsies performed for staging purposes at our centre, with >90% and 70% of patients with chronic hepatitis C and B, respectively, currently staged without a biopsy. Accordingly, in our survey we found that noninvasive diagnostic tools reduced the number of liver biopsies by >50% for >40% of Canadian physicians. As Kan et al (1) state, liver biopsy is still essential to diagnose the etiology of liver disease, such as in autoimmune hepatitis, and in case of overlap conditions.
Figure 1).
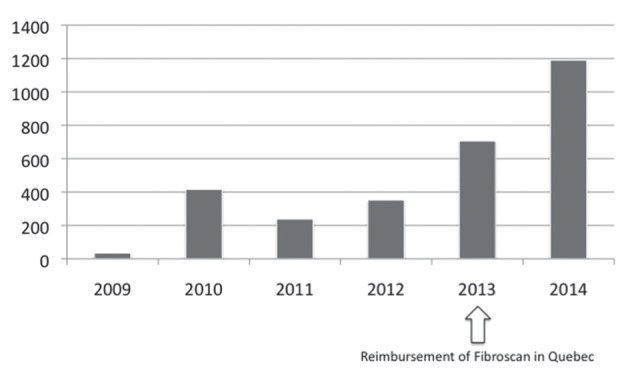
Number of Fibroscan (Echosens, France) examinations performed at McGill University Health Centre (Montreal, Quebec) from 2009 to 2014. Arrow indicates the year when reimbursement for the procedure was implemented
In conclusion, we fully support the patients’ and the physicians’ need for a homogeneous reimbursement policy across all provinces of Canada. The systematic use of transient elastography and other validated noninvasive methods as first-line screening tests would reduce costs for the health care system and complications for patients, and would enable physicians to perform a serial monitoring on patients, to define prognosis earlier and to logically dispose of resources, including prioritizing patients with hepatitis C for treatment.
Giada Sebastiani MD, Peter Ghali MD FRCPC MSc
Marc Deschenes MD, Philip Wong MD FRCPC MSc
Division of Gastroenterology and Hepatology, Royal Victoria Hospital
McGill University Health Centre, Montreal, Quebec
Footnotes
DISCLOSURES: GS has acted as speaker for Merck, Vertex, Gilead, Echosens, served as an advisory board member for Boheringer Ingelheim and Novartis and has received research funding from Vertex, ViiV and Merck. PG has acted as consultant for Merck, Vertex and Gilead. MD has served as an advisory board member for Roche, Merck, Janssen, Vertex, Gilead. PW has served as consultant for Bristol Myers Squibb, Gilead, Merck, Novartis, Roche, Vertex.
FINANCIAL SUPPORT: GS holds a Chercheur-Boursier career award from the Fonds de la Recherche en Santé du Quebéc (FRSQ).
REFERENCES
- 1.Kan VY, Azalgara VM, Ford JAE, Kwan PWC, Erb SR, Yoshida EM. Patient preference and willingness to pay for transient elastography versus liver biopsy: A perspective from British Columbia. Can J Gastroenterol Hepatol. 2015;29:72–6. doi: 10.1155/2015/169190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sebastiani G, Ghali P, Wong P, Klein MB, Deschenes M, Myers RP. Physicians’ practices for diagnosing liver fibrosis in chronic liver diseases: A nationwide, Canadian survey. Can J Gastroenterol Hepatol. 2014;28:23–30. doi: 10.1155/2014/675409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castera L, Denis J, Babany G, Roudot-Thoraval F. Evolving practices of non-invasive markers of liver fibrosis in patients with chronic hepatitis C in France: Time for new guidelines? J Hepatol. 2007;46:528–529. doi: 10.1016/j.jhep.2006.12.002. author reply 529–30. [DOI] [PubMed] [Google Scholar]
- 4.Myers RP, Fong A, Shaheen AA. Utilization rates, complications and costs of percutaneous liver biopsy: A population-based study including 4275 biopsies. Liver Int. 2008;28:705–12. doi: 10.1111/j.1478-3231.2008.01691.x. [DOI] [PubMed] [Google Scholar]
- 5.Mehta SH, Lau B, Afdhal NH, Thomas DL. Exceeding the limits of liver histology markers. J Hepatol. 2009;50:36–41. doi: 10.1016/j.jhep.2008.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myers RP, Shah H, Burak KW, Cooper C, Feld JJ. An update on the management of chronic hepatitis C: 2015 consensus guidelines from the Canadian Association for the Study of the Liver. Can J Gastroenterol Hepatol. 2015;29:19–34. doi: 10.1155/2015/692408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen T, Wong R, Wong P, et al. Occult cirrhosis diagnosed by transient elastography is a frequent and under-monitored clinical entity. Liv Int. 2015 Mar 4; doi: 10.1111/liv.12802. 2015; (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 8.Vergniol J, Foucher J, Terrebonne E, et al. Noninvasive tests for fibrosis and liver stiffness predict 5-year outcomes of patients with chronic hepatitis C. Gastroenterology. 2011;140:1970–9. doi: 10.1053/j.gastro.2011.02.058. [DOI] [PubMed] [Google Scholar]
- 9.Angulo P, Bugianesi E, Bjornsson ES, et al. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2013;145:782–9. doi: 10.1053/j.gastro.2013.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]


