Abstract
The quality of life (QOL) of men who have sex with men (MSM) has received increasing attention in recent years. Our study surveyed the QOL and explored the influence of social support on QOL in Chinese MSM. A cross-sectional survey was conducted from September 2013 to March 2014 of 438 MSM in Huludao and Zhengzhou City, China. The results of univariate analysis showed that higher QOL scores were associated with receiving psychosocial counseling, higher health education, younger age and marital status of being single or unmarried p < 0.05). The structural equation model fitted well, with χ2 = 2083.47 (p < 0.05), RMSEA = 0.07, and GFI = 0.88. Among the latent factors, social support, with a factor load of 0.47, had greater impact on QOL than demographic characteristics. Within social support, the item loads for psychosocial counseling and health education were 0.17 and 0.29, respectively. Basic demographic characteristics also influenced social support, with a factor load of -0.65. For demographic characteristics, the greatest item loads were for marital status and age (0.77 and 0.71, respectively). These findings suggest that strengthening social support, especially for older and married individuals, would improve QOL in MSM in China.
Introduction
In China, the HIV epidemic among Chinese men who have sex with men (MSM) continues to expand rapidly [1]. Sentinel surveillance data have shown that the prevalence of HIV in Chinese MSM increased from 2.0% in 2007 to 6.3% in 2011 [2]. The increase in the percentage of new HIV cases is still dramatic. Chinese MSM accounted for 0.2% of new infections in 2001, 12.2% in 2007, and 32.5% in 2009 [3,4]. The MSM population has become a high risk group for sexually transmitted disease (STD) infection in China due to their high number of partners, unprotected anal intercourse (UAI) and high migration rates [5–7]. MSM may also play a bridging role in the spread of HIV and other STDS from a high-risk population to the general population, which presents a concentrated public health problem [8]. In China, MSM have recently gained more attention from the Chinese Government in terms of HIV prevention and care [9].
The health-related quality of life (HRQoL) has increasingly been acknowledged as an important and valid health outcome measure in health services research, clinical trials, and evaluation [10]. Bucciardini et al. also proposed that the HRQoL could be an effective measure of health status [11]. Quality of life (QOL), especially mental health, can affect HIV-related sexual risk behavior in MSM, and, therefore, there is a need for comprehensive information about the health status of the MSM population [12,13]. Furthermore, mental HRQoL negatively associates with abuse, violence and HIV-related high-risk behaviour among homosexual and bisexual MSM [14]. Identification as gay or homosexual is related to poorer mental health [15,16]. The MSM population is also more concerned about their physical health than men from the general population [17]. Studies of QOL may help to understand the mental and physical status of MSM and to identify influencing factors to improve HIV prevention efficacy [12,17].
Many studies have investigated HRQoL in HIV-positive patients and people living with HIV/AIDS (PLWHA) [10,18–22]. Some have examined the association between HRQoL and different risk factors. Razavi et al. showed that, of PLWHA, participants older than 35 years and unemployed participants had significantly lower scores in overall quality of life [23]. Several studies have found that social support is a major factor positively affecting HRQoL in general and HIV-infected populations [20–22,24–26]. A previous study suggested that HIV counseling and testing could promote safe sexual behavior in PLWHA [21]. However, limited information is available about the relationship between QOL and social support in the Chinese MSM population.
In the present study, our aim was to survey the QOL of Chinese MSM and examine the relationship between QOL and social support in order to provide more effective HIV prevention information.
Materials and Methods
Ethic statements
Participation was voluntary and verbal informed consent was obtained from each of the participants prior to interview. To maintain privacy and anonymity, no personal identifying information or written consent were collected. This research was approved by the Bioethics Advisory Commission of China Medical University.
Respondents and procedures
A cross-sectional study was conducted from August 2013 to March 2014 in two Chinese cities, Zhengzhou and Huludao. Respondents were recruited from the internet, bars and saunas. All potential participants underwent a face-to-face explanation to a standardized questionnaire. All questionnaires were self-administered in a private room using the standardized version of the questionnaire.
Questionnaires
The Health Survey Short Form (SF-36) questionnaire contained 36 items and measured domains of health-related quality of life with 8 scales: physical functioning (PF), role limitation due to physical problems (RP), bodily pain (BP), general health perceptions (GH), vitality (VT), social functioning (SF), role limitation due to emotional problems (RE), and mental health (MH). Each scale is standardized on a 0–100 metric, with higher scores indicating better functioning. These dimensions were further categorized into physical component summary (PCS) and mental component summary (MCS). PCS was drawn from PF, RP, BP and GH, whereas MCS was drawn from VT, SF, RE and MH. The total score (QOL) of the SF-36 included both physical and mental health statuses. The scores of PCS, MCS and QOL ranged from 0 to 100, with higher scores representing better health [27]. The questionnaire also included demographic and social support sections. Demographic information items included age, marital status, education level, vocation, and monthly income. Social support items included family or friend awareness of sexual orientation, psychosocial counseling, health education, and receiving condoms, lubricants, peer education, HIV/syphilis testing, and AIDS information materials.
Statistical analysis
In this study, a structure equation model (SEM) was used to measure the relationship between observed and latent variables. The factor loads of the structure equation model ranged from 0 to 1. SEM can show direct and indirect relationships between variables by path maps [28–34]. In addition, whether the relationships are reasonable could be verified based on the results of SEM [28].
The distributions of total scores of the categorical QOL variables were compared by the Student’s t-test and one-way ANOVA. Reliability analysis of the data and univariate analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) for Windows, and the SEM was produced using LISREL 8.5. χ2, RMSEA (root mean square error of approximation), SRMR (standardized root mean square residual), GFI (goodness-of-fit index), AGFI (adjusted goodness-of-fit index), and IFI (incremental fit index) were used to indicate whether the model was an adequate fit [34].
Results
Participant characteristics
A total of 453 MSM were surveyed for the study and 438 MSM completed the questionnaire (response rate: 96.7%). The ages of respondents ranged from 18 to 74 years, with an average age of 28.26 ± 7.91 years. 186 (42.5%) respondents self-identified as bisexual and 252 (57.5%) as gay. The PCS and QOL scores for older individuals were significantly lower than those for younger individuals (p < 0.05). The PCS, MCS and QOL scores in the married group were lower than in the other two groups (p < 0.05). Compared to other respondents, the unemployed had the lowest MCS scores (p < 0.05). The PCS, MCS and total QOL scores increased with income level (p < 0.05). Participant characteristics and demographic information is outlined in Table 1.
Table 1. Comparison of SF-36 scores for the MSM population by participant characteristics.
| Variable | PCS | MCS | QOL | |||
|---|---|---|---|---|---|---|
| Mean ± SD | F value | Mean ± SD | F value | Mean ± SD | F value | |
| Age (years) | 15.3 | 1.1 | 4.6 | |||
| ≤25 | 80.5 ± 18.6** | 60.7 ± 20.8 | 70.6 ± 18.2** | |||
| 25–35 | 74.0 ± 18.2 | 62.6 ± 21.9 | 68.3 ± 18.4 | |||
| 35–45 | 70.8 ± 17.8 | 60.0 ± 18.3 | 65.4 ± 20.1 | |||
| ≥45 | 60.2 ± 16.4 | 59.7 ± 17.6 | 60.0 ± 18.0 | |||
| Marital status | 25.0 | 10.2 | 17.7 | |||
| Single | 77.1 ± 21.9** | 65.0 ± 19.9** | 71.1 ± 20.5** | |||
| Married | 59.9 ± 18.8 | 55.3 ± 16.7 | 57.6 ± 18.2 | |||
| Divorced or widowed | 65.4 ± 20.0 | 56.9 ± 18.4 | 61.2 ± 18.9 | |||
| Education | 1.2 | 1.1 | 1.0 | |||
| Junior high school or lower | 77.1 ± 14.8 | 59.5 ± 17.6 | 68.3 ± 17.9 | |||
| Senior high school | 74.8 ± 18.1 | 61.2 ± 18.7 | 68.0 ± 19.1 | |||
| College or above | 76.8 ± 20.2 | 62.6 ± 19.5 | 69.7 ± 19.3 | |||
| Vocation | 1.2 | 3.0 | 1.0 | |||
| Unemployed | 72.0 ± 15.9 | 70.4 ± 14.9* | 71.2 ± 19.6 | |||
| Student | 72.1 ± 16.6 | 72.8 ± 16.1 | 72.4 ± 18.7 | |||
| Blue collar | 72.3 ± 16.8 | 72.5 ± 16.0 | 72.4 ± 21.9 | |||
| White collar | 70.5 ± 17.1 | 74.9 ± 15.8 | 72.7 ± 20.9 | |||
| Monthly income | 9.8 | 9.5 | 6.2 | |||
| ≤1000 Yuan | 71.2 ± 16.7** | 58.5 ± 18.6** | 64.9 ± 18.4** | |||
| 1000–3000 Yuan | 72.1 ± 17.2 | 66.4 ± 20.2 | 69.2 ± 21.2 | |||
| ≥3000 Yuan | 79.9 ± 18.3 | 68.6 ± 19.9 | 74.2 ± 22.4 | |||
PCS, Physical Component Summary; MCS, Mental Component Summary; QOL, quality of life. One-way ANOVA was used for data analysis
*p < 0.05.
** p < 0.01.
Reliability and validity analysis
The Cronbach’s α coefficient for our analysis was 0.96, indicating good reliability. In the validity analysis, the Bartlett’s test was significant (p < 0.01), whereas the Kaiser-Meyer-Olkin measure was 0.78, justifying the application of a factor-analytic procedure, and eight factors accounted for 88% of the variance (Table 2).
Table 2. Factor analysis results.
| SF-36 Item | PF | RP | BP | GH | VT | SF | RE | MH |
|---|---|---|---|---|---|---|---|---|
| PF01 | 0.68 | |||||||
| PF02 | 0.87 | |||||||
| PF03 | 0.91 | |||||||
| PF04 | 0.93 | |||||||
| PF05 | 0.94 | |||||||
| PF06 | 0.93 | |||||||
| PF07 | 0.96 | |||||||
| PF08 | 0.97 | |||||||
| PF09 | 0.99 | |||||||
| PF10 | 0.95 | |||||||
| RP1 | 0.94 | |||||||
| RP2 | 0.93 | |||||||
| RP3 | 0.95 | |||||||
| RP4 | 0.93 | |||||||
| BP1 | 0.94 | |||||||
| BP2 | 0.96 | |||||||
| GH1 | 0.62 | |||||||
| GH2 | 0.81 | |||||||
| GH3 | 0.88 | |||||||
| GH4 | 0.84 | |||||||
| GH5 | 0.87 | |||||||
| VT1 | 0.58 | |||||||
| VT2 | 0.64 | |||||||
| VT3 | 0.83 | |||||||
| VT4 | 0.81 | |||||||
| SF1 | 0.88 | |||||||
| SF2 | 0.70 | |||||||
| RE1 | 0.94 | |||||||
| RE2 | 0.95 | |||||||
| RE3 | 0.91 | |||||||
| MH1 | 0.64 | |||||||
| MH2 | 0.74 | |||||||
| MH3 | 0.55 | |||||||
| MH4 | 0.86 | |||||||
| MH5 | 0.64 |
PF, physical function; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social function; RE, role-emotional; MH, mental health.
Social support
A total of 66.7%, 64.4% and 56.1% of the MSM surveyed received condoms, lubricant, and peer education, respectively, in the past 12 months. The proportions that received STD testing and informational materials in the past 12 months were 25.5% and 60.8%, respectively. A total of 10.7% and 59.8% of the respondents received psychosocial counseling and attended health education, respectively, in the past 12 months, and 8.6% of the MSM surveyed disclosed their sexual orientation to relatives or friends. In the univariate analyses, respondents who received STD testing had higher physical health scores (p < 0.05), and respondents who concealed their sexual orientation from relatives and friends had lower mental health scores (p < 0.05). The respondents receiving psychosocial counseling and health education had higher PCS, MCS and QOL scores (p < 0.05). These results for social support are summarized in Table 3.
Table 3. Comparison of SF-36 scores for the Chinese MSM population by social support received.
| Item | PCS | MCS | QOL | |||
|---|---|---|---|---|---|---|
| Mean ± SD | t value | Mean ± SD | t value | Mean ± SD | t value | |
| Received condoms | 0.7 | 0.8 | 0.7 | |||
| Yes | 71.2 ± 19.8 | 56.1 ± 16.6 | 63.6 ± 18.4 | |||
| No | 69.8 ± 19.1 | 54.7 ± 17.0 | 62.2 ± 20.6 | |||
| Received lubricants | 0.7 | 0.5 | 0.5 | |||
| Yes | 71.7 ± 18.6 | 58.8 ± 16.2 | 65.3 ± 21.0 | |||
| No | 70.4 ± 19.9 | 58.0 ± 15.2 | 64.2 ± 20.2 | |||
| Received peer education | 0.9 | 0.5 | 0.7 | |||
| Yes | 75.4 ± 19.4 | 71.9 ± 22.6 | 73.6 ± 19.6 | |||
| No | 73.8 ± 19.2 | 70.8 ± 20.8 | 72.3 ± 18.1 | |||
| Received STD (HIV/syphilis) testing | 2.4 | 0.3 | 0.9 | |||
| Yes | 80.5 ± 17.2* | 68.2 ± 20.6 | 74.4 ± 19.9 | |||
| No | 76.1 ± 16.4 | 69.0 ± 23.4 | 72.5 ± 20.1 | |||
| Received psychosocial counseling | 2.3 | 2.2 | 2.1 | |||
| Yes | 80.1 ± 15.2* | 86.0 ± 18.2* | 83.0 ± 16.8* | |||
| No | 74.7 ± 15.0 | 79.9 ± 17.9 | 77.3 ± 17.4 | |||
| Received health education | 2.5 | 4.1 | 3.4 | |||
| Yes | 75.6 ± 15.2* | 80.9 ± 20.0** | 78.2± 18.7** | |||
| No | 71.7 ± 16.7 | 72.5 ± 22.9 | 72.1 ± 18.4 | |||
| Received AIDS information materials | 0.3 | 0.5 | 0.5 | |||
| Yes | 71.6 ± 16.4 | 76.5 ±19.9 | 74.1 ± 15.7 | |||
| No | 71.1 ± 17.2 | 75.6 ± 16.3 | 73.3 ± 16.1 | |||
| Sexual orientation disclosed to at least one relative or friend | 0.5 | 2.1 | 1.2 | |||
| Yes | 69.3 ± 15.7 | 80.7 ± 14.9* | 75.0 ± 17.0 | |||
| No | 68.1 ± 14.6 | 75.5 ± 14.7 | 71.8 ± 15.9 | |||
PCS, Physical Component Summary; MCS, Mental Component Summary; QOL, quality of life. Student’s t-test was used for data analysis.
* p < 0.05.
** p < 0.01.
Relationships between QOL, social support and demographic characteristics
To assess the relationships between QOL, social support, and demographic characteristics information, a hypothesized recursive SEM was used to estimate the magnitude and direction of the interdependent effects using the maximum likelihood estimation method. The goodness results of best fit SEM showed χ2 = 2083.47 (P<0.00), RMSEA = 0.07, CFI = 0.88, GFI = 0.83, NFI = 0.87, and AGFI = 0.89. We estimated the direct effects of one factor on the others by path coefficients proximal to the unidirectional. The item loads for the eight QOL domains were high (ranging from 0.61 to 0.85). The factor load between QOL and social support was 0.47, which was higher than the load between QOL and demographic characteristics. For social support, the item loads for psychosocial counseling and health education were 0.17 and 0.29, respectively. Demographic characteristics also had influence on social support, with a factor load of -0.65 and, marriage status (0.77) and age (0.71) exhibited greater item loads. The relationships between demographic characteristics and social support are shown in Fig 1.
Fig 1. The structural equation modeling of the factors that influence QOL among Chinese MSM.
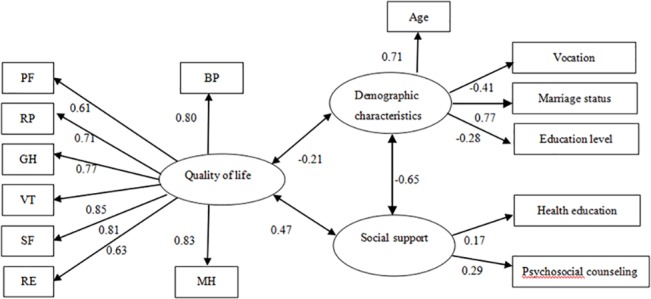
Path diagram illustrating the relationships between demographic and social support factors and QOL in Chinese MSM. Social support had the greatest impact on QOL, and demographic characteristics appeared to influence the likelihood of receiving social support.
Discussion
The results indicated that the SEM fit our data well. For the latent factors, social support had the greatest impact on QOL, and some demographic characteristics appear to influence the likelihood of receiving social support. For the observed variables, the item loads for health education and psychosocial counseling in social support were the highest and for the observed demographic factors, the greatest item loads were seen for marital status and age.
Social support was also related to physical and mental health in general populations in the world and also for individuals with HIV [21,26,35]. Effective social support can improve mental well-being, reduce substance abuse, and promote other positive health behaviors in MSM, whereas individuals who receive less social support are more likely to practice unsafe sex [36].
Homosexuality is not well accepted in China, and therefore MSM often self-isolate for fear of discrimination from society and family, which may lead to depression and decreased QOL [37,38]. Depression is known to negatively impact QOL and to accelerate disease progression in people living with HIV/AIDS [39,40]. Taken together, these findings suggest that social support should be actively implemented to reduce depression and enhance QOL in the Chinese MSM population.
Among the factors included in social support, health education and psychosocial counseling had the greatest impact on QOL. Bastardo and Kimberlin suggested that psychosocial support from professionals and non-professionals is a critical element of HIV care and can help enhance the QOL of patients in developing countries [41]. Social support and counseling to reduce stress have been found to effectively enhance interventions and reduce HIV-related high-risk behaviors in MSM [42,43]. Although the benefits of psychosocial counseling are obvious, only a small portion of the respondents (10.7%) in our study had received this type of support. Enhancing psychosocial counseling for Chinese MSM is an urgent priority that will likely be important in improving health status.
Our results also indicated the importance of health education in the MSM population. Mohamed and Mahfouz found that insufficient public health education for PLWHA resulted in misconceptions that may encourage engaging in risky behavior, such as not using condoms because they are perceived as only a contraceptive rather than a means to prevent STDs [44]. Psychosocial counseling and health education can also help reduce fear of taking the HIV test [45]. Furthermore, both HIV education and psychological counseling contributed to an increase in HIV testing in the MSM population [36]. Our results suggest that vigorously strengthening health education and psychosocial counseling programs could considerably improve QOL of the MSM population in China.
Other aspects of social support also showed great effectiveness in improving QOL in our study. For example, respondents that received STD testing had higher physical health scores. Hoover et al. proposed that increasing STD screening would greatly help to lower the prevalence of STDs in MSM in the United States [46]. Therefore, prevention programs that include STD testing should be implemented to enhance the health of the MSM population. Our study also found that concealment of sexual orientation from family and friends was associated with lower mental health scores, consistent with findings for Swedish MSM [12]. The traditional Chinese concept of filial piety and system of patrilineality may lead MSM to feel that they have failed in their duty to continue the paternal line and that they have disgraced their family, which likely increases stress in MSM and limits their willingness to disclose their sexual orientation to their family [47]. However, receiving emotional support from a family member or a sexual partner was shown to improve mental health in African American MSM [48], suggesting that emotional support from family or friends may improve the mental status of Chinese MSM.
We also found that certain demographic characteristics appeared to influence the likelihood of individuals receiving social support. Specifically, marital status and age strongly negatively correlated with social support. Many married Chinese men may not pursue HIV testing due to concern that their spouse or family members will discover their sexual orientation [49]. Fear of straining marital relationships and the possibilities of abandonment, divorce, or even violence have been identified as barriers for married MSM to pursue HIV testing [50,51]. Additionally, with increase in age, the initiative to seek social support declines [52].
This study has several limitations. Firstly, due to the social stigma of homosexuality in China and the consequent hidden nature of the MSM population, potential respondents may have decided not to participate in our study in order to protect their privacy, decreasing representation from more Chinese MSM. Secondly, the sample size was relatively small and the participants were recruited from only two cities in China and, therefore, may not be representative of all Chinese MSM. However, our study identified multiple factors that may influence QOL in MSM that can be addressed separately and in depth in future research.
Conclusion
Our study displayed the impact of social support on QOL in Chinese MSM and highlighted the urgent need to strengthen intervention efforts, with more emphasis on social support networks and programs to improve QOL, especially for older and married MSM.
Data Availability
All relevant data are within the paper.
Funding Statement
This study was supported by the National Natural Science Foundation of China (Grant Number 81273186 and 71473269). BQ received the funding.
References
- 1. Wu Z, Wang Y. Introduction: China meets new AIDS challenges. J Acquir Immune Defic Syndr. 2010;53 Suppl 1: S1–S3. 10.1097/QAI.0b013e3181c7d379 [DOI] [PubMed] [Google Scholar]
- 2. Li YZ, Xu JJ, Qian HZ, You BX, Zhang J, Zhang JM, et al. High prevalence of HIV infection and unprotected anal intercourse among older men who have sex with men in China: a systematic review and meta-analysis. BMC Infect Dis. 2014;14: 531 10.1186/1471-2334-14-531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guo Y, Li X, Stanton B. HIV-related behavioral studies of men who have sex with men in China: a systematic review and recommendations for future research. AIDS Behav. 2011;15: 521–534. 10.1007/s10461-010-9808-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang L, Zhang D, Yu B, Wang S, Liu Y, Wang J, et al. Prevalence of HIV Infection and Associated Risk Factors among Men Who Have Sex with Men (MSM) in Harbin, P.R. China. PLOS ONE. 2013;8: e58440 10.1371/journal.pone.0058440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu J, Hu Y, Jia Y, Su Y, Cui H, Liu H, et al. Prevalence of Unprotected Anal Intercourse among Men Who Have Sex with Men in China: An Updated Meta-Analysis. PLOS ONE. 2014;9: e98366 10.1371/journal.pone.0098366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chow EP, Gao L, Koo FK, Chen L, Fu X, Jing J, et al. Qualitative exploration of HIV-related sexual behaviours and multiple partnerships among Chinese men who have sex with men living in a rural area of Yunnan Province, China. Sex Health. 2013;10: 533–540. 10.1071/SH13097 [DOI] [PubMed] [Google Scholar]
- 7. Chow EP, Tucker JD, Wong FY, Nehl EJ, Wang Y, Zhuang X, et al. Disparities and Risks of Sexually Transmissible Infections among Men Who Have Sex with Men in China: A Meta-Analysis and Data Synthesis. PLOS ONE. 2014;9: e89959 10.1371/journal.pone.0089959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cao Z, Xu J, Zhang H, Song D, She M, Wang J, et al. Risk factors for syphilis among married men who have sex with men in China. Sex Transm Dis. 2014;4: 98–102. [DOI] [PubMed] [Google Scholar]
- 9. Zhang W, Han X, An M, Zhao B, Hu Q, Chu Z, et al. Identification and characterization of a novel HIV-1 circulating recombinant form (CRF59_01B) identified among Men-Who-Have-Sex-with-Men in China. PLOS ONE. 2014;9: e99693 10.1371/journal.pone.0099693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Amini Lari M, Faramarzi H, Shams M, Marzban M, Joulaei H. Sexual Dysfunction, Depression and Quality of Life in Patients With HIV Infection. Iran J Psychiatry Behav Sci. 2013;7: 61–68. [PMC free article] [PubMed] [Google Scholar]
- 11. Bucciardini R, Pugliese K, Weimer L, Digregorio M, Fragola V, Mancini M, et al. Relationship between health-related quality of life measures and high HIV viral load in HIV-infected triple-class-experienced patients. HIV Clin Trials. 2014;4: 176–183. 10.1310/hct1504-176 [DOI] [PubMed] [Google Scholar]
- 12. Li D, Jia Y, Ruan Y, Liu Y, Li Q, Liang H, et al. Correlates of incident infections for HIV, syphilis, and hepatitis B virus in a cohort of men who have sex with men in Beijing. AIDS Patient Care STDS. 2010;24: 595–602. 10.1089/apc.2010.0083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bouhnik AD, Préau M, Schiltz MA, Peretti-Watel P, Obadia Y, Lert F, et al. Unsafe sex with casual partners and quality of life among HIV-infected gay men: evidence from a large representative sample of outpatients attending French hospitals (ANRS-EN12-VESPA). Acquir Immune Defic Syndr. 2006;42: 597–603. [DOI] [PubMed] [Google Scholar]
- 14. Wong CF, Schrager SM, Holloway IW, Meyer IH, Kipke MD. Minority stress experiences and psychological well-being: the impact of support from and connection to social networks within the Los Angeles House and Ball communities. Prev Sci. 2014;15: 44–55. 10.1007/s11121-012-0348-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sandfort TG, de Graaf R, Bijl RV. Same-sex sexuality and quality of life: findings from the Netherlands Mental Health Survey and Incidence Study. Arch Sex Behav. 2003;32: 15–22. [DOI] [PubMed] [Google Scholar]
- 16. Safren SA, Blashill AJ, O'Cleirigh CM. Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS Behav. 2011;15: S30–S34. 10.1007/s10461-011-9898-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eriksson LE, Berglund T. Health-related quality of life in homo- and bisexual men attending a sexually transmitted disease clinic in Sweden. Int J STD AIDS. 2007;18: 207–211. [DOI] [PubMed] [Google Scholar]
- 18. Rao D, Chen WT, Pearson CR, Simoni JM, Fredriksen-Goldsen K, Nelson K, et al. Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int J STD AIDS. 2012;23: 481–484. 10.1258/ijsa.2009.009428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gielen AC, McDonnell KA, Wu AW, O'Campo P, Faden R. Quality of life among women living with HIV: the importance violence, social support, and self care behaviors. Soc Sci Med. 2001;52: 315–322. [DOI] [PubMed] [Google Scholar]
- 20. Srisurapanont M, Sombatmai S, Jarusuraisin N. HIV-seropositive results, health-related quality of life, and social support: a 24-week prospective study in Thailand. AIDS Patient Care STDS. 2001;15: 211–215. [DOI] [PubMed] [Google Scholar]
- 21. Yadav S. Perceived social support, hope, and quality of life of persons living with HIV/AIDS: a case study from Nepal. Qual Life Res. 2010;19: 157–166. 10.1007/s11136-009-9574-z [DOI] [PubMed] [Google Scholar]
- 22. Vyavaharkar M, Moneyham L, Corwin S, Tavakoli A, Saunders R, Annang L. HIV-disclosure, social support, and depression among HIV-infected African American women living in the rural southeastern United States. AIDS Educ Prev. 2011;23: 78–90. 10.1521/aeap.2011.23.1.78 [DOI] [PubMed] [Google Scholar]
- 23. Razavi P, Hajifathalian K, Saeidi B, Esmaeeli Djavid G, Rasoulinejad M, Hajiabdolbaghi M, et al. Quality of Life among Persons with HIV/AIDS in Iran: Internal Reliability and Validity of an International Instrument and Associated Factors. AIDS Res Treat. 2012;2012: 849406 10.1155/2012/849406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gallicchio L, Hoffman SC, Helzlsouer KJ. The relationship between gender, social support, and health-related quality of life in a community-based study in Washington County, Maryland. Qual Life Res. 2007;16: 777–786. [DOI] [PubMed] [Google Scholar]
- 25. Semple SJ, Strathdee SA, Zians J, Patterson TL. Factors associated with experiences of stigma in a sample of HIV-positive, methamphetamine-using men who have sex with men. Drug Alcohol Depend. 2012;125: 154–159. 10.1016/j.drugalcdep.2012.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang HH, Wu SZ, Liu YY. Association between social support and health outcomes: a meta-analysis. Kaohsiung J Med Sci. 2003;19: 345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ou F, Li K, Gao Q, Liu D, Li J, Hu L, et al. An urban neo-poverty population-based quality of life and related social characteristics investigation from northeast China. PLOS ONE. 2012;7: e38861 10.1371/journal.pone.0038861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. So WK, Leung DY, Ho SS, Lai ET, Sit JW, Chan CW. Associations between social support, prevalent symptoms and health-related quality of life in Chinese women undergoing treatment for breast cancer: a cross-sectional study using structural equation modelling. Eur J Oncol Nurs. 2013;17: 442–448. 10.1016/j.ejon.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 29. Mazaheri M. Structural equation model to predict subjective quality of life: a comparison of scales with different numerical anchoring. Iran J Psychiatry. 2012;5: 134–139. [PMC free article] [PubMed] [Google Scholar]
- 30. Fueki K, Yoshida E, Igarashi Y. A structural equation model relating objective and subjective masticatory function and oral health-related quality of life in patients with removable partial dentures. J Oral Rehabi. 2011;38: 86–94. [DOI] [PubMed] [Google Scholar]
- 31. Muñoz M, Sanz M, Pérez-Santos E, Quiroga Mde L. Proposal of a socio-cognitive-behavioral structural equation model of internalized stigma in people with severe and persistent mental illness. Psychiatry Res. 2011;186: 402–408. 10.1016/j.psychres.2010.06.019 [DOI] [PubMed] [Google Scholar]
- 32. Baker SR, Pankhurst CL, Robinson PG. Testing relationships between clinical and non-clinical variables in xerostomia: a structural equation model of oral health-related quality of life. Qual Life Res. 2007;16: 297–308. [DOI] [PubMed] [Google Scholar]
- 33. Yamamura S, Takehira R, Kawada K, Katayama S, Nishizawa K, Hirano M, et al. Structural equation modeling of qualification of pharmacists to improve subjected quality of life in cancer patients. J Pharm Pharm Sci. 2005;8: 544–551. [PubMed] [Google Scholar]
- 34. Tomarken AJ, Waller NG. Structural equation modeling: strengths, limitations, and misconceptions. Annu Rev Clin Psychol. 2005;1: 31–65. [DOI] [PubMed] [Google Scholar]
- 35. Mavandadi S, Zanjani F, Ten Have TR, Oslin DW. Psychological well-being among individuals aging with HIV: the value of social relationships. J Acquir Immune Defic Syndr. 2009;1: 91–98. 10.1097/QAI.0b013e318199069b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Deuba K, Ekstrom AM, Shrestha R, Ionita G, Bhatta L, Karki DK. Psychosocial Health Problems Associated with Increased HIV Risk Behavior among Men Who Have Sex with Men in Nepal: A Cross-Sectional Survey. PLOS ONE. 2013;8: e58099 10.1371/journal.pone.0058099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Feng MC, Feng JY, Chen TC, Lu PL, Ko NY, Chen YH. Stress, needs, and quality of life of family members caring for adults living with HIV/AIDS in Taiwan. AIDS Care. 2009;21: 482–489. 10.1080/09540120802290373 [DOI] [PubMed] [Google Scholar]
- 38. Sun W, Wu M, Qu P, Lu C, Wang L. Depressive symptoms in people living with HIV: Related factors Psychological well-being of people living with HIV/AIDS under the new epidemic characteristics in China and the risk factors: a population-based study. Int J Infect Dis. 2014;28: e147–e152. [DOI] [PubMed] [Google Scholar]
- 39. Gore-Felton C, Koopman C, Spiegel D, Vosvick M, Brondino M, Winningham A. Effects of quality of life and coping on depression among adults living with HIV/AIDS. Journal of Health Psychology. 2006;11: 711–729. [DOI] [PubMed] [Google Scholar]
- 40. Simoni JM, Safren SA, Manhart LE, Lyda K, Grossman CI, Rao D, et al. Challenges in addressing depression in HIV research: Assessment, cultural context, and methods. AIDS and Behavior. 2011;15: 376–388. 10.1007/s10461-010-9836-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bastardo YM, Kimberlin CL. Relationship between quality of life, social support and disease related factors in HIV-infected persons in Venezuela. AIDS Care. 2000;5: 673–684. [DOI] [PubMed] [Google Scholar]
- 42. Herbst JH, Sherba RT, Crepaz N, Deluca JB, Zohrabyan L, Stall RD, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39: 228–241. [PubMed] [Google Scholar]
- 43. Darbes LA, Chakravarty D, Beougher SC, Neilands TB, Hoff CC. Partner-provided social support influences choice of risk reduction strategies in gay male couples. AIDS Behav. 2012;16: 159–167. 10.1007/s10461-010-9868-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mohamed BA, Mahfouz MS. Factors Associated with HIV/AIDS in Sudan. Biomed Res Int. 2013;2013: 971203 10.1155/2013/971203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Oppong Asante K, Oti-Boadi M. HIV/AIDS knowledge among undergraduate university students: implications for health education programs in Ghana. Afr Health Sci. 2013;2: 270–277. 10.4314/ahs.v13i2.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hoover KW, Butler M, Workowski K, Carpio F, Follansbee S, Gratzer B, et al. STD screening of HIV-infected MSM in HIV clinics. Sex Transm Dis. 2010;12: 771–776. 10.1097/OLQ.0b013e3181e50058 [DOI] [PubMed] [Google Scholar]
- 47. Wang FT, Bih HD, Brennan DJ. Have they really come out: gay men and their parents in Taiwan. Cult Health Sex. 2009;11: 285–296. 10.1080/13691050802572711 [DOI] [PubMed] [Google Scholar]
- 48. Yang C, Latkin C, Tobin K, Patterson J, Spikes P. Informal social support and depression among African American men who have sex with men. J Community Psychol. 2013;41: 435–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Huang ZJ, He N, Nehl EJ, Zheng T, Smith BD, Zhang J, et al. Social network and other correlates of HIV testing: findings from male sex workers and other MSM in Shanghai, China. AIDS Behav. 2012;16: 858–871. 10.1007/s10461-011-0119-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chirawu P, Langhaug L, Mavhu W, Pascoe S, Dirawo J, Cowan F. Acceptability and challenges of implementing voluntary counselling and testing (VCT) in rural Zimbabwe: Evidence from the Regai Dzive Shiri Project. AIDS Care. 2010;22: 81–88. 10.1080/09540120903012577 [DOI] [PubMed] [Google Scholar]
- 51. Mlay R, Lugina H, Becker S. Couple counselling and testing for HIV at antenatal clinics: Views from men, women and counsellors. AIDS Care. 2008;20: 356–360. 10.1080/09540120701561304 [DOI] [PubMed] [Google Scholar]
- 52. Stephenson R, Chard A, Finneran C, Sullivan P. Willingness to use couples voluntary counseling and testing services among men who have sex with men in seven countries. AIDS Care. 2014;26: 191–198. 10.1080/09540121.2013.808731 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.


