Abstract
The ramifications of patient migration toward the foot of the bed in intensive care units are not well understood. Migration may cause shear and friction between the patient and the mattress, reduce elevation of the patient's torso, and require frequent repositioning of the patient. This study assesses how bed design impacts both the amount of migration that patients undergo during head section articulation to 30° and 45° and the extent of torso compression following the articulation.
Keywords: hospital bed design, low back injuries, patient migration, patient repositioning, pressure ulcers, safe patient handling
THE impact of patient migration toward the foot of the bed in hospitalized patients is not well understood. There are at least 2 causes of this migration: gravity over time and bed design. During head-of-bed elevation, some bed designs may mechanically push patients toward the foot section of the bed. Whether caused by gravity over time or from bed design, migration may be deleterious to the patient due to increased shear and friction between the patient and the mattress and by a reduction in therapeutic torso angle. Patient migration may also be deleterious to the caregiver by requiring more pull-up in bed maneuvers, which have been shown to cause musculoskeletal disorders in health care professionals.
The prevention of pressure ulcers (PUs) in the health care environment has been a quality care focus for many years. There are intrinsic patient factors that contribute to skin breakdown such as age-related deterioration of skin, muscle, and nerve cells, conditions that affect perfusion such as vascular disease and diabetes, and circulation issues that reduce oxygenation levels in the skin and muscle.1–3 Extrinsic support surface–related PU risk factors, which include increased pressure, shear, friction, heat, and moisture, have also been identified.4–7 Patient migration that causes movement across the mattress has a high probability of increasing shear and friction forces between the patient's body and the support surface.1,8
Reducing shear and friction has long been a goal of nursing care with current clinical interventions including the use of sliding sheets, a “lift” rather than “slide” repositioning approach, and others.4–7 However, there is limited information regarding the role that bed design may have in reducing or increasing the sliding that occurs both during head-of-bed elevation and flattening of the bed.
Therapeutic head-of-bed elevation has been shown to reduce the effort to breathe during ventilator weaning,9 increase Pao2/Fio2 ratios,10 increase end-expiratory lung volume,10 and prevent aspiration of gastric contents into the lungs11 and is one of the first interventions in early mobilization protocols.12 When patients migrate toward the foot of the bed, even if the bed remains at the desired 45° position, the patient's torso may flatten to the extent that it no longer receives the benefits of the head-of-bed elevation. What is not currently understood is the effect that raising the head of the bed has on patient movement and torso compression.
Patient migration is problematic not just for the patient but also for caregivers. When a patient slides down the bed, a nurse must reposition the patient toward the head of the bed. Repositioning patients can be a repetitive task, with reported frequencies for a nurse as much as 10 times per shift13 or more than 20 times per week.14 The US Occupational Safety and Health Administration15 reports that, in 2010, nursing aides, orderlies, and attendants had the highest rates of musculoskeletal disorders with an incidence rate of 249 per 10 000 workers (total of 27 020 cases). This was more than 7 times the average across all industries. “Lifting a patient in bed” was a patient-handling task that was identified as “high risk” in its report. The American Nursing Association has recently developed standards for safe patient handling and mobility aimed at eliminating manual patient handling to create safer work environments for its members.16 Technology that reduces the need for “pull-up in bed” maneuvers, therefore, may be beneficial to both patients and caregivers.
Understanding patient migration may encourage better bed design and provide objective data to allow health care providers to make informed decisions about bed purchases. Reducing migration may reduce the incidence of nosocomial PUs, allow patients to maintain therapeutic head-of-bed positioning, and protect caregivers by reducing the number of times they have to reposition the patient. The objective of this study was to evaluate patient migration of nonobese individuals during head-of-bed articulations in 4 commonly used intensive care unit (ICU) beds with different head-of-bed pivot designs.
METHODS
Study approach
This study investigated how patient migration and torso compression were impacted by bed design as the head of bed was elevated and returned to the flat position, using motion capture methods recently developed by Kotowski and associates.17 This method used a motion capture system (MotionAnalysis, Santa Rosa, California) that quantified the instantaneous 3-dimensional position of 7 markers placed on the subject's body at specified bony anatomic locations and 6 markers on the bed (Figure). Video data were collected and analyzed using Cortex software (Motion Analysis, Santa Rosa, CA). During head-of-bed articulation, the anatomic markers were compared with the stable markers placed on each of 4 ICU beds to determine relative movement. Two different bed articulations were studied: (1) 0-30-0 head of bed raised from flat to 30° to flat and (2) 0-45-0 head of bed raised from flat to 45° to flat. Each articulation condition was repeated 5 times in a random order. In total, 40 trials were completed by each participant (4 bed types × 2 articulation types × 5 repeats).
Figure.

Motion marker positions for a participant positioned on the bed including 7 markers on the body and 6 markers on the bed. Reprinted with permission from Kermit Davis. Copyright November 10, 2014, Kermit Davis, University of Cincinnati, Cincinnati, Ohio.
Subjects
To mimic the hospitalized population, 12 healthy volunteers (6 males and 6 females) were recruited who met height and weight stratification requirements. The 6 height-weight classifications were as follows: (1) tall-average weight; (2) tall-overweight; (3) average height-average weight; (4) average height-overweight; (5) short-average weight; and (6) short-overweight. The height categories were defined by short—below 25th percentile (males <171 cm, females <157 cm), average—26th to 75th percentiles (males >171 cm and <180 cm, females >157 cm and <166 cm), and tall—above the 76th percentile (males >180 cm, females >166 cm) for males and females, respectively. Weight categories were defined on the basis of body mass index with average weight (<25 kg/cm2) and overweight (between 25 and 30 kg/cm2). Obese individuals were not recruited for this study because of limited ability to locate bony landmarks for motion capture markers.
Procedure
Subjects received a full explanation of the study procedures that included instruction that they should try to act like a comatose patient during bed articulations and not to make any attempts to reposition themselves. The study was approved by the university institutional review board. The sequence of the beds was counterbalanced in random order for each subject, whereas the individual articulation conditions were randomized within each of the beds. Prior to each trial, subjects were anatomically aligned on each bed by making sure that the trochanter was positioned on the bed as designated by the manufacturer.
Outcome variables
The independent variables were bed types and articulation. Four different bed types were evaluated: bed A (Hill-Rom Progressa with StayInPlace Technology and integrated Therapy mattress) was designed with a head pivot that slides backward simultaneously with a head section that extends when the head of bed is raised; bed B (Hill-Rom Progressa without the StayInPlace feature with an integrated Therapy mattress) had the head pivot sliding with no lengthening of the head section when raising the head of bed; bed C (Linet Multicare with Virtuoso mattress, EU version) had a simple stationary head pivot where the head-of-bed section pivots around when the head of bed is raised; and bed D (Stryker InTouch with XPRT mattress) had 2 hinge points for the head pivot where the head-of-bed pivot changes from one pivot point to a second pivot at 20°.
The dependent variables consisted of the following: (1) net displacement quantified both how much movement toward the foot of bed occurred at the highest point during the articulation (net displacement—head-of-bed up) and the displacement at the end of the articulation when the bed returned to flat (net displacement—returned to flat); (2) cumulative movement was the total amount of movement of the anatomic site during the entire articulation (summation of any movement, down and up, during elevation of head of bed and when returning to flat); (3) torso compression was the maximum decrease in distance between the shoulder and trochanter markers during the articulation. Larger values indicated that torso compression was increasing. This measure provided an objective assessment of the amount of scrunching or balling up of the participant from head-of-bed elevation; (4) perceived sliding assessed the subject's perception of sliding during the articulation conditions as assessed at the end of the trial condition on an integral scale with 1 (none) to 10 (sliding several inches); (5) perceived discomfort was assessed at the end of the trial condition for any region in the body with an integral scale of 0 (no discomfort) to 10 (most unbearable pain imaginable); and (7) subject preference ranking allowed subjects to rank the 4 beds in order of best (or most desirable) to worst (least desirable) (from 1 to 4) after they had completed all 4 bed trials.
For each trial, the exact position of the trochanter and ankle was calculated by using the motion capture markers in the recorded data relative to the head, seat (thigh), and foot sections of the bed, respectively.
Statistical analyses
Descriptive statistics (means and standard deviations) were computed for all of the outcome variables as function of bed and bed by articulation interaction. A repeated-measures analysis of variance was completed on each dependent variable to identify whether there were significant effects of bed type and articulation type. Post hoc analyses in the form of Tukey standardized honest difference tests were conducted to identify the source of differences between beds.
RESULTS
Subject demographics
The 6 female subjects had an average age of 35.0 (SD = 11.5) years, standing height of 164.9 (SD = 5.9) cm, and average body weight of 63.1 (SD = 14.1) kg. The 6 male subjects were 23.8 (SD = 9.7) years old, 175.8 (SD = 9.5) cm tall, and weighed 77.3 (SD = 11.2) kg.
Study design measures
The 4 beds differed significantly in the amount of net displacement, cumulative movement, and torso compression (Table 1).
Table 1. Mean (SD) for Patient Migration and Torso Compression as Function of Bed Design and Articulation (0-30-0 and 0-45-0)a.
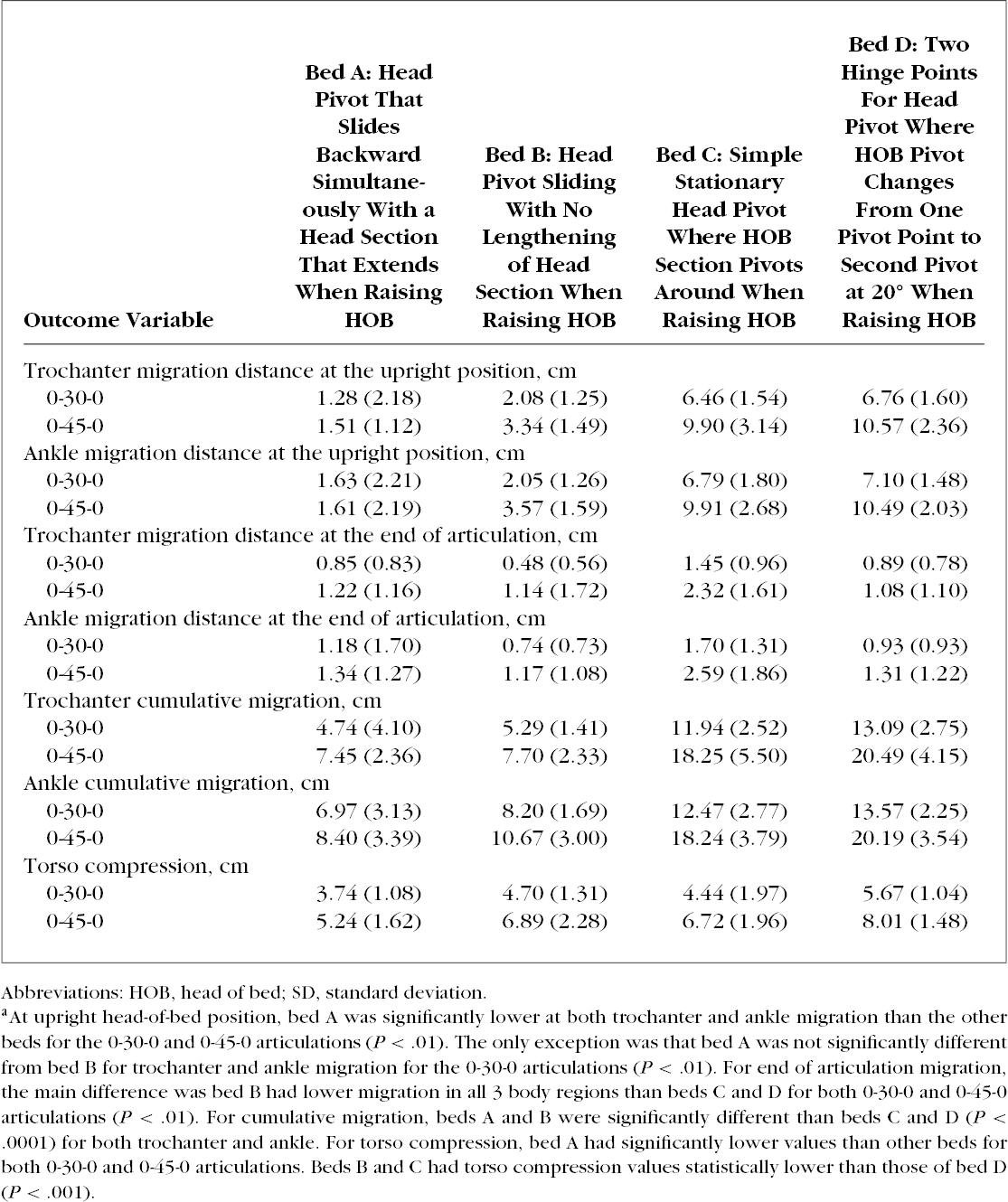
Net displacement—Head-of-bed up
When the head of bed was fully raised during the head-of-bed articulation at 0-30-0, the trochanter migrated significantly more (P < .0001) on beds C and D (6.5 and 6.8 cm, respectively) than on beds A and B, with the least migration for bed A at 1.3 cm and for bed B at 2.1 cm. The 0-45-0 articulation had more pronounced differences than the 0-30-0 articulation, with beds C and D significantly higher (P < .0001) at 9.9 and 10.6 cm, respectively, than beds A and B, with the least migration for bed A at 1.5 cm and for bed B at 3.3 cm. Ankle migration showed similar trends to the trochanter and was also significantly higher (P < .0001) for beds C and D (6.8 and 7.1 cm, respectively) at the 0-30-0 head-of-bed elevation than for beds A at 1.6 cm and for bed B at 2.0 cm. Ankle migration at the 0-45-0 articulation was 9.9 and 10.5 cm for beds C and D, respectively, which was higher than for bed A at 1.6 cm and for bed A at 3.6 cm (P < .0001).
Net displacement—Returned to flat
When the bed returned to flat, less net migration was seen than the head-of-bed up data. Mean trochanter distances on each of the 4 beds ranged from 1.1 to 2.3 cm during the 45° elevation, which was explained by patients moving back toward the head of the bed as the bed returned to flat.
Cumulative movement
Cumulative movement, which measured the entire movement of the anatomic marker during the articulation, was significantly higher (P < .0001) at the trochanter for beds C and D (12.0 and 13.0 cm, respectively) for the 0-30-0 articulation and was even higher (18.2 and 20.5 cm, respectively) for the 0-45-0 articulation, which differed significantly (P < .0001) from bed A with the least movement (4.7 cm at 0-30-0 and 7.4 cm at 0-45-0) and bed B (5.3 cm for 0-30-0 articulation and 7.7 cm for 0-45-0). Ankle migration showed similar differences in cumulative movement.
Torso compression
Bed A demonstrated significantly less torso compression than all other beds for both the 0-30-0 and the 0-45-0 articulations at 3.7 cm (P < .001) and 5.2 cm, respectively, (P < .001). Bed D was significantly higher in torso compression than bed A, B, or C (P < .001). There were no statistical differences between beds B and C for this outcome measure.
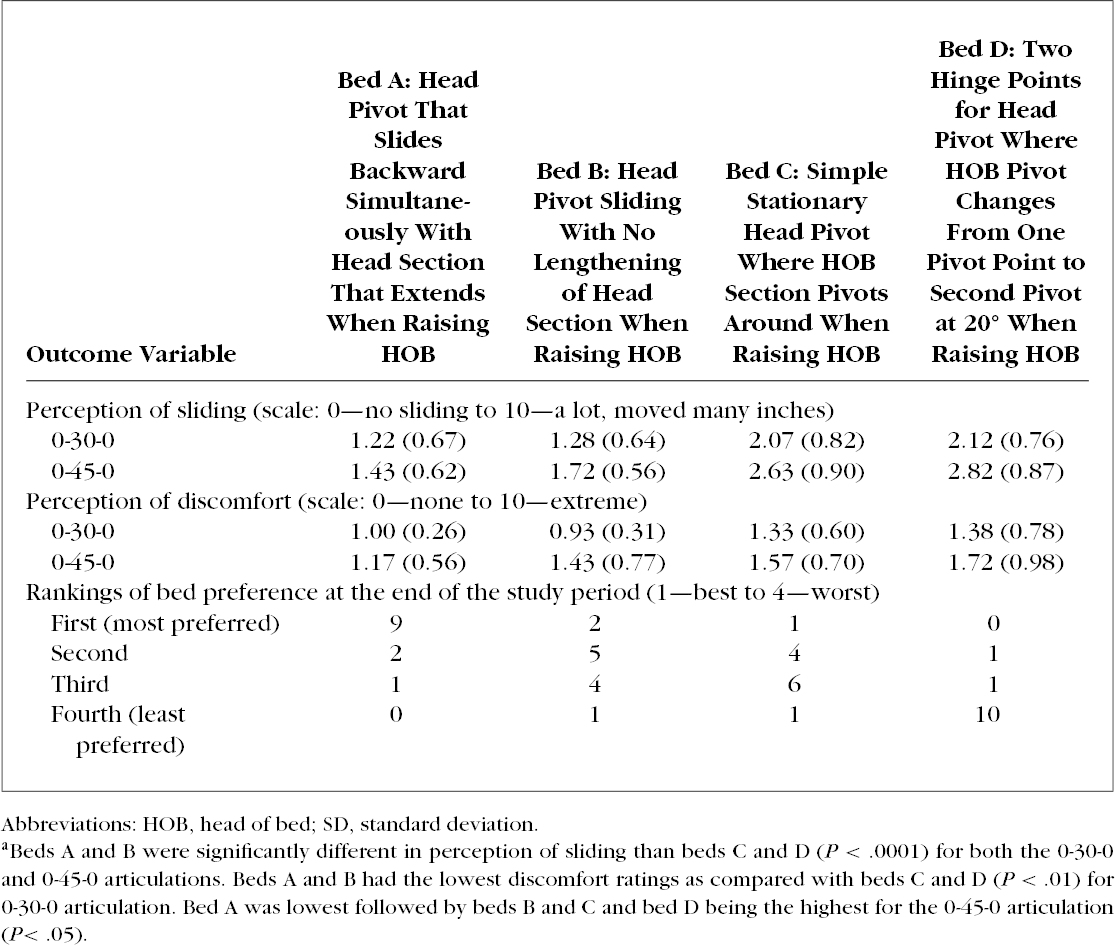
Perceptions of sliding and discomfort
Beds A and B were perceived by subjects to have significantly less sliding than beds C and D (by about 50% relative amount). Discomfort was more variable. Although it is important to note that the response level at most indicated only mild pain. These values also reflect a few participants having no discomfort in any trial.
Subject preference rankings
When ranking the beds for preference, 9 of 12 subjects ranked bed A as most preferred (Table 2). The least desirable bed was bed D, with 10 of 12 participants ranking bed D the worst. It is interesting to note that preference was similar to objective data outcomes.
Table 2. Mean (SD) for Subjective Outcome Variables as Function of Bed Design and Articulation (0-30-0 and 0-45-0) and Subject Ranking of Bed Preferencea.
DISCUSSION
Bed design, specifically head-of-bed pivot design, influenced how subjects migrated down the bed in this study. When subjects were articulated from flat to 45°, beds C and D demonstrated around 10 cm of migration at the peak of the articulation and subjects moved a total of 18 to 20 cm (cumulative migration) as the head of bed returned to flat. Bed A, which has a more complex head-of-bed pivot that elongates, had 86% less migration at the peak of articulation and 60% less cumulative movement than bed D, which, given the magnitude of the distance traveled, is likely a clinically significant finding.
Motion capture methods, which were developed by Kotowski and associates,17 provide objective video data that were analyzed to quantify movement of anatomic locations during head-of-bed articulation. Although actual patient data in a clinical setting may have been desired, actual patients would not have been able to undergo the 40 head-of-bed articulations and 4 bed transfers that were required for this testing. In addition, these methods, which were strengthened by the within subjects design, repeated conditions, and quantitative data, require a controlled laboratory environment.
This objective assessment provides the foundation to accurately assess the movement of subjects with the “best” bed minimizing migration, cumulative movement, and torso compression. Bed A was identified as the bed that minimized the most of the metrics, whereas bed D had the highest amount of migration at the head-of-bed up position, cumulative movement, and torso compression.
Bed A had 3 key characteristics of the frame design that minimized the outcome variables: (1) a complex head section pivot point; (2) a head section that lengthens as the head of bed rises; (3) knee auto contour (which is an automatic rising of the knee section during head-of-bed elevation). The complex pivot point and lengthening head section cradled the patient and accommodated the natural elongation of the torso during the articulation. The knee pivot auto contour also reduced migration of the patient toward the foot of the bed by providing a small “stop” for the thighs. The combination of these features was likely why bed A minimized both migration and torso compression. Bed B, which had a sliding head pivot but lacked lengthening of the head section, had significantly improved migration and cumulative movement as compared with beds C and D and was slightly worse that bed A.
As the head pivot design becomes simpler, the patient migration significantly increased during the articulation, which resulted in greater cumulative movement. Beds C and D had 4 to 5 times as much migration down the bed compared with beds A and B when the bed was articulated up to the upright position. This translated into 2 to 4 times as much cumulative movement. Bed C had a simple stationary head pivot, whereas bed D had 2 hinge points for the head pivot where head of bed pivot changes from one pivot point to a second pivot at 20°. In both cases, the head pivot articulation was simple and resulted in more movement of the patient (eg, pushed the patient down the bed). Both of these beds did not have any auto contour for the knee pivot during these traditional head-of-bed elevations. Even without auto contour, the articulations for beds C and D produced the most torso compression. This basically means that the shoulders are pushed toward the foot of the bed as well as down toward the lower torso and at a rate faster than the lower torso, compressing the torso by 7 to 8 cm.
Although shear and friction were not directly measured in this study, it is logical that a repetitive 18- to 20-cm movement across the mattress may increase the risk of PUs over time. The movement was measured at the trochanter and the ankle, which anatomically would demonstrate the movement for the buttocks and sacral regions and the heel, which are the most common areas for nosocomial PUs to develop.18
One of the benefits of reducing patient migration during head-of-bed elevation is the potential to limit manual lifting and patient-handling tasks, which are known causes of injuries and musculoskeletal disorders in nurses and other health care workers. The injuries sustained by health care workers have been reported as often life-altering and career-ending.16 Epidemiologic studies have found that repositioning patients accounts for between 25% and 50% of all low back injuries for nurses18–22 and has been identified as one of the worst tasks that nurses complete during their shifts.13,23–29 Biomechanical laboratory studies that estimated the spine loads on caregivers using sophisticated models have indicated that repositioning was among the worst patient-handling tasks performed by health care providers.30–33 All of these load estimates exceeded the recommended load tolerance estimates,34,35 indicating that the expected loads would be risky for the majority of the individuals performing these tasks (eg, health care providers).
A simple yet practical method to determine how much migration occurs when raising the head of a bed is to put a piece of tape on the bed that is lined up with the ankle, then raise the head of bed and measure how far down the ankle slid down the bed. A simple method for measuring torso compression would be to measure the original distance between the shoulder and the hip when the bed is in a supine position with a string and elevate the head of the bed with the string in place. Greater slack in the string would correspond to greater torso compression. With the importance of reducing PUs and low back injuries in caregivers, these simple metrics may lead to better outcomes and objective decision making.
CONCLUSION
Bed design significantly impacts the amount of migration during head-of-bed articulations. Migration, cumulative movement, and torso compression were higher on beds with simple head section pivot designs that lack the ability to elongate and slide backward. Increased migration may increase the risk of PUs for patients and increase the risk of low back injuries for caregivers. Torso compression may impact patient comfort. Designers of beds can use these results to improve on traditional and simple head-of-bed pivots.
A practical application of this study may be to visually assess the movement of the heels (to estimate migration) and assess the change in distance between the shoulders and the trochanter (to estimate torso compression) when deciding to purchase ICU beds. However, objective measurements are the only true way to understand the impact of head section articulation on a patient.
Footnotes
This project was funded by Hill-Rom, Inc.
The authors declare there is no conflict of interest. The funding was received through normal research channels, and neither author has a vested interest in Hill-Rom, Inc.
REFERENCES
- 1.Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord. 1996;34(5):255–263. [DOI] [PubMed] [Google Scholar]
- 2.Coleman S, Gorecki C, Nelson EA, et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. 2013;50(7):974–1003. [DOI] [PubMed] [Google Scholar]
- 3.Adult obesity facts. Centers for Disease Control and Prevention Web site; http://www.cdc.gov/obesity/data/adult.html. Accessed June 15, 2014. [Google Scholar]
- 4.Rappl LM. Management of pressure by therapeutic positioning. In: Wound Care: A Collaborative Practice Manual for Health Professionals. 4th ed. Baltimore, MD: Wolters Kluwer/Lippincott Williams & Wilkins; 2012:278–308. [Google Scholar]
- 5.National Pressure Ulcer Advisory Panel. Pressure Ulcer Prevention Quick Reference Guide. http://www.npuap.org/wp-content/uploads/2012/02/Final_Quick_Prevention_for_web_2010.pdf. Accessed August 15, 2014.
- 6.International Review: Pressure Ulcer Prevention Pressure Shear and Friction and Microclimate in Context. A Consensus Document. London, England: Wounds International; 2010. http://www.woundsinternational.com/pdf/content_8925.pdf. Assessed September 10, 2014. [Google Scholar]
- 7.Sterner E, Lindholm C, Berg E, Startk A. Category I pressure ulcers: how reliable is clinical assessment? Orthop Nurs. 2011;30(3):194–205. [DOI] [PubMed] [Google Scholar]
- 8.Hess CT. Did you know? The difference between friction and shear. Adv Skin Wound Care. 2004;17(5):222 http://journals.lww.com/aswcjournal/fulltext/2004/06000/did_you_know__the_difference_between_friction_and.6.aspx. Assessed September 8, 2014. [Google Scholar]
- 9.Deye N, Lellouch F, Maggiore SM, et al. The semi-seated position slightly reduces the effort to breathe during difficult weaning. Intensive Care Med. 2013;39(1):85–92. [DOI] [PubMed] [Google Scholar]
- 10.Dellamonica J, Lerolle N, Sargetini C, et al. Effect of different seated positions on lung volume and oxygenation in acute respiratory distress syndrome. Intensive Care Med. 2013;39(6):1121–1127. [DOI] [PubMed] [Google Scholar]
- 11.Drakulovic MB, Torres A, Bauer TT, et al. Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomized trial. Lancet. 1999;354(9193):1851–1858. [DOI] [PubMed] [Google Scholar]
- 12.Micheletti L. Safe mobility for ICU patients; to prevent negative outcomes, the care plan should include progressive positioning and mobility exercises. Advanced Health care Network for Nurses Web site; http://nursing.advanceweb.com/Continuing-Education/CE-Articles/Safe-Mobility-for-ICU-Patients.aspx. Assessed September 11, 2014. [Google Scholar]
- 13.Vasihadou A, Karvountzis GG, Soumilas A, Roumeliotis D, Theodosopoulou E. Occupational low-back pain in nursing staff in a Greek hospital. J Adv Nurs. 1995;21(1):125–130. [DOI] [PubMed] [Google Scholar]
- 14.Lynch RM, Freund A. Short-term efficacy of back Injury intervention project for patient care providers at one hospital. AIHAJ. 2000;61(2):290–294. [DOI] [PubMed] [Google Scholar]
- 15.Safe patient handling. US Occupational Safety and Health Administration Web site; https://www.osha.gov/SLTC/healthcarefacilities/safepatienthandling.html. Accessed August 15, 2014. [Google Scholar]
- 16.WebsiteSafe patient handling and mobility standards. American Nurses Association Web site; http://nursingworld.org/Safe-Patient-Handling-and-Mobility. Assessed August 15, 2014. [Google Scholar]
- 17.Kotowski SE, Davis KG, Wiggermann N, Williamson R. Quantification of patient migration in bed: catalyst to improve hospital bed design to reduce shear and friction forces and nurses' injuries. Hum Factors. 2013;55(1):36–47. [DOI] [PubMed] [Google Scholar]
- 18.VanGilder C, MacFarlane GD, Harrison P, Lachenbruch C, Meyer S. The demographics of suspected deep tissue injury in the United States: an analysis of the International Pressure Ulcer Prevalence Survey 2006-2009. Adv Skin Wound Care. 2010;23(6):254–261. [DOI] [PubMed] [Google Scholar]
- 19.Harber P, Billet E, Gutowski M, SooHoo K, Lew M, Roman A. Occupational low back pain in hospital nurses. J Occup Environ Med. 1985;27(7):518–524. [PubMed] [Google Scholar]
- 20.Knibbe JJ, Frielle RD. The use of logs to assess exposure to manual handling of patients, illustrated in an intervention study in home care nursing. Int J Ind Ergon. 1996;24(4):445–454. [Google Scholar]
- 21.Leighton DJ, Reilly T. Epidemiological aspects of back pain: the incidence and prevalence of back pain in nurses compared to the general population. Occup Med. 1995;45(5):263–267. [DOI] [PubMed] [Google Scholar]
- 22.Randall SB, Pories WJ, Pearson A, Drake DJ. Expanded Occupational Safety and Health Administration 300 log as metric for bariatric patient-handling staff injuries. Surg Obes Relat Dis. 2009;5(4):463–468. [DOI] [PubMed] [Google Scholar]
- 23.Hignett S. Work-related back pain in nurses. J Adv Nurs. 1996;23(6):1238–1246. [DOI] [PubMed] [Google Scholar]
- 24.Yip Y. A study of work stress, patient handling activities and the risk of low back pain among nurses in Hong Kong. J Adv Nurs. 2001;36(6):794–804. [DOI] [PubMed] [Google Scholar]
- 25.Kjellberg K, Lagerström M, Hagberg M. Patient safety and comfort during transfers in relation to nurses' work technique. J Adv Nurs. 2004;47(3):251–259. [DOI] [PubMed] [Google Scholar]
- 26.Nelson A, Baptiste AS. Evidence-based practices for safe patient handling and movement. Clin Rev Bone Miner Metab. 2006;4:55–69. [Google Scholar]
- 27.Smedley J, Inskip H, Buckle P, Cooper C, Coggon D. Epidemiological differences between back pain of sudden and gradual onset. J Rheumatol. 2005;32(3):528–532. [PubMed] [Google Scholar]
- 28.Pompeii LA, Lipscomb HJ, Schoenfisch AL, Dement JM. Musculoskeletal injuries resulting from patient handling tasks among hospital workers. Am J Ind Med. 2009;52(7):571–578. [DOI] [PubMed] [Google Scholar]
- 29.Smedley J, Egger P, Cooper C, Coggon D. Manual handling activities and risk of low back pain in nurses. Occup Environ Med. 1995;52(3):160–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Looze MP, Zinzen E, Caboor D, et al. Effect of individually chosen bed-height adjustments on the low-back stress of nurses. Scand J Work Environ Health. 1994;20(6):427–434. [DOI] [PubMed] [Google Scholar]
- 31.Jang R, Karwowski W, Quesada PM, et al. Biomechanical evaluation of nursing tasks in a hospital setting. Ergonomics. 2007;50(11):1835–1855. [DOI] [PubMed] [Google Scholar]
- 32.Marras WS, Davis KG, Kirking BC, Bertsche PK. A comprehensive analysis of low-back disorder risk and spinal loading during the transferring and repositioning of patients using different techniques. Ergonomics. 1999;42(7):904–926. [DOI] [PubMed] [Google Scholar]
- 33.Winkelmolen GHM, Landeweerd JA, Drost MR. An evaluation of patient lifting techniques. Ergonomics. 1994;37(5):921–932. [DOI] [PubMed] [Google Scholar]
- 34.Waters TR, Anderson VP, Garg A, Fine MJ. Revised NIOSH equation for the design and evaluation of manual lifting tasks. Ergonomics. 1993;36(7):749–776. [DOI] [PubMed] [Google Scholar]
- 35.McGill SM. The biomechanics of low back injury: implications on current practice in industry and the clinic. J Biomech. 1997;30(5):465–475. [DOI] [PubMed] [Google Scholar]


