At long last, we are finally making progress in our understanding of necrotizing enterocolitis (NEC). As the readership of this journal is well aware, despite all the successes of neonatal intensive care, the mortality and morbidity of NEC has remained largely unchanged. However, the past decade has seen new ground being broken in all areas of NEC research, including early diagnosis, medical and surgical management of acute NEC, and rehabilitation of those with a complicated disease course.
NEC is one of the few diseases that we still diagnose based on radiological and/or histopathological findings. Needless to say, by the time characteristic radiological findings of unrestricted bacterial overgrowth such as pneumatosis, or those of peritonitis such as fixed bowel loops and ascites are detected, or if the patient is already at a stage where histopathology is available as a diagnostic option (the infant has already had a visit to the operating room), it may be a bit too late for an ‘intestine-saving’ intervention. The lack of early-stage biomarkers has also limited our ability to enroll patients into clinical trials of new treatments at a stage when tissue can still be saved, the systemic inflammatory response can still be prevented, and yet be certain that the patient actually has NEC and not feeding intolerance due to immaturity or an alternative etiology such as septic ileus.
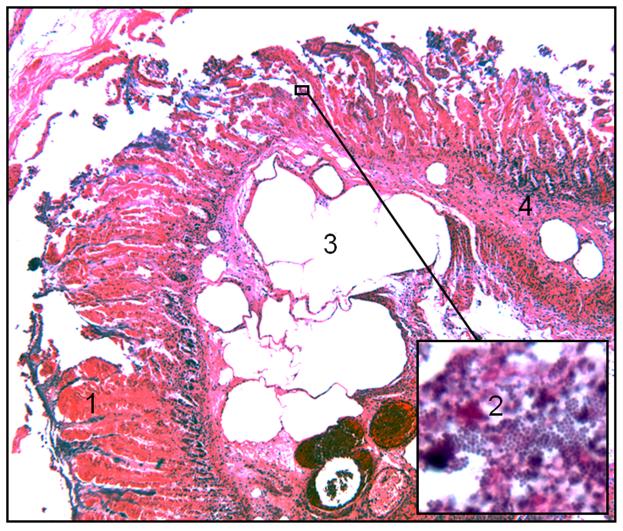
NEC is also one of the few diseases that derive their description from characteristic histopathological findings. Epidemiologically, the risk factors may originate in utero, such as chorioamnionitis and placental insufficiency; at the time of birth such as perinatal asphyxia; or later, such as indomethacin therapy, viral infections, and blood transfusions. Such diversity of risk factors is by no means unique to NEC and may possibly be the case with every condition that derives its identity in its pathoanatomy, such as cirrhosis of the liver, where viruses, alcohol, and toxins can all lead to the same histoarchitectural change. NEC, which is defined by the presence of coagulative necrosis, bacterial overgrowth, pneumatosis, and a cellular inflammatory response (Fig. 1), may also represent a situation where the pathoanatomy points not to a single etiological pathway but may instead represent a generic tissue injury response of the gastrointestinal tract at a specific stage of development. Philosophically, this realization can help in shaping our expectations – if NEC is indeed a group of several distinct nosological entities, treatment efforts may need to be tailored to each sub-group. We may also have to accept that we may never eliminate NEC completely- as we control today’s causes of NEC, it is possible that new causes will appear in time as our patient population and practices change.
Fig. 1.
Photomicrograph from a hematoxylin & eosin-stained tissue section of NEC. The diagnosis of NEC rests on the detection of characteristic histopathological features: coagulative necrosis (1), bacterial overgrowth (2), pneumatosis (3), and a cellular inflammatory response (4).
In this issue of the Clinics, our attempt has been to focus on some of the major dilemmas that all of us face in the NICU. We hope that you will enjoy the chapters by Drs. Ambalavanan and Ramani, Sharma and Hudak, and Christensen on the role of feeding, clinical presentations of NEC, and the changing face of NEC in full-term neonates, respectively. The chapters on gut microbiome and inflammatory signaling by Drs. Neu and DePlaen summarize the current state of the science in the laboratory. Drs. Sherman, Moore, and Ng, Chan, and Poon bring us authoritative descriptions of some of the most exciting developments in this field. Our own groups have contributed chapters on probiotics and on short bowel syndrome, and finally, Drs. Mangus and Subbarao bring you everything you ever wanted to know (but were afraid to ask) about intestinal transplantation.
Acknowledgments
We wish to thank Dr. Lucky Jain for his encouragement to bring out this volume, Kerry Holland, Senior Editor, for all her support, and Nicole Congleton, for editorial assistance. We, of course, are indebted to and grateful to the authors whose contributions will be fully appreciated by the readers, and to our families (Ritu, Jayant, and Vikram; and Tim, Christopher, Connor, Mia, Brianna, and Adia) for their enduring support.
Contributor Information
Patricia Wei Denning, Division of Neonatal-Perinatal Medicine, Department of Pediatrics, Emory University School of Medicine, 2015 Uppergate Drive, Atlanta, GA 30322, USA.
Akhil Maheshwari, University of Illinois at Chicago, 840 South Wood Street, CSB 1257, Chicago, IL 60612, USA.