Abstract
Purpose
In high-dose-rate (HDR) brachytherapy (BT), the source dwell times and dwell positions are essential treatment planning parameters. An optimal choice of these factors is fundamental to obtain the desired target coverage with the lowest achievable dose to the organs at risk (OARs). This study evaluates relevant dose parameters in cervix brachytherapy in order to assess existing tandem-ring dwell time ratio used at the first HDR BT center in Nigeria, and compare it with an alternative source loading pattern.
Material and methods
At the Radiotherapy Department, University College Hospital (UCH), Ibadan, Nigeria, a total of 370 standard treatment plans in two alternative sets were generated with HDR basic 2.6 software for one hundred and eighty five cervical cancer patients. The initial 185 individual plans were created for clinical treatment using the tandem-ring dwell time ratio of 1 : 1. Modifying the initial applicator loading ratio, the second set of plans with related dose data were also obtained for study purposes only. Total reference air kerma (TRAK), total time index (TTI), ICRU volume, treatment time, point B dose, ICRU bladder dose, and rectal points dose were evaluated for both sets of plans.
Results
The means of all evaluated dose parameters decreased when the existing tandem-ring dwell time ratio (1 : 1) was modified to other dwell weightings (1 : 1 – 3 : 1). These reductions were 13.43% (ICRU volume), 9.83% (rectal dose), 6.68% (point B dose), 6.08% (treatment time), 5.90% (TRAK), 5.88% (TTI), and 1.08% (bladder dose). Correspondingly, coefficients of variation changed by –7.98%, –5.02%, –5.23%, –4.20%, –3.93%, 8.65%, and 3.96% from the existing pattern to the alternative one.
Conclusion
Tandem-ring dwell time ratio has significant influence on dosimetric parameters. This study has indicated the need to modify the existing planning approach at UCH.
Keywords: brachytherapy, cervical cancer, dwell time, high-dose-rate, tandem-ring
Purpose
The advantage of brachytherapy (BT) over external beam radiotherapy (EBRT) is that the source is placed in immediate vicinity of the tumor, hence no entrance dose and rapid dose fall off the distance [1]. Intracavitary brachytherapy (ICBT) is an integral part of the treatment of cervical cancer [2]. To ensure uniformity in reporting ICBT, International Commission on Radiation Units and Measurement (ICRU) in its report 38 proposed some parameters adequate for reporting a procedure instead of only the dose prescription at point ‘A’ [3]. These include the dimensions of the ICRU reference volume, the dose to the rectum, bladder, pelvic walls, and dose to the lymphatic trapezoid. However, a survey by Pötter et al. indicated that all these parameters are usually not reported in the clinical practice or in literature [4]. Dose specification in ICBT is mainly based on Stockholm, Paris, and Manchester prescription systems [5, 6]. Optimum applicator placement is critical in maximizing local control and minimizing toxicity. It is important to choose an applicator that can optimally treat the disease and can be placed in an anatomically distorted vagina [7]. At the Department of Radiotherapy, University College Hospital (UCH), Ibadan, Nigeria, the tandem-ring applicator used is from Bebig Germany. Ring applicators are particularly useful when the vaginal fornices are asymmetric or absent, and because they have reproducible geometry and are easy to insert [8, 9]. The limitation of Bebig's ring applicators used at our centre is that they are not attachable to a rectal retractor, which increases the distance of the source positions to the rectal mucosa, thereby enabling dose reduction. This function is performed with the use of gauze vaginal packing, which sometimes is not optimal.
It is well documented in literature that in cervix brachytherapy both tumor response and complication rate are dose-dependent [10–14]. Applicator loading ratio and shape of the reference isodose (isodose line through point ‘A’) vary considerably between institutional standard plans. The use of equal (1 : 1) dwell time weighting between the tandem and ring of the applicator, and only two activated dwell positions on each side of the ring was introduced to UCH for standard BT planning during commissioning of the facility in 2008 by the visiting physicist appointed by the International Atomic Energy Agency (IAEA). This work is therefore a comparison study of two alternative loading patterns; a clinically used one and a studied one by evaluating Total Reference Air Kerma (TRAK), Total Time Index (TTI), total treatment time, ICRU isodose dimensions and volume; and doses to bladder, rectum, and the reference point ‘B’. The results of this study will give direction on how to enhance critical organ sparing in the treatment of cervical cancer patients receiving high-dose-rate (HDR) BT without the use of rectal retractor. It will also provide baseline data for other centres with this type of HDR BT technology.
Material and methods
Between July 2008 and December 2012, one hundred and eighty five patients with cervical cancer (Stages IIA to IIIB) who underwent a total of 555 ICBT applications at UCH, Nigeria, were included in this study. Approval for the study was obtained from the institution's ethical review committee. The treatment for cervical cancers at our center consists of external beam radiotherapy (EBRT) with Theratron 780C telecobalt unit (MDS Nordian, Canada Inc) and brachytherapy. External beam radiotherapy was delivered in 12 fractions of 45 Gy, while for brachytherapy, a total dose of 15-21 Gy in three equal fractions at weekly interval was given to the reference point ‘A’ using Bebig's Cobalt-60 (Eckert & Ziegler BEBIG, GmbH, Germany). Following EBRT, vaginal examination is usually done to ensure effective tumor shrinkage before HDR BT. A C-arm X-ray machine was utilized for verification of applicator positioning prior to treatment delivery. There were some difficulties in finding the ICRU rectal reference point on lateral C-arm X-ray images due to the lack of rectal retractor in our ring applicator. A rectal retractor helps in obtaining the magnification or diminution factor on the lateral film, and also marks the posterior vaginal wall, so that rectal points can be easily determined. Visualization of the posterior wall on lateral radiographs is often difficult, even with the use of gauze soaked in contrast, as a result of fatty pelvic tissues in most of the cervical cancer patients. Therefore, a re-usable rectal marker (Fig. 1) fabricated at Groote Schuur Hospital, Cape Town, South Africa was introduced subsequently in the study duration for rectum localization. Three points (1 cm apart) along the marker and around the intersection of the IUT with the ring were used on lateral radiographs as against a single point recommended by the ICRU. The points were identified only on the y and z co-ordinates of the radiograph. ICRU reference point for bladder on frontal radiograph (x co-ordinate) is the geometric center of the Foley's urethral catheter with the balloon filled with radiopaque contrast media. On lateral image (y and z co-ordinates), the point is located at the center of the posterior surface of the balloon. Therefore, the study commenced with evaluation of 5 dose parameters on individual standard plans followed by bladder and rectal doses determination. All patients had three weekly applicator insertions preceding treatment delivery. Evaluation of doses at OARs was carried at different number of fractions across patients. Brachytherapy patients prior to the availability of the rectal marker were not assessed for rectal dose. In cases where the first fraction implants showed satisfactory organs at risk sparing, such orthogonal radiographs were used as reference for subsequent applicator insertions without dose evaluation in further fractions. Therefore, only OARs doses evaluated in three or two HDR BT fractions were averaged and used for comparisons between the two dwell time patterns. To determine the point for rectal dose calculation, a re-usable rectal marker (Fig. 1) was used to locate 3 rectal points 1 cm apart (for averaging), and symmetric in relation to the anterior/posterior line passing through the middle of the intravaginal sources, for dose calculations on TPS. The lengths (tandem) and diameters (ring) of the applicators shown on radiographs were used to determine magnification factors for OARs positional coordinates before use on standard plans of individual patients.
Fig. 1.
Re-usable rectal marker for localizing rectum during applicator placement
Existing (fixed) tandem-ring loading ratio
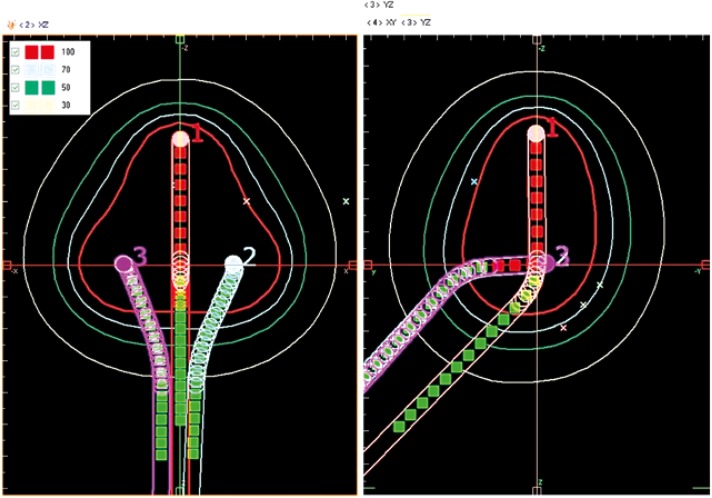
Following dose prescription and source loading on the applicators, a peer-shaped treatment isodose curve (Fig. 2) was obtained showing dose distribution using standard planning on HDR basic (version 2.6) treatment planning system (TPS) of fixed step size, 0.5 cm between dwell positions. Therefore, activated source positions on the intra-uterine part of the applicator are 4, 8, and 12 for the 2 cm, 4 cm and 6 cm tandems, respectively. Our standard loading pattern follows use of 50% of total treatment time by each of the applicator components (intra-uterine tandem, IUT and the ring, R). Hence, each of the ring sides (left and right) uses 25% of the total time. Dwell time weighting between both components is always 1 : 1, irrespective of IUT length (Fig. 3). Therefore, dwell times within the IUT or ring are same, but different across the two parts.
Fig. 2.
Standard plan showing dose distributions around a ring applicator. The reference points A and B (front al bladder point inclusive) are on the anterior view, the three rectal points and the ICRU bladder point are displayed on the lateral view with isodose lines descriptions
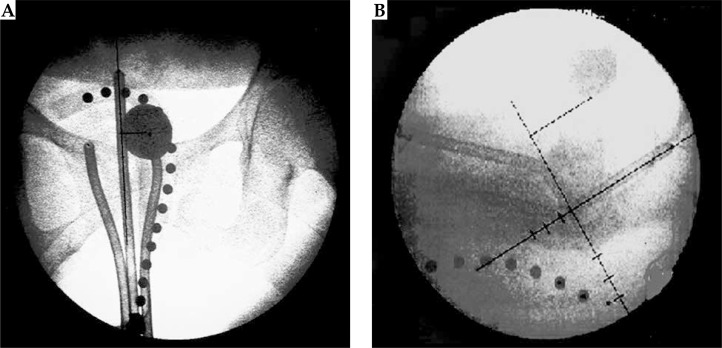
Fig. 3.
Orthogonal radiographs showing tandem-ring positioning in patients, ICRU bladder reference point (on both views) and rectal marker points (only on lateral view)
Proposed (varying) tandem-ring loading ratios
For the purpose of study, initial 185 standard treatment plans were modified by giving all dwell positions in a given ring applicator same dwell times. As such, dwell time weightings (ratios) between the tandem and the ring vary depending on length of the intrauterine tube. Consequently, the ratios of total dwell time in tandem to that in ring are 3 : 1 (6 cm tandem), 2 : 1 (4 cm tandem), and 1 : 1 (2 cm tandem) as illustrated in Tables 1–3. Therefore, standard plans involving the shortest IUT (2 cm) share the features of both loading patterns, since dwell weighting is 1 : 1 and dwell times are uniform across the two applicator components. This is due to same number of (4) dwell positions in each. Thus, while the dwell times of a vaginal ring differ from (greater than) those of the IUT in the existing loading pattern, the values are uniform for all dwell positions in the alternative system. The former maintains fixed (1 : 1) total dwell time share, but the loading ratio varies (1 : 1 – 3 : 1) in the latter.
Table 1.
Existing and proposed dwell time patterns in ring applicator with 6 cm intra-uterine (IU) tandem. IUTT/RT is 1 : 1 (existing approach) and 3 : 1 (proposed approach)
| Dwell points | From tip [cm] | X-pos [cm] | Y-pos [cm] | Z-pos [cm] | Existing pattern Dwell time [s] | Proposed pattern Dwell time [s] |
|---|---|---|---|---|---|---|
| Intra-uterine (6 cm) applicator | ||||||
| 1 | 0.68 | –0.01 | 0.04 | –5.24 | 66.87 | 83.09 |
| 2 | 1.18 | –0.01 | 0.03 | –4.74 | 66.87 | 83.09 |
| 3 | 1.68 | –0.01 | 0.01 | –4.24 | 66.87 | 83.09 |
| 4 | 2.18 | –0.01 | 0.00 | –3.74 | 66.87 | 83.09 |
| 5 | 2.68 | –0.01 | 0.01 | –3.24 | 66.87 | 83.09 |
| 6 | 3.18 | –0.01 | 0.02 | –2.74 | 66.87 | 83.09 |
| 7 | 3.68 | –0.01 | 0.03 | –2.24 | 66.87 | 83.09 |
| 8 | 4.18 | –0.01 | 0.05 | –1.74 | 66.87 | 83.09 |
| 9 | 4.68 | –0.01 | 0.06 | –1.24 | 66.87 | 83.09 |
| 10 | 5.18 | –0.01 | 0.07 | –0.74 | 66.87 | 83.09 |
| 11 | 5.68 | –0.01 | 0.08 | –0.24 | 66.87 | 83.09 |
| 12 | 6.18 | –0.01 | 0.10 | 0.26 | 66.87 | 83.09 |
| 802.44 (13.37 min) | 997.03 (16.62 min) | |||||
| Right ring (30 mm) applicator | ||||||
| 1 | 0.68 | 1.73 | 0.50 | 0.15 | 200.61 | 83.09 |
| 2 | 1.18 | 1.73 | 1.00 | 0.14 | 200.61 | 83.09 |
| 401.22 (6.69 min) | 166.17 (2.77 min) | |||||
| Left ring (30 mm) applicator | ||||||
| 1 | 0.68 | –1.69 | 0.43 | 0.24 | 200.61 | 83.09 |
| 2 | 1.18 | –1.69 | 0.93 | 0.24 | 200.61 | 83.09 |
| 401.22 (6.69 min) | 166.17 (2.77 min) | |||||
Table 3.
Existing and proposed dwell time patterns in ring applicator with 2 cm tandem. IUTT/RT is 1 : 1 in both cases
| Dwell points | From tip [cm] | X-pos [cm] | Y-Pos [cm] | Z-pos [cm] | Existing pattern Dwell time [s] | Proposed pattern Dwell time [s] |
|---|---|---|---|---|---|---|
| Intra-uterine (2 cm) applicator | ||||||
| 1 | 0.68 | 0.05 | –0.04 | –1.47 | 186.17 | 186.17 |
| 2 | 1.18 | 0.05 | –0.06 | –0.97 | 186.17 | 186.17 |
| 3 | 1.68 | 0.05 | –0.08 | –0.47 | 186.17 | 186.17 |
| 4 | 2.18 | 0.05 | –0.09 | 0.03 | 186.17 | 186.17 |
| 744.68 (12.41 min) | 744.68 (12.41 min) | |||||
| Right ring (30 mm) applicator | ||||||
| 1 | 0.68 | 1.50 | 0.08 | 0.06 | 186.17 | 186.17 |
| 2 | 1.18 | 1.51 | 0.58 | 0.09 | 186.17 | 186.17 |
| 372.34 (6.21 min) | 372.34 (6.21 min) | |||||
| Left ring (30 mm) applicator | ||||||
| 1 | 0.68 | –1.49 | 0.10 | 0.04 | 186.17 | 186.17 |
| 2 | 1.18 | –1.46 | 0.60 | 0.07 | 186.17 | 186.17 |
| 372.34 (6.21 min) | 372.34 (6.21 min) | |||||
Table 2.
Existing and proposed dwell time patterns in ring applicator with 4 cm intra-uterine (IU) tandem. IUTT/RT is 1 : 1 (existing approach) and 2 : 1 (proposed approach)
| Dwell points | From tip [cm] | X-pos [cm] | Y-pos [cm] | Z-pos [cm] | Existing attern Dwell time [s] | Proposed pattern Dwell time [s] |
|---|---|---|---|---|---|---|
| Intra-uterine (4 cm) applicator | ||||||
| 1 | 0.68 | –0.02 | –0.06 | –3.44 | 69.17 | 85.49 |
| 2 | 1.18 | –0.02 | –0.06 | –2.94 | 69.17 | 85.49 |
| 3 | 1.68 | –0.02 | –0.06 | –2.44 | 69.17 | 85.49 |
| 4 | 2.18 | –0.02 | –0.06 | –1.94 | 69.17 | 85.49 |
| 5 | 2.68 | –0.02 | –0.06 | –1.44 | 69.17 | 85.49 |
| 6 | 3.18 | –0.02 | –0.06 | –0.94 | 69.17 | 85.49 |
| 7 | 3.68 | –0.02 | –0.06 | –0.44 | 69.17 | 85.49 |
| 8 | 4.18 | –0.02 | –0.06 | 0.06 | 69.17 | 85.49 |
| 553.38 (9.22 min) | 683.95 (11.40 min.) | |||||
| Right ring (30 mm) applicator | ||||||
| 1 | 0.68 | 1.43 | 0.26 | 0.21 | 138.34 | 85.49 |
| 2 | 1.18 | 1.45 | 0.76 | 0.23 | 138.34 | 85.49 |
| 276.69 (4.62 min) | 170.99 (2.85 min) | |||||
| Left ring (30 mm) applicator | ||||||
| 1 | 0.68 | –1.55 | 0.34 | 0.03 | 138.34 | 85.49 |
| 2 | 1.18 | –1.52 | 0.84 | 0.05 | 138.34 | 85.49 |
| 276.69 (4.62 min) | 170.99 (2.85 min) | |||||
The ICRU had recommended that the treatment volume encompassed by the reference isodose should be determined and reported [2]. The dimensions of the height, width (on frontal views), and thickness (lateral view) of the ICRU reference isodose related to the fractional dose of treatment were measured directly on the treatment plans of each of the patients. The reference isodose volume was obtained as the product of these values by (1):
| 1 |
The total reference air kerma under the current and alternative dwell time ratio patterns was obtained using (2):
| 2 |
Total time index (TTI) was calculated using equation (3) given by Williamson and Nath [15]:
| 3 |
All parameters including the reference isodose volumes were re-evaluated following modification of the loading ratio on initial standard treatment plans. The paired two-sided Student's t-test was performed for comparison of the seven dose parameters across the two loading patterns using the SPSS software (version 10, IBM, USA). A p-value of less than 0.05 (95% CI) was considered statistically significant.
Results
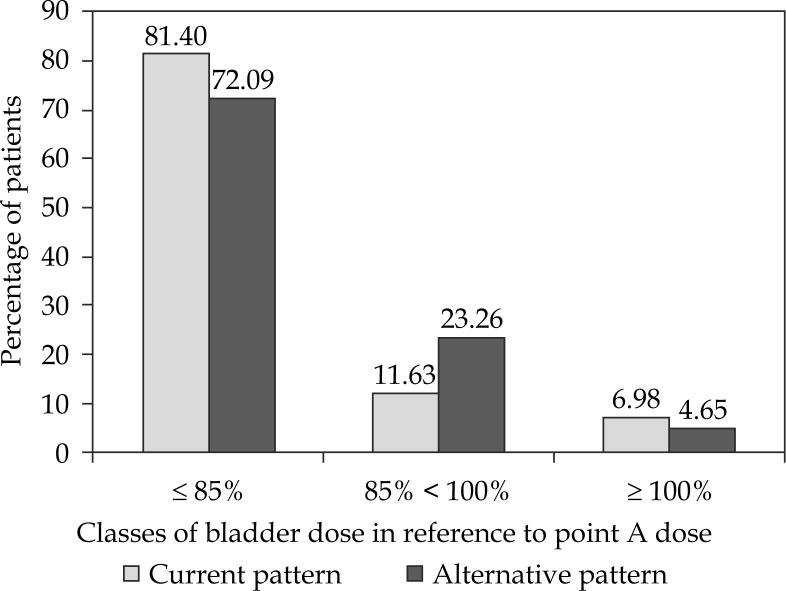
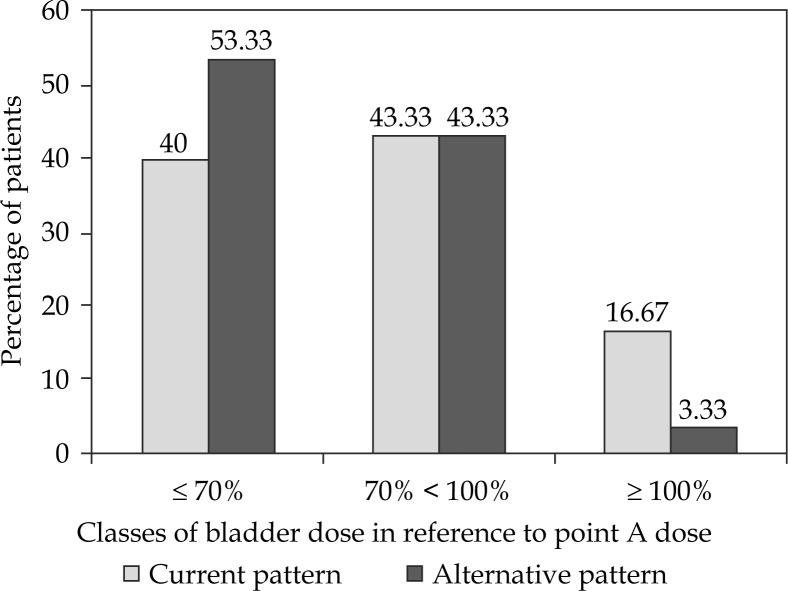
Comparisons of the two dwell time patterns in patients whose bladder and rectal doses were assessed in two and three fractions are presented in Tables 4 and 5, respectively. Further analysis of OAR doses by checking proportions of patients in different dose classes are given in Figures 4 and 5 below. Table 6 presents comparative statistics of all dose parameters from both patterns. The present work revealed that the means of all evaluated quantities decreased when the current tandem-ring dwell time pattern (1 : 1) was modified to an alternative design (1 : 1 – 3 : 1). The percentage reductions obtained were 13.43% (ICRU volume), 9.83% (rectal dose), 6.68% (point B dose), 6.08% (total treatment time), 5.90% (TRAK), 5.88% (TTI), 1.08% (bladder dose). Coefficients of variation, CV (Table 6) were determined to assess data variability for further comparisons of both dwell time patterns. The percentage differences in CV were 7.98%, 5.02%, 5.23%, 4.20%, 3.93%, 8.65%, and 3.96%, respectively. Comparisons of the ICRU reference isodose dimensions in the two loading patterns are shown in Table 7.
Table 4.
Sum of doses at point ‘A’ and associated bladder doses from two different dwell time patterns
| Dose/# (Gy) | Tumour (point A) dose (Gy) | n | Minimum Bladder dose, Gy (%) | Maximum Bladder dose, Gy (%) | Mean Bladder dose, Gy (%) | |||
|---|---|---|---|---|---|---|---|---|
| Existing pattern | Proposed pattern | Existing pattern | Proposed pattern | Existing pattern | Proposed pattern | |||
| 7 | 21 (3#s) | 34 | 5.57 (26.52) | 4.79 (22.81) | 23.88 (113.71) | 25.16 (119.81) | 13.54 ± 4.11 (64.48) | 13.56 ± 4.63 (64.57) |
| 6 | 18 (3#s) | 3 | 7.66 (42.56) | 6.58 (36.56) | 8.84 (49.11) | 8.14 (45.22) | 7.70 ± 1.12 (42.78) | 7.18 ± 0.84 (39.89) |
| 5, 5, 7 | 17 (3#s) | 1 | 5.92 (34.82) | 5.52 (32.47) | Not applicable | Not applicable | Not applicable | Not applicable |
| 5 | 15 (3#s) | 5 | 7.55 (50.33) | 7.76 (51.73) | 20.94 (139.60) | 20.94 (139.60) | 13.39 ± 5.33 (89.25) | 12.90 ± 5.25 (86.00) |
| 7 | 14 (2#s) | 30 | 4.73 (33.79) | 4.61 (32.93) | 23.39 (167.07) | 23.06 (164.71) | 10.87 ± 5.32 (77.64) | 10.74 ± 5.29 (76.71) |
| 6.5 | 13 (2#s) | 1 | 4.18 (32.15) | 4.18 (32.15) | Not applicable | Not applicable | Not applicable | Not applicable |
| 6 | ||||||||
| 12 (2#s) | 9 | 3.06 (25.5) | 2.97 (24.75) | 16.64 (138.67) | 15.98 (133.17) | 9.06 ± 5.34 (75.49) | 8.85 ± 4.98 (73.75) | |
| 5 | ||||||||
| 10 (2#s) | 30 | 4.09 (40.9) | 5.19 (51.90) | 19.28 (192.8) | 19.64 (196.40) | 9.58 ± 4.33 (95.81) | 10.13 ± 4.29 (101.30) | |
n – number of patients
Table 5.
Sum of doses to tumor (point ‘A’) and associated rectal doses from the two dwell time patterns
| Dose/# (Gy) | Tumour dose (Gy) | n | Minimum Rectal dose, Gy (%) | Maximum Rectal dose, Gy (%) | Mean Rectal dose, Gy (%) | |||
|---|---|---|---|---|---|---|---|---|
| Existing pattern | Proposed pattern | Existing pattern | Proposed pattern | Existing pattern | Proposed pattern | |||
| 7 | 21 (3#s) | 26 | 6.55 (31.19) | 6.27 (29.86) | 23.51 (111.95) | 23.51 (111.95) | 15.53 ± 4.24 (73.95) | 13.98 ± 3.66 (66.57) |
| 6 | ||||||||
| 18 (3#s) | 1 | 10.43 (57.94) | 10.19 (56.61) | Not applicable | Not applicable | Not applicable | Not applicable | |
| 5 | 15 (3#s) | 3 | 10.59 (70.60) | 9.90 (66.00) | 15.43 (102.87) | 13.27 (88.47) | 12.63 ± 2.51 (84.22) | 11.43 ± 1.71 (76.20) |
| 7 | ||||||||
| 14 (2#s) | 25 | 7.00 (50.00) | 6.86 (49.00) | 17.03 (121.64) | 15.04 (107.43) | 11.64 ± 2.60 (83.17) | 10.22 ± 1.99 (73.00) | |
| 6.5 | 13 (2#s) | 1 | 7.62 (58.62) | 7.62 (58.62) | Not applicable | Not applicable | Not applicable | Not applicable |
| 6 | 12 (2#s) | 5 | 6.50 (54.17) | 5.78 (48.17) | 10.55 (87.92) | 9.81 (81.75) | 8.92 ± 1.74 (74.31) | 7.65 ± 1.58 (63.75) |
| 5 | 10 (2#s) | 9 | 7.05 (70.50) | 6.44 (64.40) | 11.46 (114.60) | 10.59 (105.90) | 8.78 ± 1.38 (87.79) | 7.42 ± 1.18 (74.20) |
n – number of patients
Fig. 4.
Comparison of the current and proposed dwell time systems with respect to the total bladder dose expressed as percentage of prescription dose at point ‘A’
Fig. 5.
Comparison of the current and proposed dwell time systems with respect to the total rectum dose expressed as percentage of prescription dose at point ‘A’
Table 6.
Comparative statistics of the seven dose parameters obtained under the existing and proposed patterns
| Dose parameters | n | Min. | Max. | Mean | CV (%) | r | p-value |
|---|---|---|---|---|---|---|---|
| Point B dose I (%) | 185 | 17.40 | 28.90 | 23.82 ± 1.64 | 6.88 | 0.802 | 0.000 |
| Point B dose II (%) | 185 | 17.20 | 28.10 | 22.23 ± 1.45 | 6.52 | ||
| TRAK I (cGy m−2) | 185 | 0.224 | 0.551 | 0.373 ± 0.073 | 19.57 | 0.974 | 0.000 |
| TRAK II (cGy m−2) | 185 | 0.211 | 0.510 | 0.351 ± 0.066 | 18.80 | ||
| Total time I (min) | 185 | 7.98 | 32.28 | 18.43 ± 5.48 | 29.73 | 0.989 | 0.000 |
| Total time II (min) | 185 | 7.50 | 28.73 | 17.31 ± 4.93 | 28.48 | ||
| TTI I (Gy m2 s)/(h Gy) | 185 | 0.104 | 0.332 | 0.187 ± 0.045 | 24.06 | 0.985 | 0.000 |
| TTI II (Gy m2 s)/(h Gy) | 185 | 0.113 | 0.332 | 0.176 ± 0.046 | 26.14 | ||
| ICRU volume I (cm3) | 185 | 96.94 | 272.11 | 157.98 ± 28.12 | 17.80 | 0.860 | 0.000 |
| ICRU volume II (cm3) | 185 | 94.08 | 255.68 | 136.77 ± 22.40 | 16.38 | ||
| Bladder dose I (%) | 113 | 25.50 | 192.80 | 64.05 ± 25.21 | 39.36 | 0.998 | 0.132 |
| Bladder dose II (%) | 113 | 22.81 | 196.40 | 63.36 ± 25.93 | 40.92 | ||
| Rectal dose I (%) | 70 | 31.19 | 121.64 | 74.29 ± 19.37 | 26.07 | 0.992 | 0.000 |
| Rectal dose II (%) | 70 | 29.86 | 111.95 | 66.99 ± 16.59 | 24.76 |
I – existing pattern, II – proposed pattern, CV – coefficient of variation
Table 7.
Comparisons of the reference (100%) isodose dimensions in the two patterns
| ICRU isodose dimensions | Mean | r | p-value |
|---|---|---|---|
| Reference width I (cm) | 6.36 ± 0.89 | 0.990 | 0.680 |
| Reference width II (cm) | 6.32 ± 0.89 | ||
| Reference height I (cm) | 6.07 ± 0.26 | 0.680 | 0.000 |
| Reference height II (cm) | 5.58 ± 0.38 | ||
| Reference thickness I (cm) | 4.10 ± 0.43 | 0.990 | 0.000 |
| Reference thickness II (cm) | 3.90 ± 0.40 | ||
| Reference volume I (cm3) | 157.98 ± 28.12 | 0.860 | 0.000 |
| Reference olume II (cm3) | 136.77 ± 22.40 |
I – existing pattern, II – proposed pattern
Discussion
Quality assurance in cervical cancer brachytherapy entails reducing doses to the OARs as low as reasonably achievable. Radiation protection suggests maximizing the number of patients having OARs doses lower than set limits, and on the other hand, minimizing the proportion having doses higher than required. In this work, dose limits 85% (bladder) and 70% (rectum) of prescription dose at point ‘A’ were adopted to make comparisons between the two dwell time patterns. With the existing dwell time system, greater proportions of patients received total OARs doses equal or above 100% of point A dose, than the alternative pattern (Figs. 4 and 5). This undesirable trend is more pronounced for rectum. Besides, the current (fixed) dwell time ratio, resulted in average rectum dose considerably higher than bladder's (Table 6). This is not acceptable since the urinary tract has a higher tolerance to radiation than the gastrointestinal area. With plan modification to the alternate dwell time pattern, the sizable gap between the mean values is substantially reduced. This is because increasing the tandem time, which implies shortening of the dwell time used by the ring enlarges the isodose volume cranially from point A, and enlarges the upper part of the pear, thereby reducing dose to the posterior rectal canal. It is therefore evident that this change in approach will engender greater decline in dose for the rectum (9.83%) than the bladder (1.08%). Same maximum doses obtained in both patterns for the two OARs (Tables 4 and 5) were due to use of the shortest (2 cm) IUT, whereby applicator loading time is unchanged (Table 3). Applicator dwell time ratios in standard HDR BT planning vary among institutions. The use of 1 : 1 dwell time weighting between the ring and IUT components of the intracavitary applicator at our center had been assessed by evaluating 7 parameters associated with radiation protection of ICBT patients. These are doses to reference point B, bladder and rectum, and related parameters including TRAK, total treatment time, TTI, ICRU reference isodose dimensions, and volumes. Some of these are often not reported in clinical practice due to logistic reasons in carrying out estimations, especially in a department with large patient workload and limited personnel. Evaluation of an alternate loading pattern, whereby the tandem uses more of the total treatment time than the ring (depending on total dwell positions), showed decreased values for all parameters considered in this study. These differences are statistically significant (p = 0.000 at 95% CI), except for bladder dose (p = 0.132). As such, use of uniform dwell times in all dwell positions (proposed system) will engender less dose to bladder and the reference point ‘B’ in proximity to the pelvic bones. More importantly, considerable dose reduction to the rectum will result, while maintaining same dose at point A. This attributes to decrease in the dwell times for ring (vaginal) sources, which resulted in reduction of the width of the reference volume pertinent to doses at OAR, particularly the rectum. Additionally, in comparison with the existing dwell time system, less irradiation (treatment) time per HDR fraction and lower integral dose to patients and personnel (portrayed by reduction in values of TRAK and TTI) will be achieved when the alternative approach is used. In a previous study, Çetingöz et al. [16] assessed volume parameters, total treatment time, and the dose distribution variations in rectum, bladder, and point-B reference point having modified dwell times for 0.25 and 0.5 cm dwell positions using Plato TPS and a Microselectron Ir-192 unit (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden). The results of the present work showed similar trends with theirs. In our study (of 5 mm step size), the bladder reference dose was not changed considerably with different dwell times weightings as in the study of Çetingöz et al. The study of Çetingöz et al. had also shown decrements of 14% and 17% in the volume parameter for 0.25 cm and 0.5 cm steps, respectively, while all the evaluated dose parameters were decreased with increasing dwell time ratios of uterine source to vaginal colpostats. The percentage rectal dose, DR % in same study decreased with increasing dwell time ratios of uterine tandem by 23% and 28% for 0.25 cm and 0.5 cm dwell positions, respectively when compared between 1 : 1 and 4 : 1 weightings. Total Reference Air kerma is the sum of the products of the reference air kerma-rate and the irradiation time for each source. It is directly proportional to the amount of radiation delivered to the patient and the environment, hence relevant to radioprotection. The amount of radiation given by different treatment approaches can be compared directly using the TRAK. It is therefore a vital quantity, which should be used for reporting all BT applications [4]. From the foregoing, it is desirable to obtain minimum TRAK in BT plans while maintaining the prescribed dose at point A. An advantage of the HDR technique over the LDR method is shorter irradiation time per treatment fraction (in minutes), as hours or days in the latter. Shorter treatment time is preferable in brachytherapy, as there is lower degree of applicator movement during dose delivery. Our study also showed that current approach in standard treatment plan design at UCH entails longer irradiation time per HDR fraction than the varying dwell ratios system. This explains why TRAK has higher values with the existing dwell time pattern since it is proportional to irradiation time, which normally raises the degree of scattered radiation. Another significant parameter related to TRAK scarcely mentioned in literature is the total time index (TTI), which gives the average TRAK over all dwell positions per unit dose. It is also related to the integral dose to the patient, but presents no information on the shape of dose distribution. The main difficulty in cervix BT is minimizing doses at OAR and also including the whole tumor volume in the reference volume. Although, the standard dose at point A is maintained while changing dwell weightings, decrease in target coverage will result as indicated by the reduced ICRU reference volume (Tables 6 and 7) in the alternate dwell time system. However, the study of Basu et al. [17] hints at the possibility of gaining wider target coverage with the use of Manchester-style (tandem-ring) applicator – in comparison to the Fletcher-style applicator – at the cost of an increased dose to the urinary bladder. Moreover, radiation protection of the rectum, bladder, and the pelvic walls in our HDR BT is crucial in view of the elevated biologically equivalent dose (EQD2) of 60.8 Gy3 due to the hypofractionation system of EBRT at our center. The constraint at UCH, Nigeria, which warranted use of rectal marker for points’ location is the difficulty in visualizing the posterior vagina wall in implant (radiographic) lateral views of some patients even with the use of contrast. This was attributed to huge sizes of pelvic bones in such patients. The incidence of bladder complications is relatively low with HDR brachytherapy cervical treatment. Using CT-based BT planning, Uno et al. [18], in an analysis of 100 patients with Stages IIB or IIIB cervical cancer, found that depth of 6 Gy isodose volume determined in three dimension has the predictive value of late rectal complications. A successful treatment includes not only an improvement on tumor control, but also a reduction in treatment-related complications [19]. Despite the radiobiological disadvantages of the HDR technique mentioned by Eifel et al. [20], the possibility of optimizing dose distribution seems to outweigh the drawbacks. The variation of dwell time with the single stepping source permits almost infinite variation on the effective source strength and source positions, allowing for greater control of the dose distribution and potentially less morbidity [21]. Although the use of conventional X-ray based planning can get good outcomes and acceptable toxicities, many limitations are associated with this process [22] indicating the need for the use of image-guided brachytherapy (IGBT), when practicable to improve therapeutic ratios in cervical cancer. Magnetic resonance imaging guidance allows treatments to be optimized to tumor volumes, while sparing organs at risk [23].
Conclusions
This study has provided baseline data at our center on brachytherapy dose parameters using Bebig's Gynesource unit and HDR basic TPS for 0.5 cm step positions of 60Co radionuclide source. The practice of HDR ICBT at our center has been with equal (1 : 1) dwell (irradiation) time share between the IUT and ring components of the applicator. Evaluation of an alternative dwell weighting system, whereby the tandem uses greater time proportion, showed decrease in mean values of dose parameters with statistically significant differences (p-values < 0.05) except for bladder dose (p = 0.132). This is attributable to decrease in the dwell times for ring (vaginal) sources, which resulted in reduction of the width of the reference volume pertinent to doses at OARs, particularly the rectum. Moreover, less irradiation time per fraction and lower integral dose to patients will result when the alternate approach is used. It is therefore observed that if varying dwell weightings are utilized for standard BT planning at our center, as against the fixed ratio in current practice, OARs dose sparing in our patients will be significantly enhanced. While Bebig applicators cannot be used with a rectal retractor, efforts should be intensified by clinicians to increase intracavitary packing with gauze, especially posteriorly to the rectum. However, in future, individualized brachytherapy planning with the proposed dwell time pattern and giving consideration to tumor geometry and patient anatomy, using new advances in imaging would be adopted to ensure dose optimization.
Acknowledgements
The authors acknowledge the International Atomic Energy Agency (IAEA), Vienna, Austria for donating the 1st HDR brachytherapy facility to our center and the visiting Physicist who commissioned it. The technical support of Mr. Antonius Spiller of Eckert & Ziegler, BEBIG, Germany is much appreciated. We are also grateful to the Engineering workshop of the Department of Medical Physics, Groote Schuur Hospital, Cape Town, South Africa for producing the re-usable rectal marker used at our center.
Disclosure
Authors report no conflict of interest.
References
- 1.Hoekstra C, Riet A, Mak A. Dwell time optimization in HDR brachytherapy for cervical carcinoma Chapter 34. In: Mould RF, et al., editors. International brachytherapy abstract book. Veenendaal: Nucletron B.V.; 1992. [Google Scholar]
- 2.Tyagi K, Mukundan H, Mukherjee D, et al. Non isocentric film-based intracavitary brachytherapy planning in cervical cancer: a retrospective dosimetric analysis with CT planning. J Contemp Brachytherapy. 2012;4:129–134. doi: 10.5114/jcb.2012.30678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Commission on Radiation units and Measurements, Dose and Volume Specification for Reporting Intracavitary Therapy in Gynecology; ICRU Report 38; Bethesda: ICRU; 1985. [Google Scholar]
- 4.Pötter R, Limbergen E, Gerstner N, et al. Survey of the use of the ICRU 38 in recording and reporting cervical cancer brachytherapy. Radiother Oncol. 2001;58:11–18. doi: 10.1016/s0167-8140(00)00266-8. [DOI] [PubMed] [Google Scholar]
- 5.Jones DA, Notley HM, Hunter RD. Geometry adopted by Manchester radium applicators and Selectron afterloading applicators in intracavitary treatment for carcinoma cervix uteri. Br J Radiol. 1987;60:481–485. doi: 10.1259/0007-1285-60-713-481. [DOI] [PubMed] [Google Scholar]
- 6.King GC, Bloomer WD, Kalnicki S, et al. Point dose variations with time during traditional brachytherapy for cervical carcinoma. Med Dosim. 2000;25:77–80. doi: 10.1016/s0958-3947(00)00032-7. [DOI] [PubMed] [Google Scholar]
- 7.Erickson BA. Intracavitary applications in the treatment of cancer of the cervix, part II: High dose rate techniques. J Brachyther Int. 1997;13:271–287. [Google Scholar]
- 8.Abitbol AA, Houdek P, Schwade JG, et al. Ring applicator with retractor: Applicability to HDR brachytherapy of cervical cancer. Selectron Brachyther J. 1990;4:68–69. [Google Scholar]
- 9.Wollin M, Kagan AR, Olch A, et al. Comparison of the ring applicator and the Fletcher applicator for HDR brachytherapy. Selectron Brachyther J. 1991;(2 Suppl):25–27. [Google Scholar]
- 10.Hetzel H, McCoy M. Rectal screens for the ring applicator for the selectron-LDR/HDR afterloading system. In: Mould RF, editor. Brachytherapy 2. Leersum: Nucletron; 1989. pp. 136–140. [Google Scholar]
- 11.Kim RY, Trotti A, Ching-Jung W, et al. Radiation alone in the treatment of cancer of the uterine cervix: analysis of pelvic failure and dose response relationship. Int J Radiat Oncol Biol Phys. 1989;17:973–978. doi: 10.1016/0360-3016(89)90144-2. [DOI] [PubMed] [Google Scholar]
- 12.Orton CG, Wolf-Rosenblum S. Dose dependence of complication rates in cervix cancer radiotherapy. Int J Radiat Oncol Biol Phys. 1986;12:37–44. doi: 10.1016/0360-3016(86)90413-x. [DOI] [PubMed] [Google Scholar]
- 13.Rotman M, John MJ, Roussis K, et al. The intracavitary applicator in relation to complications of pelvic radiation- the Ernst system. Int J Radiat Oncol Biol Phys. 1978;4:951–956. doi: 10.1016/0360-3016(78)90004-4. [DOI] [PubMed] [Google Scholar]
- 14.Unal A, Hamberger AD, Seski J, et al. Analysis of the severe complications of irradiation of carcinoma of the uterine cervix: treatment with intracavitary radium and parametrial irradiation. Int J Radiat Oncol Biol Phys. 1981;7:999–1004. doi: 10.1016/0360-3016(81)90150-4. [DOI] [PubMed] [Google Scholar]
- 15.Williamson J, Nath R. Clinical implementation of AAPM TG 32 recommendations on brachytherapy source strength specification. Med Phys. 1991;18:439–448. doi: 10.1118/1.596691. [DOI] [PubMed] [Google Scholar]
- 16.Çetingöz R, Ataman ÖU, Tuncel N, et al. Optimization in high dose rate brachytherapy for utero-vaginal applications. Radiother Oncol. 2001;58:31–36. doi: 10.1016/s0167-8140(00)00295-4. [DOI] [PubMed] [Google Scholar]
- 17.Basu B, Basu S, Chakraborti B, et al. A comparison of dose distribution from Manchester-style and Fletcher-style intracavitary brachytherapy applicator systems in cervical cancer. J Contemp Brachytherapy. 2012;4:213–218. doi: 10.5114/jcb.2012.32555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uno T, Itami J, Aruga M, et al. High dose rate brachytherapy for carcinoma of the cervix (Risk factors for late rectal complications) Int J Radiat Oncol Biol Phys. 1998;40:615–621. doi: 10.1016/s0360-3016(97)00849-3. [DOI] [PubMed] [Google Scholar]
- 19.Patra NB, Manir KS, Basu S, et al. Effect of bladder distension on dosimetry of organs at risk in computer tomography based planning of high-dose-rate intracavitary brachytherapy for cervical cancer. J Contemp Brachytherapy. 2013;5:3–9. doi: 10.5114/jcb.2013.34339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eifel PJ, Morria M, Oswald MJ. The influence of tumor size and growth habit on outcome of patients with FIGO stage IB squamous cell carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys. 1993;27:127–128. doi: 10.1016/0360-3016(94)90220-8. [DOI] [PubMed] [Google Scholar]
- 21.Nag S, Erickson B, Thomadsen B, et al. The American Brachytherapy Society recommendations for high dose rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000;48:201–211. doi: 10.1016/s0360-3016(00)00497-1. [DOI] [PubMed] [Google Scholar]
- 22.Tharavichitkul E, Wanwilairat S, Chakrabandhu S, et al. Image-guided brachytherapy (IGBT) combined with whole pelvic intensity-modulated radiotherapy (WP-IMRT) for locally advanced cervical cancer: a prospective study from Chiang Mai University Hospital, Thailand. J Contemp Brachytherapy. 2013;5:10–16. doi: 10.5114/jcb.2013.34338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson J, Huang Y, Kim Y. Dosimetric impact of point A definition on high-dose-rate brachytherapy for cervical cancer: evaluations on conventional point A and MRI-guided, conformal plans. J Contemp Brachytherapy. 2012;4:241–246. doi: 10.5114/jcb.2012.32559. [DOI] [PMC free article] [PubMed] [Google Scholar]