Abstract
Colloidal particle size is an important characteristic that allows mapping sentinel nodes in lymphoscintigraphy. This investigation aimed to introduce different ways of making a 99mTc-tin colloid with a size of tens of nanometers. All agents, tin fluoride, sodium fluoride, poloxamer-188, and polyvinylpyrrolidone (PVP), were mixed and labeled with 99mTc. Either phosphate or sodium bicarbonate buffers were used to adjust the pH levels. When the buffers were added, the size of the colloids increased. However, as the PVP continued to increase, the size of the colloids was controlled to within tens of nanometers. In all samples, phosphate buffer added PVP (30 mg) stabilized tin colloid (99mTc-PPTC-30) and sodium bicarbonate solution added PVP (50 mg) stabilized tin colloid (99mTc-BPTC-50) were chosen for in vitro and in vivo studies. 99mTc-BPTC-50 (<20 nm) was primarily located in bone marrow and was then secreted through the kidneys, and 99mTc-PPTC-30 (>100 nm) mainly accumulated in the liver. When a rabbit was given a toe injection, the node uptake of 99mTc-PPTC-30 decreased over time, while 99mTc-BPTC-50 increased. Therefore, 99mTc-BPTC-50 could be a good candidate radiopharmaceutical for sentinel node detection. The significance of this study is that nano-sized tin colloid can be made very easily and quickly by PVP.
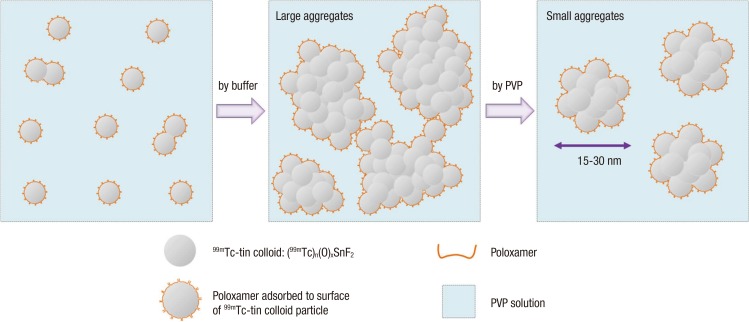
Graphical Abstract
Keywords: Sentinel Lymph Node, Lymphoscintigraphy, 99mTc-tin Colloid, Polyvinylpyrrolidone (PVP)
INTRODUCTION
One mechanism for metastasis is for cancerous cells to travel through the lymphatic system where they then spread beyond their original locations to other parts of the body. Sentinel lymph nodes (SLN) form the first group of lymph nodes that drain cancer cells from the primary tumor site (1, 2, 3, 4). Thus, SLN biopsies are standard procedures that help surgeons decide whether there is need for wide lymphadenectomy. When there is a negative SLN biopsy result, no extensive lymph node dissection is needed because cancer cells are less likely to move through the lymphatic ducts (5, 6). As such, a rapid recovery can also be expected since this procedure eliminates unnecessary lymphadenectomies and their potential adverse effects. For these reasons, developing effective SLN mapping techniques is of the utmost importance for surgeons to allow them to select the appropriate therapy.
The optimal imaging agents for SLN mapping should be able to rapidly move from a tumor to the SLNs and should have properties that permit prolonged retention and stability in vivo. The ideal particle size for SLN mapping is in the range of 10-50 nm (7, 8, 9). Large particles (0.5-2 µm) can be indefinitely retained at the injection site while particles that are too small (<5 nm) penetrate the capillary membranes and are quickly cleared from the injection site. Thus, the distribution of particle size is a major determinant of the kinetics of colloid clearance through lymphatic drainage (10, 13).
Radio-guided surgical biopsies based on lymphoscintigraphy have become a standard procedure to detect SLN metastasis. Various radiopharmaceuticals have been used for lymphoscintigraphy, including 99mTc-sulfur colloid (8, 9, 11), 99mTc-antimony sulfide colloid (ASC) (12, 13, 14), and 99mTc-nanocolloid (10, 13). The latter two are preferable to the former, since they possess a smaller particle size. The unfiltered 99mTc-sulfur colloid has an average particle size of 100-1,000 nm and, after filtration, has the largest percentage of particles smaller than 30 nm. Although 99mTc-ASC has the best size range (3-30 nm) for SLN mapping, its use has never been approved by the FDA for routine use in the USA, and it is not commercially available (15). In Europe, 99mTc-nanocolloid, with particles between 4 and about 100 nm (95% of the particles are <80 nm), is more frequently used (16).
Here, polyvinylpyrrolidone (PVP) was chosen to make the nano-sized tin colloid. PVP is a biocompatible polymer that has many good characteristics, including that it is water soluble, non-charged, non-toxic, essentially chemically inert, temperature-resistant, pH-stable, and colorless. For these reasons, PVP has been widely used and has been reported as a suspension stabilizer for oral and topical medications and has also been added to many colloidal preparations to prevent aggregation (17, 18, 19, 20). The aim of the present study was to develop a radio-colloid with optimal size ranges that can be used for effective SLN mapping. Here, we introduce a simple preparation method for nano-sized tin colloid that modifies the traditional tin colloid preparation.
MATERIALS AND METHODS
General
Polyvinlyprrolidone (PVP, Kollidon30, Mw=44,000-54,000) and poloxamer-188 (Lutrol® F 68) were donated by BASF Korea (Seoul, Korea). The other chemicals of reagent grade were purchased from Sigma Aldrich Co. (St. Louis, MO) and were used without further purification. 99mTc-pertechnetate was eluted from a technetium generator in our hospital (Daiichi Radioisotope Laboratories, Tokyo, Japan). An ITLC-SG chromatographic paper was purchased from Pall Science (Port Washington, NY). For precise work, a pH meter (PH510, Coretech, Korea) was calibrated before each measurement. Radiolabeling yield was tested with an AR-2000 radio-TLC scanner (Bioscan, Washington, D.C.). The phosphate buffer (0.1 M, pH 7.3) used consisted of a mixture of monobasic dihydrogen (NaH2PO4) and dibasic monohydrogen phosphate (Na2HPO4).
Product formulations and radiolabeling efficiency
The main components of the tin colloid were similar to Hepatate (Median Pharma, France) except for the PVP. Two types of PVP stabilized tin colloid (abbreviation: PTC) formulations were prepared as follows. The first contained tin(II) chloride (1.25 mg), sodium chloride (10 mg), poloxamer-188 (5 mg), and variable amounts of PVP (10-50 mg) in a sterile glass vial. The second contained tin(II) fluoride (1.25 mg), sodium fluoride (10 mg), poloxamer-188 (5 mg), and variable amounts of PVP (10-50 mg). Subsequently, 99mTc pertechnetate (<185 MBq) in 5 mL of normal saline (0.9% NaCl, JW Pharmaceutical, Korea) was added to each vial, and then each was vigorously shaken for 1 min using a vortexer (USA Scientific, FL). To adjust the pH, phosphate buffer (0.1 M, pH 7.3, 0.3 mL) or sodium bicarbonate solution (NaH2CO3, 10 mg/mL, 10 µL) were added and vigorously shaken using the vortexer.
The size distribution of the radioactive colloids was determined by using a particle size analyzer at 30 m, 90 m, 3 hr, and 9 hr (UPA-150, Microtrac, KBSI, Jeonju, Korea). The zeta potential of non-radioactive colloid in a dip cell kit (99mTcO4- was replaced by saline) was tested using a zetasizer equipped with a standard 633 nm laser (Zetasizer Nano ZS90, Malvern, Worcestershire, UK) at 30 m after colloid formation.
The name PPTC is short for "phosphate buffer added PTC" and BPTC stands for "sodium bicarbonate solution added PTC". PPTC and BPTC have numbers after their abbreviations that indicate the amount of PVP used. For example, for XPTC-Y, "X" =buffer abbreviation, "Y"=PVP amount. The radio-colloids were used for cell and animal studies without further purification. 99mTcO4- was analyzed via chromatography on ITLC-SG strips eluted with acetone and saline (1, 10, 30, and 60 m; 2, 3, 6, and 24 hr).
Field emission scanning electron microscopy (FE-SEM)
High-resolution morphological images of non-radioactive colloids were obtained using a field emission scanning electron microscope (SUPRA 49EP, Carl Zeiss, Germany). To observe the shape and surface morphology, 3-5 µL of the colloid was loaded on the Si wafer, and dried at room temperature and coated with a 3 nm layer for 7.5 sec of Os using a plasma CVD osmium coater (HCP-1SW, Filgen, Japan). The images were controlled with the smartSEM 5.05 version program (Carl Zeiss, Germany). The colloid images were acquired at the outer part of spotted samples for searching exact colloid forms because of a large amount of PVP and samples were not diluted.
In vitro cell uptake studies
The RAW 264.7 mouse macrophage and MDA-MB-231 human breast cancer cell lines were purchased from the Korean Cell Line Bank (KCLB, Seoul, Korea) and were grown in RPMI1640 (Gibco BRL) and DMEM (high glucose, Gibco BRL) media supplemented with 10% fetal bovine serum (FBS) and gentamycin (100 µg/mL), respectively. The cell lines were maintained at 37℃ in an atmosphere of 95% air and 5% CO2. Cells (8×104) were seeded in a 24-well plate and were allowed to adhere overnight (~22 hr) in complete medium. After 6 hr seeding, the RAW 264.7 cells were subsequently stimulated with lipopolysaccharide (LPS, Sigma, 1 µg/mL) for 16 hr. After ringing twice with FBS free media, the cells were incubated with selected compounds (99mTc-PPTC-30 and 99mTc-BPTC-50; 0.15-0.91 kBq/µL) for 1 hr at 37℃. After incubation, the cells were extensively washed with cold PBS and were plate-dried in an oven for 20 min. And then 0.2 mL of 0.1 N NaOH was added to the wells to facilitate cell lysis. The lysates were collected and counted in a gamma counter (Packard, Meriden, CT). The cell number was corrected via BCA assay (Pierce, Rockford, IL) and cpm/UV abs. was expressed as mean±standard deviation (SD). A paired t-test (Sigma Plot, Chicago, IL, USA) was used to determine the statistical significance at a 95% confidence level, with P<0.05 being considered statistically significant.
Gamma camera imaging
All animal experiments were performed in compliance with the policies and procedures of the Institutional Animal Care and Use Committee for animal treatment of Chonbuk National University. SD rat (6-7 weeks) and New Zealand white rabbit (1.8-2 kg) were purchased from Orient-Bio Inc. (Seoul, Korea) and Hanil Inc. (Jeonju, Korea), respectively. Rats were anesthetized by intra-peritoneal injection with a mixture of ketamine (50 mg/kg) and xylazine (10 mg/kg). 99mTc-PPTC-30 and 99mTc-BPTC-50 were administered in the tail vein of the rats (~11 MBq). Planar image scanning was carried out at 60 min post-injection (ECAM, SIMENS Medical Systems, Malvern, PA, USA).
For popliteal lymph node imaging, 99mTc-PPTC-30 and 99mTc-BPTC-50 were injected between the second and third toes of the right and left hind feet of the rabbit under ketamine/xylazine anesthesia. The rabbit was subjected to a 30-min dynamic scan (30 sec per frame) starting 1 min after the injection. After the dynamic scan, static planar images were acquired until 220 min. For each dynamic and static scan, the regions of interest (ROIs) were drawn over the right and left popliteal lymph nodes.
Ethics statement
The animal studies were performed after receiving approval of the institutional animal care and use committee (IACUC) in Chonbuk National University (IACUC approval No. CBU 2014-00076).
RESULTS
99mTc-PTC preparation and characterization
99mTc-PTCs composed of tin chloride, sodium chloride, poloxamer-188, and PVP showed size ranges of 7-11 nm. Over time, however, they turned into a white precipitate. The stannous ion readily undergoes hydrolysis in aqueous solutions, and for this reason, insoluble colloids were easily formed. Consequently, no further studies were performed using stannous chloride.
99mTc-PTCs composed of tin fluoride, sodium fluoride, poloxamer-188, and PVP showed size ranges of 4-13 nm (Table 1). These colloid sizes were maintained for 24 hr, regardless of the amount of PVP added. A colloid is a dispersion of very fine particles in water.
Table 1. Size distributions of 99mTc-PTCs, 99mTc-PPTCs, and 99mTc-BPTCs.
| Isotope colloid | PVP amount (mg) | Particle size (nm) by time | |||
|---|---|---|---|---|---|
| 30 min | 90 min | 3 hr | 6 hr | ||
| 99mTc-PTC | 10 | 8.4 ± 6.41 | 4.0 ± 0.36 | 5.1 ± 1.65 | 15.3 ± 2.50 |
| 20 | 9.43 ± 3.26 | 4.5 ± 0.40 | 5.6 ± 2.03 | 13.7 ± 4.57 | |
| 30 | 20.2 ± 1.76 | 5.7 ± 1.17 | 5.6 ± 1.97 | 10.9 ± 2.65 | |
| 40 | 23.4 ± 0.85 | 6.4 ± 1.72 | 7.2 ± 2.97 | 7.6 ± 0.61 | |
| 50 | 18.7 ± 4.27 | 9.6 ± 1.67 | 8.2 ± 1.25 | 10.1 ± 1.43 | |
| 99mTc-PPTC | 10 | 48.4 ± 5.12 | 46.8 ± 15.7 | 57.3 ± 6.53 | 64.4 ± 5.87 |
| 20 | 16.5 ± 12.19 | 55.8 ± 5.31 | 50.6 ± 13.24 | 54.7 ± 2.66 | |
| 30 | 55.3 ± 37.59 | 139.0 ± 139.2 | 81.9 ± 41.6 | 75.4 ± 42 | |
| 40 | 25.0 ± 6.92 | 31.5 ± 6.24 | 46.37 ± 3.46 | 44.2 ± 4.41 | |
| 50 | 25.1 ± 8.02 | 30.6 ± 7.82 | 48.5 ± 0.36 | 102.5 ± 107.3 | |
| 99mTc-BPTC | 10 | 513.7 ± 107.82 | 551.3 ± 287.17 | 1,369.4 ± 1,121.62 | 1,404 ± 1,109 |
| 20 | 9.27 ± 0.75 | 1,157.3 ± 1,344.9 | 968.58 ± 608.07 | 1,195 ± 672.6 | |
| 30 | 8.97 ± 0.49 | 184.38 ± 231.56 | 1,141 ± 1,256.02 | 643.9 ± 685.61 | |
| 40 | 8.37 ± 1.25 | 17.8 ± 4.86 | 11.3 ± 2.12 | 10.2 ± 1.15 | |
| 50 | 7.6 ± 0.69 | 16.5 ± 6.76 | 12.7 ± 1.11 | 12.6 ± 1.04 | |
Values are expressed as mean±SD (n=3).
The pH of 99mTc-tin fluoride colloid was 5.13±0.07. In other to be used in vivo and to induce colloid size growth, the pH was adjusted using buffer solutions: phosphate buffer (PPTC) and sodium bicarbonate solution (BPTC). After the buffers added, the pHs were changed to 6.51±0.10 and 5.76±0.05, respectively. Regardless of the PVP amounts, the pHs of 99mTc-PPTC 10-50 and 99mTc-BPTC 10-50 showed similar ranges, respectively. The size distributions are shown in Table 1. An addition of phosphate buffer induced a colloid size increase from tens to hundreds (Table 1), whereas larger aggregates were formed with the addition of the sodium bicarbonate solution (tens increased to thousands). The size ranges of 99mTc-BPTC were not affected by the PVP amounts until 30 mg, but the size decreased rapidly when over 40 mg (Table 1).
The range of 10-50 nm in size is generally known to be the ideal particle size for SLN mapping. These data indicated that, 99mTc-BPTC-50 shows similar sizes to this ideal size range so it was chosen, along with 99mTc-PPTC-30 (>100 nm) for comparison, for further studies.
Zeta-potential measurements were also used to confirm the surface potential changes after the nano colloid formation. The zeta-potentials of SnF2, SnF2+NaF, SnF2+NaF+poloxamer, SnF2+NaF+poloxamer+PVP were 16.33±2.08, -9.9±5.92, -5.26±3.66, and -4.15±1.92, respectively. After buffer adding, the zeta-potentials of PPTC-30 and BPTC-50 changed to -21.9±2.78 and -7.63±1.98, respectively. Regardless of the PVP amount, the zeta-potentials of 99mTc-PPTC 10-50 and 99mTc-BPTC 10-50 also were showed similar ranges, respectively. The majority of this work was performed in the absence of 99mTcO4-, and no differences were observed in those experiments using technetium generator elutes. This is reasonable in light of the few nanograms of 99mTc and 99Tc present. ITLC was performed at various time points. 99mTcO4- (Rf=1) migrate at the solvent front while the radio colloid and reduced hydrolyzed 99mTcO2 remain at the origin (Rf=0). The radiochemical purity in acetone was 98.2%, 96.9% and in saline was 94.5%, 97.9%, for 99mTc PPTC-30 and 99mTc BPTC-50, respectively.
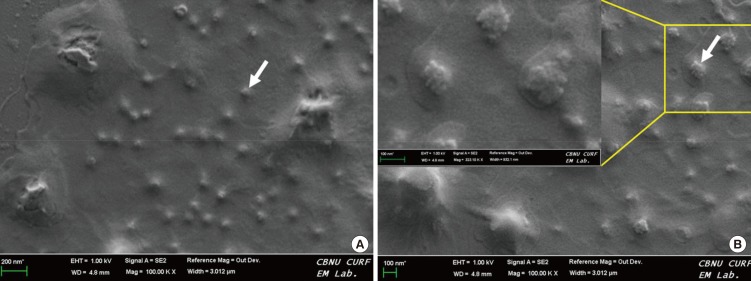
Field emission scanning electron microscopy
As shown in Fig. 1, the shape of BPTC-50 was roughly spherical, with sizes of about 50 nm or so, and with a homogeneous distribution. The gray arrow indicates that BPTC-50 colloid (Fig. 1A). In Table 1, PPTC-30 had sizes in the range of 55.3±37.59 nm. The SEM image also showed various sizes of colloids (gray arrow in Fig. 1B). It was also shown that many small particles agglomerate together and then form one larger particle clusters (Fig. 1A and B).
Fig. 1. FE-SEM micrographs of 99mTc-BPTC-50 (A) and 99mTc-PPTC-30 (B). The gray arrows indicate the colloids.
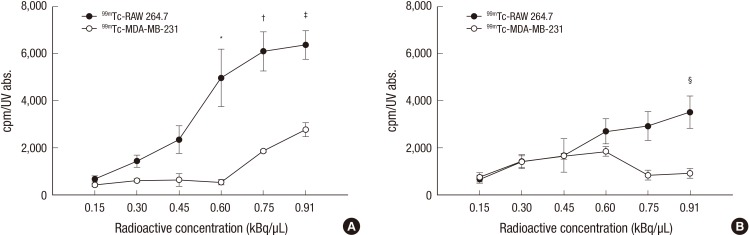
In vitro cellular uptake test
The cellular uptake of 99mTc-BPTC-50 and 99mTc-PPTC-30 were tested in both MDA-MB-231 human breast cancer and RAW 264.7 mouse macrophage cells. As shown in Fig. 2, the radioactivity of the mouse macrophage cells treated with 99mTc-BPTC-50 was higher than that of the human breast cancer cells at all concentrations. This result showed significant differences at three concentrations points (0.6, 0.75, and 0.91 kBq/µL) (*, †, ‡P<0.05). A comparably low uptake was found for 99mTc-PPTC-30 in both cell lines; however, a significant difference was only shown in the final concentration (0.91 kBq/µL) (§P<0.05).
Fig. 2. Cellular uptakes of 99mTc-BPTC-50 (A) and 99mTc-PPTC-30 (B) in RAW264.7 mouse macrophage cell line and MDA-MB-231 human breast cancer cell line. *,†, ‡, §P < 0.05.
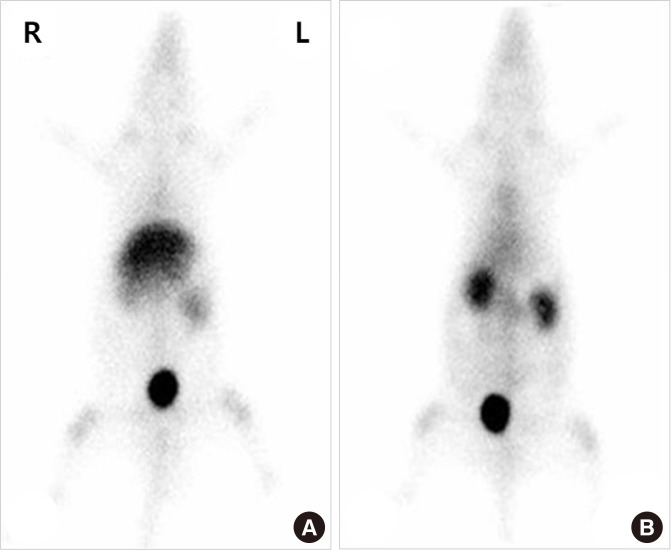
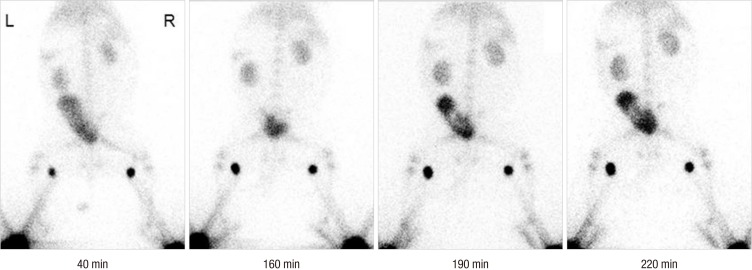
Gamma imaging and sentinel lymph node imaging
To identify the total body distribution, 99mTc-BPTC-50 and 99mTc-PPTC-30 were injected into the tail veins of the rats (Fig. 3A and B). 99mTc-PPTC-30 mainly accumulated in the liver as well as in the kidney and in bone marrow. On the other hand, 99mTc-BPTC-50s with smaller sizes <20 nm accumulated in the bone marrow and were excreted rapidly through the kidneys. These results indicate that 99mTc-BPTC-50 is small enough for uptake by the myelophagocytic system of bone marrow and is of the proper size to be washed out through the kidney glomerulus. When 99mTc-BPTC-50 and 99mTc-PPTC-30 were injected into the hind feet of the rabbit, uptake of 99mTc-BPTC-50 (left) in the popliteal lymph node increased with time, whereas 99mTc-PPTC-30 (right) showed a high initial uptake and then washed out over time (Fig. 4).
Fig. 3. Representative static planar images of rats administered with 7.4 MBq of 99mTc-PPTC-30 (A), and 99mTc-BPTC-50 (B) at 1 hr after i.v. injection. 99mTc-BPTC-50 was preliminary positioned in the bone marrow and kidneys, whereas 99mTc-PPTC-30 mainly accumulated in the liver.
Fig. 4. Representative static planar images of rabbit administered with 7.4 MBq of 99mTc-BPTC-50 and 99mTc-PPTC-30 at 40, 160, 190, and 220 min. Two 99mTc-PTCs were injected subcutaneously on the dorsum of each hind foot. 99mTc-PPTC-30 was injected in the right foot and 9mTc-BPTC-50 was injected in the left foot.
DISCUSSION
99mTc-tin colloid (Hepatate) has an average particle size of 100-1,000 nm and is the agent of choice for reticuloendothelial (RE) imaging of the liver and spleen (20). A filtration step is required for using sentinel node detection. The main components of 99mTc-tin colloid are stannous fluoride, sodium fluoride, and poloxamer. When we prepared the tin colloid formulation in the laboratory, the resulting pH was slightly acidic. In this study, some substances and conditions were applied in an attempt to control 99mTc-tin colloid size to obtain ideal colloidal particles for sentinel lymph node mapping.
The pH of a radiopharmaceutical substance is very important to ensure its stability and biological properties. The maintenance of a proper pH of the solution is achieved by adding buffers such as a phosphate buffer or Tris buffer. In this study, phosphate buffer and sodium bicarbonate buffer were used to adjust the pH of the colloid and to grow its size. When the electrolytes (salts, acids, or bases) are added, the zeta potential between the solvent and the surface of colloids was able to break down and eventually cause the aggregation or flocculation of colloids (18, 20). Actually, the particle size of 99mTc-PTC with sodium bicarbonate buffer greatly increased, while it only slightly increased with the phosphate buffer. Based on Table 1, the size of the nano-colloids with same ranges of pH and zeta potential (PPTCs or BPTCs) could be controlled with PVP amounts. Different ranges of pH and zeta potential (PPTC vs. BPTC) were achieved through the use of different buffer types (or volume). As the results show, the size of the nano-colloids prepared in this study could be controlled by the two factors: PVP amount and buffer type (or volume).
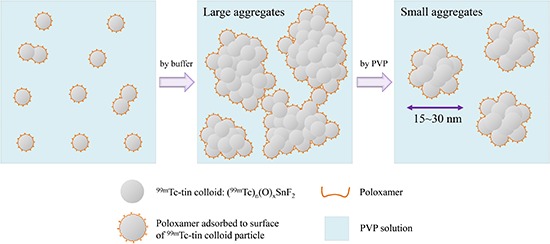
As shown in Fig. 1, the many small particles agglomerate together and then form one larger particle cluster. According to a previous study, 99mTc-tin fluoride colloid used to label leucocytes radiopharmaceutically was made by only two materials - tin fluoride and sodium fluoride (21). Although the precise structural formula of 99mTc-tin fluoride colloid is unknown, the researchers thought the presence of Sn (II) as Sn-O is likely to comprise the particle matrix. The chemical reaction could be stated as follows: 99mTcO4- + SnF2 → (99mTc)n(O)xSnF2. Similarly, 99mTc-PTC, 99mTc-PPTCs and 99mTc-BPTC are also expected to have the same matrix core. Then colloidal particles form in a manner similar to nucleation, and the remaining materials bind to the nucleation sites and subsequently growth occurs. As shown in Fig. 1, the growth was arrested at a uniform size. This may be due to the Poloxamer effect. Poloxamer is a non-ionic surface active surfactant and is adsorbed strongly at the surface of colloidal particles (22). However, this valence between the two colloid particles would be broken down by adding the buffer solution. This was shown in the clusters made by colloidal particles. Finally, the clusters (=aggregates), at a uniform size, would be made by PVP dispersant (Fig. 5).
Fig. 5. The preparation process of PVP stabilized 99mTc-tin colloid. This process is not a sequential, it is almost co-occurrence.
Stabilizing agents, such as gelatin, PVP, or carboxy methyl-cellulose are added to many colloidal preparations to prevent aggregation by keeping particles in a dispersed state. For example, 99mTc-antimony sulfide colloid (ASC) is stabilized with PVP and gelatin is added as a protective colloid in 99mTc-sulfur colloids. In this study, PVP was used to prevent the aggregation of 99mTc-PPTCs and 99mTc-BPTCs. The water solubility of PVP is attributed to the presence of the polar lactam group in the pyrrolidone moiety which increases the hydrophilic nature of the polymer. This characteristic may contribute to a stable colloid (22). In addition, PVP may sterically interfere with salts and with a colloid interaction, thus reducing aggregation.
99mTc-PPTC-30, with the size range above 100 nm, and 99mTc-BPTC-50 with a range of 7-20 nm were injected into the tail veins of rats. The total body distribution of the particles differed, depending on the size, especially in the liver, kidney, and bone. 99mTc-PPTC-30 accumulated slightly in the liver, while 99mTc-BPTC-50 accumulated in the bone marrow and was rapidly excreted through the kidneys. In fact, these distribution patterns in the reticuloendothelial imaging system, according to the size of colloid particles, are consistent with results from previous studies (23). A comparative analysis of popliteal lymph node uptake after hind feet injection of rabbit confirmed that 99mTc-BPTC-50 moves to the popliteal lymph node faster and stayed there longer than 99mTc-PPTC-30. These results suggest that 99mTc-BPTC-50 is an ideal form of a colloid to use in sentinel lymph node mapping. In this study, particle sizes ranging from 10 to 20 nm represented the best balance between the need for the fast lymphatic drainage and for satisfactory retention in the sentinel lymph nodes.
In conclusion, by simply changing the formulation and the preparation methods of existing radiotracers, we were able to prepare nano-sized 99mTc-tin colloid that can easily move to the SLN with an adequate retention time.
Since effective SLN mapping allows for less extensive surgery avoiding adverse effects, our new size-controlling method for 99mTc-tin colloid for sentinel lymph node mapping may help surgeons obtain reliable staging information of a cancer in order to plan the appropriate treatment and to minimize the potential for unnecessary surgery. Further studies are needed to define and measure the accuracy of SLN detection and to compare and analyze such detection with respect to other radio colloids.
Footnotes
This paper was supported by fund of the Biomedical Research Institute, Chonbuk National University Hospital (2012). This work was supported by the Radiation Technology R&D program through the National Research Foundation of Korea funded by the Ministry of Science, ICT and Future Planning (2012M2A2A7014020, and 2012M2A2A7035779) and the National R&D Program for Cancer Control, Ministry of Health, Welfare and Family Affairs (0620220).
DISCLOSURE: The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study conception and design: Kim EM, Jeong HJ. Data collection: Kim EM. Analysis and interpretation of data: Kim EM, Jeong HJ. Writing the manuscript: Kim EM. Final revision: Jeong HJ, Lim ST, Sohn MH. Manuscript approval: all authors.
References
- 1.Giuliano AE, Dale PS, Turner RR, Morton DL, Evans SW, Krasne DL. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg. 1995;222:394–399. doi: 10.1097/00000658-199509000-00016. discussion 9-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Na CJ, Kim J, Choi S, Han YH, Jeong HJ, Sohn MH, Youn HJ, Lim ST. The clinical value of hybrid sentinel lymphoscintigraphy to predict metastatic sentinel lymph nodes in breast cancer. Nucl Med Mol Imaging. 2015;49:26–32. doi: 10.1007/s13139-014-0298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morton DL, Thompson JF, Essner R, Elashoff R, Stern SL, Nieweg OE, Roses DF, Karakousis CP, Mozzillo N, Reintgen D, et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: a multicenter trial. Multicenter Selective Lymphadenectomy Trial Group. Ann Surg. 1999;230:453–463. doi: 10.1097/00000658-199910000-00001. discussion 63-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nune SK, Gunda P, Majeti BK, Thallapally PK, Forrest ML. Advances in lymphatic imaging and drug delivery. Adv Drug Deliv Rev. 2011;63:876–885. doi: 10.1016/j.addr.2011.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boolbol SK, Fey JV, Borgen PI, Heerdt AS, Montgomery LL, Paglia M, Petrek JA, Cody HS, 3rd, Van Zee KJ. Intradermal isotope injection: a highly accurate method of lymphatic mapping in breast carcinoma. Ann Surg Oncol. 2001;8:20–24. doi: 10.1007/s10434-001-0020-x. [DOI] [PubMed] [Google Scholar]
- 6.Kim BT. Sentinel lymph node imaging in breast vancer. Korean J Nucl Med. 1999;33:243–246. [Google Scholar]
- 7.Plut EM, Hinkle GH, Guo W, Lee RJ. Kit formulation for the preparation of radioactive blue liposomes for sentinel node lymphoscintigraphy. J Pharm Sci. 2002;91:1717–1732. doi: 10.1002/jps.10170. [DOI] [PubMed] [Google Scholar]
- 8.Eshima D, Eshima LA, Gotti NM, Herda SC, Algozine CA, Burris TG, Vansant JP, Alazraki NP, Taylor AT. Technetium-99m-sulfur colloid for lymphoscintigraphy: effects of preparation parameters. J Nucl Med. 1996;37:1575–1578. [PubMed] [Google Scholar]
- 9.Hung JC, Wiseman GA, Wahner HW, Mullan BP, Taggart TR, Dunn WL. Filtered technetium-99m-sulfur colloid evaluated for lymphoscintigraphy. J Nucl Med. 1995;36:1895–1901. [PubMed] [Google Scholar]
- 10.Mariani G, Moresco L, Viale G, Villa G, Bagnasco M, Canavese G, Buscombe J, Strauss HW, Paganelli G. Radioguided sentinel lymph node biopsy in breast cancer surgery. J Nucl Med. 2001;42:1198–1215. [PubMed] [Google Scholar]
- 11.Hauser W, Atkins HL, Richards P. Lymph node scanning with 99mTc-sulfur colloid. Radiology. 1969;92:1369–1371. doi: 10.1148/92.6.1369. [DOI] [PubMed] [Google Scholar]
- 12.Pedersen B, Kristensen K. Evaluation of methods for sizing of colloidal radiopharmaceuticals. Eur J Nucl Med. 1981;6:521–526. doi: 10.1007/BF00255885. [DOI] [PubMed] [Google Scholar]
- 13.Tsopelas C. Particle size analysis of (99m)Tc-labeled and unlabeled antimony trisulfide and rhenium sulfide colloids intended for lymphoscintigraphic application. J Nucl Med. 2001;42:460–466. [PubMed] [Google Scholar]
- 14.Tsopelas C. Lymphoscintigraphy is more effective using higher specific activity 99mTc -antimony trisulfide colloid in the rat. Hell J Nucl Med. 2014;17:19–26. [PubMed] [Google Scholar]
- 15.Bombardieri E, Bonadonna G, Gianni L. Breast cancer: nuclear medicine in diagnosis and therapeutic options. Berlin: Springer; 2007. p. 84. [Google Scholar]
- 16.Trifirò G, Viale G, Gentilini O, Travaini LL, Paganelli G. Sentinel node detection in pre-operative axillary staging. Eur J Nucl Med Mol Imaging. 2004;31:S46–S55. doi: 10.1007/s00259-004-1526-9. [DOI] [PubMed] [Google Scholar]
- 17.Cook SE, Park IK, Kim EM, Jeong HJ, Park TG, Choi YJ, Akaike T, Cho CS. Galactosylated polyethylenimine-graft-poly(vinyl pyrrolidone) as a hepatocyte-targeting gene carrier. J Control Release. 2005;105:151–163. doi: 10.1016/j.jconrel.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 18.Liu X, Xu Y, Wu Z, Chen H. Poly(N-vinylpyrrolidone)-modified surfaces for biomedical applications. Macromol Biosci. 2013;13:147–154. doi: 10.1002/mabi.201200269. [DOI] [PubMed] [Google Scholar]
- 19.Wang L, Zeng R, Li C, Qiao R. Self-assembled polypeptide-block-poly (vinylpyrrolidone) as prospective drug-delivery systems. Colloids Surf B Biointerfaces. 2009;74:284–292. doi: 10.1016/j.colsurfb.2009.07.032. [DOI] [PubMed] [Google Scholar]
- 20.Saha GB. Fundamentals of nuclear pharmacy. New York: Springer; 1997. p. 101. [Google Scholar]
- 21.Watanabe A. Cancer metastases research. 4th ed. New York: Nova Science Publishers; 2008. pp. 54–55. [Google Scholar]
- 22.Illum L, Davis SS. The organ uptake of intravenously administered colloidal particles can be altered using a non-ionic surfactant (poloxamer 338) FEBS Lett. 1984;167:79–82. doi: 10.1016/0014-5793(84)80836-4. [DOI] [PubMed] [Google Scholar]
- 23.Higashi H, Natsugoe S, Uenosono Y, Ehi K, Arigami T, Nakabeppu Y, Nakajo M, Aikou T. Particle size of tin and phytate colloid in sentinel node identification. J Surg Res. 2004;121:1–4. doi: 10.1016/j.jss.2004.02.011. [DOI] [PubMed] [Google Scholar]