Abstract
Objective
The Bishop score and length of the uterine cervix are good predictors of successful labor induction. However, little is known about the association between the funneling of the uterine cervix and successful labor induction. The study aimed to evaluate cervical funneling as a predictor of successful labor induction.
Methods
This study was designed as a prospective observational study. Subjects who delivered a baby by labor induction were enrolled in the study from July 2011 to August 2013. Cervical funneling and length were examined with transvaginal ultrasonography. The Bishop score was rated by digital pelvic examination.
Results
A total of 163 primigravida women were recruited for the study. Of these, 137 participants (84.0%) delivered vaginally by labor induction. Cervical funneling was observed in 93 women (57.1%). Successful labor induction was significantly higher in patients with cervical funneling than those without it (91.4% vs. 74.3%, P<0.01), and was significantly associated with cervical funneling, as well as the Bishop score and cervical length. In a multivariate analysis, cervical funneling was an independent predictor for successful vaginal delivery by labor induction ( odd ratio, 2.70; 95% confidence interval, 1.02 to 7.10; P=0.04). However, the Bishop score and cervical length had no association with successful vaginal delivery.
Conclusion
This study showed that cervical funneling could be a predictive marker for vaginal delivery during labor induction.
Keywords: Cervix uteri, Cesarean section, Funneling, Induction, Ultrasonography
Introduction
Labor induction involves the stimulation of contractions before the spontaneous onset of labor, with or without ruptured membranes, whereas augmentation refers to the stimulation of spontaneous contractions considered inadequate because of failed cervical dilation and fetal descent. Labor induction and augmentation are the two most frequently conducted interventional procedures, and their use has been increasing in the past several decades. According to the National Center for Health Statistics, the incidence of labor induction in the United States has more than doubled from 9.5% in 1991 to 22.5% in 2006 [1]. At Parkland Hospital, up to 35% of labors involve induction or augmentation [2]. By comparison, at the Birmingham Hospital of the University of Alabama, labor induction and augmentation were performed in up to 20% and 35% of women, resulting in a total of 55% [2].
One reason for the increase in labor induction is the growing implementation of preventative measures derived from interventional studies for reducing the risks to the fetus. The implementation of these interventional procedures has led to a surveillance instrument that has become highly developed by virtue of the technical progress in the medical sciences. An additional factor underlying the increase in labor induction is the aim of reducing apprehension and/or discomfort in pregnant women, particularly on the due date, because of the unpredictability of vaginal delivery. However, an important consideration in the use of labor induction is that women with an unfavorable cervix commonly experience delayed pain following labor induction, resulting in a failure of vaginal delivery and causing cesarean delivery to be inevitable [3,4]. For instance, in the United States, the use of labor induction resulted in cesarean delivery increasing to a rate of 31.7% in the year 2007 [5].
South Korea has one of highest rates of cesarean deliveries worldwide [6]. Hence, an important issue is the determination of the factors leading to a successful labor induction for decreasing the incidence of cesarean delivery [7]. Additionally, the identification of indicators for evaluating the state of the cervix to determine the risk failure for labor induction is also an important concern, particularly for women with an insufficient ripening of the cervix.
The Bishop score and length of the uterine cervix are considered good predictors of successful labor induction. The Bishop score, which was developed 50 years ago, was the first clinical index to allow assessment of the cervical state. As the Bishop score decreases, an increasingly unsuccessful induction rate is observed [8]. Recently, the cervical length as measured by transvaginal ultrasonography has come to be typically applied as a clinical index for predicting the success of labor induction. In particular, Iams et al [9]. found that cervical length as determined by transvaginal ultrasonography is meaningfully associated with premature labor pain, regardless of singleton/twin pregnancy and the cervical length as determined by this method is routinely implemented to assess the cervical maturity of fully pregnant women [9,10,11,12]. However, contrary to the findings of the early reports, some groups have argued the measurement of cervical length using transvaginal ultrasonography can suffer from highly variable inter-observer differences, and is therefore not suitable as a predictive index for successful labor induction [13,14].
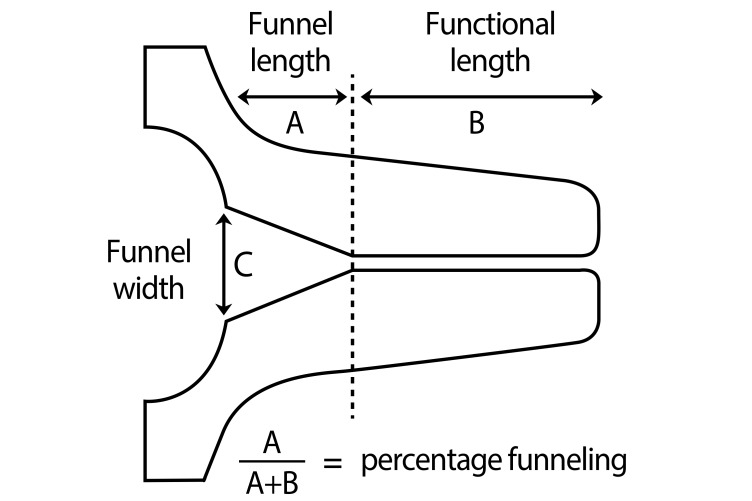
Cervical funneling is a condition that cause bulges in the amnion(and the endocervix) (Fig. 1), resulting in the closure of the exocervix [15] and thereby increasing the risk of premature birth [9,16]. However, although cervical funneling is associated with preterm labor and delivery, little is known about the association between funneling and success in the induction of labor. However, the use of transvaginal ultrasonography for examining cervical incompetence is encompassing not only measurements of length but also the funneling shape of the cervix, therefore allowing the potential association between cervical funneling and success in induction to be explored.
Fig. 1. Real transvaginal ultrasound of the cervix with funneling,functional cervical length (D1) showing funnel length (D2), and funnel width (D3).
In recent years, numerous studies have evaluated the use of transvaginal ultrasound examination for determining cervical length in predicting the outcome of labor induction. Based on various findings, the result of transvaginal ultrasonography for cervical length were concluded to likely be more objective than the Bishop score and have been shown to have reduced variability. Moreover, a favorable cervix tends to change from a closed shape to one produced by funneling, and is also a highly quite important factor for predicting successful vaginal delivery.
The study aims were to evaluate 1) the potential of cervical funneling as a predictor of successful labor induction, 2) the association of cervical funneling with an increased time from labor induction to vaginal delivery, and 3) to compare the predictive value of cervical funneling to the Bishop score and to the cervix length for predicting the successful induction of labor.
Materials and methods
This research was prospectively carried out from July 1, 2011 to August 31, 2013, on primiparous women who attempted vaginal deliveries at the National Health Insurance Service Ilsan Hospital, Korea. Among the patients undergoing labor induction, all women were included if they 1) were primigravida, 2) had a living singleton pregnancy, 3) were cephalic presentation, and 4) were gestational age between 35 and 42 weeks.
Indications for labor induction were according to accepted medical and obstetrical practices as well as Obstetrics: normal and problem pregnancies 6th edition [17], and are as follows: preeclampsia/gestational hypertension, postterm pregnancy more than 41 gestational weeks, premature rupture of membranes, maternal diabetes, suspected fetal growth restriction, oligohydramnios (amnionic fluid index <5), maternal renal disease, personal maternal reasons such as distance from hospital or psychosocial indications and suspected fetal anomaly. In case of maternal personal reason, we induced labor only after 39 gestational weeks and in premature rupture of membranes, we waited about 24 hours until spontaneous labor occurred.
The present protocol for labor induction was used in all pregnant women for vaginal delivery. Before labor induction, all patients underwent complete maternal clinical and obstetrical evaluations. Each pregnant woman was clinically evaluated by pelvic examination to measure the cervical dilatation, effacement, consistency, and position and the fetal station. These five characteristics were measured by a single expert obstetrician (EHK) and were then used to calculate the Bishop score [9]. Fetal head engagement in the maternal pelvic cavity was also assessed by pelvic exam at that time of admission in the delivery room. Engagement is the entrance of the fetal presenting part into the superior pelvic strait and the beginning of the descent through the pelvic canal [17].
The ultrasound IU22 (Philips, Bothell, WA, USA) was used in the present study. A 7-MHz vaginal probe was covered with a condom lubricated both internally and externally and inserted into the vagina to observe the cervical shape. Ultrasound scanning and pelvic examination were performed by only one expert (EHK) in order to reduce inter-observer variation. The vaginal ultrasonography probe, which was covered by a condom, was inserted 3 cm away from the cervix, and the length between the internal and external os of the cervix in the longitudinal section was measured by the probe. The cervical longitudinal section was defined by the view of the cervical canal, and the cervical length was defined as the shortest value based on more than three measurements.
Funnel width was defined as the length of an imaginary line drawn perpendicular to the longitudinal axis of the cervix (Fig. 1) [18]. In the context of these parameters, funneling was arbitrary defined as bulging of the membranes into endocervical canal and protruding at least 15% of the entire cervical length [A/(A+B)>0.15] (Fig. 1). We also evaluated the funneling shape and percentage if present, and calculated the correlation between induction success rate and funneling shape and percentage [funneling percentage=A/(A+B)] (Fig. 2).
Fig. 2. Cervical funneling was defined as bulging of the membranes into the endocervical canal and the bulging protruding at least 15% of the entire cervical length [A/(A+B)>0.15].
For patients showing with cervical conditions favorable for labor induction, intravenous oxytocin (Oxytocin Jeil Inj 10 IU/mL; Jeil Pharmaceutical Co., Yongin, Korea) 10 IU of diluted in 1,000 mL of 5% glucose solution, starting with 16 mL/hr up to the maximal dose of 120 mL/hr) was used to achieve the active phase of labor according to our routine clinical protocol. Meanwhile, pregnant women with an unfavorable cervix were started with intravaginal prostaglandin E2 (dinoprostone 10 mg, Propess vag SR; Bukwang Pharmaceutical Co., Seoul, Korea) to induce cervical ripening, and received this treatment for up to 12 hours until the Bishop score became favorable (≥6), with complementary oxytocin subsequently used for labor induction.
We proposed that failed induction be defined as failure to generate regular contractions approximately every three minutes and cervical change after at least 24 hours of oxytocin or Propess SR administration according to Society of Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists [19]. Amniotomy was performed as soon as cervical dilatation reached a mean of 5.0 cm. Cesarean delivery was performed for failed induction.
Statistical differences were evaluated by the student t-test. The adjusted odds ratio was obtained by multiple logistic regression analysis. A P-value of <0.05 was judged as statistically significant.
Results
A total of 163 primigravida women who were admitted to the delivery room to undergo labor induction were recruited to this study. The patients' demographic data including the medical charts were obtained from electronic medical records in the National Health Insurance Service Ilsan Hospital. The characteristics of these patients are shown in Table 1. The mean gestational age at delivery was 38.3 gestational weeks. Of the total patients, 93 (57.1%) had cervical funneling. Further, 137 of the participants (84%) delivered vaginally, whereas 26 of the women (16.0%) had cesarean deliveries because of a failure in labor induction (Table 1). In this study, the indications of labor induction are shown in Table 2.
Table 1. Patient characteristics.
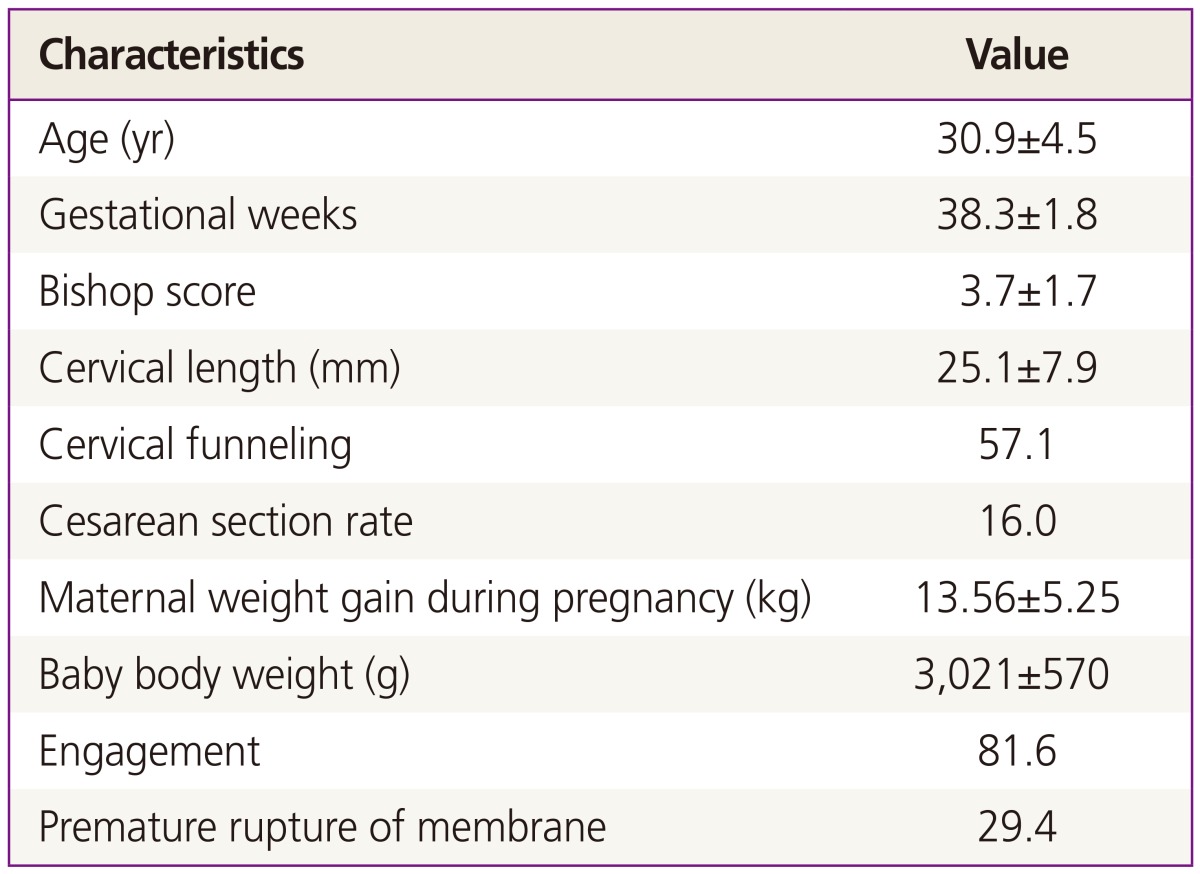
Values are presented as the mean±standard deviation or %.
Table 2. Indications of labor induction.
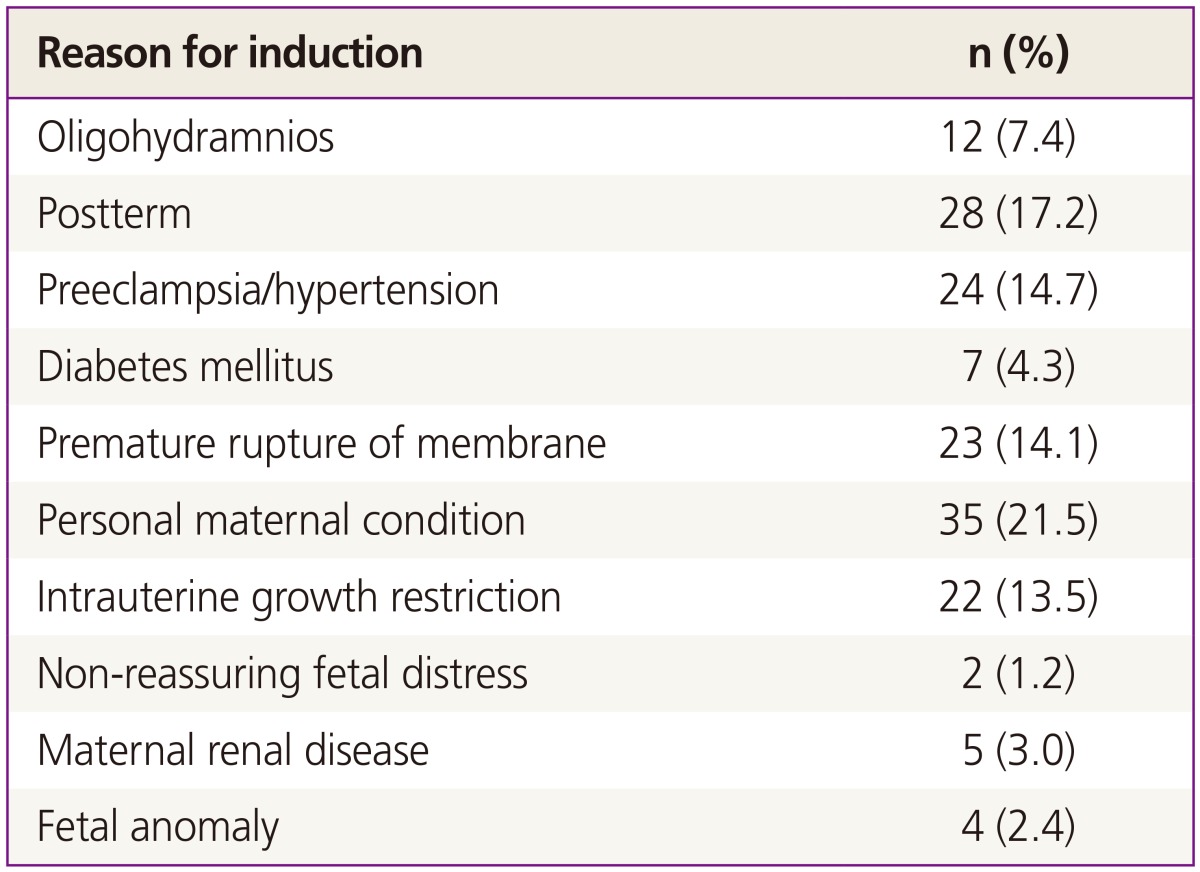
If women had more than 2 indications, we chose the one which was more essential.
No differences in maternal age, gestational age, maternal body mass index (BMI), or neonatal body weight were observed between the women with or without cervical funneling (Table 3). By contrast, cervical length, Bishop score, fetal head engagement at admission, rupture of membranes, period from labor induction to vaginal delivery, the duration of the second stage of labor, delivery within 12 hours after labor induction, and the cesarean delivery rate were significantly lower in the women with funneling as compared to those without funneling (cesarean delivery rate; 8.6% vs. 25.7%, P<0.01) (Table 4).
Table 3. Comparison of demographics in patients with or without cervical funneling.
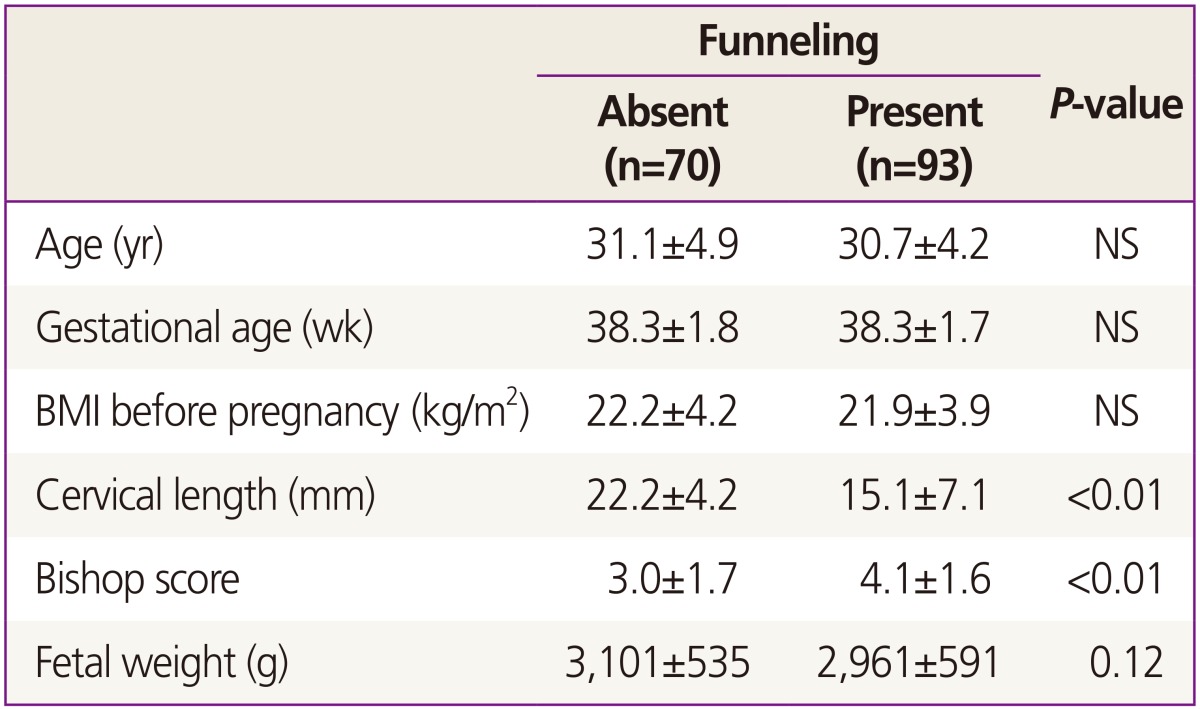
Values are presented as the mean±standard deviation.
NS, not significant; BMI, body mass index.
Table 4. Comparison of the delivery outcome.
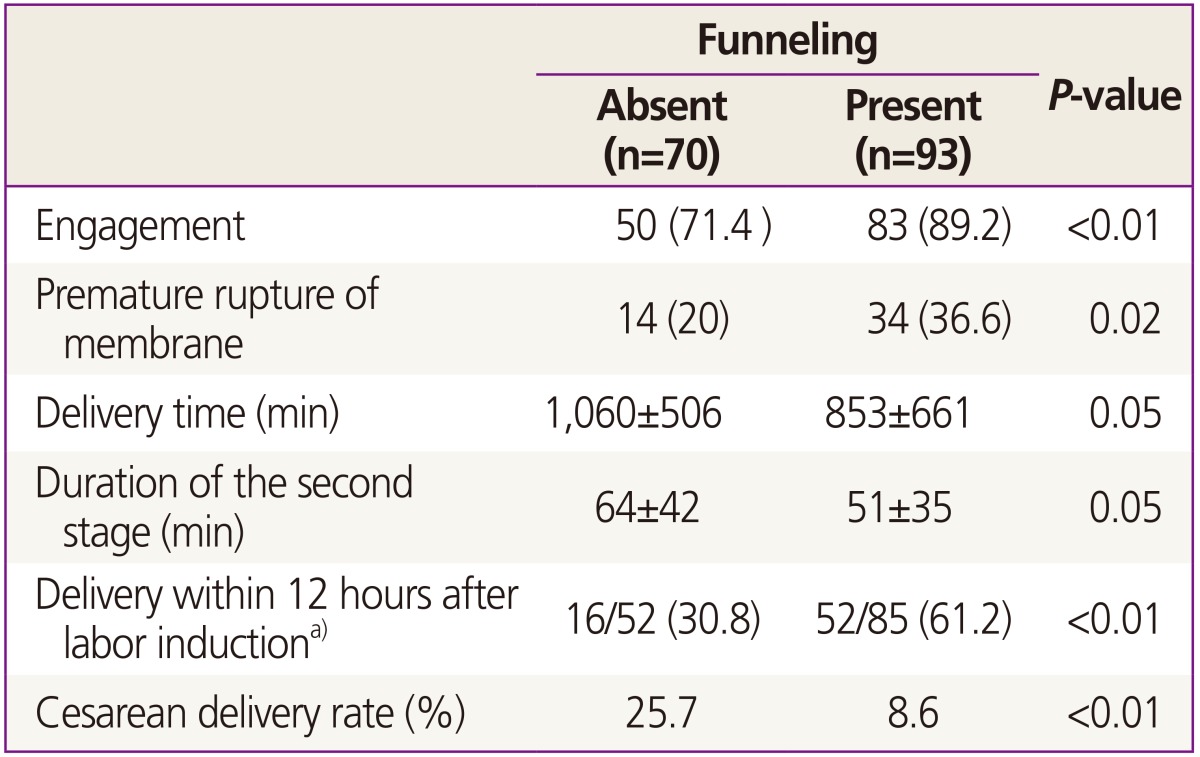
Values are presented as n (%) or mean±standard deviation unless otherwise indicated.
a)Percentage calculated from number of women with vaginal delivery (n=52 for women without funneling, n=85 for women with funneling).
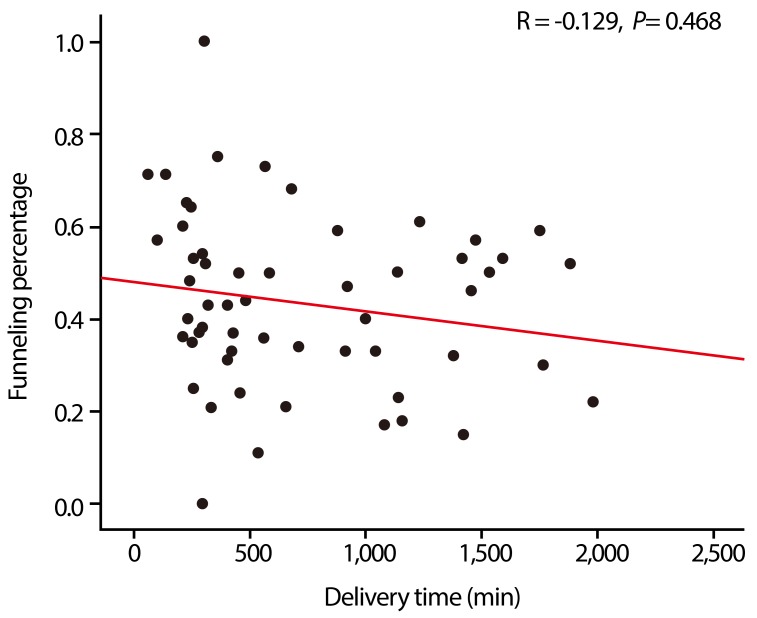
The funneling percentage was negatively correlated with the duration of labor; however, this correlation was not statistically significant (P=0.468) (Fig. 3). Based on the logistic regression analysis, successful labor induction was significantly associated with funneling, as well as the Bishop score and the cervical length (Table 5). However, in a multivariate analysis adjusted for maternal age, gestational age, pre-pregnancy BMI, fetal engagement and premature rupture of membranes, cervical funneling but not the cervical length or Bishop score was significantly associated with successful labor induction (odd ratio, 2.70; 95% confidence interval, 1.02 to 7.10; P=0.04) (Table 5).
Fig. 3. Correlation between the percentage of cervical funneling and labor time. R, Pearson correlation coefficient.
Table 5. Logistic regression analysis for successful vaginal deliverya).
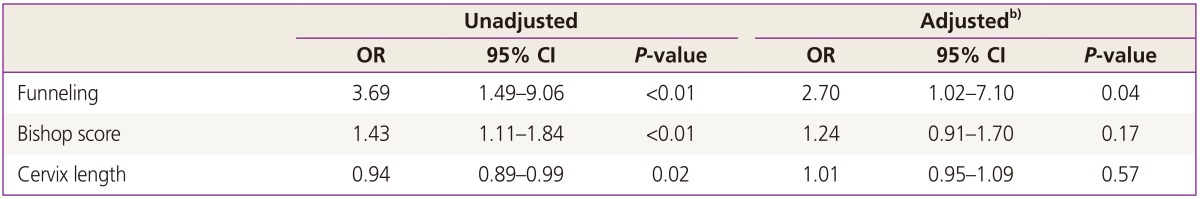
OR, odds ratio; CI, confidence interval.
a)We have conducted multivariate analysis and discussed the problem with statisticians; b)Adjusted for maternal age, gestational age, body mass index before pregnancy, engagement, and premature rupture of membranes.
Discussion
In recent years, labor induction and augmentation have become a widespread convenience for pregnant women, their families, and medical teams. Indeed, Glantz [20] stated that about one-fourth of all labor was induced or augmented. Labor induction has become clinically widespread in South Korea to ensure labor occurs when the obstetricians is in residence. There can be no doubt that elective induction for the convenience of the practitioner or the woman and her family has become more prevalent [2]. This concern for inducing labor when the obstetrician is available has resulted from the gradual decrease in the number of newly created obstetricians/gynecologists per year. In addition, the existing medical doctors have a tendency to avoid delivery. However, as noted, a problem with labor induction and augmentation is the increased possibility of cesarean delivery, particularly in nulliparous women with an unfavorable cervix [3]. Clinicians have to be interested in which patients will have a successful delivery during labor induction, and therefore patients should be examined and assessed for the risk of cesarean delivery resulting from labor induction. The lack of attention in regards to successful labor induction, as well as potential variation between institutions in assessing it, could explain to a certain degree the high and varying rates of cesarean delivery following labor induction. For example, in the United States, Garcia et al. [21] reported that the proportion of cesarean deliveries in academic medical centers was 30% less than in community hospitals. Meanwhile, Nora et al. [22] reported the cesarean delivery rate in local hospitals was 2-fold greater than in public hospitals. According to the Korea Health Insurance Review & Assessment Service published annually, the cesarean delivery rate is very different in each hospital [7]. Indeed, the rate varies between doctors working even in the same hospitals, emphasizing the importance of identifying and studying factors that can be used to predict the success of labor induction.
For a number of decades, the Bishop score has been considered the standard index for determining cervical favorability and thus the likelihood of successful interventions. Even when the Bishop score suffers from wide inter-observer variation because of subjective decision making, it is more objective than cervical length because of the assessment of the cervical state using 5 different factors. However, many pregnant women have complained of pain after pelvic examination. Hence, a method resulting in less discomfort is needed. The cervical length as assessed by vaginal ultrasonography could offer one such possible option. However, in our study, the cervical length was not significant when adjusted for other factors. Our results are in agreement with previous studies [14,15], adding to a growing body of evidence contradicting the early contention that cervical length as evaluated sonographically can be used as a predictor of labor induction success [23,24,25].
Breiger et al. [26] first suggested that cervix funneling should be explored as a predictive marker in parturient women. However, the presence of cervical funneling had no correlation with the evaluated parameter of gestational age, and therefore the findings did not support cervical shape as a predictive marker of labor pain. However, Bayramoglu et al. [27] later reported that cervical funneling could predict the onset of natural labor pain within a week. The results showed that the group with cervical funneling had a higher success rate for labor induction than the group without cervical funneling. Of interest, cervical funneling was observed in 57.1% of the patients, which was higher than the 25% reported by Brieger et al. [26]. A possible explanation for this difference between studies is that no clear criteria had been established in the prior study with respect to the types of the cervical funneling. Hence, the incidence in this previous study might have reflected the subjective tendency of the observers. In the current study, the length was set at a minimum of 15% of the total cervical length.
According to Peregrine et al. [28] and Pevzner et al. [29], the success rate of labor induction is high for multiparity, a BMI of <30, favorable cervix, and fetal body weight of <3,500 g. In the present study, the maternal age had a major impact on the success rate of labor induction, in addition to the Bishop score and cervical length. However, the pre-pregnant BMI and fetal body weight were not related to the success rate of induced labor in the present results, which is in agreement with previous findings [30].
Nonetheless, a limitation of the present study is its limited scope in terms of data and patient number. Further studies involving large-scale assessments are needed to demonstrate that funneling can be used as a predictor of successful labor induction. Other possible study limitations include the occurrence of the premature rupture of membranes. The management of premature rupture of membrane at term continues to be controversial as a best practice has yet to be established. We waited until spontaneous labor and started labor induction about 24 hours, when the risk of chorioamnionitis appear to increase significantly [17]. Only if there was no labor which changed the uterine cervix, the cases were included in this study. An additional limitation was the broad range of gestational ages, which ranged from preterm to postterm. The number of risks that can occur in the delivery process can vary according to the gestational age.
In conclusion, this study showed that the presence of funneling could be a predictor of successful vaginal delivery during labor induction. In addition, the actual duration of labor, including the second stage, was decreased in the funneling group. Observation of cervical funneling by transvaginal ultrasound scanning might be more reliable and convenient than conventional methods such as the Bishop score and cervical length in predicting the success of labor induction. Further, the evaluation of funneling is easier to perform as compared to the other assessments and also results in less patient discomfort.
Acknowledgments
This study was conducted with support of National Health Insurance Service Ilsan Hospital.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al. Births: final data for 2006. Natl Vital Stat Rep. 2009;57:1–136. [PubMed] [Google Scholar]
- 2.Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. Labor induction. In: Cunningham FG, Williams JW, editors. Williams obstetrics. 23rd ed. New York(NY): McGraw-Hill; 2010. pp. 500–510. [Google Scholar]
- 3.Luthy DA, Malmgren JA, Zingheim RW. Cesarean delivery after elective induction in nulliparous women: the physician effect. Am J Obstet Gynecol. 2004;191:1511–1515. doi: 10.1016/j.ajog.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: a review of 7001 consecutive inductions. Am J Obstet Gynecol. 1999;180:628–633. doi: 10.1016/s0002-9378(99)70265-6. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2007. Natl Vital Stat Rep. 2009;57:1–23. [PubMed] [Google Scholar]
- 6.Health Insurance Review & Assessment Service. Cesarean section rate evaluation result by hospitals [Internet] Seoul: Health Insurance Review & Assessment Service; c2013. [cited 2015 Jan 30]. Available from: http://www.hira.or.kr/cms/introduction/02/04/10/2013_14.pdf. [Google Scholar]
- 7.Health Insurance Review & Assessment Service. Cesarean section rate evaluation result by hospitals [Internet] Seoul: Health Insurance Review & Assessment Service; c2012. [cited 2015 Jan 30]. Available from: http://www.hira.or.kr/re/diag/getDiagEvlList.do?pgmid=HIRAA030004000000. [Google Scholar]
- 8.Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol. 1964;24:266–268. [PubMed] [Google Scholar]
- 9.Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334:567–572. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 10.Yang SH, Roh CR, Kim JH. Transvaginal ultrasonography for cervical assessment before induction of labor. J Ultrasound Med. 2004;23:375–382. doi: 10.7863/jum.2004.23.3.375. [DOI] [PubMed] [Google Scholar]
- 11.Tan PC, Vallikkannu N, Suguna S, Quek KF, Hassan J. Transvaginal sonographic measurement of cervical length vs. Bishop score in labor induction at term: tolerability and prediction of Cesarean delivery. Ultrasound Obstet Gynecol. 2007;29:568–573. doi: 10.1002/uog.4018. [DOI] [PubMed] [Google Scholar]
- 12.Berghella V, Bega G, Tolosa JE, Berghella M. Ultrasound assessment of the cervix. Clin Obstet Gynecol. 2003;46:947–962. doi: 10.1097/00003081-200312000-00026. [DOI] [PubMed] [Google Scholar]
- 13.Hatfield AS, Sanchez-Ramos L, Kaunitz AM. Sonographic cervical assessment to predict the success of labor induction: a systematic review with metaanalysis. Am J Obstet Gynecol. 2007;197:186–192. doi: 10.1016/j.ajog.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 14.Crane JM. Transvaginal ultrasound cervical length and successful labor induction: a systematic review. Obstet Gynecol. 2006;107:60S. doi: 10.1016/s0029-7844(01)01386-2. [DOI] [PubMed] [Google Scholar]
- 15.Owen J, Iams JD, Hauth JC. Vaginal sonography and cervical incompetence. Am J Obstet Gynecol. 2003;188:586–596. doi: 10.1067/mob.2003.137. [DOI] [PubMed] [Google Scholar]
- 16.De Carvalho MH, Bittar RE, Brizot Mde L, Bicudo C, Zugaib M. Prediction of preterm delivery in the second trimester. Obstet Gynecol. 2005;105:532–536. doi: 10.1097/01.AOG.0000154157.22500.1d. [DOI] [PubMed] [Google Scholar]
- 17.Wing DA, Farinelli CK. Abnormal labor and induction of labor. In: Gabbe SG, Niebyl JR, Simpson JL, Landon MB, Galan HL, Jauniaux EM, editors. Obstetrics: normal and problem pregnancies. 6th ed. Philadelphia (PA): Churchill Livingstone; 2012. pp. 287–310. [Google Scholar]
- 18.Berghella V, Kuhlman K, Weiner S, Texeira L, Wapner RJ. Cervical funneling: sonographic criteria predictive of preterm delivery. Ultrasound Obstet Gynecol. 1997;10:161–166. doi: 10.1046/j.1469-0705.1997.10030161.x. [DOI] [PubMed] [Google Scholar]
- 19.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012;120:1181–1193. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glantz JC. Labor induction rate variation in upstate New York: what is the difference? Birth. 2003;30:168–174. doi: 10.1046/j.1523-536x.2003.00241.x. [DOI] [PubMed] [Google Scholar]
- 21.Garcia FA, Miller HB, Huggins GR, Gordon TA. Effect of academic affiliation and obstetric volume on clinical outcome and cost of childbirth. Obstet Gynecol. 2001;97:567–576. doi: 10.1016/s0029-7844(00)01219-9. [DOI] [PubMed] [Google Scholar]
- 22.Nora D, Susan R, Edward Y, Mary-Clare D, Alfred S, Larry G. Cesarean section: community versus county hospital. Am J Obstet Gynecol. 2002;187:S183. [Google Scholar]
- 23.Rane SM, Guirgis RR, Higgins B, Nicolaides KH. The value of ultrasound in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2004;24:538–549. doi: 10.1002/uog.1100. [DOI] [PubMed] [Google Scholar]
- 24.Pereira S, Frick AP, Poon LC, Zamprakou A, Nicolaides KH. Successful induction of labor: prediction by preinduction cervical length, angle of progression and cervical elastography. Ultrasound Obstet Gynecol. 2014;44:468–475. doi: 10.1002/uog.13411. [DOI] [PubMed] [Google Scholar]
- 25.Rane SM, Pandis GK, Guirgis RR, Higgins B, Nicolaides KH. Pre-induction sonographic measurement of cervical length in prolonged pregnancy: the effect of parity in the prediction of induction-to-delivery interval. Ultrasound Obstet Gynecol. 2003;22:40–44. doi: 10.1002/uog.165. [DOI] [PubMed] [Google Scholar]
- 26.Brieger GM, Ning XH, Dawkins RR, Ying KQ, Weng C, Chang AM, et al. Transvaginal sonographic assessment of cervical dynamics during the third trimester of normal pregnancy. Acta Obstet Gynecol Scand. 1997;76:118–122. doi: 10.3109/00016349709050065. [DOI] [PubMed] [Google Scholar]
- 27.Bayramoglu O, Arslan M, Yazici FG, Erdem A, Erdem M, Bayramoglu K, et al. Prediction of spontaneous onset of labor at term: the role of cervical length measurement and funneling of internal cervical os detected by transvaginal ultrasonography. Am J Perinatol. 2005;22:35–39. doi: 10.1055/s-2004-837268. [DOI] [PubMed] [Google Scholar]
- 28.Peregrine E, O'Brien P, Omar R, Jauniaux E. Clinical and ultrasound parameters to predict the risk of cesarean delivery after induction of labor. Obstet Gynecol. 2006;107(2 Pt 1):227–233. doi: 10.1097/01.AOG.0000196508.11431.c0. [DOI] [PubMed] [Google Scholar]
- 29.Pevzner L, Rumney P, Petersen R, Wing D. Predicting a successful induction of labor: a secondary analysis of misoprostol vaginal insert trial. Abstract no. 218. Society for Maternal-Fetal Medicine; Proceedings of the 29th Annual Meeting of the Society for Maternal-Fetal Medicine; 2009 Jan 26-31; San Diego, CA, USA. Washington, DC: Society for Maternal-Fetal Medicine; 2009. [Google Scholar]
- 30.Getahun D, Kaminsky LM, Elsasser DA, Kirby RS, Ananth CV, Vintzileos AM. Changes in prepregnancy body mass index between pregnancies and risk of primary cesarean delivery. Am J Obstet Gynecol. 2007;197:376.e1–376.e7. doi: 10.1016/j.ajog.2007.06.015. [DOI] [PubMed] [Google Scholar]