Abstract
Blastocystis has been considered as the most common intestinal parasite in humans and has an augmented impact on public health. However, the prevalence of this parasite in the Philippines has not been determined. To contribute to a better understanding of the epidemiology of this infection, a cross-sectional study aimed at providing the first documented data on the prevalence and correlates, sociodemographic factors, hygiene practices, source of water supply, and dog ownership, associated with Blastocystis infection was carried out in randomly selected communities at Pateros, Metro Manila. Fecal samples from respondents were collected and cultured in diphasic agar medium for 3–7 days and examined using light microscopy. Of the 1,271 respondents, 12.98% (95% CI: 11.13–14.83) were detected positive for Blastocystis. Among the correlates of Blastocystis infection, dog ownership was found significantly associated as confirmed by multivariate analysis. Therefore, this factor should be considered in information to create awareness about Blastocystis and to prevent and control Blastocystis infection in particular and diarrheal diseases in general. Further studies using molecular approaches to distinguish subtype and to determine genetic characteristics of isolates from humans and dogs are recommended to analyze their relationship and provide more conclusive evidence of cross-transmission.
1. Introduction
Blastocystis sp. is currently the most common intestinal protist found in human feces and is considered an emerging parasite with a worldwide distribution [1, 2]. The accepted mode of transmission of the parasite is through the fecal-oral route [3]. Its pathogenic role in humans remains uncertain since Blastocystis infections are both symptomatic and asymptomatic [1]. Nevertheless, it is being associated with various nonspecific gastrointestinal symptoms including diarrhea, abdominal pain, flatulence, anorexia, nausea, and vomiting [4]. The parasite may also be linked to irritable bowel syndrome and inflammatory bowel disease [5–8].
The prevalence of Blastocystis infection is generally higher in developing than in industrialized countries partly because of poor sanitary conditions, consumption of contaminated food or water, and close animal contact [9–12]. Blastocystis infection is being linked with demographic factors such as age, gender, and level of education as well as exposure factors such as hygiene, source of water supply, and exposure to animals [13–16]. Moreover, higher risks of infection and high prevalence have been identified in food and animal handlers, providing conclusive evidence on its zoonotic potential [17–21]. In the Philippines, isolates of Blastocystis subtypes from humans were classified in the same corresponding subtypes as isolates from chickens, monkeys, and pigs in close contact with humans [22].
Diarrhea is still one of the leading causes of morbidity and is included in the top ten notifiable diseases in the Philippines [23–25]. Recent developments associating Blastocystis with diarrhea and showing the protist's zoonotic potential have become the bases of this community-based study. This study aimed to determine the prevalence of Blastocystis infection in humans using culture and light microscopy techniques and to identify which factors are associated with Blastocystis infection using univariate and multivariate analyses. The independent variables studied were age, gender, level of education, hygiene practices, water supply, and dog ownership.
2. Methods
2.1. Study Area and Population
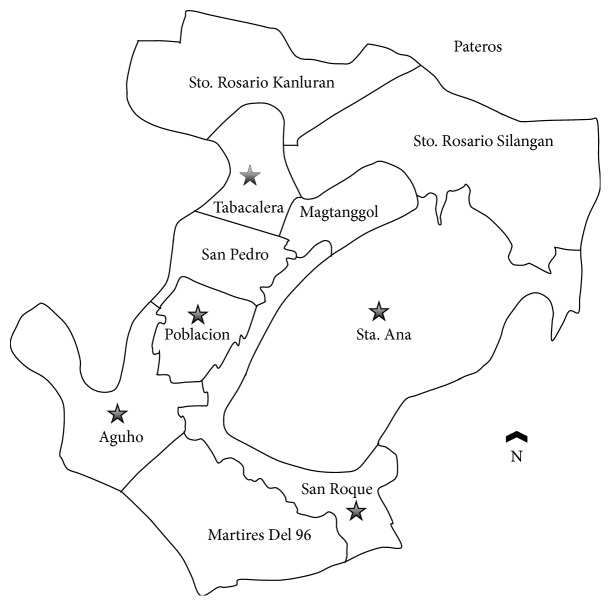
A cross-sectional study was conducted in Pateros, Metro Manila, Philippines, from April 2011 to February 2012 (Figure 1). This urban community, which is mainly residential, consists of ten villages (locally called barangay) with a total population of 60,688 and is located southeast of Metropolitan Manila [25]. Pateros has a median age of 24 years and a sex ratio of 97.5 males for every 100 females [25]. It has population proportion of young dependents (0 to 14 years) of 32.5% and has 64.1% of economically active population (15 to 64 years). One of the great concerns of local health officials is environmental sanitation, particularly potability of water sources, toilet and excreta disposal facilities, and environmental pollution. Diarrhea was reported among the top ten notifiable diseases and was cause of consultations in the health centers in Pateros [26]. The study employed a three-stage random sampling among permanent residents of households in five different villages. The study population consisted of individuals with age > 1 year and those who had not taken antiprotozoal or antidiarrheal medications two weeks prior to sample collection.
Figure 1.
Map showing the location of the villages in Pateros, Metro Manila, Philippines, involved in the study.
2.2. Data Collection
The study utilized pretested interview schedule and direct observation to collect information on the correlates of Blastocystis infection such as sociodemographic factors (age, gender, and level of education) and exposure factors (hand washing, excreta disposal, source of water supply, and dog ownership). Applicability of the questionnaire was determined using a pretest group with similar characteristics as the target population. For children who have reduced ability to judge, their parents or guardians responded on their behalf.
2.3. Sample Collection and Processing of Fecal Specimens
Containers prelabeled with individual's name and identification number and sticks were distributed to each participant. A total of 1,271 stool specimens from humans were collected using three-stage random sampling design (municipality, barangay or village, and then household) and transported immediately to the Molecular Protozoology Laboratory, Natural Sciences Research Institute, University of the Philippines, Diliman, Quezon City, Philippines, for processing and examination. The presence of parasite and stool consistency (formed or diarrheic, mucoid or watery) was determined using gross examination.
2.4. Isolation and In Vitro Cultivation of Blastocystis
Approximately 50 mg stool samples were aseptically inoculated in diphasic medium (1.5% nonnutrient agar overlaid with buffer solution containing 137 mM NaCl, 19.6 mM Na2HPO4, 1.98 mM KH2PO4, and 3.78 mM L-asparagine) supplemented with 10% heat-inactivated horse serum (Gibco, Life Technologies, Carlsbad, CA, USA) and penicillin-streptomycin antibiotics [18]. Samples were incubated at 37°C for 3–7 days and examined for Blastocystis using light microscopy. Samples having the characteristic morphology of Blastocystis under unstained microscopic examination were considered positive for culture. Cultures were reported as negative when there was no observed parasite growth until the last day of incubation.
2.5. Data Management and Statistical Analysis
Data collected from individuals who were positive for culture and completed the questionnaire were computed, coded, and analyzed using STATA Standard Edition version 11.0 for Windows (StataCorp, College Station, TX, USA). Prevalence of Blastocystis infection for humans was estimated at 95% confidence interval (95% CI). Factors having p value ≤ 0.25 in univariate analysis were considered as potential confounders. A percent change in estimate of odds ratio (OR) ≥ 10 was used as basis of significant confounding effect. Identification of association between the studied factors and Blastocystis infection was conducted using multivariate analysis.
2.6. Ethical Issues
Prior to data collection, the study protocol was reviewed and approved by the Ethics Committee of the College of Public Health, University of the Philippines, Ermita, Manila, Philippines, and permission for field work was secured from the City Mayor through the Municipality Health Officer.
3. Results
3.1. Demographic and Socioeconomic Profiles
A total of 1,271 individuals aged 1 to 70 and above participated in this study with a median age of 24.7 ± 19.9 years. The majority of participants were females (60.82%) and most of them belong to age brackets 15–29 (26.12%) and 30–44 (19.35%). Overall, the studied population came from an average socioeconomic background with more than half having more than 6 years of formal education. Among the exposure factors studied (Table 1), hygiene practices showed that most of the respondents wash their hands with soap and water immediately after using toilet (79.94%). Regarding excreta disposal, seven out of 10 (78.99%) had family owned toilets. Lastly, only a few respondents owned dogs (12.27%).
Table 1.
Prevalence of Blastocystis infection among permanent residents of Pateros, Philippines, according to sociodemographic and exposure factors.
| n (%) | % infected | 95% CI | |
|---|---|---|---|
| Overall | 1271 | 12.98 | 11.13–14.83 |
|
| |||
| Sociodemographic factors | |||
| Gender | |||
| Male | 498 (39.18) | 12.65 | 9.75–15.38 |
| Female | 773 (60.18) | 13.20 | 10.81–15.59 |
| Age (in years) | |||
| 1–4 | 165 (12.98) | 7.88 | 3.75–12.01 |
| 5–14 | 239 (18.80) | 15.06 | 10.51–19.61 |
| 15–29 | 332 (26.12) | 13.25 | 9.60–16.91 |
| 30–44 | 246 (19.35) | 14.23 | 9.85–18.61 |
| 45–59 | 195 (15.34) | 12.8 | 8.11–17.53 |
| 60–69 | 60 (4.72) | 8.33 | 1.27–15.39 |
| 70 and above | 34 (2.68) | 20.59 | 6.78–34.40 |
| Level of education | |||
| College | 331 (26.04) | 10.27 | 6.99–13.55 |
| High school | 431 (33.91) | 15.78 | 12.33–19.23 |
| Elementary | 306 (24.08) | 12.09 | 8.43–15.75 |
| No education | 203 (15.97) | 12.81 | 8.19–17.41 |
|
| |||
| Exposure factors | |||
| Hygiene practices | |||
| Hand washing | |||
| Wash hands with soap and water immediately after using toilet | 1016 (79.94) | 14.17 | 12.03–16.32 |
| Wash hands with water only after using toilet | 162 (12.75) | 8.64 | 4.30–12.99 |
| Wash hands with soap and water but delays washing for more than 5 minutes after using toilet | 93 (7.32) | 7.52 | 2.13–12.92 |
| Excreta disposal | |||
| Family owned toilet | 1003 (78.99) | 14.04 | 11.89–16.20 |
| Communal toilet | 267 (21.01) | 8.99 | 5.54–12.43 |
| Water supply | |||
| Public water system | 1085 (85.37) | 12.53 | 10.56–14.51 |
| Communal faucet | 186 (14.63) | 15.59 | 10.35–20.82 |
| Dog ownership | |||
| Nondog owner | 1115 (87.73) | 11.30 | 9.43–13.16 |
| Dog owner | 156 (12.27) | 25.00 | 18.18–32.18 |
n: number of examined.
3.2. Prevalence and Distribution of Blastocystis Infection
The overall prevalence of Blastocystis infection in humans was 12.98% (95% CI: 11.13%–14.83%). Both males and females had almost equal prevalence (12.65%, 95% CI: 9.75%–15.38% and 13.20%, 95% CI: 10.81%–15.59%). Figure 2 shows Blastocystis prevalence (%) according to age of the subjects in years. High school educational level on the other hand had the highest prevalence when grouped according to education (15.78%) (Table 1). Lastly, one for every four dog owners (25%, 95% CI: 18.18%–32.18%) was found positive with Blastocystis.
Figure 2.
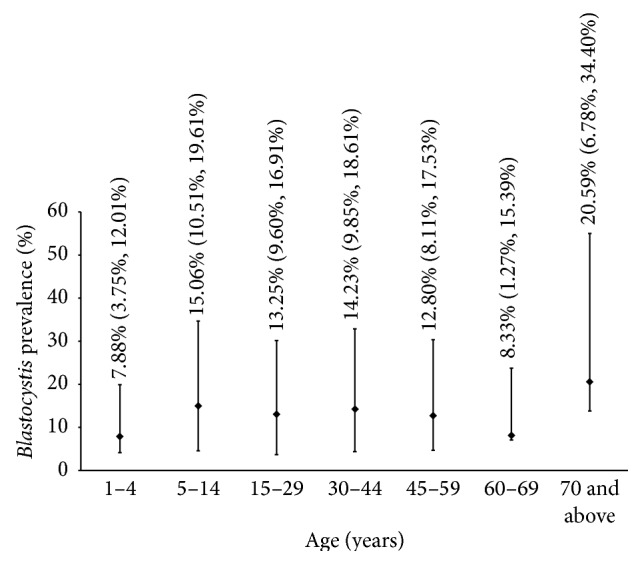
Graph showing Blastocystis prevalence (%) versus age (years).
3.3. Statistical Analysis
Potential confounders (p ≤ 0.25) such as sociodemographic factors (age and level of education), hygiene practices (hand washing and excreta disposal), water supply, and dog ownership, identified using univariate analysis, were included in multivariate analysis. Among the tested potential confounders, there was no significant confounding effect to association between Blastocystis infection and the tested predictors (% change in estimate of OR ≥ 10). Results of multivariate analysis showed that only dog ownership was significantly associated with Blastocystis infection (Table 2). The odds of having Blastocystis infection were 2.6 times higher among dog owners than nondog owners (OR = 2.6, 90% CI: 1.9–3.7, p = 0.000). Associations of other factors such as sociodemographic factors (OR = 1.0, 90% CI: 0.7–1.3, OR = 3.0, 90% CI: 1.3–5.1, and OR = 1.8, 90% CI: 1.2–2.6), hygiene practices (OR = 1.6, 90% CI: 1.0–2.5 and OR = 1.7, 90% CI: 1.0–2.5), and water supply (OR = 1.4, 90% CI: 1.0–2.0) to Blastocystis infection were weak and not statistically significant.
Table 2.
Final models for various factors and association with Blastocystis infection.
| Adjusted OR (90% CI) | p value | |
|---|---|---|
| Final Model 1: association between sociodemographic factors and Blastocystis | ||
| Sociodemographic factors | ||
| Gender | ||
| Male∗ | 1.0 (—) | — |
| Female | 1.0 (0.7–1.3) | 0.919 |
| Age (in years) | ||
| 1–4∗ | 1.0 (—) | — |
| 5–59 | 3.0 (1.3–5.1) | 0.020 |
| 60 and above | 2.0 (0.8–4.5) | 0.186 |
| Level of education | ||
| College∗ | 1.0 (—) | — |
| High school | 1.8 (1.2–2.6) | 0.179 |
| Elementary | 1.4 (0.9–2.1) | 0.040 |
| No education | 3.0 (1.7–5.4) | 0.002 |
|
| ||
| Final Model 2: association between hygiene practices and Blastocystis | ||
| Hygiene practices | ||
| Hand washing | ||
| With soap and water immediately∗ | 1.0 (—) | — |
| With water only or delayed washing | 1.6 (1.0–2.5) | 0.091 |
| Excreta disposal | ||
| Family owned toilet∗ | 1.0 (—) | — |
| Communal faucet | 1.7 (1.1–2.5) | 0.036 |
|
| ||
| Final Model 3: association between source of water supply and Blastocystis infection | ||
| Water supply | ||
| Public water system∗ | 1.0 (—) | — |
| Communal toilet | 1.4 (1.0–2.0) | 0.135 |
|
| ||
| Final Model 4: association between dog ownership and Blastocystis infection | ||
| Dog ownership | ||
| Nondog owner∗ | 1.0 (—) | — |
| Dog owner | 2.6 (1.9–3.7) | 0.000 |
∗Reference.
4. Discussion
Infection with Blastocystis is a common health problem in many tropical and subtropical areas of the world, especially in developing countries. In the Philippines, studies on the prevalence and correlates of Blastocystis sp. are not well documented. This study was the first investigation on the prevalence and epidemiology of Blastocystis in an urban community.
This study determined the prevalence of Blastocystis using culture and light microscopy techniques and its association with various factors using univariate and multivariate analyses. Culture method was preferred because of its higher sensitivity and specificity compared to direct fecal smear microscopy [27] and stool polymerase chain reaction (PCR) [28, 29]. Santos and Rivera [28] considered in vitro culture as the gold standard in detecting Blastocystis cells and reported sensitivity of the following methods: 19.4% for direct fecal smear method, 19.4% for PCR from stool, and 66.7% for PCR from Blastocystis culture. However, in vitro culture is a selective technique; it is affected by the composition of medium used and the protocol applied in cultivation [28]. Thus, some isolates of Blastocystis are refractory to in vitro culture. Stensvold et al. [30] reported 100% sensitivity and specificity for culture when compared with formol-ethyl acetate concentration (FECT), trichrome staining, and xenic in vitro culture using PCR. Roberts et al. [31] observed 82.6% sensitivity and 100% specificity for culture. In the same year, conventional polymerase chain reaction (PCR) was found to be the most effective [31]. However, factors like requirement for special equipment (PCR machine), high cost, and need for intensive labor limited its use in this study. Compared with PCR, culture method is a cost-effective method for Blastocystis detection in stool, and it can also yield valid prevalence estimates. Lastly, culture method has high detection rate, since Blastocystis are allowed to grow and propagate, even starting with low infection.
Results show prevalence of 12.98% (~13%) in the study population. High prevalence rates were found among individuals aged 5–59 (79.61%) and those who owned dogs (25%). With regard to age, a possible reason may be an increased exposure of individuals to the parasite. Studies in endemic areas of Nicaragua [32], Bangladesh [33], and Brazil [34] showed peak prevalence of Blastocystis in age group 5–14. The determined prevalence rate in this study was close to the 12% reported prevalence of the Department of Parasitology in University of the Philippines Manila among prescreened clients referred from hospitals and travel agencies (unpublished data). This study shows that stool culture method is more sensitive because it allows even few Blastocystis to grow and multiply.
Several factors that may be associated with risk of Blastocystis infection, namely, sociodemographic factors (age, gender, and level of education), hygiene practices (hand washing and excreta disposal), source of water supply, and dog ownership, were analyzed in this study. Multivariate analysis identified significant association of dog ownership with Blastocystis infection. Dog ownership as a potential risk factor may be attributed to the zoonotic potential of Blastocystis. Doyle et al. [35] observed that individuals who had close contact with animals, mainly pets, could be found positive for Blastocystis infection. In another study, Salim et al. [20] observed animal handlers in Malaysia and reported that exposure of animal handlers to their animals was associated with Blastocystis infection (p = 0.0000313).
5. Conclusion
The prevalence of Blastocystis was 12.98% in Pateros, Metro Manila. Such data is indicative of the probability of acquiring this parasite in this community. Among the correlates studied, dog ownership was significantly associated with Blastocystis infection. The borderline confidence interval of this factor showed positive direction to association with Blastocystis infection. This factor could be considered to have important role in the transmission of Blastocystis infection, and understanding it provides better interventions in its prevention and control.
Acknowledgments
The authors are grateful to the following colleagues for providing comments for unpublished results and technical assistance: Kim L. Cochon and Maylin C. Palatino (University of the Philippines, Manila, Philippines) and Davin Edric V. Adao (University of the Philippines, Diliman, Quezon City, Philippines). This work was supported financially by the Philippine Department of Science and Technology-Science Education Institute and the Natural Sciences Research Institute, University of the Philippines, Diliman, Quezon City, Philippines.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Tan K. S. W. New insights on classification, identification, and clinical relevance of Blastocystis spp. Clinical Microbiology Reviews. 2008;21(4):639–665. doi: 10.1128/cmr.00022-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alfellani M. A., Stensvold C. R., Vidal-Lapiedra A., Onuoha E. S. U., Fagbenro-Beyioku A. F., Clark C. G. Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Tropica. 2013;126(1):11–18. doi: 10.1016/j.actatropica.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 3.Yoshikawa H., Yoshida K., Nakajima A., Yamanari K., Iwatani S., Kimata I. Fecal-oral transmission of the cyst form of Blastocystis hominis in rats. Parasitology Research. 2004;94(6):391–396. doi: 10.1007/s00436-004-1230-5. [DOI] [PubMed] [Google Scholar]
- 4.Tan K. S. W., Mirza H., Teo J. D. W., Wu B., MacAry P. A. Current views on the clinical relevance of Blastocystis spp. Current Infectious Disease Reports. 2010;12(1):28–35. doi: 10.1007/s11908-009-0073-8. [DOI] [PubMed] [Google Scholar]
- 5.Abe N. Molecular and phylogenetic analysis of Blastocystis isolates from various hosts. Veterinary Parasitology. 2004;120(3):235–242. doi: 10.1016/j.vetpar.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Sheehan D. J., Raucher B. G., McKitrick J. C. Association of Blastocystis hominis with signs and symptoms of human disease. Journal of Clinical Microbiology. 1986;24(4):548–550. doi: 10.1128/jcm.24.4.548-550.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poirier P., Wawrzyniak I., Vivarès C. P., Delbac F., El Alaoui H. New insights into Blastocystis spp.: a potential link with irritable bowel syndrome. PLoS Pathogens. 2012;8(3) doi: 10.1371/journal.ppat.1002545.e1002545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boorom K. F., Smith H., Nimri L., et al. Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection. Parasites & Vectors. 2008;1(1, article 40) doi: 10.1186/1756-3305-1-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee L. I., Chye T. T., Karmacharya B. M., Govind S. K. Blastocystis sp.: waterborne zoonotic organism, a possibility? Parasites and Vectors. 2012;5(1, article 130) doi: 10.1186/1756-3305-5-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li L.-H., Zhou X.-N., Du Z.-W., et al. Molecular epidemiology of human Blastocystis in a village in Yunnan province, China. Parasitology International. 2007;56(4):281–286. doi: 10.1016/j.parint.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Eroglu F., Genc A., Elgun G., Koltas I. S. Identification of Blastocystis hominis isolates from asymptomatic and symptomatic patients by PCR. Parasitology Research. 2009;105(6):1589–1592. doi: 10.1007/s00436-009-1595-6. [DOI] [PubMed] [Google Scholar]
- 12.Graczyk T. K., Shiff C. K., Tamang L., Munsaka F., Beitin A. M., Moss W. J. The association of Blastocystis hominis and Endolimax nana with diarrheal stools in Zambian school-age children. Parasitology Research. 2005;98(1):38–43. doi: 10.1007/s00436-005-0003-0. [DOI] [PubMed] [Google Scholar]
- 13.Duda A., Stenzel D. J., Boreham P. F. L. Detection of Blastocystis sp. in domestic dogs and cats. Veterinary Parasitology. 1998;76(1-2):9–17. doi: 10.1016/s0304-4017(97)00224-0. [DOI] [PubMed] [Google Scholar]
- 14.Nimri L. F. Evidence of an epidemic of Blastocystis hominis infections in preschool children in Northern Jordan. Journal of Clinical Microbiology. 1993;31(10):2706–2708. doi: 10.1128/jcm.31.10.2706-2708.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taamasri P., Mungthin M., Rangsin R., Tongupprakarn B., Areekul W., Leelayoova S. Transmission of intestinal blastocystosis related to the quality of drinking water. Southeast Asian Journal of Tropical Medicine and Public Health. 2000;31(1):112–117. [PubMed] [Google Scholar]
- 16.Suresh K., Smith H. V., Tan T. C. Viable Blastocystis cysts in Scottish and Malaysian sewage samples. Applied and Environmental Microbiology. 2005;71(9):5619–5620. doi: 10.1128/aem.71.9.5619-5620.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoshikawa H., Wu Z., Pandey K., et al. Molecular characterization of Blastocystis isolates from children and rhesus monkeys in Kathmandu, Nepal. Veterinary Parasitology. 2009;160(3-4):295–300. doi: 10.1016/j.vetpar.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 18.Yoshikawa H., Wu Z., Kimata I., et al. Polymerase chain reaction-based genotype classification among human Blastocystis hominis populations isolated from different countries. Parasitology Research. 2004;92(1):22–29. doi: 10.1007/s00436-003-0995-2. [DOI] [PubMed] [Google Scholar]
- 19.Yoshikawa H., Wu Z., Nagano I., Takahashi Y. Molecular comparative studies among Blastocystis isolates obtained from humans and animals. Journal of Parasitology. 2003;89(3):585–594. doi: 10.1645/0022-3395(2003)089[0585:mcsabi]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 20.Salim H. R., Kumar G. S., Vellayan S., et al. Blastocystis in animal handlers. Parasitology Research. 1999;85(12):1032–1033. doi: 10.1007/s004360050677. [DOI] [PubMed] [Google Scholar]
- 21.Parkar U., Traub R. J., Vitali S., et al. Molecular characterization of Blastocystis isolates from zoo animals and their animal-keepers. Veterinary Parasitology. 2010;169(1-2):8–17. doi: 10.1016/j.vetpar.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 22.Rivera W. L. Phylogenetic analysis of Blastocystis isolates from animal and human hosts in the Philippines. Veterinary Parasitology. 2008;156(3-4):178–182. doi: 10.1016/j.vetpar.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Health and Welfare. Philippine Yearbook. 2011. http://www.census.gov.ph/sites/default/files/2011PY_Health%20and%20Welfare.pdf. [Google Scholar]
- 24.National Statistics Office. The Philippines in Figures, Manila, Philippines. National Statistics Office; 2006. [Google Scholar]
- 25.Department of Health. National Epidemiology Center. The 2009 Philippine Health Statistics. 2009. http://www.doh.gov.ph/sites/default/files/PHILIPPINE%20HEALTH%20STATISTICS%202009_0.pdf. [Google Scholar]
- 26. Pateros Health Department Annual Report, 2010.
- 27.Leelayoova S., Taamasri P., Rangsin R., Naaglor T., Thathaisong U., Mungthin M. In-vitro cultivation: a sensitive method for detecting Blastocystis hominis . Annals of Tropical Medicine and Parasitology. 2002;96(8):803–807. doi: 10.1179/000349802125002275. [DOI] [PubMed] [Google Scholar]
- 28.Santos H. J., Rivera W. L. Comparison of direct fecal smear microscopy, culture, and polymerase chain reaction for the detection of Blastocystis sp. in human stool samples. Asian Pacific Journal of Tropical Medicine. 2013;6(10):780–784. doi: 10.1016/s1995-7645(13)60138-8. [DOI] [PubMed] [Google Scholar]
- 29.Termmathurapoj S., Leelayoova S., Aimpun P., et al. The usefulness of short-term in vitro cultivation for the detection and molecular study of Blastocystis hominis in stool specimens. Parasitology Research. 2004;93(6):445–447. doi: 10.1007/s00436-004-1157-x. [DOI] [PubMed] [Google Scholar]
- 30.Stensvold C. R., Nielsen H. V., Mølbak K., Smith H. V. Pursuing the clinical significance of Blastocystis—diagnostic limitations. Trends in Parasitology. 2009;25(1):23–29. doi: 10.1016/j.pt.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 31.Roberts T., Barratt J., Harkness J., Ellis J., Stark D. Comparison of microscopy, culture, and conventional polymerase chain reaction for detection of Blastocystis sp. in clinical stool samples. American Journal of Tropical Medicine and Hygiene. 2011;84(2):308–312. doi: 10.4269/ajtmh.2011.10-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tellez Sierra A., Cortez Ruiz L., Aust Kettis A., Huldt G., Jonsson J., Schroder H. Amebiasis in Nicaragua: class specific serum antibody responses. Archives of Medical Research. 1992;23(2):261–264. [PubMed] [Google Scholar]
- 33.Hossain M. M., Ljungstrom I., Glass R. I., Lundin L., Stoll B. J., Huldt G. Amoebiasis and giardiasis in Bangladesh: parasitological and serological studies. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1983;77(4):552–554. doi: 10.1016/0035-9203(83)90135-9. [DOI] [PubMed] [Google Scholar]
- 34.Braga L. L., Lima A. A. M., Sears C. L., et al. Seroepidemiology of Entamoeba histolytica in a slum in northeastern Brazil. The American Journal of Tropical Medicine and Hygiene. 1996;55(6):693–697. doi: 10.4269/ajtmh.1996.55.693. [DOI] [PubMed] [Google Scholar]
- 35.Doyle P. W., Helgason M. M., Mathias R. G., Proctor E. M. Epidemiology and pathogenicity of Blastocystis hominis . Journal of Clinical Microbiology. 1990;28(1):116–121. doi: 10.1128/jcm.28.1.116-121.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]