Abstract
Introduction
The surgical removal of impacted third molars involves, trauma to soft and bony tissue and can result in considerable pain, swelling, and trismus. The greater the amount of tissue injury the greater is the amount of inflammation in the perisurgical region. Interleukin-6 (IL-6) is both a pro inflammatory and anti-inflammatory cytokine. It is secreted by T cells and macrophages to stimulate the immune response. IL-6 is also an early marker of tissue damage. In addition to NSAIDs, corticosteroids, opioids also have immunomodulatory effects.
Aim
To evaluate the changes in serum IL-6 levels following surgical removal of third molars under local anaesthesia after administration of two NSAIDs diclofenac and ketorolac and opioid tramadol post operatively.
Methods
Patients undergoing surgical removal of impacted mandibular third molar teeth were randomly assigned to three groups. Each group received one of the three analgesics viz diclofenac 50 mg, ketorolac 10 mg and tramadol 50 mg. The mean levels of IL-6 was then estimated by ELISA.
Results
The results of our study showed that all three drugs i.e. diclofenac, ketorolac and tramadol have properties which can downregulate the production of IL-6 in response to surgical trauma.
Conclusion
It is of clinical significance that the suppression of IL-6 values occurs in tramadol group closely following the diclofenac group. Even though the drug ketorolac suppresses the IL-6 levels similar to diclofenac initially but after 7 days tramadol and ketorolac showed similarities in suppression of IL-6 expression which is less compared to diclofenac group.
Keywords: Interleukin-6, Diclofenac, Ketorolac, Tramadol, Third molar surgery
Introduction
One of the major challenges after third molar removal is pain and swelling of surrounding tissues and resulting morbidity. Pain not only signals tissue injury, but also acts as an impediment to dental procedures and delays resumption of normal activities after the procedure. Various methods for achieving control of the post-surgical morbidity are the use of steroids (IV and oral), NSAIDs, pre-emptive analgesia, synthetic opioids, combined use of steroids and analgesics, etc.
Interleukin 6 is a protein that, in humans, is encoded by the IL-6 gene and is secreted by many cells in response to trauma especially burns or other tissue damage leading to inflammation [1]. IL-6 is both a pro inflammatory and anti-inflammatory cytokine. It is secreted by T cells and macrophages to stimulate the immune response.
IL-6 is one of the most important mediators of fever and of the acute phase response. The concentration of IL-6 may change depending on the anti-inflammatory used during the post-operative period.
The aim of this study is to evaluate the changes in serum Interleukin-6 (IL-6) levels following surgical removal of third molars under local anaesthesia after oral administration of two NSAIDs, diclofenac and ketorolac and opioid tramadol post operatively. It would help the clinicians to better understand the effect of anti-inflammatory drugs on the immunological pathways leading to post-operative sequel after third molar surgeries.
Materials and Methods
A Prospective Randomised Double Blind Clinical Trial was carried out in the Department of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, Herbal & Indian Medicine Research Laboratory, Sri Ramachandra University, Porur, Chennai for the duration of 6 months. In this study the patients were divided into three treatment groups as ketorolac, diclofenac and tramadol. The mean levels of IL-6 were assessed after the oral administration of diclofenac, ketorolac and tramadol. With 5 % level of significance and 80 % power, the required sample size selected was 20. The patients were selected according to the inclusion and exclusion criteria. Only one tooth was removed in each subject.
Inclusion Criteria
Healthy subjects,
Age: over 18 years
Sex: both genders
Patients without contraindications for NSAIDs treatment
All patients who required ostectomy and tooth sectioning to achieve extraction.
Patients who required surgical removal of any lower third molar with Pederson difficulty index ranging from 5 to 7 i.e. moderately difficult.
ASA I patients
Exclusion Criteria
Pregnant and lactating women.
Medically compromised patients including, corticosteroid therapy.
Patients who had taken analgesics or anti-inflammatory drugs within 7 days before surgery.
Patients with smoking habit
Patients with systemic pathologies
The subjects meeting the above mentioned criteria were included in the study. At the baseline visit, complete dental examination for initial documentation including medical history and dental history was undertaken. Clinical investigations included intra oral periapical radiographs and orthopantomogram. Ethical approval was obtained from IEC Sri Ramachandra University, Chennai. Randomization was carried out by draw system by the patients undergoing the surgery just before the procedure started.
Patients undergoing surgical removal of impacted mandibular third molar teeth were divided randomly into 3 groups.
- Group 1:
included 21 patients, who were given Tab diclofenac 50 mg BD for 5 days post-operatively,
- Group 2:
included 20 patients who were given Tab ketorolac 10 mg TDS for 5 days post-operatively and
- Group 3:
included 16 patients who were given Tab tramadol 50 mg BD for 5 days post-operatively
None of the patients had received pre-operatively and post-operatively corticosteroids in any form. Cap Amoxicillin 500 mg TDS was administered to all 3 groups as antibiotic and Tab Rantac 150 mg BD was given to groups 1 and 2 as antacid. Tab Emeset 4 mg BD was given to group 3 as antiemetic. Blood samples were collected pre-operatively, 24 h, 72 h and after 1 week and Intereukin-6 level was estimated in the following manner.
Venous blood sample, 3 ml, was taken from the cubital fossa of the patients 4 times and serum was separated by centrifugation.
Serum samples were stored in a vial and frozen at minus 30° C.
The collected samples were assayed using e-Bioscience ELISA kits in accordance with the standard protocol and values of Interleukin 6 interpolated.
Surgical Technique
Surgery was carried out under local anaesthesia, using a maximum of three vials of 1.8-ml of 2 % xylocaine with adrenalin (1:200,000). Inferior alveolar nerve block was administered. Buccal extension flap design was used in all impactions and ostectomy of the contiguous bone with a tapering fissure bur and the teeth sectioned with a fissure bur (carbide no. 702 or 703). Tooth split was done if it was needed. All the procedures were performed using a low-speed straight hand piece, under constant irrigation, with cool sterile physiological saline solution. After the tooth was removed from the socket, irrigation was done with 5 % povidone iodine solution. Flap was sutured with a 3–0 silk suture.
Follow Up
Routine follow ups were done on 1, 3 and 7 post-operative days. Suture removal was done at 1 week. Blood samples were taken from the patient from cubital fossa and centrifuged at 1,500 rpm at 24 °C for 10 min and serum separated and stored in eppendoff vials at −30 °C till interleukin 6 estimation.
Statistical Analysis
The collected data was subjected to statistical analysis using SPSS software version 15.
Results
In this randomised double blind prospective study 57 patients with lower third molar extraction were taken up for serum IL-6 estimation. Thirty-three patients were males (57.9 %) and 24 patients were females (42.1 %). Radiographic analysis of the type of impaction showed that mesioangular impaction constituted 35.1 % of the total cases, followed by distoangular impactions 28.1 %, and then vertical 21.1 % and least were horizontal 15.8 % in the complete study group. In our study we have compared the IL-6 values after commonly performed oral surgical procedure i.e. surgical removal of lower third molars and observed the variations after oral administration of two different NSAIDs diclofenac and ketorolac along with one semi-synthetic opioid tramadol over a period of 7 days. The data has been depicted in Tables 1–6.
Table 1.
Comparison between the pre-operative, 24 h, 72 h and 1 week values of all the 3 drugs administered with mean values and standard deviation
| N | Mean | Std. deviation | Std. error | |
|---|---|---|---|---|
| pre op | ||||
| Diclofenac | 21 | 4.6699134 | 1.557753043 | .339929583 |
| Ketorolac | 20 | 5.3181819 | 1.893745910 | .423454459 |
| Tramadol | 16 | 4.9964490 | 1.811240222 | .452810056 |
| Total | 57 | 4.9890352 | 1.743284047 | .230903613 |
| 24 h | ||||
| Diclofenac | 21 | 7.1428570 | 1.788833494 | .390356562 |
| Ketorolac | 20 | 7.6619320 | 2.310703438 | .516690114 |
| Tramadol | 16 | 10.078126 | 4.723906644 | 1.180976661 |
| Total | 57 | 8.1489236 | 3.234093734 | .428366180 |
| 72 h | ||||
| Diclofenac | 20 | 4.4204546 | 1.248313352 | .279131351 |
| Ketorolac | 20 | 5.2215907 | 1.539662951 | .344279102 |
| Tramadol | 16 | 5.2166193 | 1.740432649 | .435108162 |
| Total | 55 | 4.9340503 | 1.527275819 | .204090816 |
| 1 week | ||||
| Diclofenac | 20 | 6.1562499 | 1.270128735 | .284009419 |
| Ketorolac | 20 | 7.2414776 | 2.128456095 | .475937252 |
| Tramadol | 16 | 6.8075285 | 1.975031390 | .493757848 |
| Total | 56 | 6.7299108 | 1.844652568 | .246502068 |
Table 6.
Values at 24 h for the IL-6 levels of ketorolac and diclofenac and tramadol
| Dependent variable | (I) Drug | (J) Drug | Mean difference (l-J) | Std. error | Sig. |
|---|---|---|---|---|---|
| Pre OP | Diclofenac | Ketorolac | −.643263471 | .547604342 | .242 |
| Tramadol | −.326535571 | .581609242 | .577 | ||
| Ketorolac | Diclofenac | .648268471 | .547604942 | .242 | |
| Tramadol | .321732900 | .587863285 | .536 | ||
| Tramadol | Diclofenac | .326535571 | .581609242 | .577 | |
| Ketorolac | −.321732900 | .587863235 | .586 | ||
| 24 h | Diclofenac | Ketorolac | −.519075098 | .950893739 | .587 |
| Tramadol | −2.9352687 | 1.009940325 | .005 | ||
| Ketorolac | Diclofenac | .519075098 | .950893739 | .537 | |
| Tramadol | −2.4161936 | 1.020300716 | .022 | ||
| Tramadol | Diclofenac | 2.93526374 | 1.009940325 | .005 | |
| Ketorolac | 2.41619364 | 1.020800716 | .022 | ||
| 72 h | Diclofenac | Ketorolac | −.801136150 | .475998657 | .098 |
| Tramadol | −.796164712 | .504873030 | .121 | ||
| Ketorolac | Diclofenac | .801136150 | .475993857 | .098 | |
| Tramadol | .004971430 | .504873030 | .992 | ||
| Tramadol | Diclofenac | .796164712 | .504873030 | .121 | |
| Ketorolac | −.004971438 | .504373030 | .992 | ||
| 1 week | Diclofenac | Ketorolac | −1.0852277 | .575012272 | .065 |
| Tramadol | −.651273650 | .609892615 | .290 | ||
| Ketorolac | Diclofenac | 1.08522770 | .575012272 | .065 | |
| Tramadol | .433949050 | .609392615 | .480 | ||
| Tramadol | Diclofenac | .651273650 | .609892615 | .290 | |
| Ketorolac | −.433949050 | .609892615 | .480 |
p = .005 for diclofenac versus tramadol and p = .022 for ketorolac versus tramadol
Discussion
IL-6 is a cytokine that mediates communication between a large number of cell types by playing a role in the proliferation and differentiation of B lymphocytes, plasmacytomas and hybridomas, hematopoietic progenitors, hepatocytes and T-lymphocytes.
Thus IL-6 is considered a major immune and inflammatory mediator. Trauma or infection causes plasma level of IL-6 to rise. As an early alarm cytokine it recruits adjacent stromal cells to release high levels of IL-6 and other mediators. The sequential activation and cytokine cascade leads to raised IL-6 levels in inflammation. Since IL-6 can induce cortisol levels and cortisol is required for hepatic acute phase response, IL-6 plays an inductive role as a second signal to the liver.
Mahdy et al. [2] found that diclofenac is associated with lower IL-6 concentrations and hence may have an anti-inflammatory role to play after major surgeries. At 12 h the IL-6 concentration was significantly lower in patients receiving diclofenac than the placebo group.
In a prospective study of 22 patients Myung Hee Kim et al. [3] compared the effect of morphine and morphine-ketorolac administered to 2 groups of patients on the concentrations of IL-6 post surgically. They found lower IL-6 response in morphine-ketorolac group as compared to morphine group 24 h post-operatively. It may indicate that cyclooxygenase inhibitor ketorolac may have an important role in the attenuation of IL-6 response via inhibition of prostaglandin E2.
In their study Eman A. Sharrawy et al. [4] concluded that the combination of tramadol and NSAID ibuprofen appeared to produce supra-additive anti-inflammatory effects that may provide clinical advantages in safety or efficacy for treating postsurgical dental pain.
In a study conducted by Mishra et al. [5] on 74 patients, who underwent third molar extractions, they concluded that tramadol is equally effective as ketorolac in relieving pain in the first 6 h after molar extraction and therefore can be tried in patients who are intolerant to nonsteroidal anti-inflammatory drugs.
In a study conducted on rats Yong-Min Liu et al. [6] concluded that tramadol was associated with decreased IL-6 and unchanged IL-2 levels, thus suggesting that tramadol may supress the inflammation induced by incision and has beneficial role in the modulation of IL-2 associated cell mediated immunity.
The presence of cyclooxygenase inhibitors at the surgical site may limit the production of prostaglandins and prostacyclins associated with hyperalgesia and edema. Post-operative swelling and edema may be in part due to the conversion of phospholipids to arachidonic acid by phospholipase A2 resulting in the production of leukotrienes, prostacyclins, prostaglandins and thromboxane A2 which are mediators of the inflammatory response.
By pharmacologically controlling the extent of the inflammatory process the intensity and the severity of the post-operative sequelae such as pain, swelling and trismus may be reduced. Prostaglandins play a major role in the induction of pain, inflammation and fever.
As evident in the study by Babatunde et al. [7] the reduction of biosynthesis of prostaglandins by inhibition of cyclooxygenase enzyme system is considered an important mechanism of action of NSAIDs. Prostaglandin E2 is the predominant eicosanoid released after surgical trauma and has been associated with inflammation, pain and fever. Surgery leads to a complex systemic response in plasma PGE2 and IL-6 despite perioperative neuronal blockade.
May Hazma et al. [8] have reported downregulation of gene and protein expression of phosphodiesterase type IV enzyme by rofecoxib and ketorolac in oral mucosal biopsies 3 h after third molar tooth extraction. NFκB also plays an important role in the upregulation of IL-6 in response to several inflammatory mediators. It is known that different non-opioids produce variable effects on the activation of NFκB. NFκB inhibition lowers peptidoglycan- and PGE2 induced IL-6 production in RAW 264.7 macrophages.
The authors have shown in a study that selective COX-2 inhibitor NS398, inhibited the peptidoglycan-induced NFκB specific DNA protein complex formation from 2 to 12 h of treatment, but not in the first 60 min, suggesting that NFκB activation may be PGE2/cAMP dependant. Furthermore the authors have reported an increase in gene and protein expression of SOCS3 in response to both rofecoxib and ibuprofen in the oral mucosa 48 h after tissue injury and acute inflammation in the oral surgery model. Over expression of SOCS3 blocks the proinflammatory effects of IL-6 signalling through gene peptide.
Thus even if non-opioids under certain conditions might upregulate IL-6 production, an accompanying over expression of SOCS3 might in fact block its proinflammatory effects. In our study we have compared the IL-6 values after commonly performed oral surgical procedure i.e. surgical removal of lower third molars and observed the variations after administering two different NSAIDs, Diclofenac and Ketorolac along with one semi-synthetic opioid Tramadol over a period of 7 days.
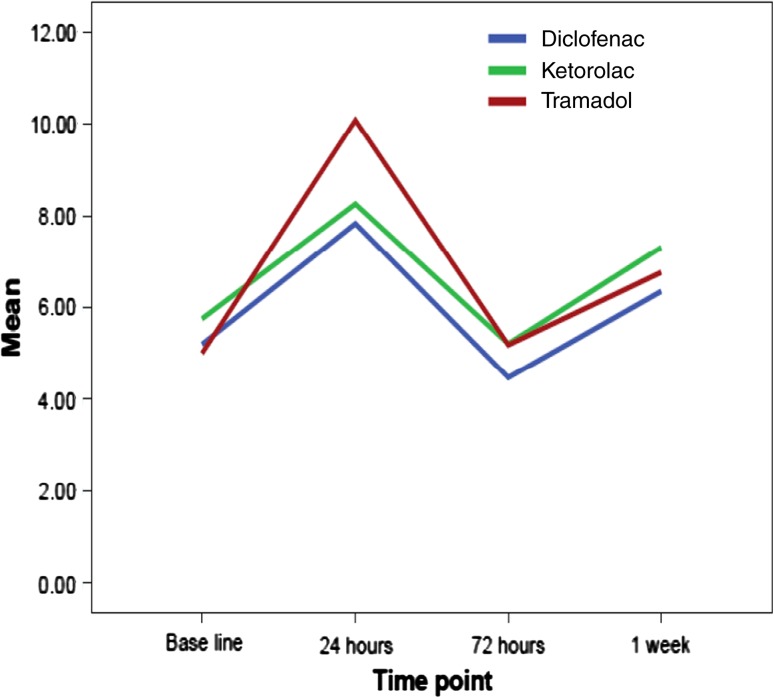
In the present study the mean concentrations of IL-6 in diclofenac group were 4.66 + 1.55 pg/ml in pre-op serum sample, 7.14 + 1.7 pg/ml in 24 h serum sample, 4.42 + 1.2 pg/ml in 72 h serum sample and 6.15 + 1.27 in 1 week serum sample. The mean concentrations of IL-6 in ketorolac group were 5.31 + 1.89 pg/ml in pre-op serum sample, 7.66 + 2.31 pg/ml in 24 h serum samples, 5.22 + 1.53 pg/ml in 72 h serum samples and 7.24 + 2.12 pg/ml in 1 week serum sample. The mean concentrations of IL-6 in tramadol group were 4.99 + 1.8 pg/ml in pre-op serum samples, 10.07 + 4.72 pg/ml in 24 serum samples, 5.2 + 1.74 pg/ml in 72 h serum samples and 6.80 + 1.97 in 1 week serum sample (Table 1). The laboratory reference for IL-6 in a study done by Giannoudis et al. [9] was <5 pg/ml. In another study done by Kraychete et al. [10] the mean range of IL-6 in 10 healthy individuals was found to be 1.2 + 0.8 pg/ml. Peak concentrations of IL-6 were detected between 4 and 6 h after surgery/trauma [11].
In the present study serum IL-6 levels were found to be elevated on first postoperative day (Table 2, 3 and 4) [12]. This was in accordance with the study of Oka et al. Also IL-6 levels had fallen sharply 48–72 h in those patients who had uneventful postoperative course which was a similar finding to that of Baigrie et al. [13]. It was also seen that levels of IL-6 which were higher after surgical extraction of 3rd lower molars decreased after 72 h and again increased on 7th day postoperatively. These results were similar to the study of Carriches et al. [14].
Table 2.
Comparison with the various values of IL-6 at different time intervals with each other within the Diclofenac group
| t | df | Sig. (2-tailed) | |||
|---|---|---|---|---|---|
| Paired sample test for diclofenac | |||||
| Pair 1 | Pre OP-24 h | −10.028 | 19 | .000 | |
| Pair 2 | Pre OP-72 h | .186 | 19 | .854 | |
| Pair 3 | Pre OP-1 week | −3.823 | 19 | .001 | |
| Pair 4 | 24–72 h | 4.370 | 19 | .000 | |
| Pair 5 | 24 h-week | .750 | 19 | .462 | |
| Pair 6 | 72 h-1 week | −6.546 | 19 | .000 | |
Table 3.
Comparison with the various values of IL-6 at different time intervals with each other within the Ketorolac group
| t | df | Sig (2-tailed) | ||
|---|---|---|---|---|
| Paired sample test for ketorolac | ||||
| Pair 1 | Pre OP-24 h | −10.028 | 19 | .000 |
| Pair 2 | Pre OP-72 h | .186 | 19 | .854 |
| Pair 3 | Pre OP-1 week | −3.823 | 19 | .001 |
| Pair 4 | 24 h-72 h | 4.370 | 19 | .000 |
| Pair 5 | 24 h-week | .750 | 19 | .462 |
| Pair 6 | 72 h-1 week | −6.546 | 19 | .000 |
Table 4.
Comparison with the various values of IL-6 at different time intervals with each other within the Tramadol group
| t | df | Siq (2-tailed) | |||
|---|---|---|---|---|---|
| Paired sample test for Tramadol | |||||
| Pair I | Pre OP-24 h | −5.172 | 15 | .000 | |
| Pair 2 | Pre OP-72 h | −.376 | 15 | .712 | |
| Pair 3 | Pre OP-1 week | −2.996 | 15 | .009 | |
| Pair 4 | 24 h-72 h | 4.464 | 15 | .000 | |
| Pair 5 | 24 h-week | 2.967 | 15 | .010 | |
| Pair 6 | 72 h-1 week | −7.162 | 15 | .000 | |
In the present study statistically significant results were obtained (p < .05) between the values of interleukins in the group diclofenac versus tramadol (p = .005) at 24 h which shows that the concentration of IL-6 in diclofenac group was less than that in tramadol group at 24 h post surgically. It indicates that diclofenac was more potent in suppressing the mechanisms which lead to expression of IL-6 in the immune regulatory pathways. There was also a statistically significant difference between the value of IL-6 concentration between ketorolac group and tramadol group (p = .022) at 24 h interval indicating that ketorolac is able to suppress the IL-6 concentration better than the tramadol group at 24 h post surgically. Comparison between the two NSAID groups showed that there was no statistically significant difference at 24 h interval between the concentrations of IL-6 (p = .587). (Table 5 and 6).
Table 5.
Results after ANOVA analysis showing statistically significant p value of 0.014 in 24 h group
| Sum of squares | df | Mean square | F | Sig. | |
|---|---|---|---|---|---|
| Pre OP | |||||
| Between groups | 4.306 | 2 | 2.163 | .701 | .501 |
| Within groups | 165.880 | 54 | 3.072 | ||
| Total | 170.186 | 56 | |||
| 24 h | |||||
| Between groups | 85.543 | 2 | 42.774 | 4.613 | .014 |
| Within groups | 500.176 | 54 | 9.263 | ||
| Total | 585.724 | 56 | |||
| 72 h | |||||
| Between groups | 8.207 | 2 | 4.103 | 1.811 | .173 |
| Within groups | 120.085 | 53 | 2.266 | ||
| Total | 126.291 | 55 | |||
| 1 week | |||||
| Between groups | 11.912 | 2 | 5.956 | 1.801 | .175 |
| Within groups | 175.239 | 53 | 3.306 | ||
| Total | 187.151 | 55 | |||
The concentration of IL-6 reverts back to the near pre-op levels at 72 h due to the action of the NSAID diclofenac. But the concentration of IL-6 at 1 week was found to be nearly similar to the concentration of IL-6 at 24 h post operatively. This indicates a rise in the concentrations of IL-6, as the drug was administered for 5 days post-operatively only (Table 1).
The present study also shows the similarity of diclofenac and ketorolac on IL-6 concentrations during all the 4 time periods (Graph 1). It also shows that the graph of tramadol is different from those of the 2 NSAIDs. There was no statistical significance between the IL-6 values in the pre-op values of the three drugs (p > .05). The peak IL-6 concentration in tramadol group at 24 h is significantly higher than those of diclofenac and ketorolac. At 72 h post op the IL-6 levels in all three drug groups were similar with the values not showing any statistical significance in comparison to each other. Also the 1 week post op concentration of IL-6 in tramadol group is different from that of the two NSAIDs. At 1 week post op there was no significant statistical significance between the values of IL-6 in the two groups ketorolac and tramadol (p = .537), and diclofenac and tramadol (p = .516) but the values between diclofenac and ketorolac (p = .031) was statistically significant. Diclofenac proved to be a better drug than ketorolac in suppression of IL-6 at 1 week. Even though tramadol was better in suppressing the IL-6 levels than ketorolac at 1 week the difference was not statistically significant. The IL-6 suppression at 1 week in tramadol and diclofenac groups was similar as the values were not different statistically.
Graph 1.
Depicts the similarity of diclofenac and ketorolac on IL-6 concentrations during all 4 time periods
Conclusion
The results of our study showed that all three drugs i.e. Diclofenac, Ketorolac and Tramadol have properties which can down regulate the production of IL-6 in response to surgical trauma after the removal of lower third molars. Amongst the three drugs, Diclofenac 50 mg and Ketorolac 10 mg administered immediately following the surgery showed similar values in suppression of IL-6 than Tramadol 50 mg at 24 h interval post surgically, but the differences were not statistically significant. Further studies would be required to elaborate the correlation between the post op morbidity and the IL-6 levels in the serum or at the surgical site to find out the analgesic drugs which best suit the needs of the patients.
Acknowledgments
Conflict of interest
None.
Contributor Information
Puneet Singh, Email: drpuneetsingh65@hmail.com.
Sanjay Rastogi, Phone: +91-8439783274, Email: docos79@gmail.com.
Mansi Bansal, Email: drmansibansal@gmail.com.
Sanjeev Kumar, Email: saxroy@yahoo.com.
Rakesh Singh, Email: dr.rakesh22@gmail.com.
Sumita G. Nishad, Email: sgiri_2000@yahoo.com
Mahendra P. Reddy, Email: docmahen78@gmail.com
Kumar Rakshak Anand, Email: gr8doctor41@gmail.com.
Saurabh Kumar, Email: neha.dentist@gmail.com.
References
- 1.Cruickshank AM, et al. Serum interleukin 6 (IL-6) - effect of surgery and under-nutrition. Clini Nutr. 1991;10(Supp):65–69. doi: 10.1016/0261-5614(91)90118-V. [DOI] [PubMed] [Google Scholar]
- 2.Mahdy AM, et al. Differential modulation of interleukin-6 and interleukin-10 by diclofenac in patients undergoing major surgery. Br J Anaesth. 2002;88(6):797–802. doi: 10.1093/bja/88.6.797. [DOI] [PubMed] [Google Scholar]
- 3.Kim MH et al (2001) Plasma levels of interleukin-6 and interleukin-10 are affected by ketorolac as an adjunct to patient-controlled morphine after abdominal hysterectomy. Clin J Pain 17:72–77 [DOI] [PubMed]
- 4.El-Sharrwy EA, et al. Attenuation of C-reactive protein increases after exodontia by tramadol and ibuprofen. Anesth Prog. 2006;53:78–82. doi: 10.2344/0003-3006(2006)53[78:AOCPIA]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mishra H, Khan FA. A double-blind, placebo-controlled randomized comparison of pre and postoperative administration of ketorolac and tramadol for dental extraction pain. J Anaesthesiol Clin Pharmacol. 2012;28(2):221–225. doi: 10.4103/0970-9185.94892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Y-M, et al. Effect of tramadol on immune responses and nociceptive thresholds in a rat model of incisional pain. J Zhejiang Univ Sci B. 2008;9(11):895–902. doi: 10.1631/jzus.B0820039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bamgbose BO, et al. Effects of co-administerd dexamethasone and diclofenac potassium on pain, swelling and trismus following third molar surgery. Head Face Med. 2005;1:11. doi: 10.1186/1746-160X-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamza M, et al. Mechanisms of non-opioid analgesics beyond cyclooxygenase enzyme inhibition. Curr Mol Pharmacol. 2009;2(1):1–14. doi: 10.2174/1874467210902010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giannoudis PV, et al. Serum CRP and IL-6 levels after trauma not predictive of septic complications in 31 patients. Acta Orthop Scand. 1998;69(2):184–188. doi: 10.3109/17453679809117625. [DOI] [PubMed] [Google Scholar]
- 10.Kraychete DC, et al. Proinflammatory cytokines in patients with neuropathic pain treated with tramadol. Rev Bras Anesthesiol. 2009;59(3):297–303. doi: 10.1590/S0034-70942009000300004. [DOI] [PubMed] [Google Scholar]
- 11.Miyawaki T, et al. Elevation of plasma interleukin-6 level in patients undergoing oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:15–20. doi: 10.1016/S1079-2104(96)80140-5. [DOI] [PubMed] [Google Scholar]
- 12.Oka Y, et al. Circulating interleukin 6 as a useful marker for predicting postoperative complications. Cytokine. 1992;4(4):298–304. doi: 10.1016/1043-4666(92)90070-8. [DOI] [PubMed] [Google Scholar]
- 13.Baigrie RJ, et al. Systemic cytokine response after major surgery. Br J Surg. 1992;79(8):757–760. doi: 10.1002/bjs.1800790813. [DOI] [PubMed] [Google Scholar]
- 14.Carriches CL, et al. Variations of interleukin-6 after surgical removal of lower third molars. Med Oral Patol Oral Cir Bucal. 2006;11:E520–E526. [PubMed] [Google Scholar]