Abstract
Facial pain associated with temporomandibular joint (TMJ) and surrounding structures has been a challenge to clinicians as far as diagnosis and management is concerned. Complexity of anatomical structures within a small area, function of teeth and surrounding periodontal ligament, action of muscles, pathologies, lack of diagnostic investigations, all these complicate specific diagnosis of TMJ disorders. Various classifications have been designed and studied to help diagnose and treat TMJ related disorders, of which the simplest one is pain from TMJ proper and surrounding muscles. Many treatment modalities to treat pain arising from muscles around TMJ like splints, mouth restriction exercises, injection of sclerosing agents etc. have been used with various degrees of success. Botulinum toxin has been shown to be effective in the treatment of oro-facial pain due to muscular disorders and the same is discussed in detail in this review literature.
Keywords: Botulinum toxin, Temporomandibular joint disorders, Muscles of TMJ, Botox in TMJ
Introduction and History
Temporomandibular joint is a diarthroidal joint, which is a discontinuous articulation of glenoid fossa and mandibular condyle permitting freedom of movement that is dictated by associated muscles and limited by associated ligaments. This joint serves many functional purposes; chief among them being deglutition and speech [1].
Temporomandibular joint disorders (TMD) occur in 10 % of population and about 20–25 % of them seek professional care [2].
The TMJ involves diverse group of disorders that are characterized by pain that is specific to and around the joint structures. These disorders may be divided into the following primary groups:
Those related to the muscles acting on the joint and those related to the joint proper [2].
The unique nature of TMD resides in the proximate anatomy of many other facial and cranial structures that complicate, interact with, and mimic other sources of head and neck pain [3].
Patients may complain of pain in and around the joint, painful opening and closing, difficulty in mastication and speech, chronic headaches or earaches due to radiation of pain. Tenderness is usually found over the temporalis, masseter and medial pterygoid muscles [4].
Pain caused by temporomandibular disorders originates from either muscular or articular conditions, or both. Signs and symptoms may be specific or nonspecific. The strong relationship between articular and muscular disorders makes accurate diagnosis difficult. Patients suffering from muscular disorders will have tenderness to palpation of two or more muscle sites. They report of pain or ache in the jaw, temples, face, preauricular area, or inside the ear at rest or during function [5]. It has been reported that approximately 50 % of all TMDs are masticatory myalgias or painful masticatory muscle disorders [6].They are more frequently induced by stress-related parafunctional habits (i.e. clenching and grinding) and rarely by mechanical causes such as occlusal prematurities or high dental restorations. Muscular disorders are thought to possibly play a causative role in degenerative disease of the TMJ.
The etiology of articular disorders may be degenerative, traumatic, infectious, immunologic, metabolic, neoplastic, congenital, or developmental. Pain in one or both joint sites during palpation, presence of joint sounds, and limitation of mandibular opening or pain in the joint during maximum unassisted and assisted opening are features of articular disorders. TMJ pain from an articular disorder may conversely lead to myofascial pain. This is thought to occur due to reflex muscle contractions in the muscles of mastication [6].
Current treatment options include medications such as systemic narcotics, anti-inflammatory agents and muscle relaxants; physical treatments such as orthotic appliances, physical or massage therapy and acupuncture and surgical interventions such as arthrocentesis, arthroscopy, and open arthrotomy [7].
Botulinum toxin is a neurotoxin, 150 kD in weight, produced by Clostridium botulinum, an anaerobic, spore-forming, gram positive, rod bacterium responsible for botulism (a disease detected by Justinius Kerner in 1817, caused by eating improperly preserved sausages). The family of botulinum neurotoxins includes seven distinct serotypes identified as A, B, C, D, E, F and G. Types A and B have shown beneficial effects in humans [8].
The therapeutic use of BTX-A was first attempted in primates by Scott et al. in 1973. They subsequently reported its application in the treatment of strabismus in humans in 1980 [9]. BTX-A has been shown to run on matter be effective in the treatment of blepharospasm [10], strabismus, hemifacial spasm [11], spasmodic torticollis [12], oromandibular dystonia and spasmodic dysphonia [13].
Botulinum toxin A acts by temporary chemical denervation of skeletal muscle. It causes dose dependent paralysis in skeletal muscle by blocking the release of acetylcholine from motor nerve endings [14, 15]. Temporomandibular joint disorders have a strong musculogenic component. Muscles with hyperactivity or injury-related pain are usually abnormally shortened with increased tone and tension. In addition are characterised by the presence of tender, firm nodules called trigger points. Within each trigger point is a hyperirritable spot, the ‘taut-band’, which is composed of hypercontracted muscle fibres. Palpation of the trigger point provokes radiating, aching-type of pain [16].
Evidence suggests botulinum toxin type A also causes an indirect reduction in sensory feedback through the inhibition of acetylcholine release from gamma motor neurons.It has also been shown to inhibit release of neurotransmitters involved in the generation of pain, such as glutamate, substance P, and calcitonin gene-related peptide [17]. This particular action has led many surgeons to use it for temporomandibular disorders which has a strong musculogenic component.
The action of botulinum toxin is reversible; occurs within 1–14 days, peaks at approximately 4 weeks, and begins wearing off after 10–12 weeks.
Over the past several years, botulinum toxin has been increasingly utilized as an adjuvant treatment for head and neck pain such as tension type headaches and migraine headaches. In recent years, there have been reports describing the use of botulinum toxin for TMDs such as bruxism, clenching, masseteric hypertrophy, recurrent dislocation of the temporomandibular joint, oromandibular dystonias, and chronic myogenous orofacial pain [18].
Botulinum Toxin for Temporomandibular Joint Disorder
Schwartz and Freund [4] conducted a study in 11 patients with muscular and arthrogenous pain symptoms and found that 90 % of them showed an overall improvement in pain and function following injection of botulinum toxin type A. Girdler [19] also reported an improvement in pain symptoms in 2 patients with chronic facial pain and muscle spasms.
In a small series, von Linder et al. [20] treated 7 patients with unilateral and bilateral masseter and temporalis muscle hypertrophy with BTX-A injections into the specific muscles. All the patients had chronic facial swelling as their primary complaint for seeking treatment. The authors noted marked decrease in the size of the affected musculature. Patients received 1, 2, or 3 sets of injections depending on the clinical response. All patients were followed up for minimum of 25 months, with no relapse of the muscular hypertrophy. In a second larger study, von Linder [21] recruited 90 patients with chronic facial pain caused by hyperactivity of the masticatory muscles, parafunctional movement and hypermobility disorders. He excluded patients with poorly defined pain syndromes, arthrogenic TMD, nonspecific pain radiation patterns and pain lacking a reference muscle. Subjects were randomized in a double-blind fashion to receive either BTX-A in saline solution or pure saline injections into their particular hyperactive muscles. Over 90 % of patients receiving the BTX-A solution showed a decrease in facial pain; the overall average improvement for the group was a decrease of 3.2 points on the VAS scale versus a 0.4 point difference for the placebo group (P _ 0.01). Noticeably, the patients with the greatest pretreatment pain intensity had the largest decrease in pain [21].
A detailed prospective report of this method was provided by Isaac et al. [22] and To et al. [23] who reported 31 % reduction in muscle mass bulk in five masseteric hypertrophy patients.
In 1997, Moore and Wood [24] described the treatment of recurrent, involuntary temporomandibular joint dislocation using botulinum toxin A. The injected target was the lateral pterygoid muscle, and they injected each lateral pterygoid using electromyography guidance. The authors reported that the effect lasted for 10 months. Daelen et al. [25] also reported on the treatment of a 56-year-old woman with a muscle spasm secondary to multiple sclerosis, which produced recurrent dislocation of the temporomandibular joint. They used botulinum toxin type A repeatedly and injected the masseter and the lateral pterygoid muscles; the effect lasted for 4 months. Bakke et al. [26] described injection of botulinum toxin in lateral pterygoid muscle bilaterally in two patients with severe, long-term TMJ clicking associated with anterior disc displacement and found clicking absent during 1 year of observation with improvement in disk–condyle relationship. Botulinum toxin-A injections for the anterior displacements in 26 patients were particularly studied by Karacalar et al. [27] with injection of toxin specifically on lateral pterygoids. They found decrease in pain scores and increase in mouth opening with this technique. Atilla Arinci et al. [28] injected 20 U of botulinum toxin into the lateral pterygoid muscles in forty-three subjects with anterior disc displacement and reported improved subjective measures starting from the first month. Blitzer et al. [29] first described the injection of botulinum toxin type A into the external pterygoid muscles under electromyographic (EMG) control for the treatment of oromandibular dystonia.
Botulinum toxin injection for patients with bruxism was first described by Van Zandijcke and Marchau [30] and has been reported to be an effective treatment. Tan and Jankovic [31] reported on the long-term treatment of 18 severe bruxism cases with botulinum toxin type A. All these patients had severe bruxism that had been causing symptoms for an average of 14.8 ± 10.0 years and all had no success with prior medical or dental treatment procedures. The investigators injected the masseter muscle with a mean dose of the 61.7 U per side. The efficacy of these injections was rated by the subjects as a 3.4 on a scale from 0 to 4 (with 4 being equal to total cessation of the behavior). Monroy and da Fonseca [32] in 2006 and subsequently Guarda-Nardini et al. [33] in 2008, showed significant improvement in patients with bruxism after injecting botulinum toxin in masseter and temporalis muscles.
Injection Technique for Botulinum Toxin
A thorough knowledge of underlying anatomy of muscles that may be involved in TMD is essential for both diagnosis and treatment. The technique was first described by Schwartz and Freund [4] in 2002.
Botulinum toxin injection for TMD primarily targets the muscles of mastication and is typically administered by injecting the primary muscle groups in a fixed position technique. The temporalis and masseter muscles are almost universally affected and are the most common muscles injected (Fig. 1).
Fig. 1.
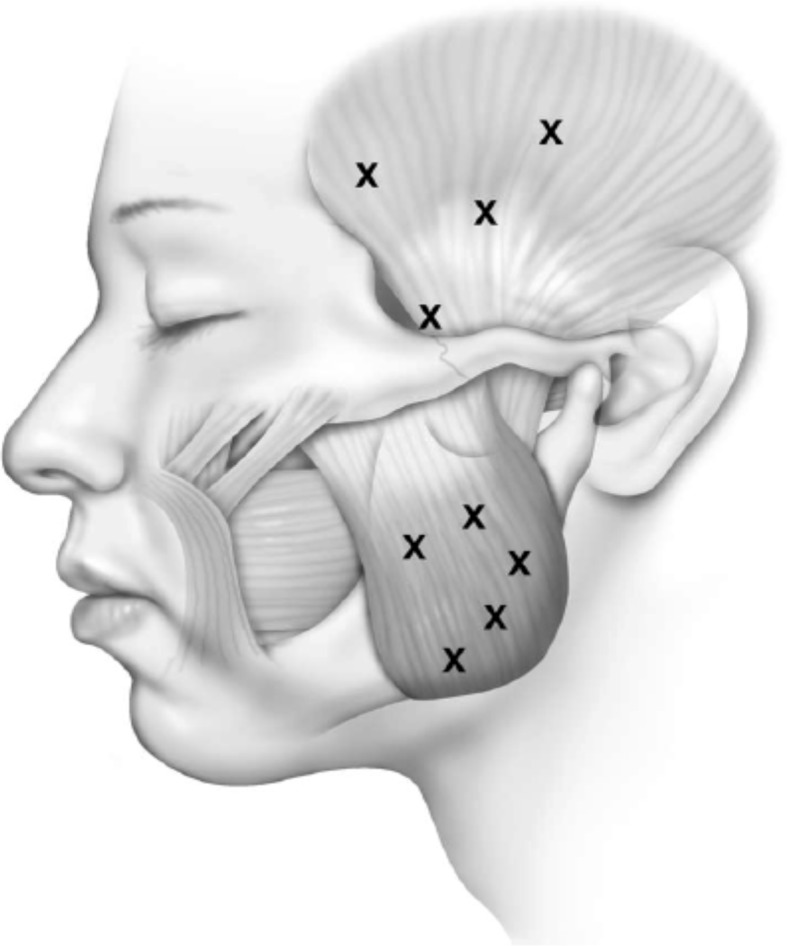
Lateral facial diagram of the position of injections in the temporalis and masseter muscles [3]
The temporalis is a large fan-shaped muscle that covers the lateral aspect of the cranium, originating from the temporal line and inserting to the coronoid process of the mandible. Two types of injections—superficial and deep are used to adequately weaken this muscle. Superficial injections are performed into the thinner upper regions of the muscle in a fan shape.
Deeper injection requires special anatomic consideration. Superficial temporal fascia is split approx. 1.5 cm superior to the zygomatic arch. In this area there are two superficial fascia layers with fat in between, whereas muscle is deeper. If the operator uses the tactile sensation of the needle through fascia as guide, two penetrations are necessary. Under EMG guidance, the muscle is located below the fascia and toxin is injected. This technique is useful as the muscle is thickest before insertion on the coronoid process of mandible (Fig. 1).
The masseter muscle originates from the inferior border of the zygomatic arch and inserts into the lateral surface of the ramus and the coronoid process. Approximately 5 diffuse injections are recommended; preferably targeted to areas of highest activity on (EMG), greatest muscle bulk and greatest discomfort. Care must be taken because, injection of the masseter muscles may cause diffusion of toxin into the nearby zygomaticus major, resulting in an asymmetric smile noted by inability to raise the corner of the mouth. Depending upon the severity, 25–50 units of botulinum toxin is injected into the masseter and temporalis muscles in cases of bruxism, clenching, muscle hypertrophy, muscle hyperactivity and oromandibular dystonia.
The lateral pterygoid muscle injection requires EMG guidance because of its size and location. Extraoral approach involves establishing the location of condyle head by palpation as the patient demonstrates a full range of mandibular motion (Fig. 2).
Fig. 2.

Botulinum toxin type A injection into masseter muscle [35]
The needle is advanced at 45° posteriorly to gently engage the condylar head. The needle is then withdrawn slightly and advanced more anteriorly and slightly deeper. The patient is then asked to mobilize the mandible from side to side and aspiration and injection performed once proper position is ascertained (Fig. 3).
Fig. 3.

Injection into lateral pterygoid under EMG guidance [36]
The intraoral approach involves access posterior to the maxillary tuberosity in a lateral direction. Once the needle is inserted through mucosa, it is helpful to visualize the patient’s ear to guide the needle laterally and posteriorly. Care must be taken not to inject into infratemporal fossa area. It is also important to note that the muscle is surrounded by pterygoid plexus of veins. The lateral pterygoid muscle has been injected in patients suffering from TMJ dislocation, anterior disc displacement, clicking, muscular hyperactivity and myofacial pain.
The efficacy of injecting medial pterygoid muscle in most cases is questionable because, adequate relaxation of masseter and temporalis muscles appears to provide enough clinical effect to relieve pain and reduce joint loading.
The medial pterygoid muscle can be injected extraorally via submandibular route. However, the angulation does not lend itself to good visibility or easy access to the superior aspect of the muscle. The intraoral approach allows palpation of the muscle before injection. The needle is targeted by inserting the EMG electrode medial to the jaw and lateral to the pterygomandiular raphe; piercing through the buccinator muscle.
In either technique, care must be taken to stay within the muscle because supero-medial injection can slip into infra-temporal fossa and its contents. Branches of trigeminal nerve, external carotid artery and muscles of pharynx can be adversely affected. Inferior medial injection outside the medial pterygoid muscle can affect the submandibular gland as well as muscles of floor of the mouth.
Safety
Botulinum toxin is a safe therapy when administered in appropriate doses by an experienced clinical specialist. Use of EMG localization to ensure proper placement of the needle is mandatory. Depending on the target muscle, injection dose is 10–50 U of Botox type A per site with a total dose of 200 U in the masticatory system. The most common side effect is adjacent muscle weakness due to diffusion of the solution [34]. Botulinum toxin is contraindicated in patients taking aminoglycosides, penicillamine, quinine, and calcium blockers, pregnant or lactating mothers, and those afflicted with a neuromuscular disorder (e.g. myasthenia gravis, Eaton-Lambert syndrome). Some patients develop antibodies to the toxin. It is unclear exactly which factors predispose to development of antibodies, but some studies suggest that risk is increased by higher and more frequent injections, and for this reason injections are done no more than once every 12 weeks.
Conclusion
Botulinum toxin is emerging as a very potent and valuable clinical tool for the diagnostic and therapeutic care of TMD. It provides significant relief from TMD pain, reduces intensity, frequency, and duration of recurrent episodes. Bruxism, clenching, subluxation, masseteric hypertrophy, recurrent dislocation of the temporomandibular joint, oromandibular dystonias, and chronic myogenous orofacial pain trigger point injections are various applications that can be successfully treated with botulinum toxin. But clinical trials are sought to provide a scientific basis for the use of botulinum toxin in TMJ disorders due to muscle dysfunction.
References
- 1.DuBrul EL (1980) Sicher’s oral anatomy. 7th ed. C.V. Mosby, St. Louis (MO), p 146–61, 174–209
- 2.Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. 1999;13:232–237. [PubMed] [Google Scholar]
- 3.Bentsianov B, et al. Botulinum toxin treatment for TMD. Operative Tech Otolaryngol Head Neck Surg. 2004;15(2):110–113. doi: 10.1016/j.otot.2004.02.002. [DOI] [Google Scholar]
- 4.Schwartz M, Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain. 2002;18(suppl 6):S198–S203. doi: 10.1097/00002508-200211001-00013. [DOI] [PubMed] [Google Scholar]
- 5.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I: epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):453–462. doi: 10.1016/j.tripleo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 6.Herb, et al. Temporomandibular joint pain and dysfunction. Curr Pain Headache Rep. 2006;10:408–414. doi: 10.1007/s11916-006-0070-7. [DOI] [PubMed] [Google Scholar]
- 7.Freund B, Schwartz M, Symington JM. Botulinum toxin: new treatment for temporomandibular disorders. Br J Oral Maxillofac Surg. 2000;38:466–471. doi: 10.1054/bjom.1999.0238. [DOI] [PubMed] [Google Scholar]
- 8.Simpson LL. The origin, structure, and pharmacological activity of botulinum toxin. Pharmacol Rev. 1981;33:155–188. [PubMed] [Google Scholar]
- 9.Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. Ophthalmology. 1980;87:1044. doi: 10.1016/S0161-6420(80)35127-0. [DOI] [PubMed] [Google Scholar]
- 10.Jankovic J. Blepharospasm with basal ganglia lesions. Arch Neurol. 1986;43:866. doi: 10.1001/archneur.1986.00520090006004. [DOI] [PubMed] [Google Scholar]
- 11.Jankovic J, Fahn S. Dystonic syndromes. In: Jankovic J, Tolosa E, editors. Parkinson’s Disease and Movement Disorders. Baltimore, MD: Urban & Schwarzenberg; 1988. pp. 283–314. [Google Scholar]
- 12.Jankovic J, Orman J. Botulinum A toxin for cranial-cervical dystonia: a double-blind, placebo-controlled study. Neurology. 1987;37:616. doi: 10.1212/WNL.37.4.616. [DOI] [PubMed] [Google Scholar]
- 13.Blitzer A, Brin MF, Green PE, et al. Botulinum toxin injection for the treatment of oromandibular dystonia. Trans Am Laryngol Assoc San Francisco. 1989;110(April):1–2. doi: 10.1177/000348948909800202. [DOI] [PubMed] [Google Scholar]
- 14.Simpson LL. The origin, structure, and pharmacological activity of botulinum toxin. Pharmacol Rev. 1981;33:155–188. [PubMed] [Google Scholar]
- 15.Brin MF. Botulinum toxin: chemistry, pharmacology, toxicity, and immunology. Muscle Nerve Suppl. 1997;6:S146–S168. doi: 10.1002/(SICI)1097-4598(1997)6+<146::AID-MUS10>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 16.Wheeler AH. Myofascial pain disorders: theory to therapy. Drugs. 2004;64(1):45–62. doi: 10.2165/00003495-200464010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Göbel H. Jost WH: Botulinum toxin in specific pain therapy. Schmerz. 2003;17:149–165. doi: 10.1007/s00482-003-0203-4. [DOI] [PubMed] [Google Scholar]
- 18.Schwartz M, Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain. 2002;18(suppl 6):S198–S203. doi: 10.1097/00002508-200211001-00013. [DOI] [PubMed] [Google Scholar]
- 19.Girdler NM. Use of botulinum toxin to alleviate facial pain (letter) Br J Hosp Med. 1994;52:363. [PubMed] [Google Scholar]
- 20.von Lindern JJ, Niederhagen B, Appel T, et al. Type A botulinum toxin for the treatment of hypertrophy of the masseter and temporal muscles: an alternative treatment. Plast Reconstr Surg. 2001;107:327–332. doi: 10.1097/00006534-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 21.von Lindern JJ, Niederhagen B, Berge S, et al. Type A botulinum toxin in the treatment of chronic facial pain associated with masticatory hyperactivity. J Oral Maxillofac Surg. 2003;61:774–778. doi: 10.1016/S0278-2391(03)00153-8. [DOI] [PubMed] [Google Scholar]
- 22.Isaac AM, Moss CE, Whear NM (2000) Unilateral temporalis muscle hypertrophy managed with botulinum toxin type-A. Br J Oral Maxillofac Surg 38:571–2. Comments in: Br J Oral Maxillofac Surg 2001;39:483 [DOI] [PubMed]
- 23.To EW, Ahuja AT, Ho WS, et al. A prospective study of the effect of botulinum toxin A on masseteric muscle hypertrophy with ultrasonographic and electromyographic measurement. Br J Plast Surg. 2001;54:197–200. doi: 10.1054/bjps.2000.3526. [DOI] [PubMed] [Google Scholar]
- 24.Moore AP, Wood GD. Medical treatment of recurrent temporomandibular joint dislocation using botulinum toxin A. Br Dent J. 1997;183:415–417. doi: 10.1038/sj.bdj.4809523. [DOI] [PubMed] [Google Scholar]
- 25.Daelen B, Thorwirth V, Koch A. Treatment of recurrent dislocation of the temporomandibular joint with type A botulinum toxin. Int J Oral Maxillofac Surg. 1997;26:458–460. doi: 10.1016/S0901-5027(97)80014-8. [DOI] [PubMed] [Google Scholar]
- 26.Bakke M, Moller E, Werdelin LM, Dalager T, Kitai N, Kreiborg S. Treatment of severe temporomandibular joint clicking with botulinum toxin in the lateral pterygoid muscle in two cases of anterior disc displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:693–700. doi: 10.1016/j.tripleo.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 27.Karacalar A, Yilmaz N, Bilgici A, Baş B, Akan H. Botulinum toxin for the treatment of temporomandibular joint disk disfigurement: clinical experience. J Craniofac Surg. 2005;16:476–481. doi: 10.1097/04.SCS.0000157263.73768.64. [DOI] [PubMed] [Google Scholar]
- 28.Arinci Atilla, et al. Effect of injection of botulinum toxin on lateral pterygoid muscle used together with the arthroscopy in patients with anterior disk displacement of the temporomandibular joint. J Cranf Surg. 2005;19:122. [PubMed] [Google Scholar]
- 29.Blitzer A, Brin MF, Greene PE, Fahn S. Botulinum toxin injection for the treatment of oromandibular dystonia. Ann Otol Rhinol Laryngol. 1989;98:93–97. doi: 10.1177/000348948909800202. [DOI] [PubMed] [Google Scholar]
- 30.Van Zandijcke M, Marchau MM. Treatment of bruxism with botulinum toxin injections. J Neurol Neurosurg Psychiatry. 1990;53:530. doi: 10.1136/jnnp.53.6.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan EK, Jankovic J. Treating severe bruxism with botulinum toxin. J Am Dent Assoc. 2000;131:211–216. doi: 10.14219/jada.archive.2000.0149. [DOI] [PubMed] [Google Scholar]
- 32.Monroy PG, da Fonseca MA. The use of botulinum toxin-A in the treatment of severe bruxism in a patient with autism: a case report. Spec Care Dentist. 2006;26:37–39. doi: 10.1111/j.1754-4505.2006.tb01508.x. [DOI] [PubMed] [Google Scholar]
- 33.Guarda-Nardini L, Manfredini D, Salamone M, et al. Efficacy of botulinum toxin in treating myofascial pain in bruxers: a controlled placebo pilot study. Cranio. 2008;26:126–135. doi: 10.1179/crn.2008.017. [DOI] [PubMed] [Google Scholar]
- 34.Eleopra R, Tugnoli V, Caniatti L, De Grandis D. Botulinum toxin treatment in the facial muscles of humans: evidence of an action in untreated near muscles by peripheral local diffusion. Neurology. 1996;46:1158–1160. doi: 10.1212/WNL.46.4.1158. [DOI] [PubMed] [Google Scholar]
- 35.Song PC, Schwartz J, Blitzer A (2007) The emerging role of botulinum toxin in the treatment of temporomandibular disorders. Oral Dis 13:253–260 [DOI] [PubMed]
- 36.Lee EH, Kim JY, Kweon HY, Jo YY, Min SK, Park YW et al (2010) A combination graft of low-molecular-weight silk fibroin with Choukroun’s platelet-rich fibrin for rabbit calvarial defect. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:e33–e38 [DOI] [PubMed]


